A Bibliometric Analysis of Leprosy during 2000–2021 from Web of Science Database
Abstract
:1. Introduction
2. Methods
2.1. Database Sources
2.2. Searching Strategy
2.3. Data Extraction and Statistical Analysis
3. Results
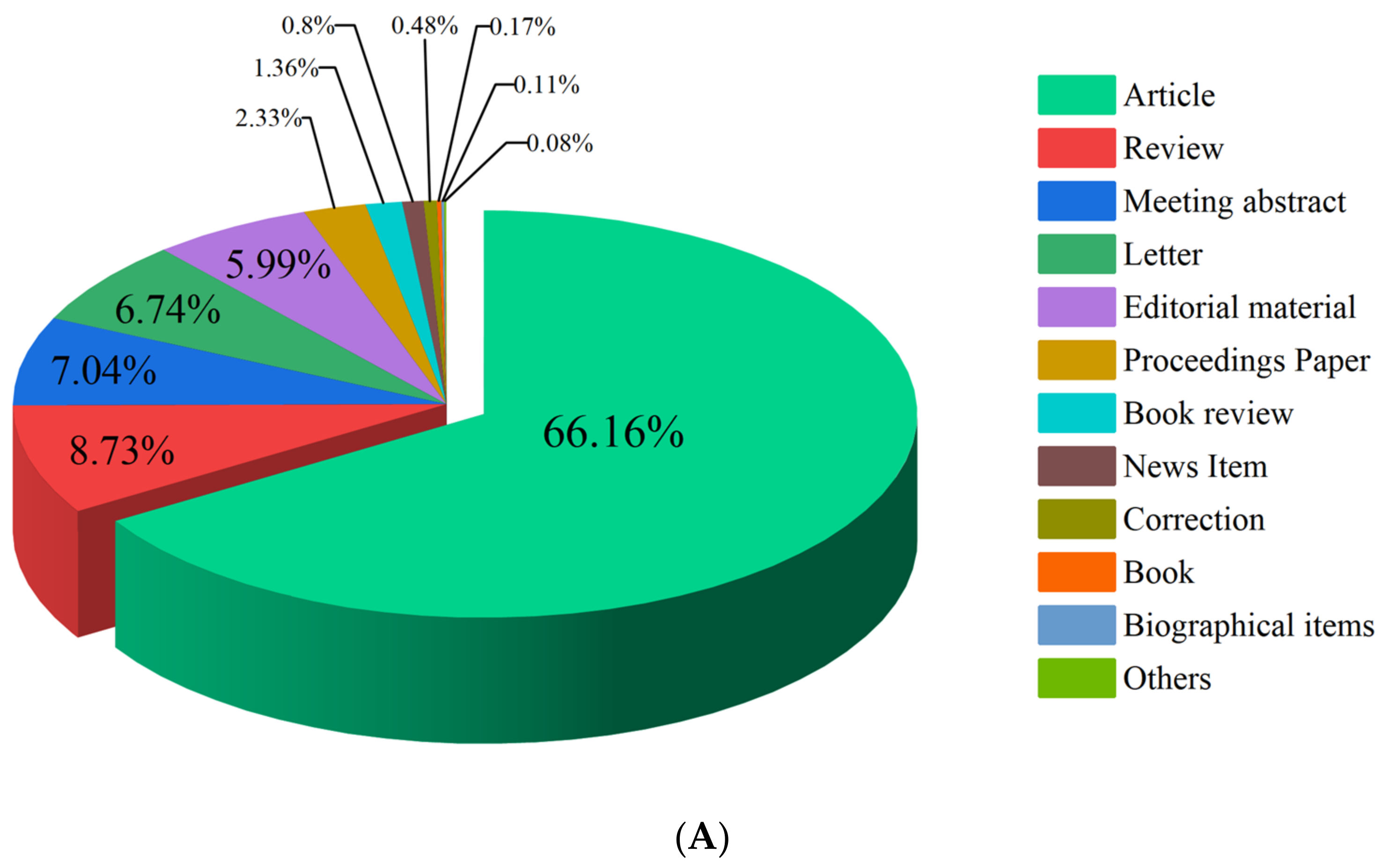
3.1. Types and Categories
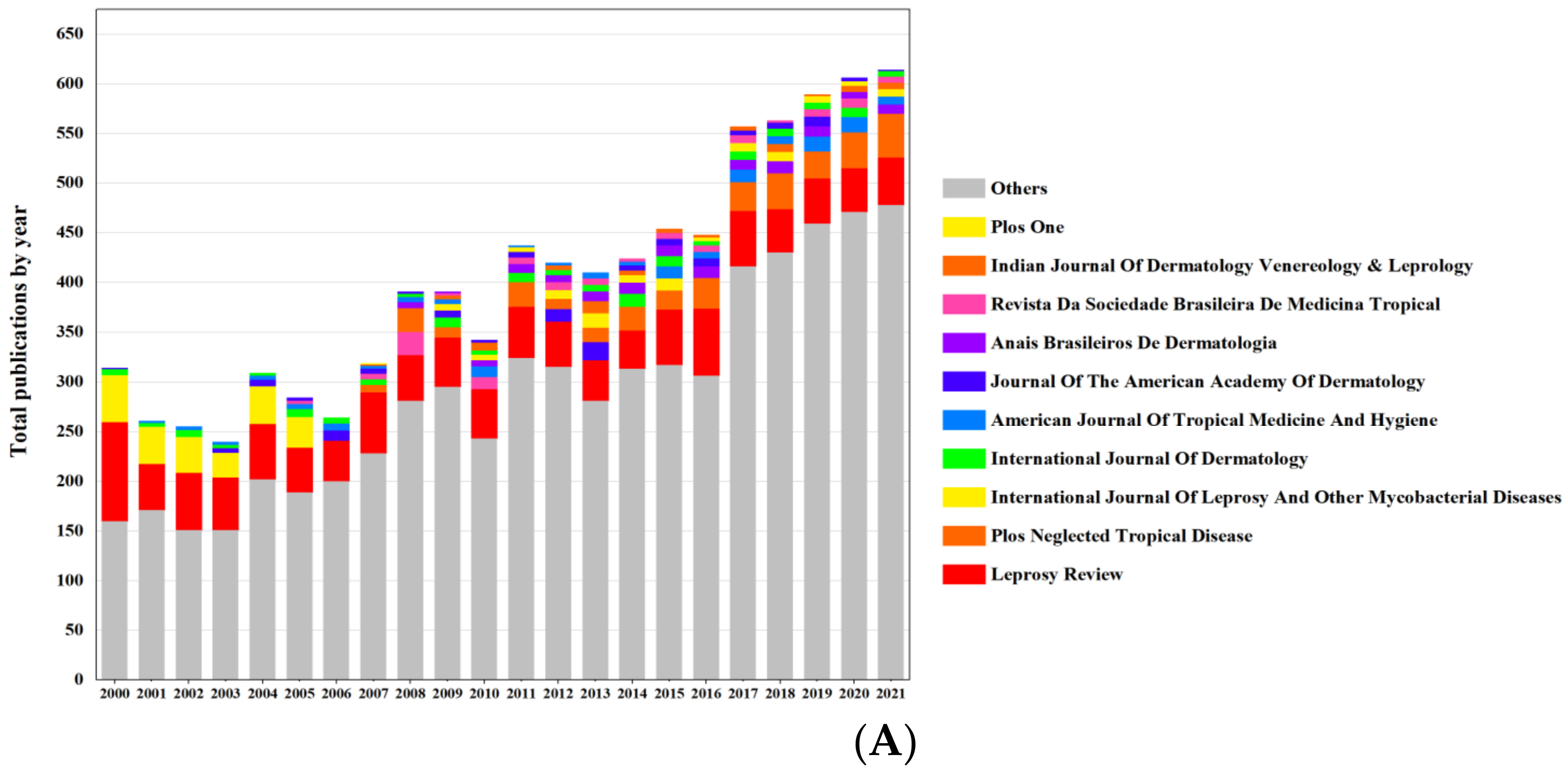
3.2. Publications Statistics
3.3. Author Analysis
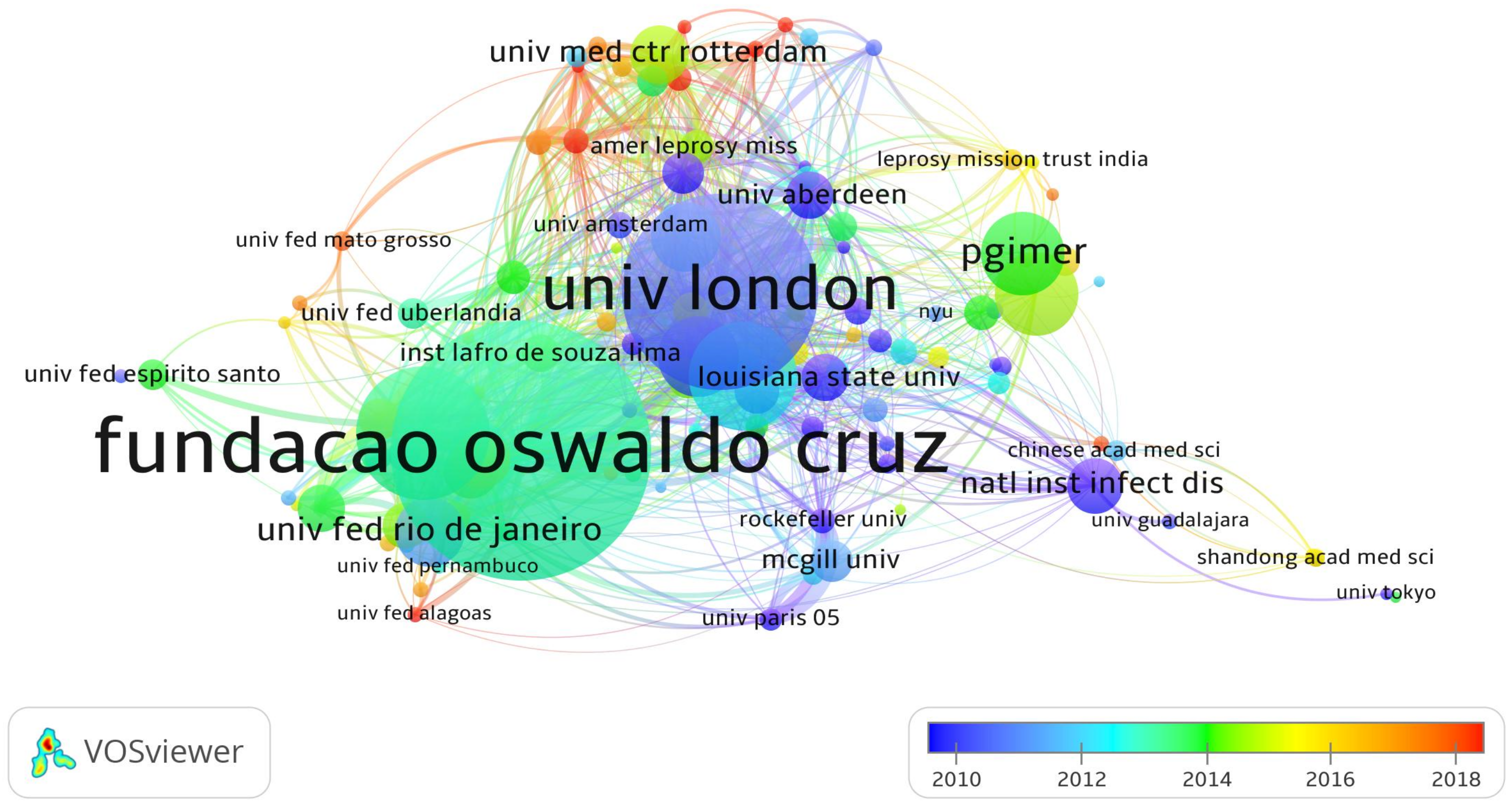
3.4. Institution Analysis
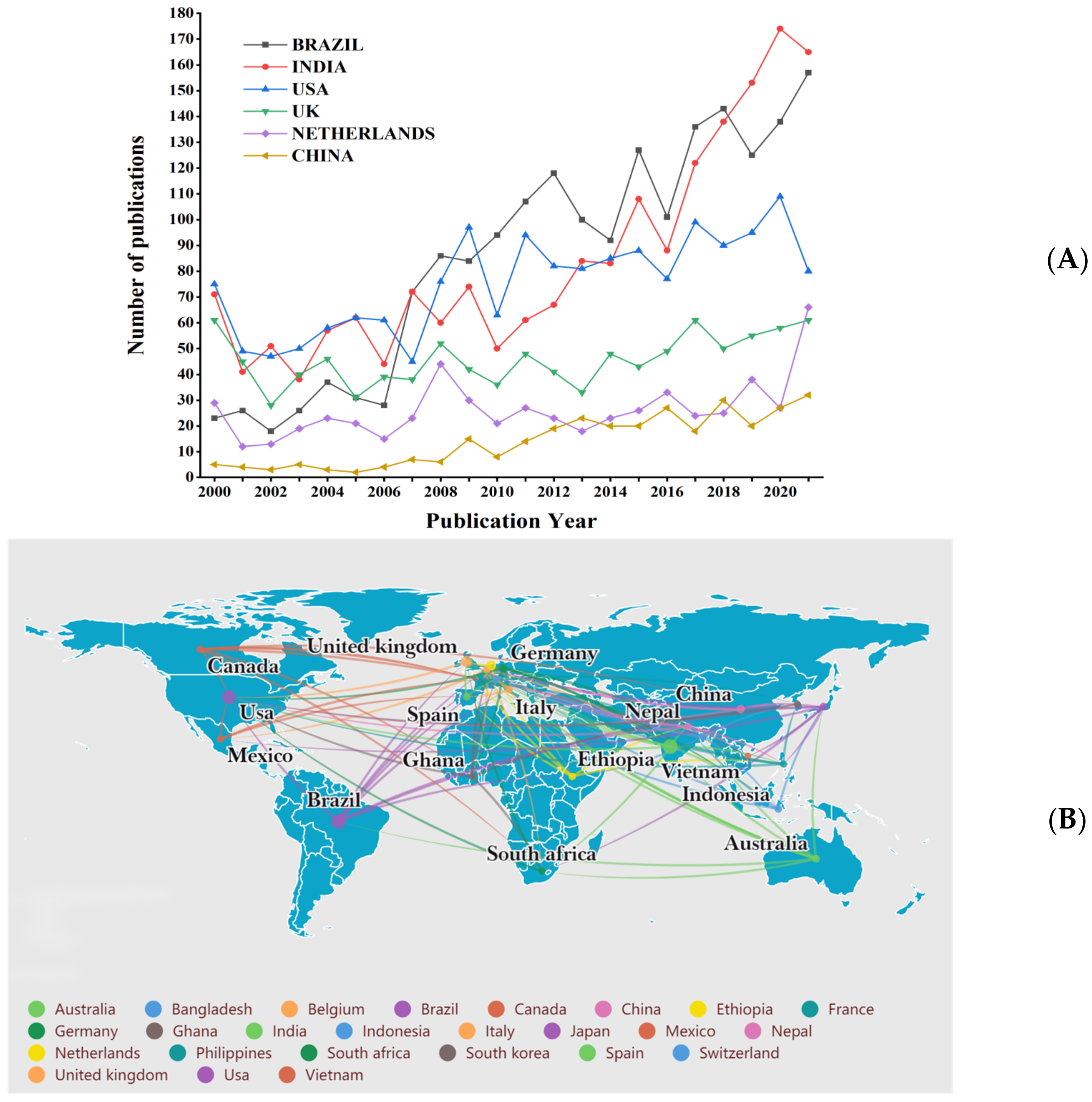
3.5. Country Analysis
3.6. Keyword Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- White, C.; Franco-Paredes, C. Leprosy