The Influence of Artificial Light at Night on Asthma and Allergy, Mental Health, and Cancer Outcomes: A Systematic Scoping Review Protocol
Abstract
:1. Introduction
2. Rationale
2.1. Allergic Conditions including Asthma
2.2. Mental Health
2.3. Cancer
3. Objectives
4. Methods and Analysis
4.1. Study Design
4.2. Eligibility Criteria
4.3. Information Sources
4.4. Search Strategy
4.5. Study Records
4.6. Data Items
4.7. Outcomes and Prioritisation
4.8. Risk of Bias in Individual Studies
4.9. Data Synthesis
4.10. Meta-Bias(es)
4.11. Confidence in Cumulative Evidence
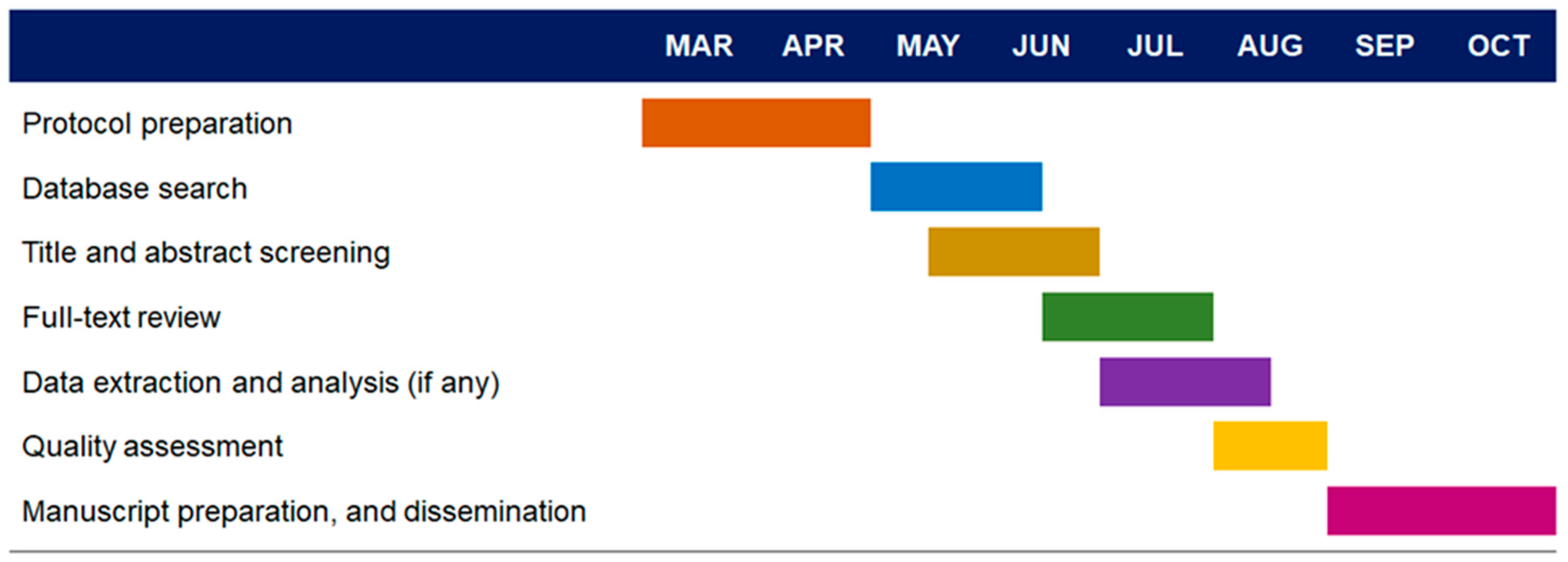
5. Study Timeline
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Munch, M.; Bromundt, V. Light and chronobiology: Implications for health and disease. Dialogues Clin. Neurosci. 2012, 14, 448–453. [Google Scholar] [CrossRef] [PubMed]
- Czeisler, C.A.; Shanahan, T.L.; Klerman, E.B.; Martens, H.; Brotman, D.J.; Emens, J.S.; Klein, T.; Rizzo, J.F., 3rd. Suppression of melatonin secretion in some blind patients by exposure to bright light. N. Engl. J. Med. 1995, 332, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Gaston, K.J.; Visser, M.E.; Holker, F. The biological impacts of artificial light at night: The research challenge. Philos. Trans. R. Soc. B Biol. Sci. 2015, 370, 20140133. [Google Scholar] [CrossRef] [Green Version]
- Haim, A.; Zubidat, A.E. Artificial light at night: Melatonin as a mediator between the environment and epigenome. Philos. Trans. R. Soc. B Biol. Sci. 2015, 370, 20140121. [Google Scholar] [CrossRef] [Green Version]
- Shier, D.M.; Bird, A.K.; Wang, T.B. Effects of artificial light at night on the foraging behavior of an endangered nocturnal mammal. Environ. Pollut. 2020, 263 Pt A, 114566. [Google Scholar] [CrossRef]
- Parkinson, E.; Lawson, J.; Tiegs, S.D. Artificial light at night at the terrestrial-aquatic interface: Effects on predators and fluxes of insect prey. PLoS ONE 2020, 15, e0240138. [Google Scholar] [CrossRef]
- Moaraf, S.; Heiblum, R.; Okuliarova, M.; Hefetz, A.; Scharf, I.; Zeman, M.; Barnea, A. Evidence That Artificial Light at Night Induces Structure-Specific Changes in Brain Plasticity in a Diurnal Bird. Biomolecules 2021, 11, 1069. [Google Scholar] [CrossRef]
- Kosicki, J.Z. The impact of artificial light at night on taxonomic, functional and phylogenetic bird species communities in a large geographical range: A modelling approach. Sci. Total Environ. 2021, 780, 146434. [Google Scholar] [CrossRef]
- Knop, E.; Zoller, L.; Ryser, R.; Gerpe, C.; Horler, M.; Fontaine, C. Artificial light at night as a new threat to pollination. Nature 2017, 548, 206–209. [Google Scholar] [CrossRef]
- Grubisic, M.; van Grunsven, R.H. Artificial light at night disrupts species interactions and changes insect communities. Curr. Opin. Insect Sci. 2021, 47, 136–141. [Google Scholar] [CrossRef]
- Giavi, S.; Fontaine, C.; Knop, E. Impact of artificial light at night on diurnal plant-pollinator interactions. Nat. Commun. 2021, 12, 1690. [Google Scholar] [CrossRef]
- Giavi, S.; Blosch, S.; Schuster, G.; Knop, E. Artificial light at night can modify ecosystem functioning beyond the lit area. Sci. Rep. 2020, 10, 11870. [Google Scholar] [CrossRef] [PubMed]
