Abstract
After more than a century of research and debate, the scientific community has yet to reach agreement on the principal causes of racialized disparities in population health. This debate currently centers on the degree to which “race residuals” are a result of unobserved differences in the social context or unobserved differences in population characteristics. The comparative study of native and foreign-born Black populations represents a quasi-experimental design where race is “held constant”. Such studies present a unique opportunity to improve our understanding of the social determinants of population health disparities. Since native and foreign-born Black populations occupy different sociocultural locations, and since populations with greater African ancestry have greater genetic diversity, comparative studies of these populations will advance our understanding of the complex relationship between sociocultural context, population characteristics and health outcomes. Therefore, we offer a conceptual framing for the comparative study of native and foreign-born Blacks along with a review of 208 studies that compare the mental and physical health of these populations. Although there is some complexity, especially with respect to mental health, the overall pattern is that foreign-born Blacks have better health outcomes than native-born Blacks. After reviewing these studies, we conclude with suggestions for future studies in this promising area of social and medical research.
1. Introduction
In recent decades, researchers in the social and medical sciences have revisited a longstanding interest in racialized disparities in population health [1,2,3,4,5]. As it stands, after more than a century of research and debate, the scientific community has yet to reach agreement on the principal causes of these multigenerational disparities. We contend that one of the central reasons for stasis rests within the most prominent study design for investigating these disparities—comparing different racial groups on various measures of health status. This design risks confounding between racial group membership and real or perceived differences in social context and/or population characteristics—factors often left unobserved [6]. That is, the debate on how to interpret race residuals (we are referring to the fact that dummy variables for race in regression models often remain statistically significant after controlling for known correlates of a disease) turns on whether these residuals reflect unobserved differences in the social context or unobserved differences in population characteristics [7,8,9]. Therefore, our understanding of health disparities is incombered by overarching disagreements as to whether “race” is defined by or rooted in social context, group behaviors or biological endowments.
We join others in suggesting that the presence of a growing and diverse foreign-born population in the United States [10,11] represents an opportunity to improve our understanding of the social determinants of racialized population health disparities [12,13,14,15,16,17] (we use the term “foreign-born Blacks” to refer to those born outside the country that are either self-identified or legally classified as Black in the United States). To this end, it is important to note that disparities in morbidity and mortality between native-born Blacks and foreign-born Blacks are larger than nativity differences within any other racialized population—e.g., between native and foreign-born Latinx or Asian populations [18,19,20,21,22] (we use the term “native-born Blacks” to refer to all Blacks born in the United States. This term includes Blacks with foreign-born parents and African Americans, or the decedents of American slaves). Therefore, in addition to improving our descriptive understanding of increasing heterogeneity in Black population health, the fact that native- and foreign-born Blacks share the same racial status but often have different health profiles also presents us with a quasi-experimental design for studying factors that might also contribute to racialized disparities in population health [12,13,14,15,16,17]. That is, since native and foreign-born Blacks share the same racial status while sometimes having different experiences, cultural values and practices [13,23,24], comparative studies of these populations might improve our understanding of the ways in which various race-related sociocultural factors might contribute to disparities in population health between these and other groups [12,13,14,15,16,17].
While there are a range of possible native/immigrant comparisons, the comparison of native and foreign-born Blacks represents a uniquely useful research paradigm because Black people are the only U.S. population whose racial classification has to do with notions of genetic ancestry [25] and also includes a large immigrant population [10,26]. While “blood quantum” has also been a key determinant of being legally classified as Native American [27], there are no Native American “immigrants” in the United States (we understand that there are many Native Americans that migrate from reservations to other locations in the United States and that this experience may be like the experiences of many foreign-national migrants. While scientists should conduct more research on the ways in which this experience shapes Native American health, we reserve the term “immigrant” to refer to the migration of foreign nationals). Conversely, there are large numbers of Asian and Latinx immigrants, but the Census Bureau legally classifies these populations according to their language and/or national origins, not blood quantum or genetic ancestry. Moreover, the current practice of the U.S. Census conceptualizes Latinx as an ethnic group that is composed of different racial population groups. That is, we continue to debate whether people with proximal ancestry in Latin America constitute their own racial group or an ethnic group that includes different racial categories. Given that this debate remains unsettled, we do not include studies that include “Black” migrants from Latin America [28,29,30].
It is also important to note that populations with greater amounts of African genetic ancestry tend to have greater genetic variation [31]. This means that we can gain a more fine-grained analysis of the potential interplay between the environment, genomics (including, single nucleotide polymorphisms, methylation and/or gene expression) and population health, especially since there is simultaneously great variation in the health of these populations [18,22].
We advance the argument for the comparative study of native and foreign-born Blacks in four ways. First, we review differences between these populations vis-à-vis the most prominently studied determinants of population health (i.e., health behaviors, socioeconomic status, environmental factors and population genetics), arguing that since these populations have different social and cultural locations and practices, comparative studies of these populations might yield important insights into the social determinants of population health. Second, we argue that, since native and foreign-born Blacks experience and interpret race differently in the U.S. [24,32,33,34,35,36], the comparative study of these populations will also advance our understanding of the role of racialized bias and discrimination in population health disparities. Third, we suggest that, since these populations share the same racial status, and since populations with greater amounts of African ancestry have greater genetic diversity [31], the comparative study of these populations will improve our understanding of the complex interplay between sociocultural context, population genetics and health outcomes in a way that avoids debates having to do with the nature of racial classification (e.g., [37,38]). Fourth, we encourage the comparative study of native and foreign-born Black health by offering a summary review of 208 existing studies that compare the health of these populations, including potential data sources for further investigation. This is the first review of its kind and offers the current state of knowledge on patterned health differences between native and foreign-born Blacks. We conclude our review with our thoughts on potential future directions within this research paradigm.
2. Descriptive Benefits
Most studies of health disparities between White and Black (read native-born Black or African American) populations in the United States have an implied interest in the relative health of native-born Whites and the decedents of enslaved Africans in the United States. However, over the last five or six decades, the country of origin of the U.S. Black population has diversified. Between 1960 and 2005, a 22-fold increase in the number of foreign-born Black people living in the United States occurred (from 125,000 to 2,815,000; [10]). Since 1990, this rapid increase in the size of the foreign-born Black population has been met with increasing diversity in the regions and countries from which immigrants originate. While foreign-born Blacks from the Caribbean have been migrating to the U.S. since the early 1900s [26], between 2000 and 2005, more foreign-born Blacks entered the U.S. from Africa than the Caribbean [10]. Moreover, there is greater diversity in the reasons for migration, especially from African countries—more enter as refugees, asylees or on diversity visas [10]. Black people also migrate to the U.S. from non-majority Black countries throughout Europe [17]. Increases in the size and diversity of the foreign-born Black population in recent decades complicates our understanding of the U.S. Black population [10,24]. That is, increasing portions of Blacks in the United States do not have ancestry in American slavery and are therefore not part of the traditional perspective on multigenerational Black–White inequality in the U.S.
Although these population trends have resulted in greater diversification in the Black population, most research into population health overlooks this diversity. This practice obscures our ability to analyze and understand the increasing variation in the health status of this rapidly diversifying population. Indeed, disparities between native and foreign-born Blacks are wider than those between other native and foreign-born populations within other racialized groups [18,22]. As our review of the literature shows, there are a range of health differences between native and foreign-born Blacks, but most studies show that foreign-born Blacks have better health profiles than native-born Blacks. This means that, in addition to not having a good understanding of the health status of an increasingly diverse Black population, it is likely that studies that do not account for this heterogeneity are underestimating and potentially misunderstanding the basic nature of population health differences between Blacks and Whites. Parsing the Black population will therefore improve our understanding of the nature of Black population health and Black–White health disparities in the United States.
3. Perspectives on Black Ethnicity and Population Health
While most are interested in the health of the decedents of American slavery, there is also a longstanding interest in the comparative study of different Black populations as part of a larger effort to understand and unpack the nature of Black–White racial disparities across a range of life domains. These began with distinctions between Blacks, both “slave” and “free” [23,39], but also included distinctions between native and foreign-born Blacks [23,40]. The more recent of these studies show that these populations have different levels and kinds of education [41,42], hold different kinds of jobs [43], attain different levels of success in the labor market [44,45] and often live in different neighborhoods, experiencing different levels of housing segregation from Whites [46,47]. Therefore, while they might share a similar multivariate distribution of skin color, hair texture and craniofacial bone structure, these populations experience the U.S. racialized social system [48] differently [24,32,33,34,35,49,50,51,52,53,54,55]. Differences in sociocultural context and practice matched with similarities in markers that are widely associated with “racial status” mean that the comparative study of these populations presents a quasi-experimental study design whereby racial status is “held constant” while allowing various factors that are associated with the “social determinants of health” to vary [12,13,14,15,16,17].
Population health researchers have previously described the basic advantages of this study design. For instance, in 1992, Richard Davis argued that, given social and cultural differences between native and foreign-born Blacks, there might be great scientific benefit to model stratification across these populations. He argued that “…it stands to reason that the assimilation patterns of native and foreign-born Blacks may be fairly different; if for no other reason than that they often speak a different language… Foreign-born bilingual or non-English speaking Blacks may find it more convenient to coalesce among themselves… these factors suggest the possibility of a very different pattern of assimilation for Black ethnics” [13].
About a decade later, James Jackson and colleagues suggested that comparisons between native and foreign-born Blacks would help refine our understanding of “… the types and amounts of racial and non-racial factors that affect the differential distribution of mental disorders within race and ethnic groups can be identified, leading to possible explications of how race and ethnic group memberships combine with different types of stressors to affect mental health” [16] and that, “… differential immigration experiences among [foreign-born Blacks] will contribute to understanding the mental health implications of racial/ethnic identity and acculturation strategies” [16]. They then suggest that this “… will result in a better understanding of the nature of racial and ethnic differences in the distribution of serious mental disorders” [16].
Shortly thereafter, Carlotta Arthur and Edward Katkin argued that comparative studies of native and foreign-born Blacks will “… raise awareness of the issue of ethnicity among Black populations and to bring attention to new ways to think about health disparities research and the promise that such explorations hold for finding new avenues through which to intervene” [12], including “…in-depth knowledge of the ways in which ethnicity and culture interact with health-related issues in Black populations in the U.S” [13].
While these scholars have done well to describe the ways in which the comparative study of native and foreign-born Blacks will allow for insights into the role of “race and culture” in population health, we develop this perspective further, offering a more detailed consideration of how such studies might improve our understanding of population health disparities. That is, the previously proposed distinctions focus on “race”, “ethnicity” and “culture”, broadly speaking. We offer a more detailed assessment, parsing these broad distinctions into four principal causes of population health: health behaviors, socioeconomic status, environmental stressors and population genetics [15,56]. Since we believe that earlier efforts were an attempt to say that the comparative study of native and foreign-born Black health might allow for a greater understanding of the relative role of these principal causes, we illustrate the utility of this comparative approach by reviewing differences between these populations across the principal causes of health disparities.
3.1. Health Behaviors
Most health scientists agree that diet, nutrition and exercise matter for individual health outcomes, but there are still questions concerning the relative importance of health behaviors in explaining racialized differences in population health. Some researchers have speculated that “unexplained differences reflect unmeasured factors that are associated with both race/ethnicity and the specified outcome but are not related to either discrimination or socioeconomic position, [including] culturally shaped patterns of food consumption” [57]. Indeed, studies show that foreign-born Blacks report what some may classify as better health behaviors than native-born Blacks, suggesting that this unobserved “cultural” factor might contribute to health differences between these populations. For instance, native-born Blacks are more likely to smoke than foreign-born Blacks [19,58,59]. Native-born Blacks are also more likely to drink and use drugs than foreign-born Blacks [59,60]. Foreign-born Blacks are more likely than native-born Blacks to report “at least some physical activity” [59], and they have more healthful diets than native-born Blacks [61]. Since these populations have known differences in health behaviors, their health differences might stem from different health behaviors.
3.2. Socioeconomic Status
One of the central arguments in studies that focus on the social determinants of health is that socioeconomic status plays a central, if not fundamental, role in shaping population health [62]. Native and foreign-born Blacks also have known differences in socioeconomic status and resources. Foreign-born Blacks have greater educational attainment than native-born Blacks [44] and are also more likely to attend more selective colleges and universities [42]. Although newly arriving foreign-born Blacks often have lower annual earnings than native-born Blacks, their earnings often match or exceed the earnings of native-born Blacks after being in the labor market for about 15 years [44,63,64]. Foreign-born Blacks also have a greater occupational status than native-born Blacks [43]. Since socioeconomic status and resources play a key role in population health disparities and foreign-born Blacks have greater socioeconomic status profiles than native-born Blacks, health differences between these populations might result from differences in socioeconomic status.
3.3. Environment
The environmental factors that contribute to health outcomes range from psychosocial stressors to the physical ecology of the built environment. Studies that assess housing segregation between native and foreign-born Blacks show that, while not as pronounced as Black–White segregation, these populations often live in different areas [47,65]. Therefore, there may be some differences in their physical ecology. Although these populations experience similar levels of racial discrimination [34], the nature of these racialized experiences may be different [32,53], and/or they may process or cope with relatively similar experiences differently [24,66,67]. Unlike native-born Blacks, foreign-born Blacks experience various forms of stress associated with the process of immigrant assimilation [32,55], and they enter the United States from both majority-White and majority-Black sending countries [17], which means Black populations in the United States might have historical differences in racial context at different stages of the life course [14,68,69]. Since these populations often live in different neighborhoods and experience different psychosocial stressors (differently), comparative studies might allow for improvements in our understanding of how the social and physical environment contributes to disparities in population health.
3.4. Genetics
In recent years, medical scientists have made tremendous headway in furthering our understanding of the links between genetics and individual health outcomes, but the relationship between genetics and health disparities between population groups remains less clear [70,71,72]. Still, some interpret race residuals as offering evidence of the role of unobserved differences in population genetics, which, when comparing Whites and Blacks, may, knowingly or unknowingly, lend credence to arguments for the genetic determinants of racial difference [73] (these scientists are often much less clear or forthcoming about what these genetic differences might be and how they might contribute to differences in health between populations with different racial statuses). Notwithstanding the fact that native and foreign-born Blacks share the same racial status and similar distributions of African genetic ancestry while occupying different sociocultural contexts, comparative studies avoid contentious debates on the genetic basis of racial difference and the potential role of such genetic differences in population health disparities. However, scientists can still further investigate the potential role of genetics in population health (e.g., single-nucleotide polymorphisms, genetic methylation and gene expression; [37,38,74]). For instance, while native and foreign-born Blacks have similar physical features that are widely associated with Blackness (i.e., skin color, hair texture and craniofacial bone structure; [75]), it is entirely possible that these populations have other important biological differences. Indeed, there is more genetic variation in populations with greater African ancestry, which might further advance our understandings of complex interactions between genes, the environment and health. For example, such studies might consider differences in DNA methylation and/or gene expression [76] and how such differences might be related to differences in historical traumas [77,78].