in the 21st century. Clin. Microbiol. Rev. 2015, 28, 80–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horta-Baas, G.; Hernández-Cabrera, M.F.; Barile-Fabris, L.A.; Romero-Figueroa, M.; Del, S.; Arenas-Guzmán, R. Multibacillary leprosy mimicking systemic lupus erythematosus: Case report and literature review. Lupus 2015, 24, 1095–1102. [Google Scholar] [CrossRef]
- Chokkakula, S.; Chen, Z.; Wang, L.; Jiang, H.; Chen, Y.; Shi, Y.; Zhang, W.; Gao, W.; Yang, J.; Li, J.; et al. Molecular surveillance of antimicrobial resistance and transmission pattern of Mycobacterium leprae in Chinese leprosy patients. Emerg. Microbes Infect. 2019, 8, 1479–1489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonçalves, F.G.; Rosa, P.S.; de Farias Fernandes Belone, A.; Carneiro, L.B.; Queiroz de Barros, V.L.; Bispo, R.F.; Alves da Silva Sbardelott, Y.; Viana Macedo Neves, S.A.; Vittor, A.Y.; Woods, W.J.; et al. Multidrug Therapy for Leprosy Can Cure Patients with Lobomycosis in Acre State, Brazil: A Proof of Therapy Study. Am. J. Trop. Med. Hyg. 2020, 104, 634–639. [Google Scholar] [CrossRef] [PubMed]
- Pescarini, J.M.; Strina, A.; Nery, J.S.; Skalinski, L.M.; Andrade, K.V.F.D.; Penna, M.L.F.; Brickley, E.B.; Rodrigues, L.C.; Barreto, M.L.; Penna, G.O. Socioeconomic risk markers of leprosy in high-burden countries: A systematic review and meta-analysis. PLoS Negl. Trop. Dis. 2018, 12, e0006622. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarode, G.; Sarode, S.; Anand, R.; Patil, S.; Jafer, M.; Baeshen, H.; Awan, K.H. Epidemiological aspects of leprosy. Dis.-Mon. DM 2020, 66, 100899. [Google Scholar] [CrossRef] [PubMed]
- GHO. By Category. Leprosy-Number of New Leprosy Cases-Data by Country. Available online: https://apps.who.int/gho/data/node.main.A1639?lang=en (accessed on 11 April 2022).
