Three-Dimensional Evaluation of the Frontal Sinus in Koreans
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. CBCT Data
2.3. 3D Modeling
2.3.1. Frontal Sinus 3D Modeling
2.3.2. Cranial Bone 3D Modeling
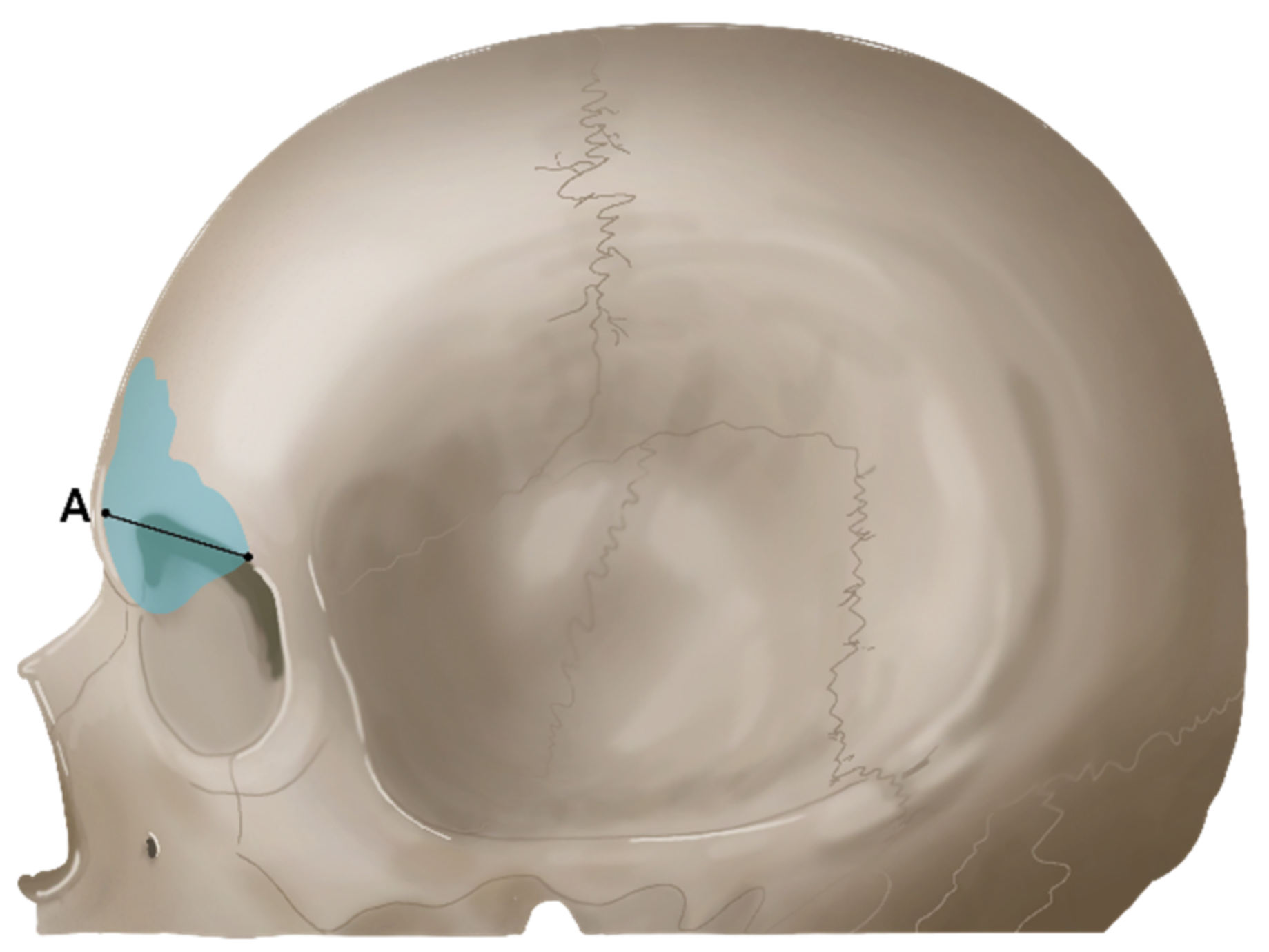
2.4. Measurements
2.5. Statistical Analysis
3. Results
3.1. Frontal Sinus Width (XW) and Height (XH)
3.2. Frontal Sinus Width (ZW) and Volume (FSV)
3.3. Cranial Bone Transversal Width
3.4. Correlation between Frontal Sinus Width and Cranial Bone Transversal Width
3.5. Correlation between Frontal Sinus Height and Cranial Bone Transversal Width
3.6. Correlation between Frontal Sinus Volume and Cranial Bone Transversal Width
3.7. Frontal Sinus Width (XW) and Height (XH) According to Malocclusion
3.8. Frontal Sinus Width (ZW) and Volume (FSV) According to Malocclusion
3.9. Cranial Bone Transversal Width According to Malocclusion
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nikolova, S.; Toneva, D.; Georgiev, I.; Lazarov, N. Digital radiomorphometric analysis of the frontal sinus and assessment of the relation between persistent metopic suture and frontal sinus development. Am. J. Phys. Anthropol. 2018, 165, 492–506. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.; Acharya, A.B.; Sattur, A.P.; Naikmasur, V.G. Are frontal sinuses useful indicators of sex? J. Forensic Leg. Med. 2013, 20, 91–94. [Google Scholar] [CrossRef] [PubMed]
- Coemert, S.; Roth, R.; Strauss, G.; Schmitz, P.M.; Lueth, T.C. A handheld flexible manipulator system for frontal sinus surgery. Int. J. Comput. Assist. Radiol. Surg. 2020, 15, 1549–1559. [Google Scholar] [CrossRef] [PubMed]
- Kountakis, S.E.; Senior, B.A.; Draf, W. (Eds.) . The Frontal Sinus; Springer: Berlin, Germany, 2005; Volume 14, p. 294. [Google Scholar]
- Barham, H.P.; Hall, C.A.; Hernandez, S.C.; Zylicz, H.E.; Stevenson, M.M.; Zito, B.A.; Harvey, R.J. Impact of Draf III, Draf IIb, and Draf IIa frontal sinus surgery on nasal irrigation distribution. Int. Forum Allergy Rhinol. 2020, 10, 49–52. [Google Scholar] [CrossRef]
- Svider, P.F.; Sekhsaria, V.; Cohen, D.S.; Eloy, J.A.; Setzen, M.; Folbe, A.J. Geographic and temporal trends in frontal sinus surgery. Int. Forum Allergy Rhinol. 2015, 5, 46–54. [Google Scholar] [CrossRef]