4. Methods
Since we believed that, compared to the study of other native and immigrant populations, there were few studies of native and foreign-born Black populations, we began with an effort to find all existing studies that compared the health of these populations. The initial timeframe for our review took place between August 2017 and May 2018. We began by searching the MEDLINE/PubMed database using the keyword “Black immigrant”. Given our larger argument, we only retained studies that included a comparison with native and foreign-born Blacks. We excluded studies that only included foreign-born Blacks because they do not allow for direct comparisons with native-born Blacks. This search resulted in 29 “seed studies”. We then reviewed the citations included at the end of these studies and used the “cited by” feature on Google Scholar to find studies that cited any of the seed studies. We repeated this process for each study that we found until we no longer found additional studies (i.e., checking the references at the end of studies for more studies and finding all known citations of each study that we identified, using Google Scholar). This process identified 139 studies. We then re-ran this process again in April 2022. We reviewed all the 139 previous identified studies and used the “cited by” feature of Google Scholar to identify recently published studies that cited any of our 139 previously identified studies. As we identified more recently published studies, we then checked their references for previously unidentified studies. This process resulted in a total of 208 studies of health disparities between native and foreign-born Blacks. As the focus was on health outcomes, we excluded studies that focused on health-seeking behaviors and the use of health services. While some studies also controlled for health status co-morbidity, we did not specify this in our tables, as health status did not fit within our set of principal causes for population health.
5. Results
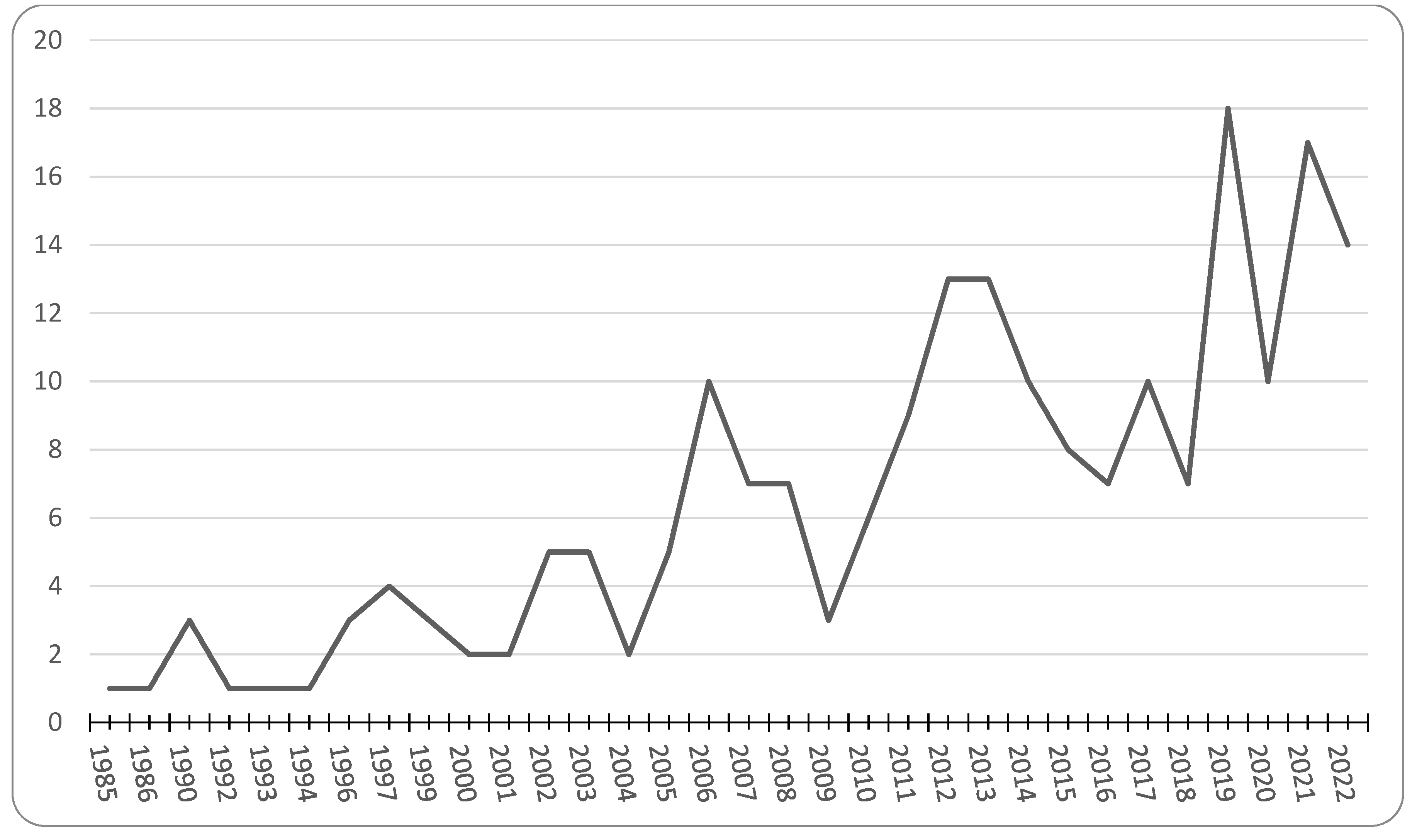
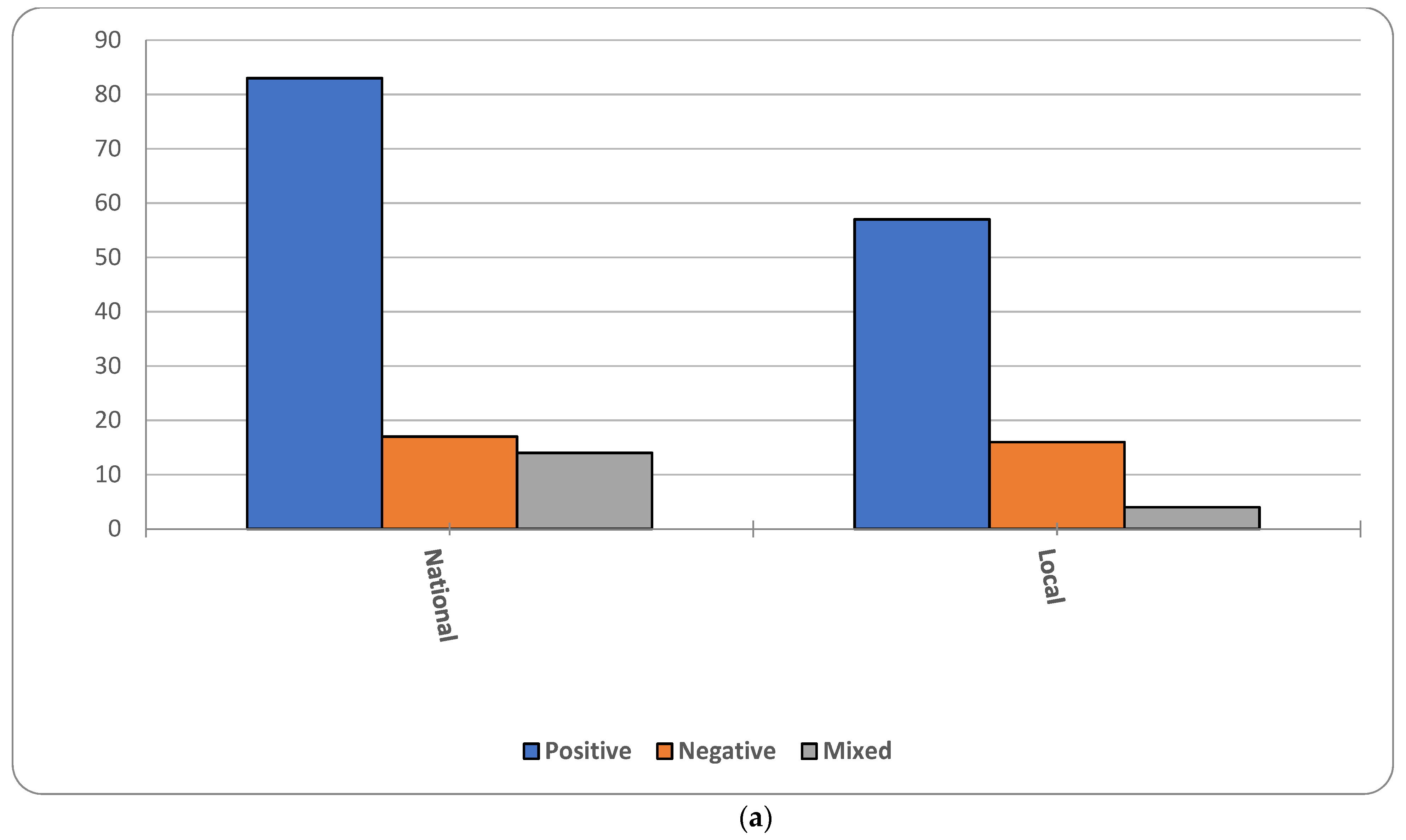
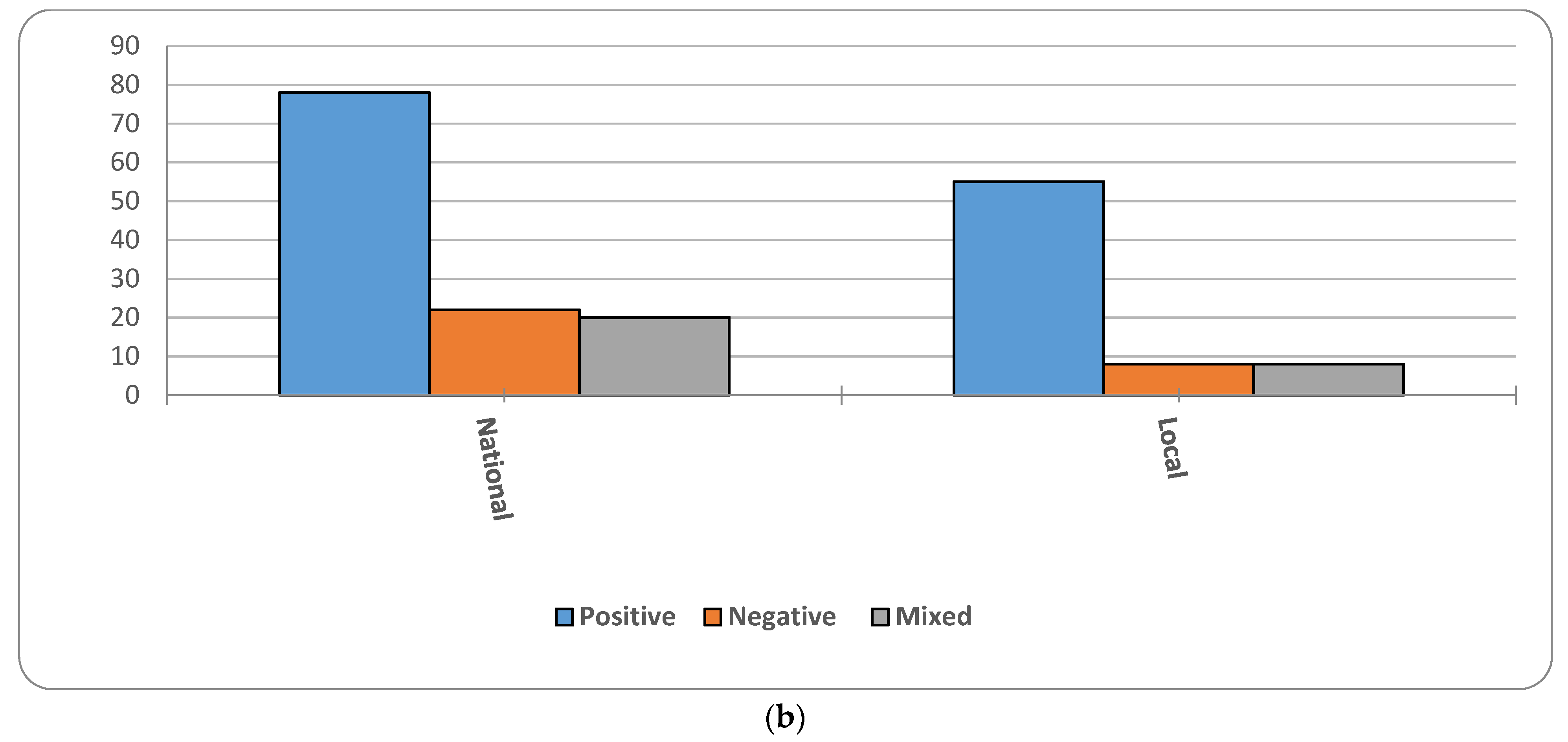
We organized the studies that we identified in Table 1 according to the Institutes of the National Institutes of Health. Most of the studies controlled for differences in socioeconomic status (194), followed by environment (55) and health behaviors (60), while very few considered genetics (6). The majority of national studies used data from the National Survey of American Life (NSAL, 45; [79]), followed by the National Health Interview Survey (NHIS, 34), the National Health and Nutrition Examination Study (NHANES, 11) and the U.S. Census (10). The remaining studies included small non-probability samples from specific community locations. Figure 1 shows the overall trend in the number of studies. The first study appeared in 1985. Since then, there has been a general increase in the rate of publications, but this increase has tapered off in recent years. Figure 2a,b shows that most studies, both bi-variate (or descriptive) and multivariate (or adjusted), report better health among foreign-born Blacks. We use the term “positive” to infer that our basic hypothesis holds true in these cases—i.e., foreign-born Blacks have better health than native-born Blacks. We use the term “negative” to denote the opposite and “mixed” when multiple outcomes had different “directions.” Although these populations are sometimes different on measures of health behavior, socioeconomic status and environment, our summary of the multivariate figures suggests that studies that account for these factors often do not provide a full accounting for health disparities between these populations.

