Distance to Healthcare Facility and Lady Health Workers’ Visits Reduce Malnutrition in under Five Children: A Case Study of a Disadvantaged Rural District in Pakistan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Theoretical Framework
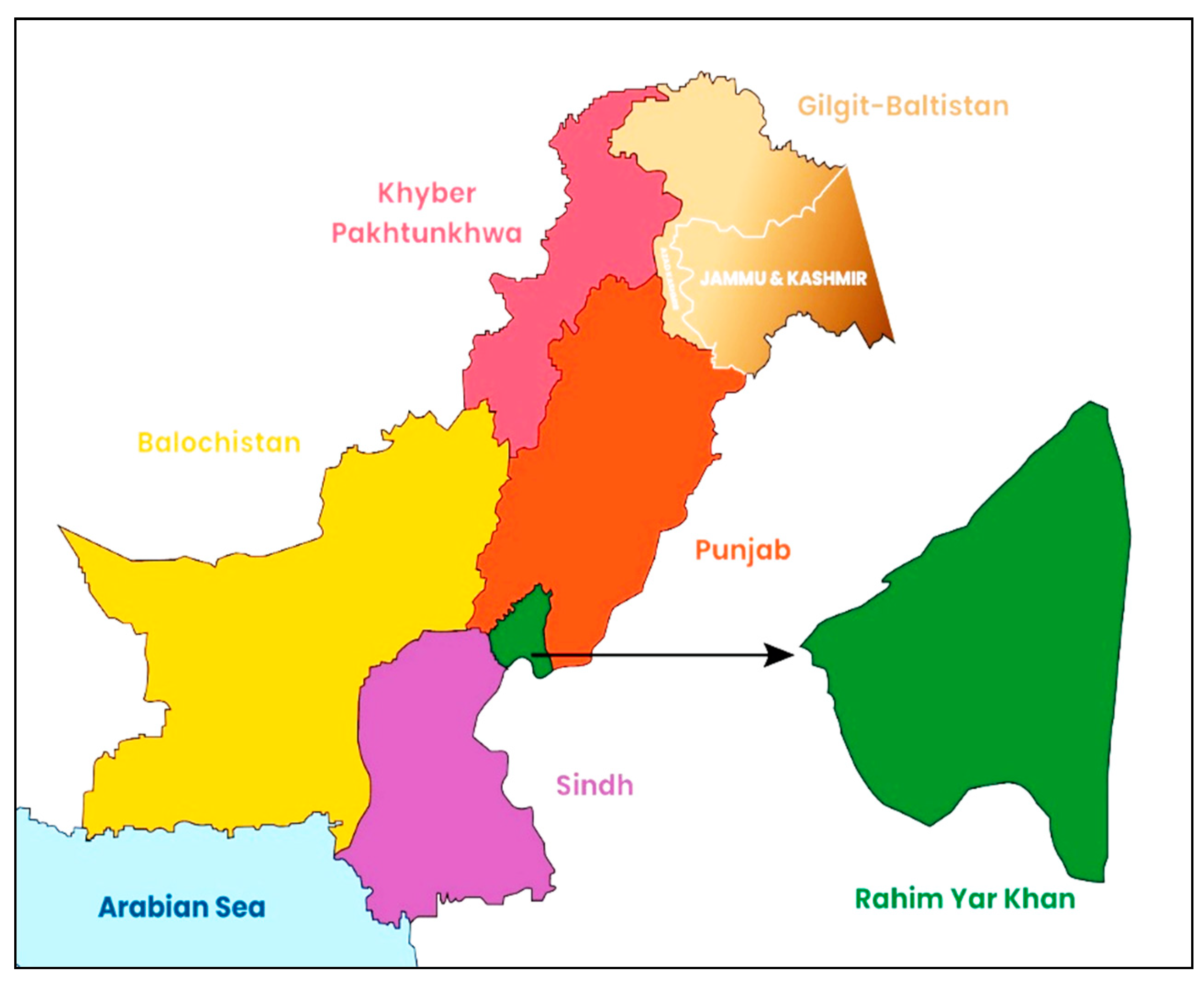
2.2. Study Area and Sampling
2.3. Data Collection
2.4. Ethical Considerations
2.5. Measuring Important Variables
2.6. Statistical Analysis
3. Results
4. Discussion
Limitation of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Wali, N.; Agho, K.; Renzaho, A.M. Past drivers of and priorities for child undernutrition in South Asia: A mixed-methods systematic review protocol. Syst. Rev. 2019, 8, 189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fanzo, J.; Hawkes, C.; Udomkesmalee, E.; Afshin, A.; Allemandi, L.; Assery, O.; Schofield, D. Global Nutrition Report: Shining a Light to Spur Action on Nutrition. 2018. Available online: https://globalnutritionreport.org/reports/global-nutrition-report-2018/ (accessed on 20 April 2020).