- Maymone, M.B.C.; Venkatesh, S.; Laughter, M.; Abdat, R.; Hugh, J.; Dacso, M.M.; Rao, P.N.; Stryjewska, B.M.; Dunnick, C.A.; Dellavalle, R.P. Leprosy: Treatment and management of complications. J. Am. Acad. Dermatol. 2020, 83, 17–30. [Google Scholar] [CrossRef]
- Saxena, S.; Spaink, H.P.; Forn-Cuní, G. Drug Resistance in Nontuberculous Mycobacteria: Mechanisms and Models. Biology 2021, 10, 96. [Google Scholar] [CrossRef]
- Sottie, C.A.; Darkey, J. Living with stigma: Voices from the Cured Lepers’ village in Ghana. Soc. Work Health Care 2019, 58, 151–165. [Google Scholar] [CrossRef]
- Blakeman, K. Bibliometrics in a digital age: Help or hindrance. Sci. Prog. 2018, 101, 293–310. [Google Scholar] [CrossRef]
- Fassoulaki, A.; Vassi, A.; Kardasis, A.; Chantziara, V. Altmetrics versus traditional bibliometrics: Short-time lag and short-time life? Eur. J. Anaesthesiol. 2020, 37, 944–946. [Google Scholar] [CrossRef] [PubMed]
- Romanelli, J.P.; Gonçalves, M.C.P.; de Abreu Pestana, L.F.; Soares, J.A.H.; Boschi, R.S.; Andrade, D.F. Four challenges when conducting bibliometric reviews and how to deal with them. Environ. Sci. Pollut. Res. Int. 2021, 28, 60448–60458. [Google Scholar] [CrossRef] [PubMed]
- Trueger, N.S.; Yilmaz, Y.; Chan, T.M. Leveraging Tweets, Citations, and Social Networks to Improve Bibliometrics. JAMA Netw. Open 2020, 3, e2010911. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Zhang, J.; Ma, R. The Prediction of Infectious Diseases: A Bibliometric Analysis. Int. J. Environ. Res. Public Health 2020, 17, 6218. [Google Scholar] [CrossRef]
- Steinmann, P.; Dusenbury, C.; Addiss, D.; Mirza, F.; Smith, W.C.S. A comprehensive research agenda for zero leprosy. Infect. Dis. Poverty 2020, 9, 156. [Google Scholar] [CrossRef]
- Penna, M.L.; Penna, G.O. Leprosy frequency in the world, 1999-2010. Mem. Inst. Oswaldo Cruz. 2012, 107 (Suppl. 1), 3–12. [Google Scholar] [CrossRef] [Green Version]
- Barbui, C.; Cipriani, A.; Malvini, L.; Tansella, M. Validity of the impact factor of journals as a measure of randomized controlled trial quality. J. Clin. Psychiatry 2006, 67, 37–40. [Google Scholar] [CrossRef]
- Ramos-E-Silva, M.; Silveira Lima, T. Advances in tropical diseases. G. Ital. Dermatol. Venereol. 2011, 146, 353–371. Available online: https://pubmed.ncbi.nlm.nih.gov/21956272/ (accessed on 12 April 2022).