- Lunn, R.M.; Blask, D.E.; Coogan, A.N.; Figueiro, M.G.; Gorman, M.R.; Hall, J.E.; Hansen, J.; Nelson, R.J.; Panda, S.; Smolensky, M.H.; et al. Health consequences of electric lighting practices in the modern world: A report on the National Toxicology Program’s workshop on shift work at night, artificial light at night, and circadian disruption. Sci. Total Environ. 2017, 607–608, 1073–1084. [Google Scholar] [CrossRef] [Green Version]
- Allada, R.; Bass, J. Circadian Mechanisms in Medicine. N. Engl. J. Med. 2021, 384, 550–561. [Google Scholar] [CrossRef]
- Ralph, M.R.; Foster, R.G.; Davis, F.C.; Menaker, M. Transplanted suprachiasmatic nucleus determines circadian period. Science 1990, 247, 975–978. [Google Scholar] [CrossRef] [Green Version]
- Albrecht, U. Timing to perfection: The biology of central and peripheral circadian clocks. Neuron 2012, 74, 246–260. [Google Scholar] [CrossRef] [Green Version]
- Fernandez, D.C.; Fogerson, P.M.; Lazzerini Ospri, L.; Thomsen, M.B.; Layne, R.M.; Severin, D.; Zhan, J.; Singer, J.H.; Kirkwood, A.; Zhao, H.; et al. Light Affects Mood and Learning through Distinct Retina-Brain Pathways. Cell 2018, 175, 71–84.e18. [Google Scholar] [CrossRef] [Green Version]
- Touitou, Y.; Reinberg, A.; Touitou, D. Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: Health impacts and mechanisms of circadian disruption. Life Sci. 2017, 173, 94–106. [Google Scholar] [CrossRef]
- Reiter, R.J.; Tan, D.X.; Korkmaz, A.; Erren, T.C.; Piekarski, C.; Tamura, H.; Manchester, L.C. Light at night, chronodisruption, melatonin suppression, and cancer risk: A review. Crit. Rev. Oncog. 2007, 13, 303–328. [Google Scholar] [CrossRef]
- Cho, Y.; Ryu, S.H.; Lee, B.R.; Kim, K.H.; Lee, E.; Choi, J. Effects of artificial light at night on human health: A literature review of observational and experimental studies applied to exposure assessment. Chronobiol. Int. 2015, 32, 1294–1310. [Google Scholar] [CrossRef]
- Walker, W.H., 2nd; Bumgarner, J.R.; Becker-Krail, D.D.; May, L.E.; Liu, J.A.; Nelson, R.J. Light at night disrupts biological clocks, calendars, and immune function. Semin. Immunopathol. 2022, 44, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Blask, D.E. Melatonin, sleep disturbance and cancer risk. Sleep Med. Rev. 2009, 13, 257–264. [Google Scholar] [CrossRef]
- Auger, R.R.; Burgess, H.J.; Dierkhising, R.A.; Sharma, R.G.; Slocumb, N.L. Light Exposure Among Adolescents with Delayed Sleep Phase Disorder: A Prospective Cohort Study. Chronobiol. Int. 2011, 28, 911–920. [Google Scholar] [CrossRef] [PubMed]
- Paksarian, D.; Rudolph, K.E.; Stapp, E.K.; Dunster, G.P.; He, J.; Mennitt, D.; Hattar, S.; Casey, J.A.; James, P.; Merikangas, K.R. Association of Outdoor Artificial Light at Night with Mental Disorders and Sleep Patterns Among US Adolescents. JAMA Psychiatry 2020, 77, 1266–1275. [Google Scholar] [CrossRef] [PubMed]
- Dierick, B.J.H.; van der Molen, T.; Flokstra-de Blok, B.M.J.; Muraro, A.; Postma, M.J.; Kocks, J.W.H.; van Boven, J.F.M. Burden and socioeconomics of asthma, allergic rhinitis, atopic dermatitis and food allergy. Expert Rev. Pharmacoecon. Outcomes Res. 2020, 20, 437–453. [Google Scholar] [CrossRef] [PubMed]
- Soriano, J.B.; Kendrick, P.J.; Paulson, K.R.; Gupta, V.; Abrams, E.M.; Adedoyin, R.A.; Adhikari, T.B.; Advani, S.M.; Agrawal, A.; Ahmadian, E.; et al. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir. Med. 2020, 8, 585–596. [Google Scholar] [CrossRef]
