The Typology and Topography of Child Abuse and Neglect: The Experience of a Tertiary Children’s Centre
Abstract
:1. Introduction
1.1. Background
1.2. Aims
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Measures
- -
- Care (or physical) neglect: carer fails to provide for the child’s basic needs, such as food or clothing;
- -
- Environmental neglect: when a serious health and safety hazard is present in a child’s physical surroundings or the house is not adequate in size or cleanliness;
- -
- Medical neglect: failure to provide appropriate medical care when a child is in need of a medical assessment or treatment for injury, illness or disability;
- -
- Educational neglect: carers failing to send the child to school or prevent the child from having a suitable education;
- -
- Supervisory neglect: concerns a situation where a carer leaves a child alone or in inappropriate substitute care.
2.4. Data Analysis
3. Results
3.1. Geographic Mapping and Socioeconomic Profile
3.2. Ethnicity
3.3. Potential Predisposing Factors to Child Abuse and Neglect within the Family Domain
3.3.1. Parental Vulnerability
3.3.2. Previous Involvement with Children’s Social Care
3.3.3. Childhood Disability or Chronic Health Condition
3.4. Presenting Concerns
3.5. Neglect and Emotional Abuse
3.6. Categories of Abuse
4. Discussion
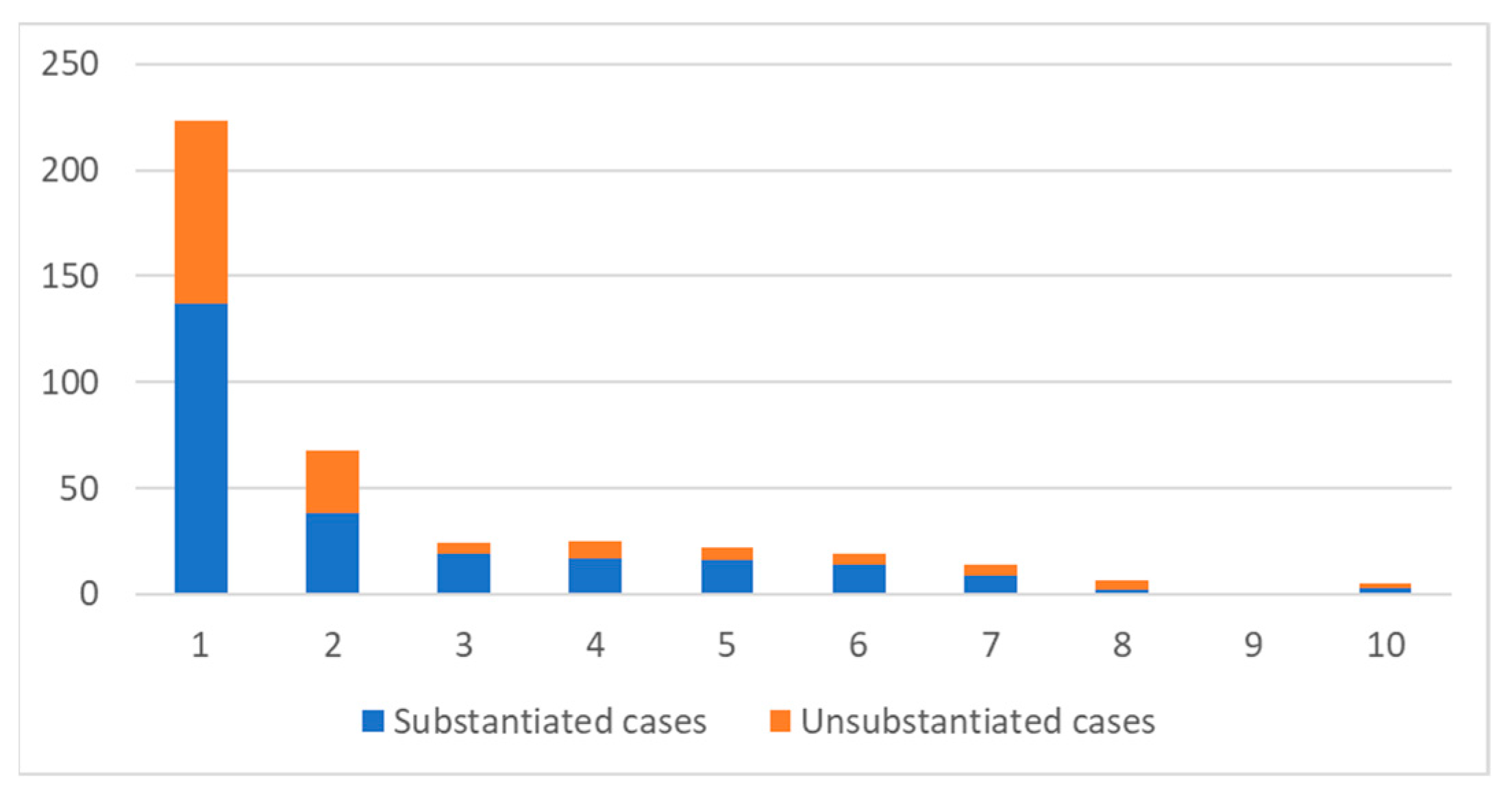
4.1. Case Substantiation
4.2. Ethnicity
4.3. Neighbourhood Poverty
4.4. Potential Predisposing Factors to Child Abuse and Neglect within the Family Domain
4.5. Child’s Previous Involvement with Statutory Bodies
4.6. Presenting Concerns
4.7. Neglect
4.8. Emotional Abuse
4.9. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Reading, R.; Bissell, S.; Goldhagen, J.; Harwin, J.; Masson, J.; Moynihan, S.; Parton, N.; Pais, M.S.; Thoburn, J.; Webb, E. Promotion of children’s rights and prevention of child maltreatment. Lancet 2009, 373, 332–343. [Google Scholar] [CrossRef]
- Connolly, M.; Katz, I. Typologies of Child Protection Systems: An International Approach. Child Abus. Rev. 2019, 28, 381–394. [Google Scholar] [CrossRef]
- Participation, E. Children Act 1989. Statute Law Database. Available online: https://www.legislation.gov.uk/ukpga/1989/41 (accessed on 4 April 2022).
- World Health Organization. Preventing Child Maltreatment: A Guide to Taking Action and Generating Evidence/World Health Organization and International Society for Prevention of Child Abuse and Neglect. Guide Sur Prév Maltraitance Enfants Interv Produire Données. 2006. Available online: https://apps.who.int/iris/handle/10665/43499 (accessed on 4 April 2022).