- Khaliq, A.; Wraith, D.; Miller, Y.; Nambiar-Mann, S. Prevalence, Trends, and Socioeconomic Determinants of Coexisting Forms of Malnutrition Amongst Children under Five Years of Age in Pakistan. Nutrients 2021, 13, 4566. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Nutrition Landscape Information System (NLIS) Country Profile Indicators: Interpretation Guide; WHO: Geneva, Switzerland, 2019; Available online: https://www.who.int/publications/i/item/9789241516952 (accessed on 30 November 2021).
- World Health Organization. Primary Health Care Systems (PRIMASYS): Comprehensive Case Study from Pakistan; No. WHO/HIS/HSR/17.37; WHO: Geneva, Switzerland, 2017; Available online: https://www.who.int/alliance-hpsr/projects/AHPSR-PRIMASYS-Pakistan-comprehensive-v2.pdf (accessed on 10 March 2022).
- Puett, C.; Coates, J.; Alderman, H.; Sadler, K. Quality of care for severe acute malnutrition delivered by community health workers in southern Bangladesh. Mater. Child. Nutr. 2013, 9, 130–142. [Google Scholar] [CrossRef] [PubMed]
- Rogers, E.; Martínez, K.; Morán, J.L.; Alé, F.G.; Charle, P.; Guerrero, S.; Puett, C. Cost-effectiveness of the treatment of uncomplicated severe acute malnutrition by community health workers compared to treatment provided at an outpatient facility in rural Mali. Hum. Resour. Health 2018, 16, 12. [Google Scholar] [CrossRef]
- López-Ejeda, N.; Charle, C.P.; Vargas, A.; Guerrero, S. Can community health workers manage uncomplicated severe acute malnutrition? A review of operational experiences in delivering severe acute malnutrition treatment through community health platforms. Mater. Child. Nutr. 2019, 15, e12719. [Google Scholar] [CrossRef]
- Punjab Bureau of Statistics. Punjab 2017-18 Multiple Indicator Cluster Survey Key Findings Provincial Report. Lahore, 2018. Available online: https://mics-surveys-prod.s3.amazonaws.com/MICS6/South%20Asia/Pakistan%20%28Punjab%29/2017-2018/Survey%20findings/MICS%20SFR_Final_English.pdf (accessed on 13 February 2022).
- Government of Pakistan. Population Census. Islamabad, 2017. Available online: https://www.pbs.gov.pk/content/final-results-census-2017 (accessed on 9 July 2020).
- Becker, G.S. A Theory of the Allocation of Time. Econ. J. 1965, 75, 493–517. [Google Scholar] [CrossRef] [Green Version]
- Strauss, J.; Thomas, D. Human Resources: Empirical Modeling of Household and Family Decisions. In Handbook of Development Economics; Behrman, J.B., Srinivasan, T.N., Eds.; Elsevier: Amsterdam, The Netherlands, 1995; p. 3. [Google Scholar]
- World Health Organization. Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children: A Joint Statement by the World Health Organization and the United Nations Children’s Fund; WHO: Geneva, Switzerland, 2009; Available online: https://www.who.int/nutrition/publications/severemalnutrition/9789241598163/en/ (accessed on 2 September 2018).