Table 1.
Stress, behavior and outcomes.
Figure 1.
Number of Publications Comparing native- and foreign-born Blacks, By Year.
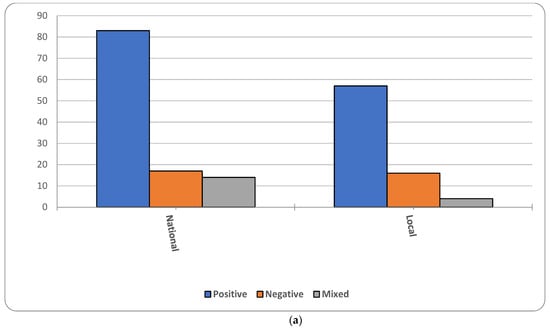
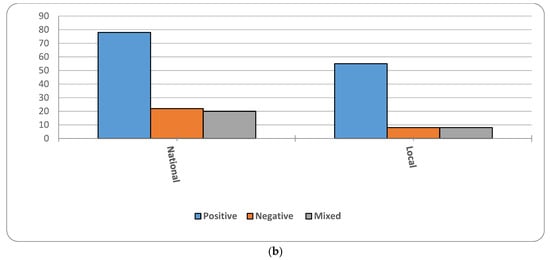
Figure 2.
(a); Proportion of studies affirming hypothesis, Bivariate results (b) Proportion of studies affirming hypothesis, Multivariate results.
6. Mental Health
According to Table 1, the most often studied set of health outcomes falls under the scope of mental health. A total of 40 studies examined differences in mental health between native and foreign-born Blacks. Studies that assessed mental health disorders used either clinical assessments or validated self-report scales. A total of 26 studies used clinical, structured interviews that diagnosed the respondent using classifications in the Diagnostic and Statistical Manual of Mental Health Disorders, Fourth Edition (DSM-IV). Some studies that used DSM-IV classifications also used the World Mental Health Composite International Diagnostic Interview (WMH-CIDI). Cohen and colleagues [80] used clinically diagnosed mental health disorders assessed by medical chart reviews. A few studies used The Center for Epidemiologic Studies Depression Scale (7, CES-D), all of which used the NSAL. The remaining studies used validated self-report scales evaluating self-rated mental health and the Short Form–8 or 12 scales.
These studies present a mixed picture across both national and local community samples and within and across mental health categories. Most of the studies used nationally representative samples (37 of 40), of which 34 of the 37 used data from the NSAL. Studies using the NSAL evaluated a range of mental health outcomes including, but not limited to, depressive symptomatology, mania, panic disorders, phobias, anxiety disorders, suicidality and developmental disorders. Even when accounting for the variability across mental health outcomes, there was no clear pattern in mental health disparities between native and foreign-born Blacks. For example, the most common mental health outcome, depressive symptomatology, had studies that varied in results, with most studies either having better or the same depressive symptoms for these populations. This pattern was also evident in the three local studies, which took place in a range of metropolitan areas in the East and Midwest [81,101,242].
7. Maternal and Child Health
We identified 42 maternal and child health studies in Table 1, making this the most studied physical health outcome. Of these 42 studies, 26 focused on low birthweight (LBW) and/or preterm birth (PTB). These studies mostly used vital records data, one study used census data, another study used data from the National Center of Health Statistics, and two studies relied on local samples. The study that used data from the U.S. Census [130], found a relatively equal rate of adverse birth outcomes between native and foreign-born Blacks. The other 14 national and local studies consistently found that foreign-born Blacks had lower rates of adverse birth outcomes than native-born Blacks.
Studies that examined low birthweight, defined as an infant born under 2500 g, found that native-born Blacks had higher rates of infants born at a low birthweight than foreign-born Blacks [69,118,120,121,123,124,125,126,127,128]. For instance, a study using vital statistics data [126] found that foreign-born Blacks had a reduced risk of giving birth to a low birthweight infant by approximately 25% when compared to native-born Blacks.
Studies that examined preterm birth, defined as an infant born prior to 37 weeks of gestation, found that native-born Blacks had higher rates of infants born preterm than foreign-born Blacks [18,69,128,129,131]. A recent study that used birth record data from 27 states [131] found that, compared to native-born Blacks, foreign-born Blacks had significantly lower rates of PTB. When examining the foreign-born Blacks by region of origin, this study also found that Sub-Saharan African-born Black women had significantly lower rates of PTB compared to Caribbean-born Black women.
8. Cardiovascular
In Table 1, we list 26 studies of disparities in cardiovascular health between native and foreign-born Black populations. National studies consistently show higher blood pressure and a greater risk of hypertension among native-born Blacks, but several local studies paint a more complex picture. Nationally, about 37% of native-born Blacks report hypertension diagnosis, compared to a little over 20% of foreign-born Blacks [171,173]. Although much less common, several studies consider other indicators of cardiovascular health, including heart trouble and problems with blood circulation. Native-born Blacks appear to have a higher rate of death by coronary heart disease than Blacks born in the Caribbean [157]. Foreign-born Black women have lower rates of myocardial infraction than native-born Black women [161], and a small study of 125 native-born and 150 Caribbean-born Black hospital patients in New York City found that the native-born were more likely to have suffered a myocardial infraction, but no differences in previous cerebrovascular disease or peripheral vascular disease [166]. Another study of the 1988–1994 NHANES III shows that foreign-born Blacks had a lower risk of stroke and heart attack than native-born Blacks [61].
9. Metabolic Conditions
Metabolic conditions include diabetes mellitus, abnormal cholesterol levels and potential complications with obesity. In Table 1, we identified 21 of these studies. Studies measured obesity using self-reported height and weight. Nine out of ten studies reported that native-born Black adults had higher obesity than foreign-born Black adults [170,187,188,189,190,191,194,251]. Most studies evaluated the NHIS or NHANES. The picture for diabetes was generally mixed [22,161,173,179,180,181,182]. Like obesity-related studies, national studies used NHIS or NHANES. National studies more often showed better outcomes for foreign-born Blacks. The three local studies reported similar trends between the two groups. The only study that reported better diabetes outcomes among native-born Blacks assessed type 1 diabetes (T1D) among youth in Washington state, showing that foreign-born Black populations had T1D prevalence rates that were four times higher than African American youth (6.20/1000 vs. 1.56/1000; [181]).
10. Cancer
We list 30 cancer studies in Table 1. The majority were local and primarily conducted in the Northeast [196,197,199,200,207]. While cancer encompasses a range of outcomes, the outcomes evaluated were specific to the reproductive system (e.g., breast, cervical, and the human papillomavirus). The national studies included data from the NHIS, NHANES and the U.S. Census [58,202,203,205]. The outcomes focused on cancer-related behaviors such as prostate cancer screening, pap smear tests and tobacco use. These studies presented mixed findings. Seven of the 17 local studies reported that foreign-born Blacks had worse cancer outcomes than native-born Blacks, and the other studies were generally mixed. The most recent of these studies found that native-born Black women reported that HPV vaccinations were more accessible to them than foreign-born Black women (Χ = 4.19, p < 0.05; [207]). Eight of the 12 national studies reported that foreign-born Blacks had better cancer outcomes and cancer-related behaviors than native-born Blacks. Some studies that reported that native-born Black populations had better cancer-related outcomes related to cancer screenings and outcomes ([(OR=3.37, 95% CI (1.89, 5.96)]; [205]).
11. Substance Use and Alcohol Use
In Table 1, twenty-four studies focused on substance and alcohol use outcomes. Substance use disorders occur when recurrent use of alcohol and/or drugs clinically impedes personal health [252]. The 16 studies on substance use disorders evaluated marijuana use, tobacco use and use of controlled substances. Using the National Longitudinal Study of Adolescent to Adult Health (or Add Health), Bui and colleagues, 2013 [232] assessed substance use disorders in Black adolescents and found that there were no differences in substance use when comparing native and foreign-born Blacks. The remaining national studies reported that, among adults, foreign-born Blacks were less likely to report substance use disorders than native-born Blacks. The three studies that were conducted in local settings, in Northeastern cities, were consistent with the national studies [118,231].
Eight of the 24 studies focused on alcohol use disorders. Alcohol use encompassed studies that evaluated binge drinking, alcohol abuse and alcohol use initiation. These studies trended towards better outcomes for foreign-born Blacks. Three studies deviated from this general pattern. A local study that evaluated alcohol initiation in Black adolescents found that Caribbean-born adolescents were more likely to have been in contact with alcohol than the native-born adolescents ([OR = 1.51; 95%CI (1.18–1.95)]; [226]). An examination of the National Epidemiological Survey on Alcohol and Related Conditions (NESARC) assessed alcohol use in the past 12 months and risky alcohol use behaviors (i.e., binge drinking) and found that, before adjusting for relevant covariates, foreign-born Blacks were less likely than native-born Blacks to drink or drink in a risky manner [229]. However, the adjusted estimates showed that foreign-born Black women were more likely to report using alcohol in the past 12 months than native-born women [229]. Overall, substance and alcohol use disorders are more likely among native-born than foreign-born Black adults; however, this pattern may not hold for adolescents.
12. Health-Related Quality of Life
We list 23 studies related to health-related quality of life in Table 1. For our review, health-related quality of life studies included self-rated physical and mental health, aging, as well as epidemiological studies assessing morbidity and mortality. Most of the studies evaluated national data, with the majority being from the NHIS (8), U.S. Census (7), and the NSAL (5). Two studies focused on local populations in Boston, Massachusetts and Florida [242,253]. When compared to foreign-born Blacks, all studies found that native-born Blacks reported poorer physical and/or mental health.
13. Discussion
We have joined others in offering the comparative study of native and foreign-born Blacks as a useful approach to the study of the social determinants of population health disparities and for improving our understanding of the complex interplay between social context and population characteristics in various health outcomes [12,13,14,15,16,17]. Our assessment is that, while disparities in mental health are complex, across a variety of physical health outcomes, on average, foreign-born Black populations have better health profiles than native-born Black populations—before and after controlling for various measures of health behaviors, socioeconomic status, environmental factors and/or genomics. As very few studies have been able to account for health differences between these populations, there is much more for us to learn. We conclude with some preliminary thoughts on the trends we reviewed, what we believe to be important omissions and promising opportunities for largely descriptive research in the near term, and how studies might use this comparative research design to advance our understanding of the social determinants of (racialized) population health over the longer term.
Most of the studies we reviewed are on mental health outcomes; however, the overall pattern of findings in this area is less clear than the pattern for physical health. There might be a range of explanations for this pattern. One thing to consider is that this is an artifact of measurement bias. Not only is mental health more difficult than physical health to assess in survey studies, but our current measures may not be culturally equivalent for these populations [254,255]. Conversely, measures of physical health outcomes might be more valid and reliable across these populations. That said, it is also possible that existing studies have revealed the true underlying pattern; however, mental health is complex, and so, for different dimensions of mental health, disparities between native and foreign-born Blacks are different. Therefore, we believe that, in addition to paying greater attention to disparities within a given mental health outcome, we need more studies that assess the relative construct validity of mental health measures across these populations.
We also observed a few areas of research that could benefit from more attention. For example, there are very few studies of cancer disparities. Most of the work on cancer draws on small local studies and involves screening for the presence of disease. We also need more studies that include the children and grandchildren of foreign-born Blacks. Exceedingly few studies considered the role of time since migration or the ways in which return migration might shape these disparities. While some have likely avoided an assessment of years since migration because of concerns about model identification, studies from the labor market show that these models are “identified” [34,44]. Another strategy is to estimate separate models, parsing foreign-born Blacks by different groups of years since migration (e.g., <1 to 5, >5 to 10, etc.). Finally, we only found two studies that considered any genetic differences between these populations [38,74].
In addition to a more refined description of health disparities between native and foreign-born Blacks, we continue to believe that the comparative study of these populations can improve our larger understanding of the social determinants of (racialized) disparities in population health. First, since these populations are both racially classified as Black in the U.S., sharing a multivariate distribution of skin color, hair texture and craniofacial bone structure and very likely have similar distributions of African genetic ancestry, health disparities between these populations are not likely to invoke explanations that, knowingly or unknowingly, promote the notion that race is a biological or genetic construct. That is, when or if social factors (e.g., health behaviors, socioeconomic status, and environmental factors) do not account for health disparities between native and foreign-born Blacks, any speculation on unobserved genetic differences will not be mired in contentious debates on the genetic basis of racial classification. Indeed, our review shows that several studies considered various social factors but that there remained a residual health difference between native and foreign-born Blacks. We cannot attribute this residual difference to differences in racialized notions of population genetics. This restriction will improve clarity on the nature of racialized differences in population health by muting such speculation.
The comparative study of these populations might also provide greater insight into the links between racial discrimination and health. While native and foreign-born Blacks both report experiences with racial discrimination, they may interpret or process these experiences differently. Differences in perception include differences in whether an act constitutes racial discrimination and differences in the meaning or importance of the experience. While these differences are also present among native-born Blacks, there are potentially unique reasons for similar differences between native and foreign-born Blacks. For instance, while any given two native-born Blacks might disagree on whether an experience was racially discriminatory or may differ on the importance of their experience, similar differences in perception between native and foreign-born Blacks might be uniquely motivated by nativity or differences in orientation to the centrality of American slavery in their life histories. As foreign-born Blacks are not decedents of the American “colonial situation” of chattel slavery [29] and are largely in the country by choice, except for instances of forced migration (and often with previous knowledge of American racism), their interpretation of the event might resonate differently than for native-born Blacks. While the former might understand the experience as an inconvenient nuisance in their immediate circumstance, for the latter, the same experience might trigger psycho-historical traumas that are rooted in the belief that this experience is a continuance of generations of dehumanization and restricted freedoms. While foreign-born Blacks often hail from countries with histories of slavery and colonialism, foreign-born Blacks might experience or read anti-Black and/or racialized experiences in the United States as existing outside of or unrelated to histories of slavery and colonialism in their sending countries, resulting in a different level or kind of “dose response”. Therefore, studies that compare these stress processes might help us to better understand the psychosocial factors that help link historical traumas to health outcomes [77,78].