- World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision, 2nd ed.; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- McKenzie, K.; Scott, D.A. Using Routinely Collected Hospital Data for Child Maltreatment Surveillance: Issues, Methods and Patterns. BMC Public Health 2011, 11, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonzalez-Izquierdo, A.; Woodman, J.; Copley, L.; van der Meulen, J.; Brandon, M.; Hodes, D.; Lecky, F.; Gilbert, R. Variation in recording of child maltreatment in administrative records of hospital admissions for injury in England, 1997–2009. Arch. Dis. Child. 2010, 95, 918–925. [Google Scholar] [CrossRef]
- Scott, D.; Tonmyr, L.; Fraser, J.; Walker, S.; McKenzie, K. The utility and challenges of using ICD codes in child maltreatment research: A review of existing literature. Child Abus. Negl. 2009, 33, 791–808. [Google Scholar] [CrossRef] [Green Version]
- Chandan, J.S.; Keerthy, D.; Zemedikun, D.T.; Okoth, K.; Gokhale, K.M.; Raza, K.; Bandyopadhyay, S.; Taylor, J.; Nirantharakumar, K. The association between exposure to childhood maltreatment and the subsequent development of functional somatic and visceral pain syndromes. eClinicalMedicine 2020, 23, 100392. [Google Scholar] [CrossRef]
- Feng, J.-Y.; Chiang, W.-L.; Lu, T.-H. What’s new in ICD-10-CM in classifying child maltreatment? Child Abus. Negl. 2011, 35, 655–657. [Google Scholar] [CrossRef]
- Schnitzer, P.G.; Slusher, P.L.; Kruse, R.L.; Tarleton, M.M. Identification of ICD codes suggestive of child maltreatment. Child Abus. Negl. 2011, 35, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Department of Education. Characteristics of Children in Need: 2013 to 2014; Table D1 HM Government; Department for Education: Manchester, UK, 2014. [Google Scholar]
- Benbenishty, R.; Jedwab, M.; Chen, W.; Glasser, S.; Slutzky, H.; Siegal, G.; Lavi-Sahar, Z.; Lerner-Geva, L. Predicting the decisions of hospital based child protection teams to report to child protective services, police and community welfare services. Child Abus. Negl. 2014, 38, 11–24. [Google Scholar] [CrossRef]
- Kistin, C.J.; Tien, I.; Bauchner, H.; Parker, V.; Leventhal, J.M. Factors That Influence the Effectiveness of Child Protection Teams. Pediatrics 2010, 126, 94–100. [Google Scholar] [CrossRef] [Green Version]
- 2011 Census Analysis: Ethnicity and Religion of the Non-UK Born Population in England and Wales—Office for National Statistics. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity/articles/2011censusanalysisethnicityandreligionofthenonukbornpopulationinenglandandwales/2015-06-18 (accessed on 4 April 2022).
