Lower-Limb Kinematic Change during Pelvis Anterior and Posterior Tilt in Double-Limb Support in Healthy Subjects with Knee Malalignment
Abstract
:1. Introduction
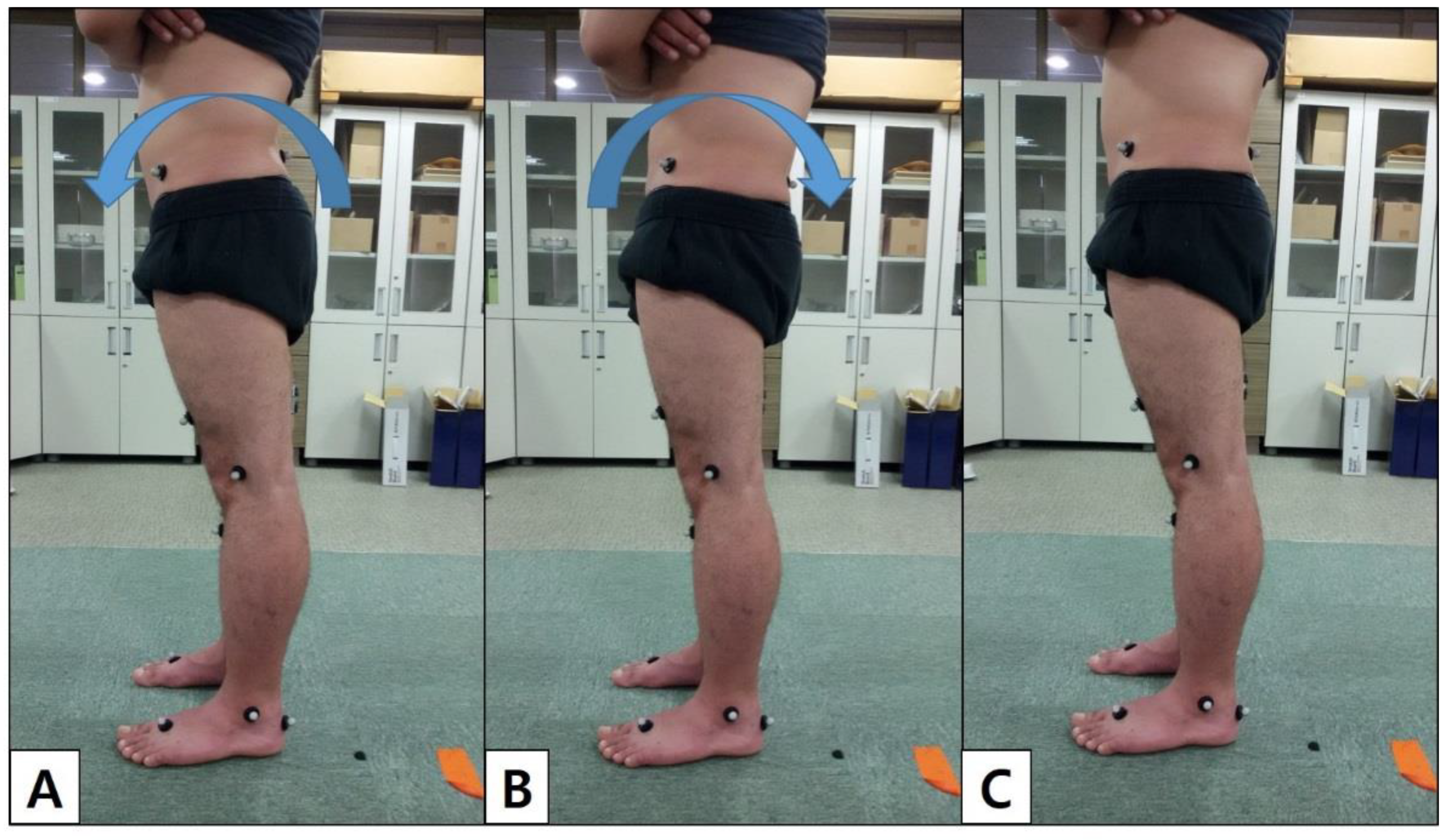
2. Methods
2.1. Participants
2.2. Determination of the Sample Size
2.3. Protocol
2.4. Data Analysis
2.5. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Emami, M.-J.; Ghahramani, M.-H.; Abdinejad, F.; Namazi, H. Q-angle: An invaluable parameter for evaluation of anterior knee pain. Arch. Iran. Med. 2007, 10, 24–26. [Google Scholar]
- Herrington, L.; Nester, C. Q-angle undervalued? The relationship between Q-angle and medio-lateral position of the patella. Clin. Biomech. 2004, 19, 1070–1073. [Google Scholar] [CrossRef] [PubMed]
- Fredericson, M.; Yoon, K. Physical examination and patellofemoral pain syndrome. Am. J. Phys. Med. Rehabil. 2006, 85, 234–243. [Google Scholar] [CrossRef] [PubMed]
- Khasawneh, R.R.; Allouh, M.Z.; Abu-El-Rub, E. Measurement of the quadriceps (Q) angle with respect to various body parameters in young Arab population. PLoS ONE 2019, 14, e0218387. [Google Scholar] [CrossRef]
- Horton, M.G.; Hall, T.L. Quadriceps femoris muscle angle: Normal values and relationships with gender and selected skeletal measures. Phys. Ther. 1989, 69, 897–901. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, Y.; Kumagai, M.; Mattessich, S.M.; Elias, J.J.; Ramrattan, N.; Cosgarea, A.J.; Chao, E.Y. Q-angle influences tibiofemoral and patellofemoral kinematics. J. Orthop. Res. 2001, 19, 834–840. [Google Scholar] [CrossRef]
- Aglietti, P.; Insall, J.N.; Cerulli, G. Patellar pain and incongruence. I: Measurements of incongruence. Clin. Orthop. Relat. Res. 1983, 176, 217–224. [Google Scholar] [CrossRef]
- Daneshmandi, H.; Saki, F.; Shahheidari, S.; Khoori, A. Lower extremity Malalignment and its linear relation with Q angle in female athletes. Procedia-Soc. Behav. Sci. 2011, 15, 3349–3354. [Google Scholar] [CrossRef] [Green Version]
- Smith, T.O.; Hunt, N.J.; Donell, S.T. The reliability and validity of the Q-angle: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2008, 16, 1068–1079. [Google Scholar] [CrossRef]
- Fairbank, J.; Pynsent, P.; van Poortvliet, J.A.; Phillips, H. Mechanical factors in the incidence of knee pain in adolescents and young adults. J. Bone Jt. Surgery. Br. Vol. 1984, 66, 685–693. [Google Scholar] [CrossRef] [Green Version]
- Riegger-Krugh, C.; Keysor, J.J. Skeletal malalignments of the lower quarter: Correlated and compensatory motions and postures. J. Orthop. Sports Phys. Ther. 1996, 23, 164–170. [Google Scholar] [CrossRef]