- Hanewinckel, R.; van Oijen, M.; Ikram, M.A.; van Doorn, P.A. The epidemiology and risk factors of chronic polyneuropathy. Eur. J. Epidemiol. 2016, 31, 5–20. [Google Scholar] [CrossRef] [Green Version]
- Cai, Z.; Chang, Q.; Yip, P.S.F. A scientometric analysis of suicide research: 1990-2018. J. Affect. Disord. 2020, 266, 356–365. [Google Scholar] [CrossRef]
- Chen, S.; Lu, Q.; Bai, J.; Deng, C.; Wang, Y.; Zhao, Y. Global publications on stigma between 1998–2018: A bibliometric analysis. J. Affect. Disord. 2020, 274, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Yuan, T.; Zhang, Z.; Yang, Q.; Chen, M.; Wang, Q.; Deng, H.; Qiu, H.; Wang, X.; Huang, X. The top 100 most impactful articles and recent trends in nasopharyngeal carcinoma from 1970 to 2018: A bibliometric analysis. J. Int. Med. Res. 2020, 48, 300060519896149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monot, M.; Honoré, N.; Garnier, T.; Araoz, R.; Coppée, J.-Y.; Lacroix, C.; Sow, S.; Spencer, J.S.; Truman, R.W.; Williams, D.L.; et al. On the origin of leprosy. Science 2005, 308, 1040–1042. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, G.W.; Xu, C.; Chen, K.; Huang, H.Q.; Chen, J.; Song, B.; Chan, J.K.C.; Li, W.; Liu, W.; Shih, L.Y.; et al. Genetic risk of extranodal natural killer T-cell lymphoma: A genome-wide association study in multiple populations. Lancet Oncol. 2020, 21, 306–316. [Google Scholar] [CrossRef]
- You, J.; Sun, L.; Zhao, Q.; Zhang, H.; Huai, P.; Yu, G.; Wang, Z.; Mi, Z.; Pang, Z.; Liu, H.; et al. Dynamic cytokine profiles combined with enzyme-linked immunospot assay are useful for immunologically confirming the dapsone hypersensitivity syndrome. J. Am. Acad. Dermatol. 2021, 84, 814–816. [Google Scholar] [CrossRef]
- Chen, X.; Zha, S.; Shui, T.-J. Presenting symptoms of leprosy at diagnosis: Clinical evidence from a cross-sectional, population-based study. PLoS Negl. Trop. Dis. 2021, 15, e0009913. [Google Scholar] [CrossRef]
- Moraes, M.O.; Düppre, N.C. Leprosy post-exposure prophylaxis: Innovation and precision public health. Lancet Glob. Health 2021, 9, e8–e9. [Google Scholar] [CrossRef]
- The Lancet. Abandoning the stigma of leprosy. Lancet 2019, 393, 378. [Google Scholar] [CrossRef] [Green Version]
- Nyblade, L.; Stockton, M.A.; Giger, K.; Bond, V.; Ekstrand, M.L.; Lean, R.M.; Mitchell, E.M.H.; Nelson, L.R.E.; Sapag, J.C.; Siraprapasiri, T.; et al. Stigma in health facilities: Why it matters and how we can change it. BMC Med. 2019, 17, 25. [Google Scholar] [CrossRef]
- Wu, L.; Shen, Y.; Yao, Q.; Sang, X.; Fei, L.; Kong, W.; Huang, Y.; Wang, Y.; Zeng, F.; Du, N. Temporal-spatial distribution characteristics of leprosy: A new challenge for leprosy prevention and control in Zhejiang, China. PLoS Negl. Trop. Dis. 2021, 15, e0008956. [Google Scholar] [CrossRef]
- Machado, L.M.G.; Dos Santos, E.S.; Cavaliero, A.; Steinmann, P.; Ignotti, E. Spatio-temporal analysis of leprosy risks in a municipality in the state of Mato Grosso-Brazilian Amazon: Results from the leprosy post-exposure prophylaxis program in Brazil. Infect. Dis. Poverty 2022, 11, 21. [Google Scholar] [CrossRef] [PubMed]
- Joshua, V. Spatial and temporal trends in new case detection of leprosy in India. Lepr. Rev. 2016, 87, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Modlin, R.L. The innate immune response in leprosy. Curr. Opin. Immunol. 2010, 22, 48–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davies, L.C.; Taylor, P.R. Tissue-resident macrophages: Then and now. Immunology 2015, 144, 41–48. [Google Scholar] [CrossRef] [Green Version]
- Ma, F.; Hughes, T.K.; Teles, R.M.B.; Andrade, P.R.; de Andrade Silva, B.J.; Plazyo, O.; Tsoi, L.C.; Do, T.; Wadsworth, M.H., II; Oulee, A.; et al. The cellular architecture of the antimicrobial response network in human leprosy granulomas. Nat. Immunol. 2021, 22, 839–850. [Google Scholar] [CrossRef]