- Marco, M.; Maguire-Jack, K.; Gracia, E.; López-Quílez, A. Disadvantaged neighborhoods and the spatial overlap of substantiated and unsubstantiated child maltreatment referrals. Child Abus. Negl. 2020, 104, 104477. [Google Scholar] [CrossRef] [PubMed]
- Nadan, Y.; Spilsbury, J.C.; Korbin, J.E. Culture and context in understanding child maltreatment: Contributions of intersectionality and neighborhood-based research. Child Abus. Negl. 2015, 41, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Gearing, R.E.; Mian, I.A.; Barber, J.; Ickowicz, A. A Methodology for Conducting Retrospective Chart Review Research in Child and Adolescent Psychiatry. J. Can. Acad. Child Adolesc. Psychiatry 2006, 15, 126–134. [Google Scholar] [PubMed]
- Durand, M.B.; McLaughlin, C.M.; Imagawa, K.K.; Upperman, J.S.; Jensen, A.R. Identifying Targets to Improve Coding of Child Physical Abuse at a Pediatric Trauma Center. J. Trauma Nurs. 2019, 26, 239–242. [Google Scholar] [CrossRef]
- Goldman, R.L. The Reliability of Peer Assessments of Quality of Care. JAMA 1992, 267, 958–960. [Google Scholar] [CrossRef]
- Mennen, F.E.; Kim, K.; Sang, J.; Trickett, P.K. Child neglect: Definition and identification of youth’s experiences in official reports of maltreatment. Child Abus. Negl. 2010, 34, 647–658. [Google Scholar] [CrossRef] [Green Version]
- Knutson, J.F.; DeGarmo, D.; Koeppl, G.; Reid, J.B. Care neglect, supervisory neglect, and harsh parenting in the development of children’s aggression: A replication and extension. Child Maltreat. 2005, 10, 92–107. [Google Scholar] [CrossRef] [Green Version]
- Welch, G.; Johnson, H.; Wilhelm, L. The Neglected Child: How to Recognize, Respond, and Prevent; Gryphon House, Incorporated: Lewisville, NC, USA, 2013; 128p. [Google Scholar]
- Department for Education. Working Together to Safeguard Children; Department for Education: Manchester, UK, 2018; Volume 111. [Google Scholar]
- Department for Communities and Local Government. The English Indices of Deprivation 2015. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/465791/English_Indices_of_Deprivation_2015_-_Statistical_Release.pdf (accessed on 24 March 2022).
- IMD Postcode Checker. Available online: https://www.fscbiodiversity.uk/imd/ (accessed on 5 April 2022).