- Turner-Warwick, M. Nocturnal asthma: A study in general practice. J. R. Coll. Gen. Pract. 1989, 39, 239–243. [Google Scholar]
- Sutherland, E.R. Nocturnal asthma. J. Allergy Clin. Immunol. 2005, 116, 1179–1186, quiz 1187. [Google Scholar] [CrossRef]
- Durrington, H.J.; Gioan-Tavernier, G.O.; Maidstone, R.J.; Krakowiak, K.; Loudon, A.S.I.; Blaikley, J.F.; Fowler, S.J.; Singh, D.; Simpson, A.; Ray, D.W. Time of Day Affects Eosinophil Biomarkers in Asthma: Implications for Diagnosis and Treatment. Am. J. Respir. Crit. Care Med. 2018, 198, 1578–1581. [Google Scholar] [CrossRef]
- Spengler, C.M.; Shea, S.A. Endogenous circadian rhythm of pulmonary function in healthy humans. Am. J. Respir. Crit. Care Med. 2000, 162, 1038–1046. [Google Scholar] [CrossRef]
- Haldar, P.; Carsin, A.E.; Debnath, S.; Maity, S.G.; Annesi-Maesano, I.; Garcia-Aymerich, J.; Bandyopadhayay, A.; Moitra, S.; Kogevinas, M.; Moitra, S. Individual circadian preference (chronotype) is associated with asthma and allergic symptoms among adolescents. ERJ Open Res. 2020, 6, 00226–02020. [Google Scholar] [CrossRef] [PubMed]
- Maidstone, R.J.; Turner, J.; Vetter, C.; Dashti, H.S.; Saxena, R.; Scheer, F.; Shea, S.A.; Kyle, S.D.; Lawlor, D.A.; Loudon, A.S.I.; et al. Night shift work is associated with an increased risk of asthma. Thorax 2021, 76, 53–60. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar] [CrossRef]
- Musiek, E.S.; Holtzman, D.M. Mechanisms linking circadian clocks, sleep, and neurodegeneration. Science 2016, 354, 1004–1008. [Google Scholar] [CrossRef] [Green Version]
- Leng, Y.; Musiek, E.S.; Hu, K.; Cappuccio, F.P.; Yaffe, K. Association between circadian rhythms and neurodegenerative diseases. Lancet Neurol. 2019, 18, 307–318. [Google Scholar] [CrossRef]
- Ehlers, C.L.; Frank, E.; Kupfer, D.J. Social zeitgebers and biological rhythms. A unified approach to understanding the etiology of depression. Arch. Gen. Psychiatry 1988, 45, 948–952. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, U. Molecular Connections Between Circadian Clocks and Mood-related Behaviors. J. Mol. Biol. 2020, 432, 3714–3721. [Google Scholar] [CrossRef]
- Yates, N.J. Schizophrenia: The role of sleep and circadian rhythms in regulating dopamine and psychosis. Rev. Neurosci. 2016, 27, 669–687. [Google Scholar] [CrossRef]
- Serrano-Serrano, A.B.; Marquez-Arrico, J.E.; Navarro, J.F.; Martinez-Nicolas, A.; Adan, A. Circadian Characteristics in Patients under Treatment for Substance Use Disorders and Severe Mental Illness (Schizophrenia, Major Depression and Bipolar Disorder). J. Clin. Med. 2021, 10, 4388. [Google Scholar] [CrossRef]
- Hashemzadeh, I.; Marquez-Arrico, J.E.; Hashemzadeh, K.; Navarro, J.F.; Adan, A. Circadian Functioning and Quality of Life in Substance Use Disorder Patients with and Without Comorbid Major Depressive Disorder. Front. Psychiatry 2021, 12, 750500. [Google Scholar] [CrossRef]
- Mersch, P.P.; Middendorp, H.M.; Bouhuys, A.L.; Beersma, D.G.; van den Hoofdakker, R.H. Seasonal affective disorder and latitude: A review of the literature. J. Affect. Disord. 1999, 53, 35–48. [Google Scholar] [CrossRef] [Green Version]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease 2019 Cancer Collaboration; Kocarnik, J.M.; Compton, K.; Dean, F.E.; Fu, W.; Gaw, B.L.; Harvey, J.D.; Henrikson, H.J.; Lu, D.; Pennini, A.; et al. Cancer Incidence, Mortality, Years of Life Lost, Years Lived with Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 2021, 8, 420–444. [Google Scholar]