- Chen, X.; He, J.; Liu, J.; You, Y.; Yuan, L.; Wen, Y. Nested PCR and the TaqMan SNP Genotyping Assay enhanced the sensitivity of drug resistance testing of Mycobacterium leprae using clinical specimens of leprosy patients. PLoS Negl. Trop. Dis. 2019, 13, e0007946. [Google Scholar] [CrossRef]
- Liu, D.; Zhang, Q.; Sun, Y.; Wang, C.; Zhang, Y.; Fu, X.; Chen, M.; Zhou, G.; Yu, X.; Wang, J.; et al. Drug resistance in Mycobacterium leprae from patients with leprosy in China. Clin. Exp. Dermatol. 2015, 40, 908–911. [Google Scholar] [CrossRef]
- Sharma, M.; Singh, P. Repurposing Drugs to Combat Drug Resistance in Leprosy: A Review of Opportunities. Comb. Chem. High Throughput Screen. 2021. epub ahead of print. [Google Scholar] [CrossRef]
- Benjak, A.; Avanzi, C.; Singh, P.; Loiseau, C.; Girma, S.; Busso, P.; Fontes, A.N.B.; Miyamoto, Y.; Namisato, M.; Bobosha, K.; et al. Phylogenomics and antimicrobial resistance of the leprosy bacillus Mycobacterium leprae. Nat. Commun. 2018, 9, 352. [Google Scholar] [CrossRef]
- Tawfik, G.M.; Biala, M.; Yousef, Y.M.; Tiwari, R.; Dobs, M.; Lotfy, C.I.; Farrag, D.A.; Hue, A.T.; Yotsu, R.R.; Huy, N.T. Efficacy of chemoprophylaxis and immunoprophylaxis in leprosy prevention: A systematic review and network meta-analysis of randomized controlled trials. Clin. Microbiol. Infect. 2021, 27, 1754–1761. [Google Scholar] [CrossRef]
- van Hooij, A.; van den Eeden, S.J.F.; Khatun, M.; Soren, S.; Franken, K.L.M.C.; Chandra Roy, J.; Alam, K.; Chowdhury, A.S.; Richardus, J.H.; Geluk, A. BCG-induced immunity profiles in household contacts of leprosy patients differentiate between protection and disease. Vaccine 2021, 39, 7230–7237. [Google Scholar] [CrossRef] [PubMed]
- Coppola, M.; van den Eeden, S.J.F.; Robbins, N.; Wilson, L.; Franken, K.L.M.C.; Adams, L.B.; Gillis, T.P.; Ottenhoff, T.H.M.; Geluk, A. Vaccines for Leprosy and Tuberculosis: Opportunities for Shared Research, Development, and Application. Front. Immunol. 2018, 9, 308. [Google Scholar] [CrossRef] [PubMed]
- Waman, V.P.; Vedithi, S.C.; Thomas, S.E.; Bannerman, B.P.; Munir, A.; Skwark, M.J.; Malhotra, S.; Blundell, T.L. Mycobacterial genomics and structural bioinformatics: Opportunities and challenges in drug discovery. Emerg. Microbes Infect. 2019, 8, 109–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sauer, M.E.; Salomão, H.; Ramos, G.B.; D’Espindula, H.R.; Rodrigues, R.S.; Macedo, W.C.; Sindeaux, R.H.; Mira, M.T. Genetics of leprosy: Expected and unexpected developments and perspectives. Clin. Dermatol. 2015, 33, 99–107. [Google Scholar] [CrossRef] [PubMed]
- De Souza, M.L.M.; Lopes, G.A.; Branco, A.C.; Fairley, J.K.; Fraga, L.A.O. Leprosy Screening Based on Artificial Intelligence: Development of a Cross-Platform App. JMIR Mhealth Uhealth 2021, 9, e23718. [Google Scholar] [CrossRef] [PubMed]





| Journal | Publications | Percentage (%) | IF | AC |
|---|---|---|---|---|
| Leprosy Review | 1148 | 12.91 | 0.54 | 8.12 |
| Plos Neglected Tropical Disease | 309 | 3.48 | 4.41 | 20.36 |
| International Journal of Leprosy and Other Mycobacterial Diseases | 214 | 2.41 | 0.22 | 9.95 |
| International Journal of Dermatology | 155 | 1.74 | 2.74 | 8.61 |
| American Journal of Tropical Medicine and Hygiene | 141 | 1.59 | 2.35 | 10.25 |
| Journal of the American Academy of Dermatology | 122 | 1.37 | 11.53 | 4.64 |
| Anais Brasileiros De Dermatologia | 119 | 1.34 | 1.90 | 7.22 |
| Revista Da Sociedade Brasileira De Medicina Tropical | 112 | 1.26 | 1.58 | 7.85 |
| Indian Journal of Dermatology Venereology & Leprology | 97 | 1.09 | 2.55 | 7.72 |
| Plos One | 94 | 1.06 | 3.24 | 15.85 |
| Author | Publication | Percentage | H-Index | Citation |
|---|---|---|---|---|
| Sarno EN | 199 | 2.24% | 35 | 5059 |