- Shultz, S.J.; Nguyen, A.-D.; Levine, B.J. The relationship between lower extremity alignment characteristics and anterior knee joint laxity. Sports Health 2009, 1, 54–60. [Google Scholar] [CrossRef]
- Alizadeh, S.; Mattes, K. How anterior pelvic tilt affects the lower extremity kinematics during the late swing phase in soccer players while running: A time series analysis. Hum. Mov. Sci. 2019, 66, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Khamis, S.; Dar, G.; Peretz, C.; Yizhar, Z. The relationship between foot and pelvic alignment while standing. J. Hum. Kinet. 2015, 46, 85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lankhorst, N.E.; Bierma-Zeinstra, S.M.; van Middelkoop, M. Factors associated with patellofemoral pain syndrome: A systematic review. Br. J. Sports Med. 2013, 47, 193–206. [Google Scholar] [CrossRef]
- Khamis, S.; Yizhar, Z. Effect of feet hyperpronation on pelvic alignment in a standing position. Gait Posture 2007, 25, 127–134. [Google Scholar] [CrossRef]
- Baumhauer, J.F.; Alosa, D.M.; Renström, P.A.; Trevino, S.; Beynnon, B. A prospective study of ankle injury risk factors. Am. J. Sports Med. 1995, 23, 564–570. [Google Scholar] [CrossRef]
- Kan, J.H.; Heemskerk, A.M.; Ding, Z.; Gregory, A.; Mencio, G.; Spindler, K.; Damon, B.M. DTI-based muscle fiber tracking of the quadriceps mechanism in lateral patellar dislocation. J. Magn. Reson. Imaging Off. J. Int. Soc. Magn. Reson. Med. 2009, 29, 663–670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramappa, A.J.; Apreleva, M.; Harrold, F.R.; Fitzgibbons, P.G.; Wilson, D.R.; Gill, T.J. The effects of medialization and anteromedialization of the tibial tubercle on patellofemoral mechanics and kinematics. Am. J. Sports Med. 2006, 34, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Neumann, D.A. Kinesiology of the Musculoskeletal System-E-Book: Foundations for Rehabilitation; Elsevier Health Sciences: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Ilahi, O.A.; Kohl, H., 3rd. Lower extremity morphology and alignment and risk of overuse injury. Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 1998, 8, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Powers, C.M. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: A theoretical perspective. J. Orthop. Sports Phys. Ther. 2003, 33, 639–646. [Google Scholar] [CrossRef] [PubMed]