- Gilard-Pioc, S.; Cottenet, J.; Mikaeloff, Y.; Gouyon, J.; Francois-Purssell, I.; Quantin, C. Eight-Year Period Prevalence of Physical Abuse in Hospitalised Infants and Corresponding In-hospital Mortality in France. Child Abus. Rev. 2019, 28, 353–365. [Google Scholar] [CrossRef]
- Lindberg, D.M.; Beaty, B.; Juarez-Colunga, E.; Wood, J.N.; Runyan, D.K. Testing for Abuse in Children With Sentinel Injuries. Pediatrics 2015, 136, 831–838. [Google Scholar] [CrossRef] [Green Version]
- Louwers, E.C.F.M.; Korfage, I.J.; Affourtit, M.J.; Scheewe, D.J.H.; van de Merwe, M.H.; Vooijs-Moulaert, F.A.F.S.R.; Woltering, C.M.C.; Jongejan, M.H.T.M.; Ruige, M.; Moll, H.A.; et al. Detection of child abuse in emergency departments: A multi-centre study. Arch. Dis. Child. 2011, 96, 422–425. [Google Scholar] [CrossRef]
- Stoltenborgh, M.; Bakermans-Kranenburg, M.J.; Alink, L.R.A.; van IJzendoorn, M.H. The Prevalence of Child Maltreatment across the Globe: Review of a Series of Meta-Analyses. Child Abus. Rev. 2015, 24, 37–50. [Google Scholar] [CrossRef]
- Jud, A.; Lips, U.; Landolt, M.A. Characteristics associated with maltreatment types in children referred to a hospital protection team. Eur. J. Pediatr. 2010, 169, 173–180. [Google Scholar] [CrossRef] [Green Version]
- Sahin, F.; Cepik-Kuruoğlu, A.; Demirel, B.; Akar, T.; Duyan-Camurdan, A.; Iseri, E.; Demiroğullari, B.; Pasli, F.; Beyazova, U.; Oral, R. Six-year experience of a hospital-based child protection team in Turkey. Turk J Pediatr. 2009, 51, 336–343. [Google Scholar]
- Stoddart, J.; Fallon, B.; Trocmé, N.; Fluke, J. Substantiated Child Maltreatment: Which factors do workers focus on when making this critical decision? Child. Youth Serv. Rev. 2018, 87, 1–8. [Google Scholar] [CrossRef]
- Kistin, C.J.; Tien, I.; Leventhal, J.M.; Bauchner, H. A Novel Self-Evaluation Tool to Assess the Team Function of a Child Protection Team. Acad. Pediatr. 2011, 11, 451–459. [Google Scholar] [CrossRef] [Green Version]
- Hussey, J.M.; Marshall, J.M.; English, D.J.; Knight, E.D.; Lau, A.S.; Dubowitz, H.; Kotch, J.B. Defining maltreatment according to substantiation: Distinction without a difference? Child Abus. Negl. 2005, 29, 479–492. [Google Scholar] [CrossRef] [PubMed]
- Featherstone, B.; Morris, K.; Susan, W. Re-Imagining Child Protection: Towards Humane Social Work with Families; Policy Press: Bristol, UK, 2014; 192p. [Google Scholar]
- Sidebotham, P.; Heron, J.; ALSPAC Study Team. Child maltreatment in the ‘children of the nineties’: A cohort study of risk factors. Child Abus. Negl. 2006, 30, 497–522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palusci, V.J.; Botash, A.S. Race and Bias in Child Maltreatment Diagnosis and Reporting. Pediatrics 2021, 148, e2020049625. [Google Scholar] [CrossRef] [PubMed]
- Maguire-Jack, K.; Lanier, P.; Johnson-Motoyama, M.; Welch, H.; Dineen, M. Geographic variation in racial disparities in child maltreatment: The influence of county poverty and population density. Child Abus. Negl. 2015, 47, 1–13. [Google Scholar] [CrossRef]
- Cheng, T.C.; Lo, C.C. Racial disparity in risk factors for substantiation of child maltreatment. Child. Youth Serv. Rev. 2013, 35, 1962–1969. [Google Scholar] [CrossRef]
- Ards, S.D.; Myers, S.L.; Malkis Erin, A.; Zhou, L. Racial disproportionality in reported and sustained child abuse and nelgect: An examination of systematic bias. Child. Youth Serv. Rev. 2003, 25, 375–392. [Google Scholar] [CrossRef]