| Richardus JH | 153 | 1.72% | 33 | 2905 |
| Lockwood DNJ | 115 | 1.29% | 32 | 3606 |
| Dogra S | 96 | 1.08% | 12 | 547 |
| Moraes MO | 90 | 1.01% | 28 | 2149 |
| Van Brakel WH | 84 | 0.94% | 26 | 1921 |
| Geluk A | 79 | 0.89% | 25 | 1805 |
| Brennan PJ | 77 | 0.87% | 31 | 2908 |
| Pessolani MCV | 73 | 0.82% | 23 | 1393 |
| Modlin RL | 70 | 0.79% | 27 | 3427 |
| Hong Liu * (32nd) | 47 | 0.53% | 13 | 1285 |
| Furen Zhang * (45th) | 39 | 0.44% | 13 | 1231 |
| Institutions | Country | Publication/% | H-Index/Rank |
|---|---|---|---|
| Fundacao Oswaldo Cruz | Brazil | 480 (5.40) | 45/(2) |
| University Of London | UK | 425 (4.78) | 56/(1) |
| Universidade De Sao Paulo | Brazil | 249 (2.80) | 23/(9) |
| Indian Council of Medical Research Icmr | India | 202 (2.27) | 26/(7) |
| University Of California System | USA | 196 (2.20) | 38/(3) |
| Erasmus University Rotterdam | Netherlands | 187 (2.10) | 34/(6) |
| CoLorado State University | USA | 153 (1.72) | 37/(4) |
| Leiden University | Netherlands | 134 (1.51) | 36/(5) |
| Post Graduate Institute of Medical Education Research Pgimer Chandigarh129(PGIMER) | India | 129 (1.45) | 15/(10) |
| Universidade Federal do Rio de Janeiro | Brazil | 127 (1.43) | 24/(8) |
| China | Netherlands | UK | USA | India | Brazil | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Keywords | N | Keywords | N | Keywords | N | Keywords | N | Keywords | N | Keywords |
| 93 | leprosy | 72 | leprosy | 138 | leprosy | 183 | mycobacterium leprae | 117 | leprosy | 179 | mycobacterium leprae |
| 35 | mycobacterium leprae | 68 | mycobacterium leprae | 102 | mycobacterium leprae | 151 | leprosy | 84 | mycobacterium leprae | 144 | disease |
| 22 | association | 48 | contact | 83 | tuberculosis | 58 | tuberculosis | 33 | lepromatous leprosy | 66 | diagnosis |
| 21 | identification | 41 | diagnosis | 60 | infection | 57 | diagnosis | 33 | disease | 55 | infection |
| 21 | diagnosis | 35 | risk factor | 43 | disease | 53 | infection | 32 | diagnosis | 51 | risk factor |
| 20 | susceptibility | 33 | tuberculosis | 32 | identification | 52 | disease | 22 | tuberculosis | 47 | lepromatous leprosy |
| 19 | disease | 29 | infection | 31 | mycobacterium tuberculosis | 40 | identification | 21 | expression | 48 | leprosy |
| 18 | tuberculosis | 28 | disease | 28 | diagnosis | 35 | contact | 20 | erythema nodosum leprosum | 43 | susceptibility |
| 16 | gene | 27 | Bangladesh | 26 | risk factor | 32 | lepromatous leprosy | 19 | multidrug therapy | 42 | association |
| 14 | variants | 25 | chemoprophylaxi | 23 | lepromatous leprosy | 31 | antigen | 18 | childhood leprosy | 41 | expression |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, X.; Yang, J.; Zhang, L.; Jin, G.; Xu, L.; Fang, F.; Li, Y.; Wei, P. A Bibliometric Analysis of Leprosy during 2000–2021 from Web of Science Database. Int. J. Environ. Res. Public Health 2022, 19, 8234. https://doi.org/10.3390/ijerph19148234
Li X, Yang J, Zhang L, Jin G, Xu L, Fang F, Li Y, Wei P. A Bibliometric Analysis of Leprosy during 2000–2021 from Web of Science Database. International Journal of Environmental Research and Public Health. 2022; 19(14):8234. https://doi.org/10.3390/ijerph19148234
Chicago/Turabian StyleLi, Xiang, Jing Yang, Lianhua Zhang, Guangjie Jin, Li Xu, Fujin Fang, Yunhui Li, and Pingmin Wei. 2022. "A Bibliometric Analysis of Leprosy during 2000–2021 from Web of Science Database" International Journal of Environmental Research and Public Health 19, no. 14: 8234. https://doi.org/10.3390/ijerph19148234
APA StyleLi, X., Yang, J., Zhang, L., Jin, G., Xu, L., Fang, F., Li, Y., & Wei, P. (2022). A Bibliometric Analysis of Leprosy during 2000–2021 from Web of Science Database. International Journal of Environmental Research and Public Health, 19(14), 8234. https://doi.org/10.3390/ijerph19148234