- Bhutta, Z.A.; Hafeez, A. What can Pakistan do to address maternal and child health over the next 386 decade? Health Res. Policy Syst. 2015, 13, 13–16. [Google Scholar] [CrossRef] [Green Version]
- Afzal, S.; Naeem, A.; Shahid, U.; Syed, W.N.; Khan, U.; Zaidi, N.M. Effective role of lady health 388 workers in immunization of children in Pakistan. Pak. J. Med. Sci. 2016, 32, 1500–1505. [Google Scholar] [CrossRef]
- Noh, J.W.; Kim, Y.M.; Akram, N.; Yoo, K.B.; Cheon, J.; Lee, L.J.; Kwon, Y.D.; Stekelenburg, J. Impact of socio-economic factors and health information sources on place of birth in Sindh Province, Pakistan: A secondary analysis of cross-sectional survey data. Int. J. Environ. Res. Pub. Health 2019, 16, 932. [Google Scholar] [CrossRef] [Green Version]
- Rogers, E.; Ali, M.; Fazal, S.; Kumar, D.; Guerrero, S.; Hussain, I.; Soofi, S.; Morán, J.L. Quality of care of treatment for uncomplicated severe acute malnutrition provided by lady health workers in Pakistan. Pub. Health Nutr. 2018, 21, 385–390. [Google Scholar] [CrossRef] [Green Version]
- Zaidi, S.; Huda, M.; Ali, A.; Gul, X.; Jabeen, R.; Shah, M.M. Pakistan’s Community-based Lady Health Workers (LHWs): Change Agents for Child Health? Glob. J. Health Sci. 2020, 12, 177–187. [Google Scholar] [CrossRef]
- Gogia, S.; Sachdev, H.S. Home visits by community health workers to prevent neonatal deaths in developing countries: A systematic review. Bull. World Health Organ. 2010, 88, 658–666. [Google Scholar] [CrossRef]
- Sitrin, D.; Guenther, T.; Waiswa, P.; Namutamba, S.; Namazzi, G.; Sharma, S.; Ashish, K.C.; Rubayet, S.; Bhadra, S.; Ligowe, R.; et al. Improving newborn care practices through home visits: Lessons from Malawi, Nepal, Bangladesh, and Uganda. Glob. Health Action 2015, 8, 23963. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mannan, I.; Rahman, S.M.; Sania, A.; Seraji, H.R.; Arifeen, S.E.; Winch, P.J.; Darmstadt, G.L.; Baqui, A. Can early postpartum home visits by trained community health workers improve breastfeeding of newborns? J. Perinat. 2008, 28, 632–640. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tripathi, A.; Kabra, S.K.; Sachdev, H.P.; Lodha, R. Home visits by community health workers to improve identification of serious illness and care seeking in newborns and young infants from low-and middle-income countries. J. Perinatal. 2016, 36, S74–S82. [Google Scholar] [CrossRef] [Green Version]
- Tesfau, Y.B.; Kahsay, A.B.; Gebrehiwot, T.G.; Medhanyie, A.A.; Godefay, H. Postnatal home visits by health extension workers in rural areas of Ethiopia: A cross-sectional study design. BMC Pregn. Childbirth 2020, 20, 305. [Google Scholar] [CrossRef]
- Stansert, K.L.; Tomlinson, M.; Christodoulou, J.; Laurenzi, C.; Le Roux, I.; Baker, V.; Mbewu, N.; Le Roux, K.W.; Rotheram, B.M.J. Home visits by community health workers in rural South Africa have a limited, but important impact on maternal and child health in the first two years of life. BMC Health Serv. Res. 2020, 20, 594. [Google Scholar] [CrossRef]
- Teshome, G.; Bosha, T.; Gebremedhin, S. Time-to-recovery from severe acute malnutrition in children 6–59 months of age enrolled in the outpatient treatment program in Shebedino, Southern Ethiopia: A prospective cohort study. BMC Pediatrics 2019, 19, 33. [Google Scholar] [CrossRef]
- Massa, D.; Woldemichael, K.; Tsehayneh, B.; Tesfay, A. Treatment outcome of severe acute malnutrition and determinants of survival in Northern Ethiopia: A prospective cohort study. Int. J. Nutr. Metab. 2016, 8, 12–23. [Google Scholar]
- Kelly, V.A.; Tefft, J.F.; Oehmke, J.F.; Staatz, J.M. Identifying Policy Relevant Variables for Reducing Childhood Malnutrition in Rural Mali; Michigan State University: East Lansing, MI, USA, 2004; pp. 1–18. [Google Scholar]
- Feikin, D.R.; Nguyen, L.M.; Adazu, K.; Ombok, M.; Audi, A.; Slutsker, L.; Lindblade, K.A. The impact of distance of residence from a peripheral health facility on pediatric health utilisation in rural western Kenya. Trop. Med. Int. Health. 2009, 14, 54–61. [Google Scholar] [CrossRef]
- Schoeps, A.; Gabrysch, S.; Niamba, L.; Sié, A.; Becher, H. The effect of distance to health-care facilities on childhood mortality in rural Burkina Faso. Am. J. Epidemiol. 2011, 173, 492–498. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Timerga, G.; Desta, G.; Haile, G. Magnitude and Factors Associated with Malnutrition in Under Five Children in Semen Shoa Zone, Amhara Region, Ethiopia. Berhan Int. J. Humanit. Soc. Sci. 2020, 3, 1–14. Available online: http://197.156.88.196/index.php/birjsh/article/view/23 (accessed on 29 March 2022).