- Franz, J.R.; Paylo, K.W.; Dicharry, J.; Riley, P.O.; Kerrigan, D.C. Changes in the coordination of hip and pelvis kinematics with mode of locomotion. Gait Posture 2009, 29, 494–498. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.R.; Nepple, J.J.; Philippon, M.J.; Kelly, B.T.; Larson, C.M.; Bedi, A. Effect of changes in pelvic tilt on range of motion to impingement and radiographic parameters of acetabular morphologic characteristics. Am. J. Sports Med. 2014, 42, 2402–2409. [Google Scholar] [CrossRef]
- Obeid, I.; Hauger, O.; Aunoble, S.; Bourghli, A.; Pellet, N.; Vital, J.-M. Global analysis of sagittal spinal alignment in major deformities: Correlation between lack of lumbar lordosis and flexion of the knee. Eur. Spine J. 2011, 20, 681–685. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schache, A.G.; Blanch, P.D.; Murphy, A.T. Relation of anterior pelvic tilt during running to clinical and kinematic measures of hip extension. Br. J. Sports Med. 2000, 34, 279–283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nguyen, A.-D.; Boling, M.C.; Levine, B.; Shultz, S.J. Relationships between lower extremity alignment and the quadriceps angle. Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 2009, 19, 201. [Google Scholar] [CrossRef]
- Ruwe, P.A.; Gage, J.R.; Ozonoff, M.; DeLuca, P. Clinical determination of femoral anteversion. A comparison with established techniques. J. Bone Jt. Surg. Am. Vol. 1992, 74, 820–830. [Google Scholar] [CrossRef]
- Levine, D.; Whittle, M.W. The effects of pelvic movement on lumbar lordosis in the standing position. J. Orthop. Sports Phys. Ther. 1996, 24, 130–135. [Google Scholar] [CrossRef]
- Robinson, R.L.; Nee, R.J. Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J. Orthop. Sports Phys. Ther. 2007, 37, 232–238. [Google Scholar] [CrossRef]
- Malinzak, R.A.; Colby, S.M.; Kirkendall, D.T.; Yu, B.; Garrett, W.E. A comparison of knee joint motion patterns between men and women in selected athletic tasks. Clin. Biomech. 2001, 16, 438–445. [Google Scholar] [CrossRef]
- Hollman, J.H.; Ginos, B.E.; Kozuchowski, J.; Vaughn, A.S.; Krause, D.A.; Youdas, J.W. Relationships between knee valgus, hip-muscle strength, and hip-muscle recruitment during a single-limb step-down. J. Sport Rehabil. 2009, 18, 104–117. [Google Scholar] [CrossRef] [PubMed]
- Kiriyama, S.; Sato, H.; Takahira, N. Gender differences in rotation of the shank during single-legged drop landing and its relation to rotational muscle strength of the knee. Am. J. Sports Med. 2009, 37, 168–174. [Google Scholar] [CrossRef]