- Sulli, G.; Lam, M.T.Y.; Panda, S. Interplay between Circadian Clock and Cancer: New Frontiers for Cancer Treatment. Trends Cancer 2019, 5, 475–494. [Google Scholar] [CrossRef]
- Sancar, A.; Van Gelder, R.N. Clocks, cancer, and chronochemotherapy. Science 2021, 371, eabb0738. [Google Scholar] [CrossRef] [PubMed]
- Masri, S.; Sassone-Corsi, P. The emerging link between cancer, metabolism, and circadian rhythms. Nat. Med. 2018, 24, 1795–1803. [Google Scholar] [CrossRef]
- Battaglin, F.; Chan, P.; Pan, Y.; Soni, S.; Qu, M.; Spiller, E.R.; Castanon, S.; Roussos Torres, E.T.; Mumenthaler, S.M.; Kay, S.A.; et al. Clocking cancer: The circadian clock as a target in cancer therapy. Oncogene 2021, 40, 3187–3200. [Google Scholar] [CrossRef]
- Angelousi, A.; Kassi, E.; Ansari-Nasiri, N.; Randeva, H.; Kaltsas, G.; Chrousos, G. Clock genes and cancer development in particular in endocrine tissues. Endocr. Relat. Cancer 2019, 26, R305–R317. [Google Scholar] [CrossRef] [Green Version]
- Schernhammer, E.S.; Laden, F.; Speizer, F.E.; Willett, W.C.; Hunter, D.J.; Kawachi, I.; Colditz, G.A. Rotating night shifts and risk of breast cancer in women participating in the nurses’ health study. J. Natl. Cancer Inst. 2001, 93, 1563–1568. [Google Scholar] [CrossRef] [Green Version]
- Schernhammer, E.S.; Laden, F.; Speizer, F.E.; Willett, W.C.; Hunter, D.J.; Kawachi, I.; Fuchs, C.S.; Colditz, G.A. Night-shift work and risk of colorectal cancer in the nurses’ health study. J. Natl. Cancer Inst. 2003, 95, 825–828. [Google Scholar] [CrossRef] [Green Version]
- IARC Monographs Vol 124 Group. Carcinogenicity of night shift work. Lancet Oncol. 2019, 20, 1058–1059. [Google Scholar] [CrossRef]
- Wise, J. Danish night shift workers with breast cancer awarded compensation. BMJ 2009, 338, b1152. [Google Scholar] [CrossRef] [PubMed]
- Hurley, S.; Goldberg, D.; Nelson, D.; Hertz, A.; Horn-Ross, P.L.; Bernstein, L.; Reynolds, P. Light at night and breast cancer risk among California teachers. Epidemiology 2014, 25, 697–706. [Google Scholar] [CrossRef]
- James, P.; Bertrand, K.A.; Hart, J.E.; Schernhammer, E.S.; Tamimi, R.M.; Laden, F. Outdoor Light at Night and Breast Cancer Incidence in the Nurses’ Health Study II. Environ. Health Perspect. 2017, 125, 087010. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Saenz, A.; Sanchez de Miguel, A.; Espinosa, A.; Valentin, A.; Aragones, N.; Llorca, J.; Amiano, P.; Martin Sanchez, V.; Guevara, M.; Capelo, R.; et al. Evaluating the Association between Artificial Light-at-Night Exposure and Breast and Prostate Cancer Risk in Spain (MCC-Spain Study). Environ. Health Perspect. 2018, 126, 047011. [Google Scholar] [CrossRef]
- Garcia-Saenz, A.; de Miguel, A.S.; Espinosa, A.; Costas, L.; Aragones, N.; Tonne, C.; Moreno, V.; Perez-Gomez, B.; Valentin, A.; Pollan, M.; et al. Association Between Outdoor Light-at-night Exposure and Colorectal Cancer in Spain. Epidemiology 2020, 31, 718–727. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 9 April 2022).