- Boyd, E. Examining Response to Treatment of Severe Acute Malnutrition in Children 6–59 Months Old in Afghanistan, Chad, Mali, and Niger (P12-002-19). Curr. Dev. Nutr. 2019, 3 (Suppl. 1), nzz035-P12. [Google Scholar] [CrossRef] [Green Version]
- Puett, C.; Guerrero, S. Barriers to access for severe acute malnutrition treatment services in Pakistan and Ethiopia: A comparative qualitative analysis. Pub. Health Nutri. 2015, 18, 1873–1882. [Google Scholar] [CrossRef] [Green Version]
- Aziz, S.Z.; Hanif, I. Primary care and health system performance in Pakistan: A study of basic health units of South Punjab. J. Pak. Med. Assoc. 2016, 66, 1632–1636. Available online: https://jpma.org.pk/article-details/8017 (accessed on 3 March 2021).
- Corden, E.; Siddiqui, S.H.; Sharma, Y.; Raghib, M.F.; Adorno, W.; Zulqarnain, F.; Ehsan, L.; Shrivastava, A.; Ahmed, S.; Umrani, F.; et al. Distance from Healthcare Facilities Is Associated with Increased Morbidity of Acute Infection in Pediatric Patients in Matiari, Pakistan. Int. J. Environ. Res. Public Health 2021, 18, 11691. [Google Scholar] [CrossRef]
- Ahmed, F.; Malik, N.I.; Malik, N.; Qureshi, M.G.; Shahzad, M.; Shahid, M.; Zia, S.; Tang, K. Key Challenges to Optimal Therapeutic Coverage and Maternal Utilization of CMAM Program in Rural Southern Pakistan: A Qualitative Exploratory Study. Nutrients 2022, 14, 2612. [Google Scholar] [CrossRef]
- Shahid, M.; Qureshi, M.G.; Ahmed, J.F. Socio-economic Causes of Malnutrition among Pre-School Children in Pakistan: A Gender-Disaggregated Analysis. Glob. Eco. Rev. 2020, 5, 147–159. [Google Scholar] [CrossRef]
- Shahid, M.; Cao, Y.; Shahzad, M.; Saheed, R.; Rauf, U.; Qureshi, M.G.; Hasnat, A.; Bibi, A.; Ahmed, F. Socio-Economic and Environmental Determinants of Malnutrition in under Three Children: Evidence from PDHS-2018. Children 2022, 9, 361. [Google Scholar] [CrossRef]
- Shahid, M.; Leghari, I.U.; Ahmed, F. Socio-Economic Correlates of Children’s Nutritional Status: Evidence from Pakistan Demographic and Health Survey 2017–18. Glob. Econ. Rev. 2020, 1, 221–233. [Google Scholar] [CrossRef]
- Shahid, M. Interaction of Household Wealth and Women’s Working Status on Child Malnutrition: Evidence from PDHS-2013. Pak. Perspect. 2020, 25, 71–84. [Google Scholar] [CrossRef]