- Bakhtiary, A.H.; Fatemi, E. Open versus closed kinetic chain exercises for patellar chondromalacia. Br. J. Sports Med. 2008, 42, 99–102. [Google Scholar] [CrossRef]
- Fonda, B.; Babič, J.; Šarabon, N. The Medial-Lateral Pedal Force Component Correlates with Q-Angle during Steady-State Cycling at Different Workloads and Cadences. Appl. Sci. 2021, 11, 1004. [Google Scholar] [CrossRef]
- McClay, I.; Manal, K. A comparison of three-dimensional lower extremity kinematics during running between excessive pronators and normals. Clin. Biomech. 1998, 13, 195–203. [Google Scholar] [CrossRef]
- Fulkerson, J.P.; Arendt, E.A. Anterior knee pain in females. Clin. Orthop. Relat. Res. 2000, 372, 69–73. [Google Scholar] [CrossRef] [PubMed]

| Variables | CON (n = 12) | ABQ (n = 10) |
|---|---|---|
| Gender(male/female) | 7/5 | 3/7 |
| Age (years) | 23.08 ± 1.72 | 22.50 ± 0.97 |
| Height (cm) | 168.33 ± 7.43 | 164.30 ± 10.02 |
| Weight (kg) | 66.58 ± 10.95 | 57.50 ± 12.56 |
| Q-angle (°) | 17.08 ± 2.50 | 27.00 ± 2.98 |
| Pelvic | Joint | Kinematics | ABQ | CON | t | p |
|---|---|---|---|---|---|---|
| Resting Position | Flex/Ext | −4.14 ± 4.53 | −4.57 ± 5.16 | −0.21 | 0.83 | |
| Hip (°) | Add/Abd | −2.91 ± 2.47 | −3.28 ± 3.57 | −0.28 | 0.77 | |
| Int/Ext | −5.36 ± 4.97 | −0.54 ± 4.61 | 2.33 | 0.03 * | ||
| Flex/Ext | 0.63 ± 6.41 | 0.99 ± 3.99 | 0.16 | 0.87 | ||
| Knee (°) | Add/Abd | −1.26 ± 2.41 | −2.10 ± 3.70 | −0.64 | 0.53 | |
| Int/Ext | 10.15 ± 7.04 | 5.48 ± 10.02 | −1.28 | 0.21 | ||
| Dorsi/Plantar | 10.89 ± 3.81 | 10.55 ± 3.25 | −0.22 | 0.82 | ||
| Ankle (°) | Inv/Ev | −1.76 ± 5.56 | −4.11 ± 5.73 | −0.97 | 0.34 | |
| Add/Abd | 14.62 ± 3.10 | 11.95 ± 4.37 | −1.67 | 0.11 | ||
| Anterior Tilt | Flex/Ext | −20.27 ± 7.73 | −17.74 ± 6.59 | 0.81 | 0.42 | |
| Hip (°) | Add/Abd | −3.46 ± 2.55 | −4.47 ± 2.41 | −0.94 | 0.35 | |
| Int/Ext | −6.10 ± 5.09 | −1.17 ± 5.26 | 2.22 | 0.03 * | ||
| Flex/Ext | −1.31 ± 8.59 | −6.38 ± 2.94 | −1.91 | 0.07 | ||
| Knee (°) | Add/Abd | −1.02 ± 2.47 | −1.80 ± 4.18 | −0.54 | 0.59 | |
| Int/Ext | 11.10 ± 7.31 | 7.90 ± 9.63 | −0.88 | 0.38 | ||
| Dorsi/Plantar | 13.77 ± 3.77 | 13.32 ± 3.23 | −0.29 | 0.77 | ||
| Ankle (°) | Inv/Ev | −0.56 ± 5.14 | −2.89 ± 5.63 | −1.01 | 0.32 | |
| Add/Abd | 14.29 ± 3.52 | 11.08 ± 4.46 | −1.88 | 0.07 | ||
| Posterior Tilt | Flex/Ext | 4.02 ± 3.41 | 4.37 ± 4.92 | 0.19 | 0.84 | |
| Hip (°) | Add/Abd | −3.60 ± 2.66 | −2.78 ± 2.50 | 0.73 | 0.46 | |
| Int/Ext | −1.63 ± 8.55 | 6.12 ± 2.23 | 3.02 | 0.01 * | ||
| Flex/Ext | 7.38 ± 8.42 | 8.54 ± 4.49 | 0.41 | 0.68 | ||
| Knee (°) | Add/Abd | −0.70 ± 2.72 | −1.68 ± 3.67 | −0.71 | 0.48 | |