14. Conclusions
Finally, there is the issue of the collection and availability of nationally representative data on these populations. For the first time, between 2001 and 2004, the Program for Research on Black Americans at the Institute for Social Research at the University of Michigan at Ann Arbor collected nationally representative data on both native-born Blacks and Afro-Caribbeans (including known f probabilities; [16,79]). While researchers have found this dataset tremendously fruitful (as shown above), the dataset is aging (very well), but it does not include a representative sample of foreign-born Blacks from African or other countries. It is also cross-sectional and does not include biomarkers for health and genomics. As we approach the 20th anniversary of this novel and productive data collection, it may be time to begin the process of planning the next major national data collection with the aim of understanding “Race, Ethnicity and the African Diaspora in the United States”—one that might take the best from other national data collections, such as the National Survey of Black Americans, the National Survey of American Life, the National Longitudinal Study of Adolescent to Adult Health and the Health and Retirement Survey.
Author Contributions
M.A.I.: Lead in the development of the conceptual framing, lead in the writing of the manuscript, managed and directed the literature search, advised on the development of tables and figures; Y.F.: contributed to the conceptual framing, contributed to the writing of the manuscript, contributed to the development of the tables, assisted with finding studies; W.L.: assisted with the development of the tables and figures, assisted with finding studies, provided copy editing; D.W.: contributed to the conceptual framing, contributed to the writing of the manuscript, lead in the development of the tables and figures, assisted with finding studies. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Arul, K.; Mesfin, A. The Top 100 Cited Papers in Health Care Disparities: A Bibliometric Analysis. J. Racial Ethn. Health Disparities 2017, 4, 854–865. [Google Scholar] [CrossRef] [PubMed]
- Du Bois, W.E.B. The Philadelphia Negro; University of Pennsylvania Press: Philadelphia, PA, USA, 1899. [Google Scholar]
- Rogers, R.G.; Lawrence, E.M.; Hummer, R.A.; Tilstra, A.M. Racial/Ethnic Differences in Early-Life Mortality in the United States. Biodemography Soc. Biol. 2017, 63, 189–205. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.K.; Jemal, A. Socioeconomic and Racial/Ethnic Disparities in Cancer Mortality, Incidence, and Survival in the United States, 1950–2014: Over Six Decades of Changing Patterns and Widening Inequalities. J. Environ. Public Health 2017, 2017, 2819372. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.M. On the Fourteenth Query of Thomas Jefferson’s Notes on Virginia. Anglo-Afr. Mag. 1859, 1, 225–238. [Google Scholar]
- Williams, D.R.; Jackson, P.B. Social Sources of Racial Disparities in Health. Health Aff. 2005, 24, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Hicken, M.T.; Kravitz-Wirtz, N.; Durkee, M.; Jackson, J.S. Racial inequalities in health: Framing future research. Soc. Sci. Med. 2018, 199, 11–18. [Google Scholar] [CrossRef]
- Kawachi, I.; Daniels, N.; Robinson, D.E. Health Disparities by Race and Class: Why Both Matter. Health Aff. 2005, 24, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Collins, C. Us Socioeconomic and Racial Differences in Health: Patterns and Explanations. Annu. Rev. Sociol. 1995, 21, 349–386. [Google Scholar] [CrossRef]
- Kent, M.M. Immigration and America’s Black Population. Popul. Bull. 2007, 62, 5–17. [Google Scholar]
- Tamir, C. The Growing Diversity of Black America; Pew Research Center: Washington, DC, USA, 2021. [Google Scholar]
- Arthur, C.M.; Katkin, E.S. Making a Case for the Examination of Ethnicity of Blacks in United States Health Research. J. Health Care Poor Underserved 2006, 17, 25–36. [Google Scholar] [CrossRef]
- Davis, R.A. Black Ethnicity: A Case for Conceptual and Methodological Clarity. West. J. Black Stud. 1992, 16, 147–151. [Google Scholar]
- Hamilton, T.G.; Hummer, R.A. Immigration and the health of U.S. black adults: Does country of origin matter? Soc. Sci. Med. 2011, 73, 1551–1560. [Google Scholar] [CrossRef] [PubMed]
- Jackson, J.; Hamilton, T.; Ifatunji, M.A.; Lacey, K.; Lee, H.; Rafferty, J. Using Analytic Domains within the Black Population to Understand Disparities in Population Health; Volume Princeton; Robert Wood Johnson Foundation and Policy Link: Princeton, NJ, USA, 2018. [Google Scholar]
- Jackson, S.J.; Torres, M.; Caldwell, C.H.; Neighbors, H.W.; Nesse, R.M.; Taylor, R.J.; Trierweiler, S.J.; Williams, D.R. The National Survey of American Life: A Study of Racial, Ethnic and Cultural Influences on Mental Disorders and Mental Health. Int. J. Methods Psychiatr. Res. 2004, 13, 196–207. [Google Scholar] [CrossRef] [PubMed]
- Read, J.G.; Emerson, M.O. Racial Context, Black Immigration and the U.S. Black/White Health Disparity. Soc. Forces 2005, 84, 181–1999. [Google Scholar] [CrossRef]
- Hummer, R.A.; Biegler, M.; de Turk, P.B.; Forbes, D.; Frisbie, W.P.; Hong, Y.; Pullum, S.G. Race/Ethnicity, Nativity, and Infant Mortality in the United States. Soc. Forces 1999, 77, 1083–1117. [Google Scholar] [CrossRef]
- Singh, G.K.; Siahpush, M.; Liu, L.; Allender, M. Racial/ethnic, nativity, and sociodemographic disparities in maternal hypertension in the United States, 2014-2015. Int. J. Hypertens. 2018, 2018, 7897189. [Google Scholar] [CrossRef]
- Singh, G.K.; Miller, B.A. Health, Life Expectancy, and Mortality Patterns Among Immigrant Populations in the United States. Can. J. Public Health 2004, 95, 14–21. [Google Scholar] [CrossRef]
- Singh, G.K.; Rodriguez-Lainz, A.; Kogan, M.D. Immigrant Health Inequalities in the United States: Use of Eight Major National Data Systems. Sci. World J. 2013, 2013, 1–21. [Google Scholar] [CrossRef]
- Singh, G.K.; Hiatt, R.A. Trends and Disparities in Socioeconomic and Behavioural Characteristics, Life Expectancy, and Cause-Specific Mortality of Native-Born and Foreign-Born Populations in the United States, 1979–2003. Int. J. Epidemiol. 2006, 35, 903–919. [Google Scholar] [CrossRef]
- Sowell, T. Three Black Histories. In Essays and Data on American Ethnic Groups; Sowell, T., Collin, L.D., Eds.; Urban Institute: Washington, DC, USA, 1978; pp. 7–64. [Google Scholar]
- Waters, M.C. Black Identities: West Indian Immigrant Dreams and American Realities; Harvard University Press: Cambridge, MA, UK, 1999. [Google Scholar]
- Davis, F.J. Who Is Black? One Nation’s Definition; Pennsylvania State University: University Park, PA, USA, 1991. [Google Scholar]
- Reid, I.D.A. Negro Immigration to the United States. Soc. Forces 1938, 16, 411–417. [Google Scholar] [CrossRef]
- TallBear, K. Genomic articulations of indigeneity. Soc. Stud. Sci. 2013, 43, 509–533. [Google Scholar] [CrossRef]
- Roth, W. Race Migrations: Latinos and the Cultural Transformation of Race; Stanford University Press: Stanford, CA, USA, 2012. [Google Scholar]
- Grosfoguel, R. Colonial Subjects: Puerto Ricans in a Global Perspective; University of California Press: Los Angeles, CA, USA, 2003. [Google Scholar]
- Aranda, E.M. Emotional Bridges to Puerto Rico: Migration, Return Migration, and the Struggles of Incorporation; Rowman & Littlefield Publishers: Lanham, MD, USA, 2006. [Google Scholar]
- Conley, D.; Fletcher, J. The Genome Factor: What the Social Genomics Revolution Reveals About Ourselves, Our History, and the Future; Princeton University Press: Princeton, NJ, USA, 2017. [Google Scholar]
- Bryce-Laporte, R.S. Black Immigrants: The Experience of Invisibility and Inequality. J. Black Stud. 1972, 3, 29–56. [Google Scholar] [CrossRef]
- Bryce-Laporte, R.S. Black Immigrants. In Through Different Eyes: Black and White Perspectives on American Race Relations; Rose, P.I., Rothman, S., Wilson, W.J., Eds.; Oxford University Press: New York, NY, USA, 1973; pp. 44–61. [Google Scholar]
- Ifatunji, M.A. A Test of the Afro Caribbean Model Minority Hypothesis: Exploring the Role of Cultural Attributes in Labor Market Disparities between African Americans and Afro Caribbeans. Du Bois Rev. Soc. Sci. Res. Race 2016, 31, 109–138. [Google Scholar] [CrossRef]
- Pierre, J. Black Immigrants in the United States and the “Cultural Narratives” of Ethnicity. Identities 2004, 11, 141–170. [Google Scholar] [CrossRef]
- Rogers, R. Afro-Caribbean Immigrants and the Politics of Incorporation: Ethnicity, Exception or Exit; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2006. [Google Scholar]
- Taylor, J.Y.; Sun, Y.V.; de Mendoza, V.B.; Ifatunji, M.A.; Rafferty, J.; Fox, E.R.; Musani, S.K.; Sims, M.; Jackson, J.S. The Combined Effects of Genetic Risk and Perceived Discrimination on Blood Pressure among African Americans in the Jackson Heart Study. Medicine 2017, 96, e8369. [Google Scholar] [CrossRef] [PubMed]
- Tsai, H.-J.; Surkan, P.J.; Yu, S.M.; Caruso, D.; Hong, X.; Bartell, T.R.; Wahl, A.D.; Sampankanpanich, C.; Reily, A.; Zuckerman, B.S.; et al. Differential effects of stress and African ancestry on preterm birth and related traits among US born and immigrant Black mothers. Medicine 2017, 96, e5899. [Google Scholar] [CrossRef] [PubMed]
- Reyburn. Remarks Concerning Some of the Diseases Prevailing among the Freedpeople in the District of Columbia (Bureau Refugees, Freedmen, and Abandoned Lands). Am. J. Med. Sci. 1866, 51, 364. [Google Scholar] [CrossRef]
- Reid, I.D.A. The Negro Immigrant, His Background, Characteristics and Social Adjustment; Arno Press: New York, NY, USA, 1939. [Google Scholar]
- Bennett, P.R.; Lutz, A. How African American Is the Net Black Advantage? Differences in College Attendance among Immigrant Blacks, Native Blacks, and Whites. Sociol. Educ. 2009, 82, 70–99. [Google Scholar] [CrossRef]
- Massey, D.S.; Mooney, M.; Torres, K.C.; Charles, C.Z. Black Immigrants and Black Natives Attending Selective Colleges and Universities in the United States. Am. J. Educ. 2007, 113, 243–271. [Google Scholar] [CrossRef]
- Hamilton, T.G.; Easley, J.A.; Dixon, A.R. Black Immigration, Occupational Niches, and Earnings Disparities between Us-Born and Foreign-Born Blacks in the United States. Russell Sage Found. J. Soc. Sci. 2018, 4, 60–77. [Google Scholar]
- Hamilton, T.G. Selection, Language Heritage, and the Earnings Trajectories of Black Immigrants in the United States. Demography 2014, 51, 975–1002. [Google Scholar] [CrossRef] [PubMed]
- Model, S. West Indian Immigrants: A Black Success Story? Russell Sage Foundation: New York, NY, USA, 2008. [Google Scholar]
- Logan, J.R.; Zhang, W.; Alba, R.D. Immigrant Enclaves and Ethnic Communities in New York and Los Angeles. Am. Sociol. Rev. 2002, 67, 299–322. [Google Scholar] [CrossRef]
- Scopilliti, M.; Iceland, J. Residential Patterns of Black Immigrants and Native-Born Blacks in the United States. Soc. Sci. Q. 2008, 89, 551–572. [Google Scholar] [CrossRef]
- Bonilla-Silva, E. Rethinking Racism: Toward a Structural Interpretation. Am. Sociol. Rev. 1997, 62, 465–480. [Google Scholar] [CrossRef]
- Bashi Bobb, V.; Clarke, A. Experiencing Success: Structuring the Perception of Opportunities for West Indians. In Islands in the City: West Indian Migration to New York; Berkeley, N.F., Ed.; University of California Press: Berkeley, CA, USA; Los Angeles, CA, USA, 2001; pp. 216–236. [Google Scholar]
- Domínguez, V.R. From Neighbor to Stranger: The Dilemma of Caribbean Peoples in the U.S.; Antilles Research Program: New Haven, CT, USA, 1975. [Google Scholar]
- Foner, N.; Napoli, R. Jamaican and Black-American Migrant Farm Workers: A Comparative Analysis. Soc. Probl. 1978, 25, 491–503. [Google Scholar] [CrossRef]
- Greer, C.M. Black Ethnics: Race, Immigration and the Pursuit of the American Dream; Oxford University Press: New York, NY, USA, 2013. [Google Scholar]
- Ifatunji, M.A. White Managers, Ethnoracism and Black Ethnic Labor Market Disparities. Sociol. Perspect. 2021, 65, 437–460. [Google Scholar] [CrossRef]
- Patterson, O. The Culture of Caution: The Caribbean Roots of Powell’s Decision. New Repub. 1995, 27, 22–26. [Google Scholar]
- Vickerman, M. Crosscurrents: West Indian Immigrants and Race; Oxford University Press: New York, NY, USA, 1999. [Google Scholar]