- Naz, L.; Patel, K.K.; Uzoma, I.E. The prevalence of undernutrition and associated factors among preschool children: Evidence from Pakistan Demographic and Health Survey 2017–18. Child. Youth Serv. Rev. 2020, 119, 105579. [Google Scholar] [CrossRef]
- Shafiq, A.; Hussain, A.; Asif, M.; Jameel, A.; Sadiq, S.; Kanwel, S. Determinants of Gender Disparity in Nutritional Intake among Children in Pakistan: Evidence from PDHS. Children 2021, 9, 7. [Google Scholar] [CrossRef]
- Shahid, M.; Ahmed, F.; Ameer, W.; Guo, J.; Raza, S.; Fatima, S.; Qureshi, M.G. Prevalence of child malnutrition and household socioeconomic deprivation: A case study of marginalized district in Punjab, Pakistan. PLoS ONE 2022, 17, e0263470. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.; Shahid, M. Understanding food insecurity experiences, dietary perceptions and practices in the households facing hunger and malnutrition in Rajanpur District, Punjab Pakistan. Pak Perspect. 2019, 24, 115–133. [Google Scholar]
- Shahid, M.; Cao, Y.; Ahmed, F.; Raza, S.; Guo, J.; Malik, N.I.; Rauf, U.; Qureshi, M.G.; Saheed, R.; Maryam, R. Does Mothers’ Awareness of Health and Nutrition Matter? A Case Study of Child Malnutrition in Marginalized Rural Community of Punjab, Pakistan. Front. Pub. Health 2022, 10, 792164. [Google Scholar] [CrossRef]
- Saheed, R.; Hina, H.; Shahid, M. Water, Sanitation and Malnutrition in Pakistan: Challenge for Sustainable Development. Glob. Polit. Rev. 2021, 6, 2521–2974. [Google Scholar] [CrossRef]
- Ahmed, F.; Shahid, M.; Cao, Y.; Qureshi, M.G.; Zia, S.; Fatima, S.; Guo, J. A Qualitative Exploration in Causes of Water Insecurity Experiences, and Gender and Nutritional Consequences in South-Punjab, Pakistan. Int. J. Environ. Res. Pub. Health 2021, 18, 12534. [Google Scholar] [CrossRef]
- Ahmed, F.; Malik, N.I.; Shahzad, M.; Ahmad, M.; Shahid, M.; Feng, X.L.; Guo, J. Determinants of infant young child feeding among mothers of malnourished children in South Punjab, Pakistan: A qualitative study. Front. Public Health 2022, 10, 1–11. [Google Scholar] [CrossRef]


| District | Tehsil | Union Council Name | Availability of LHW | Average Distance to HC Facility | Sample |
|---|---|---|---|---|---|
| Rahim Yar | Khanpur | 1. Bagh-o-Bahar | Yes | 8 km | 26 |
| Khan | 2. Azeem Shah | No | 15 km | 34 | |
| 3. Kotla Pathan | Yes | 12 km | 36 | ||
| Rahim Yar | 4. Bahishti | No | 13 km | 34 | |
| Khan | 5. Sonak | No | 17 km | 46 | |
| 6. Chak No. 84/P | Yes | 19 km | 35 | ||