- Downes, M.J.; Brennan, M.L.; Williams, H.C.; Dean, R.S. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open 2016, 6, e011458. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.A.; Hernan, M.A.; Reeves, B.C.; Savovic, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, L.; Shi, L.; Chu, H.; Murad, M.H. The magnitude of small-study effects in the Cochrane Database of Systematic Reviews: An empirical study of nearly 30 000 meta-analyses. BMJ Evid. Based Med. 2020, 25, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schunemann, H.J.; Group, G.W. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [Green Version]
| Interested Outcome | Example MEDLINE Search Strategy |
|---|---|
| Asthma and Allergies | Ovid MEDLINE(R) ALL <1946 to 16 June 2022> 1. (artificial light at night or ALAN or light at night).mp. 2. (blue light * or white light * or artificial light *).mp. 3. (night * or dark * or sleep * or chronotyp *).mp. 4. (asthma * or allerg * or immun *).mp. 5. 2 and 3 6. 1 or 5 7. 4 and 6 mp = title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms 379 results returned |
| Mental Health | Ovid MEDLINE(R) ALL <1946 to 16 June 2022> 1. (artificial light at night or ALAN or light at night).mp. 2. (blue light * or white light * or artificial light *).mp. 3. (night * or dark * or sleep * or chronotyp *).mp. 4. (mental health or mental illness or anxiety or depression or mood or schizophrenia or bipolar disorder or sleep disorder or insomnia).mp. 5. 2 and 3 6. 1 or 5 7. 4 and 6 mp = title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms 341 results returned |
| Cancer | Ovid MEDLINE(R) ALL <1946 to 16 June 2022> 1. (artificial light at night or ALAN or light at night).mp. 2. (blue light * or white light * or artificial light *).mp. 3. (night * or dark * or sleep * or chronotyp *).mp. 4. Cancer *.mp.a 5. 2 and 3 6. 1 or 5 7. 4 and 6 mp = title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms 429 results returned |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deprato, A.; Rao, H.; Durrington, H.; Maidstone, R.; Adan, A.; Navarro, J.F.; Palomar-Cros, A.; Harding, B.N.; Haldar, P.; Moitra, S.; et al. The Influence of Artificial Light at Night on Asthma and Allergy, Mental Health, and Cancer Outcomes: A Systematic Scoping Review Protocol. Int. J. Environ. Res. Public Health 2022, 19, 8522. https://doi.org/10.3390/ijerph19148522
Deprato A, Rao H, Durrington H, Maidstone R, Adan A, Navarro JF, Palomar-Cros A, Harding BN, Haldar P, Moitra S, et al. The Influence of Artificial Light at Night on Asthma and Allergy, Mental Health, and Cancer Outcomes: A Systematic Scoping Review Protocol. International Journal of Environmental Research and Public Health. 2022; 19(14):8522. https://doi.org/10.3390/ijerph19148522
Chicago/Turabian StyleDeprato, Andy, Himasha Rao, Hannah Durrington, Robert Maidstone, Ana Adan, Jose Francisco Navarro, Anna Palomar-Cros, Barbara N. Harding, Prasun Haldar, Saibal Moitra, and et al. 2022. "The Influence of Artificial Light at Night on Asthma and Allergy, Mental Health, and Cancer Outcomes: A Systematic Scoping Review Protocol" International Journal of Environmental Research and Public Health 19, no. 14: 8522. https://doi.org/10.3390/ijerph19148522