- Dressler, W.W.; Oths, K.S.; Gravlee, C.C. Race and ethnicity in public health research: Models to explain health disparities. Annu. Rev. Anthropol 2005, 34, 231–252. [Google Scholar] [CrossRef]
- Krieger, N. Embodying Inequality: A Review of Concepts, Measures and Methods for Studying Health Consequences of Discrimiation. Int. J. Health Serv. 1999, 29, 295–352. [Google Scholar] [CrossRef]
- King, G.; Polednak, A.P.; Bendel, R.; Hovey, D. Cigarette Smoking among Native and Foreign-Born African Americans. Ann. Epidemiol. 1999, 9, 236–244. [Google Scholar] [CrossRef]
- Lucas, J.W.; Barr-Anderson, D.J.; Kington, R.S. Health Status, Health Insurance, and Health Care Utilization Patterns of Immigrant Black Men. Am. J. Public Health 2003, 93, 1740–1747. [Google Scholar] [CrossRef] [PubMed]
- Elo, I.T.; Culhane, J.F. Variations in Health and Health Behaviors by Nativity among Pregnant Black Women in Philadelphia. Am. J. Public Health 2010, 100, 2185–2192. [Google Scholar] [CrossRef] [PubMed]
- Lancaster, K.J.; Watts, S.O.; Dixon, L.B. Dietary Intake and Risk of Coronary Heart Disease Differ among Ethnic Subgroups of Black Americans. J. Nutr. 2006, 136, 446–451. [Google Scholar] [CrossRef]
- Link, B.G.; Phelan, J. Social Conditions as Fundamental Causes of Disease. J. Health Soc. Behav. 1995, 35, 80–94. [Google Scholar] [CrossRef]
- Ifatunji, M.A.; Mouw, T. Black Nativity Matters: Relative Earnings Growth Trajectories among African Americans and Black Immigrants; American Sociological Association: Philadelphia, PA, USA, 2018. [Google Scholar]
- Villarreal, A.; Tamborini, C.R. Immigrants’ Economic Assimilation: Evidence from Longitudinal Earnings Records. Am. Sociol. Rev. 2018, 83, 686–715. [Google Scholar] [CrossRef]
- Logan, J.R. Who Are the Other African Americans? Contemporary African and Caribbean Immigrants in the United States. In The Other African Americans: Contemporary African and Caribbean Immigrants in the United States; Shaw-Taylor, Y., Lanham, S.A.T., Eds.; Rowman & Littlefield Publishers, Inc.: Boulder, NY, USA; Toronto, ON, Canada; Plymouth, UK, 2007; pp. 49–68. [Google Scholar]
- Deaux, K.; Bikmen, N.; Gilkes, A.; Ventuneac, A.; Joseph, Y.; Payne, Y.A.; Steele, C.M. Becoming American: Stereotype Threat Effects in Afro-Caribbean Immigrant Groups. Soc. Psychol. Q. 2007, 70, 384–404. [Google Scholar] [CrossRef]
- Rogers, R. Black Like Who?: Afro-Caribbean Immigrants, African Americans and the Politics of Group Identity. In Islands in the City: West Indian Migration to New York; Berkeley, N.F., Ed.; University of California Press: Los Angeles, CA, USA, 2001; pp. 163–92. [Google Scholar]
- Elo, I.; Mehta, N.; Huang, C. Health of Native-Born and Foreign-Born Black Residents in the United States: Evidence from the 2000 Census of Population and the National Health Interview Survey; PARC Working Paper Series; WPS 08–04; University of Pennsylvania: Philadelphia, PA, USA, 2008. [Google Scholar]
- Howard, D.L.; Marshall, S.S.; Kaufman, J.S.; Savitz, D.A. Variations in Low Birth Weight and Preterm Delivery Among Blacks in Relation to Ancestry and Nativity: New York City, 1998–2002. Pediatrics 2006, 118, e1399–e1405. [Google Scholar] [CrossRef]
- Cooper, R.; David, R. The Biological Concept of Race and Its Application to Public Health and Epidemiology. J. Health Politics Policy Law 1986, 11, 97–116. [Google Scholar] [CrossRef]
- Fujimura, J.H.; Rajagopalan, R. Different Differences: The Use of ‘Genetic Ancestry’ Versus Race in Biomedical Human Genetic Research. Soc. Stud. Sci. 2011, 41, 5–30. [Google Scholar] [CrossRef]
- Fujimura, J.H.; Bolnick, D.A.; Rajagopalan, R.; Kaufman, J.S.; Lewontin, R.C.; Duster, T.; Ossorio, P.; Marks, J. Clines without Classes: How to Make Sense of Human Variation. Sociol. Theory 2014, 32, 208–227. [Google Scholar] [CrossRef]
- Yudell, M.; Roberts, D.; DeSalle, R.; Tishkoff, S. Taking Race out of Human Genetics. Science 2016, 351, 564–565. [Google Scholar] [CrossRef] [PubMed]
- Poston, W.C.; Pavlik, V.; Hyman, D.; Ogbonnaya, K.; Hanis, C.; Haddock, C.; Hyder, M.; Foreyt, J. Genetic bottlenecks, perceived racism, and hypertension risk among African Americans and first-generation African immigrants. J. Hum. Hypertens. 2001, 15, 341–351. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Du Bois, W.E.B. The Conservation of Races. In The American Negro Academy Occasional Papers 2; Arno Press: New York, NY, USA, 1897. [Google Scholar]
- Allis, C.D.; Caparros, Ma.; Jenuwein, T.; Reinberg, D. Epigenetics, 2nd ed.; Cold Spring Harbor Laboratory Press: New York, NY, USA, 2015. [Google Scholar]
- Mohatt, N.V.; Thompson, A.B.; Thai, N.D.; Tebes, J.K. Historical trauma as public narrative: A conceptual review of how history impacts present-day health. Soc. Sci. Med. 2014, 106, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Sotero, M. A Conceptual Model of Historical Trauma: Implications for Public Health Practice and Research. J. Health Disparities Res. Pract. 2006, 1, 93–108. [Google Scholar]
- Jackson, J.S.; Neighbors, H.W.; Nesse, R.M.; Trierweiler, S.J.; Torres, M. Methodological Innovations in the National Survey of American Life. Int. J. Methods Psychiatr. Res. 2004, 13, 289–298. [Google Scholar] [CrossRef]
- Cohen, C.I.; Berment, F.; Magai, C. A Comparison of Us-Born African-American and African-Caribbean Psychiatric Outpatients. J. Natl. Med. Assoc. 1997, 89, 117. [Google Scholar]
- Miranda, J.; Siddique, J.; Belin, T.R.; Kohn-Wood, L.P. Depression Prevalence in Disadvantaged Young Black Women. Soc. Psychiatry Psychiatr. Epidemiol. 2005, 40, 253–258. [Google Scholar] [CrossRef]
- Joe, S.; Baser, R.E.; Breeden, G.; Neighbors, H.W.; Jackson, J.S. Prevalence of and Risk Factors for Lifetime Suicide Attempts among Blacks in the United States. JAMA 2006, 296, 112–123. [Google Scholar] [CrossRef]
- Jackson, J.S.; Govia, I.O.; Forsythe-Brown, I. Age Cohort, Ancestry, and Immigrant Generation Influences in Family Relations and Psychological Well-Being among Black Caribbean Family Members. J. Soc. Issues 2007, 63, 729–743. [Google Scholar] [CrossRef]
- Williams, D.R.; Gonzalez, H.M.; Neighbors, H.; Nesse, R.; Abelson, J.M.; Sweetman, J.; Jackson, J.S. Prevalence and Distribution of Major Depressive Disorder in African Americans, Caribbean Blacks, and Non-Hispanic Whites: Results from the National Survey of American Life. Arch. Gen. Psychiatry 2007, 64, 305–315. [Google Scholar] [CrossRef]
- Williams, D.R.; Haile, R.; González, H.M.; Neighbors, H. The Mental Health of Black Caribbean Immigrants: Results from the Survey of American Life. Am. J. Public Health 2007, 97, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.Y.; Caldwell, C.H.; Baser, R.E.; Faison, N.; Jackson, J.S. Prevalence of eating disorders among Blacks in the National Survey of American Life. Int. J. Eat. Disord. 2007, 40, S10–S14. [Google Scholar] [CrossRef] [PubMed]
- Himle, J.A.; Muroff, J.R.; Taylor, R.J.; Baser, R.E.; Abelson, J.M.; Hanna, G.; Abelson, J.L.; Jackson, J.S. Obsessive-compulsive disorder among African Americans and blacks of Caribbean descent: Results from the national survey of American life. Depress. Anxiety 2008, 25, 993–1005. [Google Scholar] [CrossRef]
- Himle, J.A.; Baser, R.E.; Taylor, R.J.; Campbell, R.D.; Jackson, J.S. Anxiety disorders among African Americans, blacks of Caribbean descent, and non-Hispanic whites in the United States. J. Anxiety Disord. 2009, 23, 578–590. [Google Scholar] [CrossRef]
- Lincoln, K.D.; Taylor, R.J.; Chae, D.H.; Chatters, L.M. Demographic Correlates of Psychological Well-Being and Distress Among Older African Americans and Caribbean Black Adults. Best Pract. Ment. Health 2010, 6, 103–126. [Google Scholar]
- Boyd, R.C.; Joe, S.; Michalopoulos, L.; Davis, E.; Jackson, J.S. Prevalence of Mood Disorders and Service Use among Us Mothers by Race and Ethnicity: Results from the National Survey of American Life. J. Clin. Psychiatry 2011, 72, 15442. [Google Scholar] [CrossRef] [PubMed]
- Soto, J.A.; Dawson-Andoh, N.A.; BeLue, R. The Relationship between Perceived Discrimination and Generalized Anxiety Disorder among African Americans, Afro Caribbeans, and Non-Hispanic Whites. J. Anxiety Disord. 2011, 25, 258–265. [Google Scholar] [CrossRef]
- Taylor, R.J.; Chatters, L.M.; Joe, S. Religious involvement and suicidal behavior among African Americans and Black Caribbeans. J. Nerv. Ment. Dis. 2011, 199, 478. [Google Scholar] [CrossRef]
- Aranda, M.P.; Chae, D.H.; Lincoln, K.D.; Taylor, R.J.; Woodward, A.T.; Chatters, L.M. Demographic correlates of DSM-IV major depressive disorder among older African Americans, Black Caribbeans, and non-Hispanic Whites: Results from the National Survey of American Life. Int. J. Geriatr. Psychiatry 2012, 27, 940–947. [Google Scholar] [CrossRef]
- Doyle, O.; Joe, S.; Caldwell, C.H. Ethnic Differences in Mental Illness and Mental Health Service Use among Black Fathers. Am. J. Public Health 2012, 102, S222–S231. [Google Scholar] [CrossRef]
- Goosby, B.J.; Caldwell, C.H.; Bellatorre, A.; Jackson, J.S. Ethnic Differences in Family Stress Processes Among African-Americans and Black Caribbeans. J. Afr. Am. Stud. 2012, 16, 406–422. [Google Scholar] [CrossRef] [PubMed]
- Ida, A.K.; Christie-Mizell, C.A. Racial group identity, psychosocial resources, and depressive symptoms: Exploring ethnic heterogeneity among black Americans. Sociol. Focus 2012, 45, 41–62. [Google Scholar] [CrossRef]
- Lincoln, K.D.; Chae, D.H. Emotional Support, Negative Interaction and Major Depressive Disorder among African Americans and Caribbean Blacks: Findings from the National Survey of American Life. Soc. Psychiatry Psychiatr. Epidemiol. 2012, 47, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Woodward, A.T.; Taylor, R.J.; Bullard, K.M.; Aranda, M.P.; Lincoln, K.D.; Chatters, L.M. Prevalence of lifetime DSM-IV affective disorders among older African Americans, Black Caribbeans, Latinos, Asians and Non-Hispanic White people. Int. J. Geriatr. Psychiatry 2012, 27, 816–827. [Google Scholar] [CrossRef]
- Assari, S.; Lankarani, M.M.; Lankarani, R.M. Ethnicity Modifies the Additive Effects of Anxiety and Drug Use Disorders on Suicidal Ideation among Black Adults in the United States. Int. J. Prev. Med. 2013, 4, 1251. [Google Scholar]
- Gibbs, T.A.; Okuda, M.; Oquendo, M.A.; Lawson, W.B.; Wang, S.; Thomas, Y.F.; Blanco, C. Mental Health of African Americans and Caribbean Blacks in the United States: Results from the National Epidemiological Survey on Alcohol and Related Conditions. Am. J. Public Health 2013, 103, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Henning-Smith, C.; Shippee, T.P.; McAlpine, D.; Hardeman, R.; Farah, F. Stigma, Discrimination, or Symptomatology Differences in Self-Reported Mental Health Between US-Born and Somalia-Born Black Americans. Am. J. Public Health 2013, 103, 861–867. [Google Scholar] [CrossRef]
- Levine, D.S.; Himle, J.A.; Taylor, R.J.; Abelson, J.M.; Matusko, N.; Muroff, J.; Jackson, J. Panic Disorder among African Americans, Caribbean Blacks and Non-Hispanic Whites. Soc. Psychiatry Psychiatr. Epidemiol. 2013, 48, 711–723. [Google Scholar] [CrossRef]
- Marshall, G.L.; Hooyman, N.R.; Hill, K.G.; Rue, T.C. Association of socio-demographic factors and parental education with depressive symptoms among older African Americans and Caribbean Blacks. Aging Ment. Health 2013, 17, 732–737. [Google Scholar] [CrossRef]
- Woodward, A.T.; Taylor, R.J.; Abelson, J.M.; Matusko, N. Major depressive disorder among older african americans, caribbean blacks, and non-hispanic whites: Secondary analysis of the national survey of american life. Depress. Anxiety 2013, 30, 589–597. [Google Scholar] [CrossRef]
- Levine, D.S.; Himle, J.A.; Abelson, J.M.; Matusko, N.; Dhawan, N.; Taylor, R.J. Discrimination and Social Anxiety Disorder among African-Americans, Caribbean Blacks, and Non-Hispanic Whites. J. Nerv. Ment. Dis. 2014, 202, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Brewton-Tiayon, S.; Watkins, D.C.; Matusko, N.; Jackson, J.S. Depression Among Blacks During Late Life: Examining Within-Group Variations. In Prevention of Late-Life Depression; Humana Press: Cham, Switzerland, 2015. [Google Scholar]