| Liaquatpur | 7. Ghooka | Yes | 20 km | 25 | |
| 8. Shadani | Yes | 18 km | 26 | ||
| 9. Trinda Gurgaij | Yes | 9 km | 30 | ||
| Sadiqabad | 10. Kot Sanger Khan | Yes | 10 km | 33 | |
| 11. Muhammad Pur | No | 15 km | 32 | ||
| 12. Roshan Bhet | No | 14 km | 27 | ||
| Total | 4 | 12 | Available in UCs = 7 | N = 384 |
| Variables | Categories | Frequencies | Percentages | p-Values |
|---|---|---|---|---|
| Gender of Child | Male | 93 | 47.45 | 0.140 |
| Female | 103 | 52.55 | ||
| Age range of Child (in months) | 0 to 12 | 19 | 9.69 | 0.000 *** |
| 13–24 | 26 | 13.27 | ||
| 25–36 | 60 | 30.61 | ||
| 37–48 | 51 | 26.02 | ||
| 49–60 | 40 | 20.41 | ||
| Birth Order Number | Birth order 1 | 52 | 26.53 | 0.079 * |
| 2 or 3 | 79 | 40.31 | ||
| 4 or 5 | 41 | 20.92 | ||
| 6 or above | 24 | 12.24 | ||
| Income/Wealth Status | Poor | 180 | 91.84 | 0.008 *** |
| Middle | 11 | 5.61 | ||
| Rich | 5 | 2.55 | ||
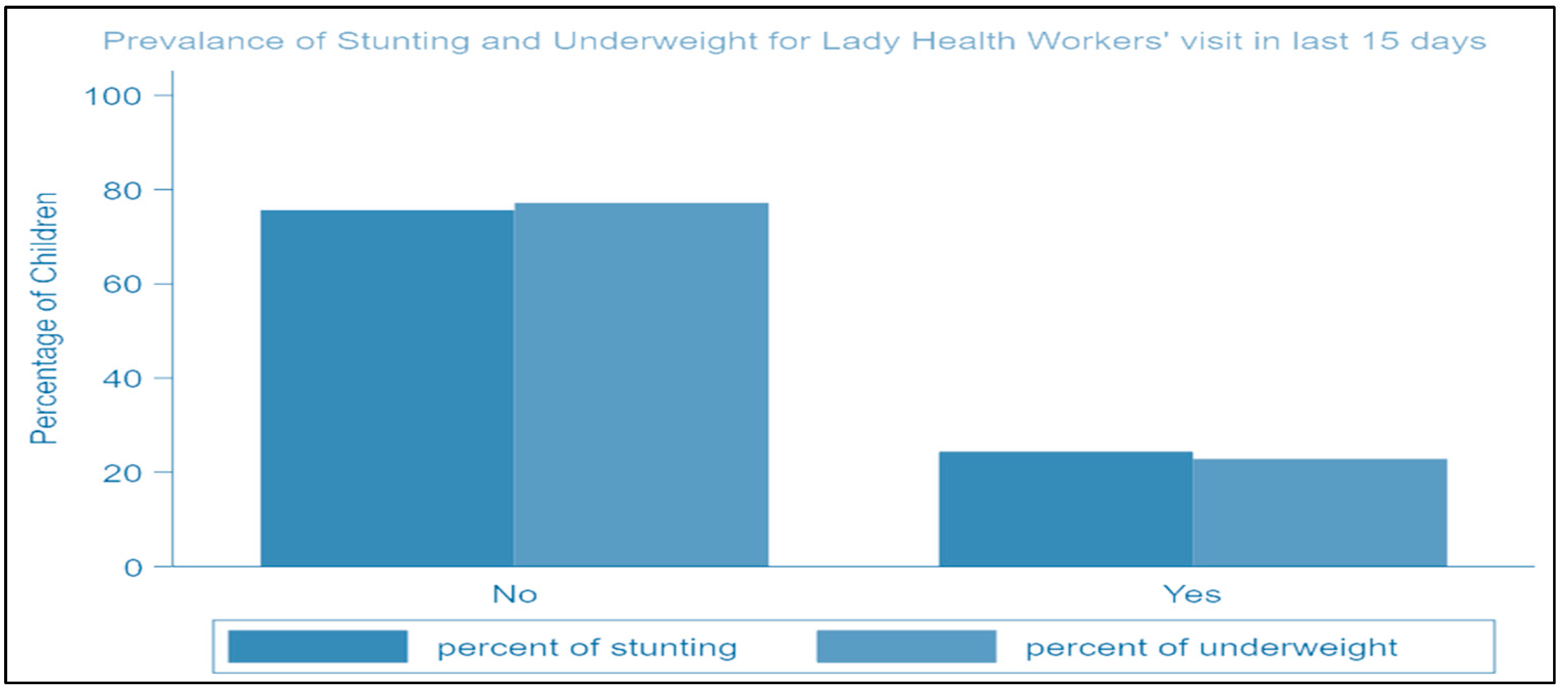
| LHW visit in last 15 days | Yes | 47 | 23.98 | 0.006 *** |
| No | 149 | 76.02 | ||
| Distance to Health Facility | ≤ 2 km | 18 | 9.18 | 0.040 ** |
| 3–4 km | 18 | 9.18 | ||
| ≥5 km | 160 | 81.63 |
| Variables | Categories | Odds Ratio | 95% CI |
|---|---|---|---|
| Gender of Child | Female (Reference-category) | ||
| Male | 0.79 | (0.42, 1. 25) | |
| Age of Child | 0–12 months (Reference-category) | ||
| 13–24 months | 1.31 | (0.55, 3.08) | |
| 25–36 months | 2.39 * | (0.85, 6.67) | |
| 37–48 months | 7.34 *** | (2.63, 20.52) | |
| 49–60 months | 1.04 | (0.43, 2.49) | |
| Number of Birth Order | Birth order 1 (Reference-category) | ||
| 2 or 3 | 0.82 | (0.41, 1.67) | |
| 4 or 5 | 0.44 ** | (0.21, 0.94) | |
| 6 or above | 0.94 | (0.3, 25.57) | |
| Income/Wealth Status | Poor (Reference-category) | ||
| Middle | 3.54 | (0.61, 20.54) | |
| Rich | 0.28 * | (0.07, 1.14) | |
| LHW visit in last 15 days | No (Reference-category) | ||
| Yes | 0.28 *** | (0.09, 0.82) | |
| Distance to Health Facility | ≤2 Km (Reference-category) | ||
| 3–4 km | 2.61 * | (0.85, 8.14) | |
| ≥5 km | 2.88 ** | (0.94, 8.82) | |
| Significance of the overall model | |||
| Number of observations = 310 | Prob > Chi2 = 0.0001 | ||
| LR Chi2 (13) = 54.18 | Pseudo R2 = 0.1329 | ||
| References: Odd ratios and Confidence Intervals | |||
| Indicators (Statements) | St. Agree (5) | Agree (4) | Neutral (3) | Disagree (2) | St. Disagree (1) | Total (N) | A*N | RII | Rank |