- Dettlaff, A.J.; Rivaux, S.L.; Baumann, D.J.; Fluke, J.D.; Rycraft, J.R.; James, J. Disentangling substantiation: The influence of race, income, and risk on the substantiation decision in child welfare. Child. Youth Serv. Rev. 2011, 33, 1630–1637. [Google Scholar] [CrossRef]
- Cangiano, A. Mapping of Race and Poverty in Birmingham; University of Oxford: Oxford, UK, 2007; Volume 56. [Google Scholar]
- Garbarino, J.; Sherman, D. High-risk neighborhoods and high-risk families: The human ecology of child maltreatment. Child Dev. 1980, 51, 188–198. [Google Scholar] [CrossRef]
- Garbarino, J.; Kostelny, K. Child maltreatment as a community problem. Child Abus. Negl. 1992, 16, 455–464. [Google Scholar] [CrossRef]
- Sampson, R.J.; Raudenbush, S.W.; Earls, F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science 1997, 277, 918–924. [Google Scholar] [CrossRef]
- Coulton, C.J.; Crampton, D.S.; Irwin, M.; Spilsbury, J.C.; Korbin, J.E. How neighborhoods influence child maltreatment: A review of the literature and alternative pathways. Child Abus. Negl. 2007, 31, 1117–1142. [Google Scholar] [CrossRef]
- Cao, Y.; Maguire-Jack, K. Interactions with community members and institutions: Preventive pathways for child maltreatment. Child Abus. Negl. 2016, 62, 111–121. [Google Scholar] [CrossRef] [Green Version]
- Ahmadabadi, Z.; Najman, J.M.; Williams, G.M.; Clavarino, A.M.; d’Abbs, P.; Abajobir, A.A. Maternal intimate partner violence victimization and child maltreatment. Child Abus. Negl. 2018, 82, 23–33. [Google Scholar] [CrossRef]
- O’Donnell, M.; Maclean, M.J.; Sims, S.; Morgan, V.A.; Leonard, H.; Stanley, F.J. Maternal mental health and risk of child protection involvement: Mental health diagnoses associated with increased risk. J. Epidemiol. Community Health 2015, 69, 1175–1183. [Google Scholar] [CrossRef] [Green Version]
- Sprang, G.; Clark, J.J.; Bass, S. Factors that contribute to child maltreatment severity: A multi-method and multidimensional investigation. Child Abus. Negl. 2005, 29, 335–350. [Google Scholar] [CrossRef]
- Munro, E.; Taylor, J.S.; Bradbury-Jones, C. Understanding the Causal Pathways to Child Maltreatment: Implications for Health and Social Care Policy and Practice: Understanding the Causal Pathways to Child Maltreatment. Child Abus. Rev. 2014, 23, 61–74. [Google Scholar] [CrossRef]
- Berlin, L.J.; Appleyard, K.; Dodge, K.A. Intergenerational continuity in child maltreatment: Mediating mechanisms and implications for prevention. Child Dev. 2011, 82, 162–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dixon, L.; Hamilton-Giachritsis, C.; Browne, K. Attributions and behaviours of parents abused as children: A mediational analysis of the intergenerational continuity of child maltreatment [Part II]. J. Child Psychol. Psychiatry 2005, 46, 58–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Narang, D.S.; Contreras, J.M. The relationships of dissociation and affective family environment with the intergenerational cycle of child abuse. Child Abus. Negl. 2005, 29, 683–699. [Google Scholar] [CrossRef] [PubMed]
- Pears, K.C.; Capaldi, D.M. Intergenerational transmission of abuse: A two-generational prospective study of an at-risk sample. Child Abus. Negl. 2001, 25, 1439–1461. [Google Scholar] [CrossRef]