- Lankarani, M.M.; Assari, S. Association between number of comorbid medical conditions and depression among individuals with diabetes; race and ethnic variations. J. Diabetes Metab. Disord. 2015, 14, 56. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.J.; Chae, D.H.; Lincoln, K.D.; Chatters, L.M. Extended family and friendship support networks are both protective and risk factors for major depressive disorder, and depressive symptoms among African Americans and Black Caribbeans. J. Nerv. Ment. Dis. 2015, 203, 132. [Google Scholar] [CrossRef]
- Assari, S.; Dejman, M.; Neighbors, H.W. Ethnic Differences in Separate and Additive Effects of Anxiety and Depression on Self-Rated Mental Health among Blacks. J. Racial Ethn. Health Disparities 2016, 3, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Mereish, E.H.; N’Cho, H.S.; Green, C.E.; Jernigan, M.M.; Helms, J.E. Discrimination and Depressive Symptoms Among Black American Men: Moderated-Mediation Effects of Ethnicity and Self-Esteem. Behav. Med. 2016, 42, 190–196. [Google Scholar] [CrossRef]
- Molina, K.M.; James, D. Discrimination, internalized racism, and depression: A comparative study of African American and Afro-Caribbean adults in the US. Group Processes Intergroup Relat. 2016, 19, 439–461. [Google Scholar] [CrossRef] [PubMed]
- Blostein, F.; Assari, S.; Caldwell, C.H. Gender and ethnic differences in the association between body image dissatisfaction and binge eating disorder among Blacks. J. Racial Ethn. Health Disparities 2017, 4, 529–538. [Google Scholar] [CrossRef]
- Mouzon, D.M.; McLean, J.S. Internalized racism and mental health among African-Americans, US-born Caribbean Blacks, and foreign-born Caribbean Blacks. Ethn. Health 2017, 22, 36–48. [Google Scholar] [CrossRef]
- Moon, H.; Badana, A.N.; Hwang, S.Y.; Sears, J.S.; Haley, W.E. Dementia prevalence in older adults: Variation by race/ethnicity and immigrant status. Am. J. Geriatr. Psychiatry 2019, 27, 241–250. [Google Scholar] [CrossRef]
- Erving, C.L.; Hills, O. Neighborhood social integration and psychological well-being among African Americans and Afro-Caribbeans. Race Soc. Probl. 2019, 11, 133–148. [Google Scholar] [CrossRef]
- Ikonte, C.O.; Prigmore, H.L.; Dawson, A.Z.; Egede, L.E. Trends in prevalence of depression and serious psychological distress in United States immigrant and non-immigrant populations, 2010–2016. J. Affect. Disord. 2020, 274, 719–725. [Google Scholar] [CrossRef] [PubMed]
- Erving, C.L.; Smith, M.V. Disrupting monolithic thinking about Black women and their mental health: Does stress exposure explain intersectional ethnic, nativity, and socioeconomic differences? Soc. Probl. 2021. [Google Scholar] [CrossRef]
- Cabral, H.; Fried, L.E.; Levenson, S.; Amaro, H.; Zuckerman, B. Foreign-Born and Us-Born Black Women: Differences in Health Behaviors and Birth Outcomes. Am. J. Public Health 1990, 80, 70–72. [Google Scholar] [CrossRef]
- Friedman, D.J.; Cohen, B.B.; Mahan, C.M.; Lederman, R.I.; Vezina, R.J.; Dunn, V.H. Maternal ethnicity and birthweight among blacks. Ethn. Dis. 1993, 3, 255–269. [Google Scholar] [PubMed]
- Wasse, H.; Holt, V.L.; Daling, J.R. Pregnancy risk factors and birth outcomes in Washington State: A comparison of Ethiopian-born and US-born women. Am. J. Public Health 1994, 84, 1505–1507. [Google Scholar] [CrossRef] [PubMed]
- David, R.J.; Collins, J.W. Differing Birth Weight among Infants of Us-Born Blacks, African-Born Blacks, and Us-Born Whites. N. Engl. J. Med. 1997, 337, 1209–1214. [Google Scholar] [CrossRef]
- Fang, J.; Madhavan, S.; Alderman, M.H. Low birth weight: Race and maternal nativity—Impact of community income. Pediatrics 1999, 103, e5. [Google Scholar] [CrossRef]
- Pallotto, E.K.; Collins, J.J.W.; David, R.J. Enigma of Maternal Race and Infant Birth Welght: A Population-based Study of US-born Blac and Caribbean-born Black Women. Am. J. Epidemiol. 2000, 151, 1080–1085. [Google Scholar] [CrossRef]
- Collins, J.W.; Wu, S.-Y.; David, R.J. Differing Intergenerational Birth Weights among the Descendants of Us-Born and Foreign-Born Whites and African Americans in Illinois. Am. J. Epidemiol. 2002, 155, 210–216. [Google Scholar] [CrossRef]
- Rosenberg, K.D.; Desai, R.A.; Kan, J. Why do foreign-born blacks have lower infant mortality than native-born blacks? New directions in African-American infant mortality research. J. Natl. Med Assoc. 2002, 94, 770–778. [Google Scholar]
- Acevedo-Garcia, D.; Soobader, M.-J.; Berkman, L.F. The Differential Effect of Foreign-Born Status on Low Birth Weight by Race/Ethnicity and Education. Pediatrics 2005, 115, e20–e30. [Google Scholar] [CrossRef] [PubMed]
- Grady, S.C.; McLafferty, S. Segregation, Nativity, and Health: Reproductive Health Inequalities for Immigrant and Native-Born Black Women in New York City1. Urban Geogr. 2007, 28, 377–397. [Google Scholar] [CrossRef]
- Dominguez, T.P.; Strong, E.F.; Krieger, N.; Gillman, M.W.; Rich-Edwards, J.W. Differences in the Self-Reported Racism Experiences of Us-Born and Foreign-Born Black Pregnant Women. Soc. Sci. Med. 2009, 69, 258–265. [Google Scholar] [CrossRef]
- Mason, S.M.; Kaufman, J.S.; Emch, M.E.; Hogan, V.K.; Savitz, D.A. Ethnic Density and Preterm Birth in African-, Caribbean-, and US-Born Non-Hispanic Black Populations in New York City. Am. J. Epidemiol. 2010, 172, 800–808. [Google Scholar] [CrossRef] [PubMed]
- Bloch, J.R. Using Geographical Information Systems to Explore Disparities in Preterm Birth Rates among Foreign-Born and Us-Born Black Mothers. J. Obstet. Gynecol. Neonatal Nurs. 2011, 40, 544–554. [Google Scholar] [CrossRef] [PubMed]
- Elo, I.T.; Vang, Z.; Culhane, J.F. Variation in Birth Outcomes by Mother’s Country of Birth among Non-Hispanic Black Women in the United States. Matern. Child Health J. 2014, 18, 2371–2381. [Google Scholar] [CrossRef]
- Hendi, A.S.; Mehta, N.K.; Elo, I.T. Health Among Black Children by Maternal and Child Nativity. Am. J. Public Health 2015, 105, 703–710. [Google Scholar] [CrossRef]
- DeSisto, C.L.; Hirai, A.H.; Collins Jr, J.W.; Rankin, K.M. Deconstructing a disparity: Explaining excess preterm birth among US-born black women. Ann. Epidemiol. 2018, 28, 225–230. [Google Scholar] [CrossRef]
- Oliver, E.A.; Klebanoff, M.; Yossef-Salameh, L.; Oza-Frank, R.; Moosavinasab, S.; Reagan, P.; Buhimschi, I.A. Preterm birth and gestational length in four race–nativity groups, including Somali Americans. Obstet. Gynecol. 2018, 131, 281–289. [Google Scholar] [CrossRef]
- 135. Kirby, R.S.; Mai, C.T.; Wingate, M.S.; Janevic, T.; Copeland, G.E.; Flood, T.J.; Isenburg, J.; Canfield, M.A. Prevalence of selected birth defects by maternal nativity status, United States, 1999–2007. Birth Defects Res. 2019, 111, 630–639. [Google Scholar] [CrossRef]
- Elsayed, A.; Amutah-Onukagha, N.N.; Navin, L.; Gittens-Williams, L.; Janevic, T. Impact of immigration and duration of residence in US on length of gestation among black women in Newark, New Jersey. J. Immigr. Minority Health 2019, 21, 1095–1101. [Google Scholar] [CrossRef]
- Singh, G.K.; DiBari, J.N. Marked disparities in pre-pregnancy obesity and overweight prevalence among US women by race/ethnicity, nativity/immigrant status, and sociodemographic characteristics, 2012–2014. J. Obes. 2019, 2019, 2419263. [Google Scholar] [CrossRef] [PubMed]
- Scott, K.A.; Chambers, B.D.; Baer, R.J.; Ryckman, K.K.; McLemore, M.R.; Jelliffe-Pawlowski, L.L. Preterm birth and nativity among Black women with gestational diabetes in California, 2013–2017: A population-based retrospective cohort study. BMC Pregnancy Childbirth 2020, 20, 593. [Google Scholar] [CrossRef] [PubMed]
- Araneta, M.R.G.; Baer, R.J.; Muglia, L.J.; Ryckman, K.K.; Ryu, J.; Sidelinger, D.E.; Chambers, C.D. Health advantages and disparities in preterm birth among immigrants despite disparate sociodemographic, behavioral, and maternal risk factors in San Diego, California. Matern. Child Health J. 2020, 24, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Hoyt, A.T.; Ramadhani, T.; Le, M.T.; Shumate, C.J.; Canfield, M.A.; Scheuerle, A.E.; National Birth Defects Prevention Study. Acculturation and selected birth defects among non-Hispanic Blacks in a population-based case–control study. Birth Defects Res. 2020, 112, 535–554. [Google Scholar] [CrossRef] [PubMed]
- Boakye, E.; Kwapong, Y.A.; Obisesan, O.; Ogunwole, S.M.; Hays, A.G.; Nasir, K.; Sharma, G. Nativity-related disparities in preeclampsia and cardiovascular disease risk among a racially diverse cohort of US women. JAMA Netw. Open 2021, 4, e2139564. [Google Scholar] [CrossRef]
- Hong, X.; Rosenberg, A.Z.; Zhang, B.; Binns-Roemer, E.; David, V.; Lv, Y.; Winkler, C.A. Joint associations of maternal-fetal APOL1 genotypes and maternal country of origin with preeclampsia risk. Am. J. Kidney Dis. 2021, 77, 879–888. [Google Scholar] [CrossRef]
- McKenzie-Sampson, S.; Baer, R.J.; Blebu, B.E.; Karasek, D.; Oltman, S.P.; Pantell, M.S.; Chambers, B.D. Maternal nativity and risk of adverse perinatal outcomes among Black women residing in California, 2011–2017. J. Perinatol. 2021, 41, 2736–2741. [Google Scholar] [CrossRef]
- Adegoke, T.M.; Pinder, L.F.; Ndiwane, N.; Parker, S.E.; Vragovic, O.; Yarrington, C.D. Inequities in adverse maternal and perinatal outcomes: The effect of maternal race and nativity. Matern. Child Health J. 2022, 26, 823–833. [Google Scholar] [CrossRef]
- Andrasfay, T. Birth Outcomes among Descendants of Foreign-Born and US-Born Women in California: Variation by Race and Ethnicity. J. Immigr. Minority Health 2022, 24, 605–613. [Google Scholar] [CrossRef]
- Green, T.L.; Simuzingili, M.; Bodas, M.; Xue, H. Pregnancy-related weight among immigrant and US-born mothers: The role of nativity, maternal duration of residence, and age at arrival. Women’s Health 2021, 17, 17455065211003692. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Ji, Y.; Hong, X.; Zuckerman, B.; Wang, X.; Surkan, P.J. Effects of Stress and Nativity on Maternal Antenatal Substance Use and Postnatal Mental Disorders. J. Women’s Health 2022, 31, 878–886. [Google Scholar] [CrossRef] [PubMed]
- Blebu, B.E. Neighborhood Context and the Nativity Advantage in Preterm Birth among Black Women in California, USA. J. Urban Health 2021, 98, 801–811. [Google Scholar] [CrossRef] [PubMed]
- Kwapong, Y.A.; Boakye, E.; Obisesan, O.H.; Shah, L.M.; Ogunwole, S.M.; Hays, A.G.; Sharma, G. Nativity-Related Disparities in Preterm Birth and Cardiovascular Risk in a Multiracial US Cohort. Am. J. Prev. Med. 2022, 62, 885–894. [Google Scholar] [CrossRef]
- Minhas, A.S.; Boakye, E.; Obisesan, O.H.; Kwapong, Y.A.; Zakaria, S.; Creanga, A.A.; Sharma, G. The Association of Preterm Birth with Maternal Nativity and Length of Residence Among Non-Hispanic Black Women. CJC Open 2022, 4, 289–298. [Google Scholar] [CrossRef]
- Maiyegun, S.O.; Yusuf, K.K.; Dongarwar, D.; Ibrahimi, S.; Ikedionwu, C.; Salihu, H.M. Risk of Stillbirth Among Foreign-Born Mothers in the United States. J. Immigr. Minority Health 2022, 24, 318–326. [Google Scholar] [CrossRef]
- Egbe, T.I.; Montoya-Williams, D.; Wallis, K.; Passarella, M.; Lorch, S.A. Risk of extreme, moderate, and late preterm birth by maternal race, ethnicity, and nativity. J. Pediatrics 2022, 240, 24–30. [Google Scholar] [CrossRef]
- Shah, L.M.; Kwapong, Y.A.; Boakye, E.; Ogunwole, S.M.; Bennett, W.L.; Blumenthal, R.S.; Sharma, G. Racial Disparities in Prevalence of Gestational Diabetes by Maternal Nativity and Length of US Residence in an Urban Low-Income Population in the United States. CJC Open 2022, 4, 540–550. [Google Scholar] [CrossRef]
- Belanoff, C.; Alade, M.O.; Almeida, J. Preterm Birth Among US and Foreign-Born Non-Hispanic Black Birthing Parents in Massachusetts: Variation by Nativity, Region, and Country of Origin. Matern. Child Health J. 2022, 26, 834–844. [Google Scholar] [CrossRef]
- Noah, A.; Hill, A.V.; Perez-Patron, M.J.; Berenson, A.B.; Comeaux, C.R.; Taylor, B.D. Disparities in Prenatal Sexually Transmitted Infections among a Diverse Population of Foreign-Born and US-Born Women. Reprod. Sci. 2022, 29, 1651–1660. [Google Scholar] [CrossRef]