- Manson, P.N.; Stanwix, M.G.; Yaremchuk, M.J.; Nam, A.J.; Hui-Chou, H.; Rodriguez, E.D. Frontobasal fractures: Anatomical classification and clinical significance. Plast. Reconstr. Surg. 2009, 124, 2096–2106. [Google Scholar] [CrossRef]
- Kim, D.W.; Yoon, E.S.; Lee, B.I.; Dhong, E.S.; Park, S.H. Fracture depth and delayed contour deformity in frontal sinus anterior wall fracture. J. Craniofac. Surg. 2012, 23, 991–994. [Google Scholar] [CrossRef]
- Chegini, S.; Gallighan, N.; Mcleod, N.; Corkill, R.; Bojanic, S.; Griffiths, S.; Dhariwal, D. Outcomes of treatment of fractures of the frontal sinus: Review from a tertiary multispecialty craniofacial trauma service. Br. J. Oral Maxillofac. Surg. 2016, 54, 801–805. [Google Scholar] [CrossRef]
- Buller, J.; Maus, V.; Grandoch, A.; Kreppel, M.; Zirk, M.; Zöller, J.E. Frontal sinus morphology: A reliable factor for classification of frontal bone fractures? J. Oral Maxillofac. Surg. 2018, 76, 2168.e1. [Google Scholar] [CrossRef]
- Ruiz, C.R.; Wafae, N. Anatomo-radiological and morphometrical study of the frontal sinus in humans. J. Morphol. Sci. 2017, 21, 53–56. [Google Scholar]
- Yun, I.S. Three Dimensional Computed Tomographic Analysis of Frontal Sinus in Koreans. Ph.D. Thesis, Yonsei University, Seoul, Korea, 2010. [Google Scholar]
- Motawei, S.M.; Wahba, B.A.; Aboelmaaty, W.M.; Tolba, E.M. Assessment of frontal sinus dimensions using CBCT to determine sexual dimorphism amongst Egyptian population. J. Forensic Radiol. Imaging 2016, 6, 8–13. [Google Scholar] [CrossRef]
- Aki, T.; Nanda, R.S.; Currier, G.F.; Nanda, S.K. Assessment of symphysis morphology as a predictor of the direction of mandibular growth. Am. J. Orthod. Dentofac. Orthop. 1994, 106, 60–69. [Google Scholar] [CrossRef]
- Shapiro, R.; Schorr, S. A consideration of the systemic factors that influence frontal sinus pneumatization. Investig. Radiol. 1980, 15, 191–202. [Google Scholar] [CrossRef]