|---|---|---|---|---|---|---|---|---|---|
| 1. Gives proper Counselling Regarding Health and Wellbeing | 130 | 84 | 75 | 18 | 23 | 330 | 1920 | 0.17 | 4 |
| 2. Proper Aware to Community on WASH | 80 | 92 | 78 | 22 | 28 | 300 | 1920 | 0.16 | 7 |
| 3. Active in Mother and Childcare (checkups, safe deliveries) | 240 | 80 | 48 | 16 | 12 | 396 | 1920 | 0.21 | 1 |
| 4. Visit Regularly | 110 | 84 | 84 | 26 | 9 | 313 | 1920 | 0.163 | 6 |
| 5. LHW Behavior Remains Good | 100 | 120 | 75 | 34 | 12 | 341 | 1920 | 0.18 | 3 |
| 6. Refer the Complicated Cases to the hospital on time | 80 | 76 | 111 | 46 | 9 | 322 | 1920 | 0.168 | 5 |
| 7. Active on Child Immunization | 210 | 84 | 72 | 18 | 8 | 392 | 1920 | 0.20 | 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shahid, M.; Ameer, W.; Malik, N.I.; Alam, M.B.; Ahmed, F.; Qureshi, M.G.; Zhao, H.; Yang, J.; Zia, S. Distance to Healthcare Facility and Lady Health Workers’ Visits Reduce Malnutrition in under Five Children: A Case Study of a Disadvantaged Rural District in Pakistan. Int. J. Environ. Res. Public Health 2022, 19, 8200. https://doi.org/10.3390/ijerph19138200
Shahid M, Ameer W, Malik NI, Alam MB, Ahmed F, Qureshi MG, Zhao H, Yang J, Zia S. Distance to Healthcare Facility and Lady Health Workers’ Visits Reduce Malnutrition in under Five Children: A Case Study of a Disadvantaged Rural District in Pakistan. International Journal of Environmental Research and Public Health. 2022; 19(13):8200. https://doi.org/10.3390/ijerph19138200
Chicago/Turabian StyleShahid, Muhammad, Waqar Ameer, Najma Iqbal Malik, Muhammad Babar Alam, Farooq Ahmed, Madeeha Gohar Qureshi, Huiping Zhao, Juan Yang, and Sidra Zia. 2022. "Distance to Healthcare Facility and Lady Health Workers’ Visits Reduce Malnutrition in under Five Children: A Case Study of a Disadvantaged Rural District in Pakistan" International Journal of Environmental Research and Public Health 19, no. 13: 8200. https://doi.org/10.3390/ijerph19138200
APA StyleShahid, M., Ameer, W., Malik, N. I., Alam, M. B., Ahmed, F., Qureshi, M. G., Zhao, H., Yang, J., & Zia, S. (2022). Distance to Healthcare Facility and Lady Health Workers’ Visits Reduce Malnutrition in under Five Children: A Case Study of a Disadvantaged Rural District in Pakistan. International Journal of Environmental Research and Public Health, 19(13), 8200. https://doi.org/10.3390/ijerph19138200