- Fumo, M.T.; Teeger, S.; Lang, R.M.; Bednarz, J.; Sareli, P.; Murphy, M.B. Diurnal blood pressure variation and cardiac mass in American blacks and whites and South African blacks. Am. J. Hypertension 1992, 5, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Fang, J.; Madhavan, S.; Alderman, M.H. The Association between Birthplace and Mortality from Cardiovascular Causes among Black and White Residents of New York City. N. Engl. J. Med. 1996, 335, 1545–1551. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, J.S.; Durazo-Arvizu, R.A.; Rotimi, C.N.; McGee, D.L.; Cooper, R.S. Obesity and hypertension prevalence in populations of African origin. Epidemiology 1996, 7, 398–405. [Google Scholar] [CrossRef]
- Osei, K.; Schuster, D.P. Effects of Race and Ethnicity on Insulin Sensitivity, Blood Pressure, and Heart Rate in Three Ethnic Populations: Comparative Studies in African-Americans, African Immigrants (Ghanaians), and White Americans Using Ambulatory Blood Pressure Monitoring. Am. J. Hypertens. 1996, 9, 1157–1164. [Google Scholar] [CrossRef]
- Hyman, D.J.; Ogbonnaya, K.; Pavlik, V.N.; Poston, W.S.; Ho, K. Lower Hypertension Prevalence in First-Generation African Immigrants Compared to Us-Born African Americans. Ethn. Dis. 2000, 10, 343–349. [Google Scholar]
- Hicks, L.S.; Fairchild, D.G.; Cook, E.F.; Ayanian, J.Z. Association of region of residence and immigrant status with hypertension, renal failure, cardiovascular disease, and stroke, among African-American participants in the third National Health and Nutrition Examination Survey (NHANES III). Ethn. Dis. 2003, 13, 316–323. [Google Scholar]
- Ryan, A.M.; Gee, G.C.; Laflamme, D.F. The Association between Self-Reported Discrimination, Physical Health and Blood Pressure: Findings from African Americans, Black Immigrants, and Latino Immigrants in New Hampshire. J. Health Care Poor Underserved 2006, 17, 116–132. [Google Scholar] [CrossRef]
- Davis, E.E.; Huffman, F.G. Differences in Coronary Heart Disease Risk Markers among Apparently Healthy Individuals of African Ancestry. J. Natl. Med. Assoc. 2007, 99, 658. [Google Scholar]
- Borrell, L.N.; Crawford, N.D.; Barrington, D.S.; Maglo, K.N. Black/White Disparity in Self-Reported Hypertension: The Role of Nativity Status. J. Health Care Poor Underserved 2008, 19, 1148–1162. [Google Scholar] [CrossRef]
- White, K.; Borrell, L.N.; Wong, D.W.; Galea, S.; Ogedegbe, G.; Glymour, M.M. Racial/Ethnic Residential Segregation and Self-Reported Hypertension Among US- and Foreign-Born Blacks in New York City. Am. J. Hypertens. 2011, 24, 904–910. [Google Scholar] [CrossRef]
- Bamimore, A.; Olafiranye, O.; Demede, M.; Zizi, F.; Browne, R.; Brown, C.; McFarlane, S.I.; Jean-Louis, G. High Prevalence of Hypertension and Other Cardiometabolic Risk Factors in Us-and Caribbean-Born Blacks with Chest Pain Syndromes. Cardiorenal Med. 2012, 2, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Sellers, S.L.; Neighbors, H.W.; Zhang, R.; Jackson, J.S. The impact of goal-striving stress on physical health of white Americans, African Americans, and Caribbean blacks. Ethn. Dis. 2012, 22, 21–28. [Google Scholar]
- Yu, S.S.K.; Ramsey, N.L.M.; Castillo, D.C.; Ricks, M.; Sumner, A.E. Triglyceride-Based Screening Tests Fail to Recognize Cardiometabolic Disease in African Immigrant and African-American Men. Metab. Syndr. Relat. Disord. 2013, 11, 15–20. [Google Scholar] [CrossRef]
- Dagadu, H.E.; Christie-Mizell, C.A. Heart trouble and racial group identity: Exploring ethnic heterogeneity among Black Americans. Race Soc. Probl. 2014, 6, 143–160. [Google Scholar] [CrossRef][Green Version]
- O’Connor, M.Y.; Thoreson, C.K.; Ricks, M.; Courville, A.B.; Thomas, F.; Yao, J.; Katzmarzyk, P.; Sumner, A.E. Worse Cardiometabolic Health in African Immigrant Men than African American Men: Reconsideration of the Healthy Immigrant Effect. Metab. Syndr. Relat. Disord. 2014, 12, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.G.M.; Houser, R.F.; Mattei, J.; Mozaffarian, D.; Lichtenstein, A.H.; Folta, S.C. Hypertension among Us-Born and Foreign-Born Non-Hispanic Blacks: National Health and Nutrition Examination Survey 2003–2014 Data. J. Hypertens. 2017, 35, 2380–2387. [Google Scholar] [CrossRef] [PubMed]
- Cole, H.; Duncan, D.T.; Ogedegbe, G.; Bennett, S.; Ravenell, J. Neighborhood Socioeconomic Disadvantage; Neighborhood Racial Composition; and Hypertension Stage, Awareness, and Treatment among Hypertensive Black Men in New York City: Does Nativity Matter? J. Racial Ethn. Health Disparities 2017, 4, 866–875. [Google Scholar] [CrossRef]
- Commodore-Mensah, Y.; Matthie, N.; Wells, J.; Dunbar, S.B.; Himmelfarb, C.D.; Cooper, L.A.; Chandler, R.D. African Americans, African Immigrants, and Afro-Caribbeans Differ in Social Determinants of Hypertension and Diabetes: Evidence from the National Health Interview Survey. J. Racial Ethn. Health Disparities 2018, 5, 995–1002. [Google Scholar] [CrossRef]
- Cole, H.V.; Reed, H.E.; Tannis, C.; Trinh-Shevrin, C.; Ravenell, J.E. Peer reviewed: Awareness of high blood pressure by nativity among Black men: Implications for interpreting the immigrant health paradox. Prev. Chronic Dis. 2018, 15, E121. [Google Scholar] [CrossRef]
- Fang, J.; Yuan, K.; Gindi, R.M.; Ward, B.W.; Ayala, C.; Loustalot, F. Association of birthplace and coronary heart disease and stroke among US adults: National Health Interview Survey, 2006 to 2014. J. Am. Heart Assoc. 2018, 7, e008153. [Google Scholar] [CrossRef]
- Turkson-Ocran, R.A.N.; Nmezi, N.A.; Botchway, M.O.; Szanton, S.L.; Golden, S.H.; Cooper, L.A.; Commodore-Mensah, Y. Comparison of cardiovascular disease risk factors among African immigrants and African Americans: An analysis of the 2010 to 2016 National Health Interview Surveys. J. Am. Heart Assoc. 2020, 9, e013220. [Google Scholar] [CrossRef]
- Whaley, A.L. Ethnicity, nativity, and the effects of stereotypes on cardiovascular health among people of African ancestry in the United States: Internal versus external sources of racism. Ethn. Health 2020, 27, 1010–1030. [Google Scholar] [CrossRef] [PubMed]
- Doamekpor, L.A.; Gleason, J.L.; Opara, I.; Amutah-Onukagha, N.N. Nativity and Cardiovascular Dysregulation: Evidence from the 2001–2016 National Health and Nutrition Examination Survey. J. Racial Ethn. Health Disparities 2021, 8, 136–146. [Google Scholar] [CrossRef] [PubMed]
- Oza-Frank, R.; Chan, C.; Liu, K.; Burke, G.; Kanaya, A.M. Incidence of Type 2 Diabetes by Place of Birth in the Multi-Ethnic Study of Atherosclerosis (MESA). J. Immigr. Minor. Health 2013, 15, 918–924. [Google Scholar] [CrossRef] [PubMed]
- Ford, N.D.; Venkat Narayan, K.M.; Mehta, N.K. Diabetes among US- and foreign-born blacks in the USA. Ethn. Health 2015, 21, 71–84. [Google Scholar] [CrossRef]
- O’Connor, M.R.; Dobra, A.; Voss, J.; Pihoker, C.; Doorenbos, A. Type 1 Diabetes Among East African Immigrant and Nonimmigrant Black Youth in the U.S. J. Pediatric Nurs. Nurs. Care Child. Fam. 2015, 30, 834–841. [Google Scholar] [CrossRef]
- Harvey, R.D.; Tennial, R.; Banks, K.H. The Development and Validation of a Colorism Scale. J. Black Psychol. 2017, 43, 740–764. [Google Scholar] [CrossRef]
- Horlyck-Romanovsky, M.F.; Wyka, K.; Echeverria, S.E.; Leung, M.M.; Fuster, M.; Huang, T.T.K. Foreign-born blacks experience lower odds of obesity but higher odds of diabetes than US-born blacks in New York City. J. Immigr. Minority Health 2019, 21, 47–55. [Google Scholar] [CrossRef]
- Engelman, M.; Ye, L.Z. The immigrant health differential in the context of racial and ethnic disparities: The case of diabetes. Immigr. Health 2019, 19, 147–171. [Google Scholar]
- Ogunwole, S.M.; Turkson-Ocran, R.A.N.; Boakye, E.; Creanga, A.A.; Wang, X.; Bennett, W.L.; Commodore-Mensah, Y. Disparities in cardiometabolic risk profiles and gestational diabetes mellitus by nativity and acculturation: Findings from 2016–2017 National Health Interview Survey. BMJ Open Diabetes Res. Care 2022, 10, e002329. [Google Scholar] [CrossRef]
- Choi, D.; Narayan, K.V.; Patel, S.A. Disparities in diabetes between US-born and foreign-born population: Using three diabetes indicators. Biodemography Soc. Biol. 2022, 67, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Antecol, H.; Bedard, K. Unhealthy Assimilation: Why Do Immigrants Converge to American Health Status Levels? Demography 2006, 43, 337–360. [Google Scholar] [CrossRef] [PubMed]
- Bennett, G.G.; Wolin, K.Y.; Askew, S.; Fletcher, R.; Emmons, K.M. Immigration and Obesity among Lower Income Blacks. Obesity 2007, 15, 1391–1394. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Vaznaugh, E.V.; Kawachi, I.; Subramanian, S.V.; Sánchez, B.N.; Acevedo-Garcia, D. Differential Effect of Birthplace and Length of Residence on Body Mass Index (Bmi) by Education, Gender and Race/Ethnicity. Soc. Sci. Med. 2008, 67, 1300–1310. [Google Scholar] [CrossRef]
- Barrington, D.S.; Baquero, M.C.; Borrell, L.N.; Crawford, N.D. Racial/Ethnic Disparities in Obesity among Us-Born and Foreign-Born Adults by Sex and Education. Obesity 2010, 18, 422–424. [Google Scholar] [CrossRef]
- Wen, M.; Kowaleski-Jones, L.; Fan, J.X. Ethnic-immigrant Disparities in Total and Abdominal Obesity in the US. Am. J. Health Behav. 2013, 37, 807–818. [Google Scholar] [CrossRef]
- Assari, S. Additive effects of anxiety and depression on body mass index among blacks: Role of ethnicity and gender. Int. Cardiovasc. Res. J. 2014, 8, 44. [Google Scholar]
- Sullivan, S.M.; Brashear, M.M.; Broyles, S.T.; Rung, A.L. Neighborhood environments and obesity among Afro-Caribbean, African American, and Non-Hispanic white adults in the United States: Results from the National Survey of American Life. Prev. Med. 2014, 61, 1–5. [Google Scholar] [CrossRef]
- Mehta, N.K.; Elo, I.T.; Ford, N.D.; Siegel, K.R. Obesity among Us-and Foreign-Born Blacks by Region of Birth. Am. J. Prev. Med. 2015, 49, 269–273. [Google Scholar] [CrossRef]
- Cuevas, A.G.; Ortiz, K.; Ransome, Y. The moderating role of race/ethnicity and nativity in the relationship between perceived discrimination and overweight and obesity: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. BMC Public Health 2019, 19, 1458. [Google Scholar] [CrossRef]
- Fruchter, R.G.; Wright, C.; Habenstreit, B.; Remy, J.C.; Boyce, J.G.; Imperato, P.J. Screening for cervical and breast cancer among Caribbean immigrants. J. Community Health 1985, 10, 121–135. [Google Scholar] [CrossRef] [PubMed]
- Fruchter, R.G.; Remy, J.C.; Burnett, W.S.; Boyce, J.G. Cervical Cancer in Immigrant Caribbean Women. Am. J. Public Health 1986, 76, 797–799. [Google Scholar] [CrossRef] [PubMed]
- Magnus, M. Prostate cancer knowledge among multiethnic black men. J. Natl. Med. Assoc. 2004, 96, 650. [Google Scholar] [PubMed]
- Garbers, S.; Chiasson, M.A. Breast Cancer Screening and Health Behaviors among African American and Caribbean Women in New York City. J. Health Care Poor Underserved 2006, 17, 37–46. [Google Scholar] [CrossRef]
- Bennett, G.G.; Wolin, K.Y.; Okechukwu, C.A.; Arthur, C.M.; Askew, S.; Sorensen, G.; Emmons, K.M. Nativity and Cigarette Smoking among Lower Income Blacks: Results from the Healthy Directions Study. J. Immigr. Minority Health 2008, 10, 305–311. [Google Scholar] [CrossRef][Green Version]
- Taioli, E.; Attong-Rogers, A.; Layne, P.; Roach, V.; Ragin, C. Breast cancer survival in women of African descent living in the US and in the Caribbean: Effect of place of birth. Breast Cancer Res. Treat. 2010, 122, 515–520. [Google Scholar] [CrossRef]
- Odedina, F.T.; Dagne, G.; Larose-Pierre, M.; Scrivens, J.; Emanuel, F.; Adams, A.; Pressey, S.; Odedina, O. Within-Group Differences Between Native-Born and Foreign-Born Black Men on Prostate Cancer Risk Reduction and Early Detection Practices. J. Immigr. Minor. Health 2011, 13, 996–1004. [Google Scholar] [CrossRef]
- Wade, B.; Lariscy, J.T.; Hummer, R.A. Racial/Ethnic and Nativity Patterns of U.S. Adolescent and Young Adult Smoking. Popul. Res. Policy Rev. 2013, 32, 353–371. [Google Scholar] [CrossRef]
- Consedine, N.S.; Tuck, N.L.; Ragin, C.R.; Spencer, B.A. Beyond the Black Box: A Systematic Review of Breast, Prostate, Colorectal, and Cervical Screening among Native and Immigrant African-Descent Caribbean Populations. J. Immigr. Minority Health / Cent. Minority Public Health 2015, 17, 905–924. [Google Scholar] [CrossRef]
- Forney-Gorman, A.; Kozhimannil, K.B. Differences in Cervical Cancer Screening Between African-American Versus African-Born Black Women in the United States. J. Immigr. Minor. Health 2016, 18, 1371–1377. [Google Scholar] [CrossRef]