- Wathen, C.N.; MacMillan, H.L. Children’s exposure to intimate partner violence: Impacts and interventions. Paediatr. Child Health 2013, 18, 419–422. [Google Scholar] [PubMed]
- White, O.G.; Hindley, N.; Jones, D.P. Risk factors for child maltreatment recurrence: An updated systematic review. Med. Sci. Law 2015, 55, 259–277. [Google Scholar] [CrossRef]
- Bae, H.; Solomon, P.L.; Gelles, R.J. Multiple child maltreatment recurrence relative to single recurrence and no recurrence. Child.Youth Serv. Rev. 2009, 31, 617–624. [Google Scholar] [CrossRef]
- Jakeman, M.; Oxley, J.A.; Owczarczak-Garstecka, S.C.; Westgarth, C. Pet dog bites in children: Management and prevention. BMJ Paediatr. Open 2020, 4, e000726. [Google Scholar] [CrossRef]
- Parmeter, J.; Tzioumi, D.; Woolfenden, S. Medical neglect at a tertiary paediatric hospital. Child Abus. Negl. 2018, 77, 134–143. [Google Scholar] [CrossRef]
- Chester, D.L.; Jose, R.M.; Aldlyami, E.; King, H.; Moiemen, N.S. Non-accidental burns in children—Are we neglecting neglect? Burns 2006, 32, 222–228. [Google Scholar] [CrossRef]
- James-Ellison, M.; Barnes, P.; Maddocks, A.; Wareham, K.; Drew, P.; Dickson, W.; Lyons, R.A.; Hutchings, H.A. Social health outcomes following thermal injuries: A retrospective matched cohort study. Arch. Dis. Child. 2009, 94, 663–667. [Google Scholar] [CrossRef] [PubMed]
- Peh, C.X.; Shahwan, S.; Fauziana, R.; Mahesh, M.V.; Sambasivam, R.; Zhang, Y.; Ong, S.H.; Chong, S.A.; Subramaniam, M. Emotion dysregulation as a mechanism linking child maltreatment exposure and self-harm behaviors in adolescents. Child Abus. Negl. 2017, 67, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Featherstone, B.; Morris, K.; Daniel, B.; Bywaters, P.; Brady, G.; Bunting, L.; Mason, W.; Mirza, N. Poverty, inequality, child abuse and neglect: Changing the conversation across the UK in child protection? Child. Youth Serv. Rev. 2019, 97, 127–133. [Google Scholar] [CrossRef]
- Latham, R.M.; Meehan, A.J.; Arseneault, L.; Stahl, D.; Danese, A.; Fisher, H.L. Development of an individualized risk calculator for poor functioning in young people victimized during childhood: A longitudinal cohort study. Child Abus. Negl. 2019, 98, 104188. [Google Scholar] [CrossRef] [PubMed]
- Russell, J. Predictive analytics and child protection: Constraints and opportunities. Child Abus. Negl. 2015, 46, 182–189. [Google Scholar] [CrossRef]



| Ethnic Category | Substantiated Cases | Total No. of Cases | 2011 Census Birmingham | ||
|---|---|---|---|---|---|
| Yes | No | No. | % | % | |
| White | |||||
| 127 | 90 | 217 | 53.0 | 53 |
| 1 | 0 | 1 | 0.2 | 2 |
| 10 | 11 | 21 | 5.1 | 2.7 |
| Mixed or multiple ethnic groups | |||||
| 9 | 2 | 11 | 2.7 | 2.3 |
| 2 | 0 | 2 | 0.5 | 0.3 |
| 1 | 3 | 4 | 1.0 | 1.4 |
| 5 | 2 | 7 | 1.8 | 0.8 |
| Asian or Asian British | |||||
| 6 | 3 | 9 | 2.3 | 6.0 |
| 31 | 13 | 44 | 10.8 | 13.5 |
| 7 | 3 | 10 | 2.4 | 3.0 |
| 9 | 8 | 17 | 4.2 | 0.8 |
| Black and Black British | |||||
| 19 | 11 | 30 | 7.3 | 4.4 |
| 12 | 7 | 19 | 4.6 | 2.8 |
| 2 | 2 | 4 | 0.9 | 1.8 |
| Any other Ethnic Group | 7 | 6 | 13 | 3.2 | 1.0 |
| Total | 248 | 161 | 409 | 100 | 100 |
| Potential Predisposing Factor | Substantiated Cases | Total No. of Cases | p-Value | ||
|---|---|---|---|---|---|
| Yes | No | No. | % | ||