| Int/Ext | 7.93 ± 6.71 | 5.77 ± 9.83 | −0.61 | 0.54 | ||
| Dorsi/Plantar | 7.57 ± 3.87 | 5.88 ± 3.32 | −1.08 | 0.29 | ||
| Ankle (°) | Inv/Ev | −1.98 ± 5.88 | −1.91 ± 6.48 | 0.02 | 0.97 | |
| Add/Abd | 15.66 ± 3.36 | 13.28 ± 4.23 | −1.53 | 0.14 |
| Pelvic | Joint | Kinematics | R | p |
|---|---|---|---|---|
| Resting Position | Flex/Ext | 0.203 | 0.364 | |
| Hip | Add/Abd | 0.135 | 0.549 | |
| Int/Ext | −0.547 | 0.008 ** | ||
| Flex/Ext | −0.166 | 0.461 | ||
| Knee | Add/Abd | 0.156 | 0.489 | |
| Int/Ext | 0.385 | 0.077 | ||
| Dorsi/Plantar | 0.007 | 0.976 | ||
| Ankle | Inv/Ev | 0.159 | 0.479 | |
| Add/Abd | 0.241 | 0.279 | ||
| Anterior Tilt | Flex/Ext | −0.011 | 0.961 | |
| Hip | Add/Abd | 0.307 | 0.165 | |
| Int/Ext | −0.482 | 0.023 * | ||
| Flex/Ext | 0.122 | 0.587 | ||
| Knee | Add/Abd | 0.104 | 0.645 | |
| Int/Ext | 0.304 | 0.169 | ||
| Dorsi/Plantar | 0.106 | 0.638 | ||
| Ankle | Inv/Ev | 0.151 | 0.502 | |
| Add/Abd | 0.237 | 0.287 | ||
| Posterior Tilt | Flex/Ext | −0.179 | 0.425 | |
| Hip | Add/Abd | 0.073 | 0.747 | |
| Int/Ext | −0.629 | 0.002 ** | ||
| Flex/Ext | −0.353 | 0.107 | ||
| Knee | Add/Abd | 0.184 | 0.411 | |
| Int/Ext | 0.315 | 0.153 | ||
| Dorsi/Plantar | 0.328 | 0.136 | ||
| Ankle | Inv/Ev | −0.102 | 0.653 | |
| Add/Abd | 0.149 | 0.508 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, S.H.; Yong, M.S.; Lee, H.Y. Lower-Limb Kinematic Change during Pelvis Anterior and Posterior Tilt in Double-Limb Support in Healthy Subjects with Knee Malalignment. Int. J. Environ. Res. Public Health 2022, 19, 9164. https://doi.org/10.3390/ijerph19159164
Park SH, Yong MS, Lee HY. Lower-Limb Kinematic Change during Pelvis Anterior and Posterior Tilt in Double-Limb Support in Healthy Subjects with Knee Malalignment. International Journal of Environmental Research and Public Health. 2022; 19(15):9164. https://doi.org/10.3390/ijerph19159164
Chicago/Turabian StylePark, So Hyun, Min Sik Yong, and Hae Yong Lee. 2022. "Lower-Limb Kinematic Change during Pelvis Anterior and Posterior Tilt in Double-Limb Support in Healthy Subjects with Knee Malalignment" International Journal of Environmental Research and Public Health 19, no. 15: 9164. https://doi.org/10.3390/ijerph19159164
APA StylePark, S. H., Yong, M. S., & Lee, H. Y. (2022). Lower-Limb Kinematic Change during Pelvis Anterior and Posterior Tilt in Double-Limb Support in Healthy Subjects with Knee Malalignment. International Journal of Environmental Research and Public Health, 19(15), 9164. https://doi.org/10.3390/ijerph19159164