- Pinheiro, P.S.; Callahan, K.E.; Ragin, C.; Hage, R.W.; Hylton, T.; Kobetz, E.N. Black heterogeneity in cancer mortality: US-Blacks, Haitians, and Jamaicans. Cancer Control 2016, 23, 347–358. [Google Scholar] [CrossRef] [PubMed]
- Ashing, K.T.; Carrington, A.; Ragin, C.; Roach, V. Examining Hpv-and Hpv Vaccine-Related Cognitions and Acceptability among Us-Born and Immigrant Hispanics and Us-Born and Immigrant Non-Hispanic Blacks: A Preliminary Catchment Area Study. Cancer Causes Control 2017, 28, 1341–1347. [Google Scholar] [CrossRef] [PubMed]
- Barreto-Coelho, P.; Cerbon, D.; Schlumbrecht, M.; Parra, C.M.; Hurley, J.; George, S.H. Differences in breast cancer outcomes amongst Black US-born and Caribbean-born immigrants. Breast Cancer Res. Treat. 2019, 178, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Hallowell, B.D.; Endeshaw, M.; McKenna, M.T.; Senkomago, V.; Razzaghi, H.; Saraiya, M. Cervical cancer death rates among US-and foreign-born women: US, 2005–2014. Am. J. Prev. Med. 2019, 56, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Schlumbrecht, M.; Huang, M.; Hurley, J.; George, S. Endometrial cancer outcomes among non-Hispanic US born and Caribbean born black women. Int. J. Gynecol. Cancer 2019, 29. [Google Scholar] [CrossRef]
- Cofie, L.E.; Hirth, J.M.; Berenson, A.B.; Wong, R. Chronic comorbidities and receipt of breast cancer screening in United States and Foreign-Born Women: Data from the national health interview survey. J. Women’s Health 2019, 28, 583–590. [Google Scholar] [CrossRef]
- Bhattacharya, M.; Reiter, P.L.; McRee, A.L. Nativity status and genital HPV infection among adults in the US. Hum. Vaccines Immunother. 2019, 15, 1897–1903. [Google Scholar] [CrossRef] [PubMed]
- Boakye, E.A.; Zeng, W.; Governor, S.; Nagendra, S.; Tobo, B.B.; Simpson, M.C.; Osazuwa-Peters, N. Differences in human papillomavirus (HPV) vaccine uptake by nativity status among men aged 18–34 years. Prev. Med. Rep. 2019, 16, 101010. [Google Scholar] [CrossRef]
- Endeshaw, M.; Hallowell, B.D.; Razzaghi, H.; Senkomago, V.; McKenna, M.T.; Saraiya, M. Trends in liver cancer mortality in the United States: Dual burden among foreign-and US-born persons. Cancer 2019, 125, 726–734. [Google Scholar] [CrossRef]
- Hallowell, B.D.; Endeshaw, M.; McKenna, M.T.; Senkomago, V.; Razzaghi, H.; Saraiya, M. Cancer mortality rates among US and foreign-born individuals: United States 2005–2014. Prev. Med. 2019, 126, 105755. [Google Scholar] [CrossRef]
- Hallowell, B.D.; Endeshaw, M.; Senkomago, V.; Razzaghi, H.; McKenna, M.T.; Saraiya, M. Gastric cancer mortality rates among US and foreign-born persons: United States 2005–2014. Gastric Cancer 2019, 22, 1081–1085. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, P.S.; Medina, H.; Callahan, K.E.; Kwon, D.; Ragin, C.; Sherman, R.; Jemal, A. Cancer mortality among US blacks: Variability between African Americans, Afro-Caribbeans, and Africans. Cancer Epidemiol. 2020, 66, 101709. [Google Scholar] [CrossRef] [PubMed]
- Amuta-Jimenez, A.O.; Smith, G.; Brown, K.K. Patterns and correlates of cervical cancer prevention among Black immigrant and African American women in the USA: The role of ethnicity and culture. J. Cancer Educ. 2020, 37, 798–805. [Google Scholar] [CrossRef] [PubMed]
- Donley, T.; Tshiswaka, D.I.; Blanc, J.; Seixas, A.; Okafor, A.; Mbizo, J. Differences in breast and cervical cancer screening among US women by nativity and family history. Am. J. Prev. Med. 2020, 59, 578–587. [Google Scholar] [CrossRef] [PubMed]
- McRoy, L.; Epané, J.; Ramamonjiarivelo, Z.; Zengul, F.; Weech-Maldonado, R.; Rust, G. Examining the relationship between self-reported lifetime cancer diagnosis and nativity: Findings from the National Health and Nutrition Examination Survey (NHANES) 2011–2018. Cancer Causes Control 2022, 33, 321–329. [Google Scholar] [CrossRef]
- Blackman, E.L.; Ragin, C.; Jones, R.M. Colorectal Cancer Screening Prevalence and Adherence for the Cancer Prevention Project of Philadelphia (CAP3) Participants Who Self-Identify as Black. Front. Oncol. 2021, 11, 690718. [Google Scholar] [CrossRef]
- McElfish, P.A.; Narcisse, M.R.; Felix, H.C.; Cascante, D.C.; Nagarsheth, N.; Teeter, B.; Faramawi, M.F. Race, nativity, and sex disparities in human papillomavirus vaccination among young adults in the USA. J. Racial Ethn. Health Disparities 2021, 8, 1260–1266. [Google Scholar] [CrossRef]
- Pinheiro, P.S.; Medina, H.N.; Koru-Sengul, T.; Qiao, B.; Schymura, M.; Kobetz, E.N.; Schlumbrecht, M.P. Endometrial cancer type 2 incidence and survival disparities within subsets of the US Black population. Front. Oncol. 2021, 11, 699577. [Google Scholar] [CrossRef]
- Llanos, A.A.; Li, J.; Tsui, J.; Gibbons, J.; Pawlish, K.; Nwodili, F.; Stroup, A.M. Variation in Cancer Incidence Rates Among Non-Hispanic Black Individuals Disaggregated by Nativity and Birthplace, 2005-2017: A Population-Based Cancer Registry Analysis. Front. Oncol. 2022, 12, 857548. [Google Scholar] [CrossRef]
- Millender, E.; Dickey, S.L.; Ouma, C.; Bruneau, D.; Wisdom-Chambers, K.; Bagneris, J.R.; Harris, R.M. Addressing Disparities by Evaluating Depression as a Predictor of Prostate Screenings among Black Men in a Community Health Clinic. J. Community Health Nurs. 2022, 39, 25–39. [Google Scholar] [CrossRef]
- Epstein, J.A.; Williams, C.; Botvin, G.J. How Universal Are Social Influences to Drink and Problem Behaviors for Alcohol Use?: A Test Comparing Urban African-American and Caribbean-American Adolescents. Addict. Behav. 2002, 27, 75–86. [Google Scholar] [CrossRef]
- Hunte, H.E.R.; Barry, A.E. Perceived Discrimination and Dsm-Iv–Based Alcohol and Illicit Drug Use Disorders. Am. J. Public Health 2012, 102, e111–e117. [Google Scholar] [CrossRef]
- Lo, C.C.; Howell, R.J.; Cheng, T.C. Problem Drinking by Race and Nativity: What Is Learned from Social Structural and Mental Health-Related Data of US-Born and Immigrant Respondents? Am. J. Addict. 2012, 21, S77–S87. [Google Scholar] [CrossRef] [PubMed]
- Szaflarski, M.; Cubbins, L.A.; Meganathan, K. Anxiety disorders among US immigrants: The role of immigrant background and social-psychological factors. Issues Ment. Health Nurs. 2017, 38, 317–326. [Google Scholar] [CrossRef]
- Broman, C.L.; Neighbors, H.W.; Delva, J.; Torres, M.; Jackson, J.S. Prevalence of Substance Use Disorders among African Americans and Caribbean Blacks in the National Survey of American Life. Am. J. Public Health 2008, 98, 1107–1114. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, S.; Jarrett, S.T.B.; Kelvin, E.A.; Wallace, S.A.; Augenbraun, M.; Hogben, M.; Liddon, N.; McCormack, W.M.; Rubin, S.; Wilson, T.E. HIV and Sexually Transmitted Infection Risk Behaviors and Beliefs Among Black West Indian Immigrants and US-Born Blacks. Am. J. Public Health 2008, 98, 2042–2050. [Google Scholar] [CrossRef] [PubMed]
- Bui, H.N. Racial and Ethnic Differences in the Immigrant Paradox in Substance Use. J. Immigr. Minority Health 2013, 15, 866–881. [Google Scholar] [CrossRef]
- Lacey, K.K.; Mouzon, D.M.; Govia, I.; Matusko, N.; Forsythe-Brown, I.; Abelson, J.M.; Jackson, J.S. Substance Abuse Among Blacks Across the Diaspora. Subst. Use Misuse 2016, 51, 1147–1158. [Google Scholar] [CrossRef]
- Molina, K.M.; Alegría, M.; Chen, C.N. Neighborhood context and substance use disorders: A comparative analysis of racial and ethnic groups in the United States. Drug Alcohol Depend. 2012, 125, S35–S43. [Google Scholar] [CrossRef]
- Mays, V.M.; Jones, A.L.; Cochran, S.D.; Taylor, R.J.; Rafferty, J.; Jackson, J.S. Chronicity and mental health service utilization for anxiety, mood, and substance use disorders among black men in the United States; ethnicity and nativity differences. In Healthcare 2018, 6, 53. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.B.; Zhao, X.; Hoffman, L.; Morse, A.L.; Delahanty, J. Nicotine and addiction beliefs and perceptions among the US-born and foreign-born populations. Prev. Med. 2018, 114, 107–114. [Google Scholar] [CrossRef]
- Saint-Fort, L.; Choi, K. Heterogeneity in Tobacco-Use Behaviors Among US Blacks per Global Region of Origin. J. Immigr. Minority Health 2019, 21, 1185–1189. [Google Scholar] [CrossRef]
- Jones, A.L.; Cochran, S.D.; Rafferty, J.; Taylor, R.J.; Mays, V.M. Lifetime and twelve-month prevalence, persistence, and unmet treatment needs of mood, anxiety, and substance use disorders in African American and US versus foreign-born Caribbean women. Int. J. Environ. Res. Public Health 2020, 17, 7007. [Google Scholar] [CrossRef] [PubMed]
- Jegede, O.; Na, P.J.; Rhee, T.G.; Stefanovics, E.A.; Rosenheck, R.A. Psychiatric and Substance Use Disorders and Related Service Use in the Diverse Black Sub-Populations in the United States. J. Racial Ethn. Health Disparities 2021, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Okpala, P.C.; Rosario, C.; Dupont-Reyes, M.J.; Martin Romero, M.Y.; Alam, M.T.; Paivanas, H.; Echeverria, S.E. Nativity Status and Poly Tobacco Use among Young Adults in the United States. Int. J. Environ. Res. Public Health 2022, 19, 1230. [Google Scholar] [CrossRef]
- Cano, M.; Sparks, C.S. Drug overdose mortality by race/ethnicity across US-born and immigrant populations. Drug Alcohol Depend. 2022, 232, 109309. [Google Scholar] [CrossRef]
- Keane, F.; Tappen, R.M.; Williams, C.L.; Rosselli, M. Comparison of African American and Afro-Caribbean Older Adults’ Self-Reported Health Status, Function, and Substance Use. J. Black Psychol. 2009, 35, 44–62. [Google Scholar] [CrossRef]
- Acevedo-Garcia, D.; Bates, L.M.; Osypuk, T.; McArdle, N. The Effect of Immigrant Generation and Duration on Self-Rated Health among Us Adults 2003–2007. Soc. Sci. Med. 2010, 71, 1161–1172. [Google Scholar] [CrossRef]
- Griffith, D.M.; Johnson, J.L.; Zhang, R.; Neighbors, H.W.; Jackson, J.S. Ethnicity, nativity, and the health of American Blacks. J. Health Care Poor Underserved 2011, 22, 142. [Google Scholar] [CrossRef]
- Erving, C.L. Ethnic and nativity differences in the social support-physical health association among black Americans. J. Immigr. Minority Health 2016, 20, 124–139. [Google Scholar] [CrossRef]
- Christie-Mizell, C.A.; Leslie, E.T.A.; Hearne, B.N. Self-Rated Health, Discrimination, and Racial Group Identity: The Consequences of Ethnicity and Nativity among Black Americans. J. Afr. Am. Stud. 2017, 21, 643–664. [Google Scholar] [CrossRef]
- Maskileyson, D.; Seddig, D.; Davidov, E. The comparability of perceived physical and mental health measures across immigrants and natives in the United States. Demography 2021, 58, 1423–1443. [Google Scholar] [CrossRef] [PubMed]
- Erving, C.L. Stress exposure and physical health among older African American and Caribbean Black women. J. Aging Health 2022, 34, 320–333. [Google Scholar] [CrossRef]
- Singh, G.K.; Siahpush, M. Ethnic-Immigrant Differentials in Health Behaviors, Morbidity, and Cause-Specific Mortality in the United States: An Analysis of Two National Data Bases. Hum. Biol. 2002, 74, 83–109. [Google Scholar] [CrossRef] [PubMed]
- Doamekpor, L.A.; Dinwiddie, G.Y. Allostatic Load in Foreign-Born and Us-Born Blacks: Evidence from the 2001–2010 National Health and Nutrition Examination Survey. Am. J. Public Health 2015, 105, 591–597. [Google Scholar] [CrossRef]
- Goel, M.S.; McCarthy, E.P.; Phillips, R.S.; Wee, C.C. Obesity among Us Immigrant Subgroups by Duration of Residence. JAMA 2004, 292, 2860–2867. [Google Scholar] [CrossRef]
- Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53); Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2018; Available online: https://www.samhsa.gov/data/ (accessed on 5 July 2022).
- Krieger, N.; Kosheleva, A.; Waterman, P.D.; Chen, J.T.; Koenen, K. Racial Discrimination, Psychological Distress, and Self-Rated Health among Us-Born and Foreign-Born Black Americans. Am. J. Public Health 2011, 101, 1704–1713. [Google Scholar] [CrossRef] [PubMed]
- Harkness, J.A.; Braun, M.; Edwards, B.; Johnson, T.P.; Lyberg, L.; Mohler, P.P.; Pennell, Be.; Smith, T.W. Survey Methods in Multinational, Multiregional, and Multicultural Contexts; Wiley: Hoboken, NJ, USA, 2010. [Google Scholar]
- Johnson, T.P.; Bowman, P.J. Cross-cultural sources of measurement error in substance use surveys. Subst. Use Misuse 2003, 38, 1447–1490. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).