| Parent/carer ‘vulnerability’ | |||||
| 76 | 28 | 104 | 24 | 0.004 |
| 36 | 21 | 57 | 13 | n.s. |
| 41 | 22 | 63 | 14 | n.s. |
| Childhood disability or chronic illness | 44 | 35 | 79 | 17 | n.s. |
| Previous involvement with statutory body | 140 | 71 | 211 | 48 | 0.001 |
| Reason for Referral | Substantiated Cases | Total No. of Cases | ||
|---|---|---|---|---|
| Yes | No | No. | % | |
| Soft tissue injuries (e.g., bruises, lacerations, bites) | 44 | 23 | 67 | 14.8 |
| Burns | 58 | 35 | 93 | 20.5 |
| Skeletal fractures | 25 | 10 | 35 | 7.7 |
| Head injury | 26 | 18 | 44 | 9.7 |
| Other injuries (e.g., multiple trauma, falls from heights, stairway falls) | 13 | 18 | 31 | 6.8 |
| Self-harm | 21 | 14 | 35 | 7.8 |
| Accidental ingestion | 4 | 7 | 11 | 2.4 |
| Fabricated or induced illness | 4 | 4 | 8 | 1.8 |
| Primary Neglect | 50 | 6 | 56 | 12.4 |
| Primary Emotional abuse | 32 | 4 | 36 | 8.0 |
| Sexual abuse/exploitation | 11 | 5 | 16 | 3.5 |
| Other (e.g., BRUE, oronasal haemorrhage) | 6 | 14 | 20 | 4.5 |
| Total | 294 | 158 | 452 | 100 |
| Supervisory Neglect | Care Neglect | Medical Neglect | Emotional Abuse | Environmental Neglect | Total Neglect | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| S | NS | S | NS | S | NS | S | NS | S | NS | ||
| Dog bites | 5 | 8 | 1 | 14 | |||||||
| Burns (Total) | |||||||||||
| 14 | 5 | 1 | 1 | 21 | ||||||
| 3 | 1 | 2 | 1 | 7 | ||||||
| 11 | 4 | 15 | ||||||||
| 2 | 2 | |||||||||
| 6 | 3 | 1 | 10 | |||||||
| 4 | 4 | 8 | ||||||||
| Falls from windows | 3 | 5 | 8 | ||||||||
| Motor vehicle injury | 6 | 1 | 1 | 8 | |||||||
| Self-harm | 21 | 9 | 30 | ||||||||
| Ingestion | 4 | 4 | 1 | 9 | |||||||
| 58 | 35 | 0 | 0 | 3 | 1 | 21 | 10 | 2 | 2 | 132 | |
| Category of Abuse | Study | England & Wales (%) | |
|---|---|---|---|
| No. | % | ||
| Physical | 166 | 41.4 | 9.8 |
| Neglect | 157 | 39.1 | 41.9 |
| Emotional abuse (including witnessing domestic violence) | 67 | 16.7 | 32.8 |
| Sexual abuse | 11 | 2.7 | 4.5 |
| Multiple categories | Not known | 11.0 | |
| Total | 401 | 100 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Debelle, G.; Efstathiou, N.; Khan, R.; Williamson, A.; Summan, M.; Taylor, J. The Typology and Topography of Child Abuse and Neglect: The Experience of a Tertiary Children’s Centre. Int. J. Environ. Res. Public Health 2022, 19, 8213. https://doi.org/10.3390/ijerph19138213
Debelle G, Efstathiou N, Khan R, Williamson A, Summan M, Taylor J. The Typology and Topography of Child Abuse and Neglect: The Experience of a Tertiary Children’s Centre. International Journal of Environmental Research and Public Health. 2022; 19(13):8213. https://doi.org/10.3390/ijerph19138213
Chicago/Turabian StyleDebelle, Geoff, Nikolaos Efstathiou, Rafiyah Khan, Annette Williamson, Manjit Summan, and Julie Taylor. 2022. "The Typology and Topography of Child Abuse and Neglect: The Experience of a Tertiary Children’s Centre" International Journal of Environmental Research and Public Health 19, no. 13: 8213. https://doi.org/10.3390/ijerph19138213
APA StyleDebelle, G., Efstathiou, N., Khan, R., Williamson, A., Summan, M., & Taylor, J. (2022). The Typology and Topography of Child Abuse and Neglect: The Experience of a Tertiary Children’s Centre. International Journal of Environmental Research and Public Health, 19(13), 8213. https://doi.org/10.3390/ijerph19138213