- Galletti, B.; Gazia, F.; Freni, F.; Sireci, F.; Galletti, F. Endoscopic sinus surgery with and without computer assisted navigation: A retrospective study. Auris Nasus Larynx 2019, 46, 520–525. [Google Scholar] [CrossRef] [PubMed]
- Stankiewicz, J.A. Complications of endoscopic sinus surgery. Otolaryngol. Clin. N. Am. 1989, 22, 749–758. [Google Scholar] [CrossRef]
- Tehranchi, A.; Motamedian, S.R.; Saedi, S.; Kabiri, S.; Shidfar, S. Correlation between frontal sinus dimensions and cephalometric indices: A cross-sectional study. Eur. J. Dent. 2017, 11, 64–70. [Google Scholar] [CrossRef]
- Buyuk, S.K.; Karaman, A.; Yasa, Y. Association between frontal sinus morphology and craniofacial parameters: A forensic view. J. Forensic Leg. Med. 2017, 49, 20–23. [Google Scholar] [CrossRef]
- Soman, B.A.; Sujatha, G.P.; Lingappa, A. Morphometric evaluation of the frontal sinus in relation to age and gender in subjects residing in Davangere, Karnataka. J. Forensic Dent. Sci. 2016, 8, 57. [Google Scholar] [CrossRef] [Green Version]
- Kjær, I.; Pallisgaard, C.; Brock-Jacobsen, M.T. Frontal sinus dimensions can differ significantly between individuals within a monozygotic twin pair, indicating environmental influence on sinus sizes. Acta Oto-Laryngol. 2012, 132, 988–994. [Google Scholar] [CrossRef]
- Pirner, S.; Tingelhoff, K.; Wagner, I.; Westphal, R.; Rilk, M.; Wahl, F.M.; Bootz, F.; Eichhorn, K.W. CT-based manual segmentation and evaluation of paranasal sinuses. Eur. Arch. Oto-Rhino-Laryngol. 2009, 266, 507–518. [Google Scholar] [CrossRef]
- Shah, R.K.; Dhingra, J.K.; Carter, B.L.; Rebeiz, E.E. Paranasal sinus development: A radiographic study. Laryngoscope 2003, 113, 205–209. [Google Scholar] [CrossRef]
- Blaney, S.P.A. Why paranasal sinuses? J. Laryngol. Otol. 1990, 104, 690–693. [Google Scholar] [CrossRef] [PubMed]
- Sabharwal, A.; Patil, A.S.; Shinde, S.; Swami, V. Analysis of frontal sinus in various malocclusions. Int. J. Orthod. Rehabil. 2019, 10, 116. [Google Scholar] [CrossRef]
- Nahm, F.S. Understanding effect sizes. Hanyang Med. Rev. 2015, 35, 40–43. [Google Scholar] [CrossRef] [Green Version]
- Fleckenstein, P.; Tranum-Jensen, J. Anatomy in Diagnostic Imaging; John Wiley & Sons: New York, NY, USA, 2014. [Google Scholar]


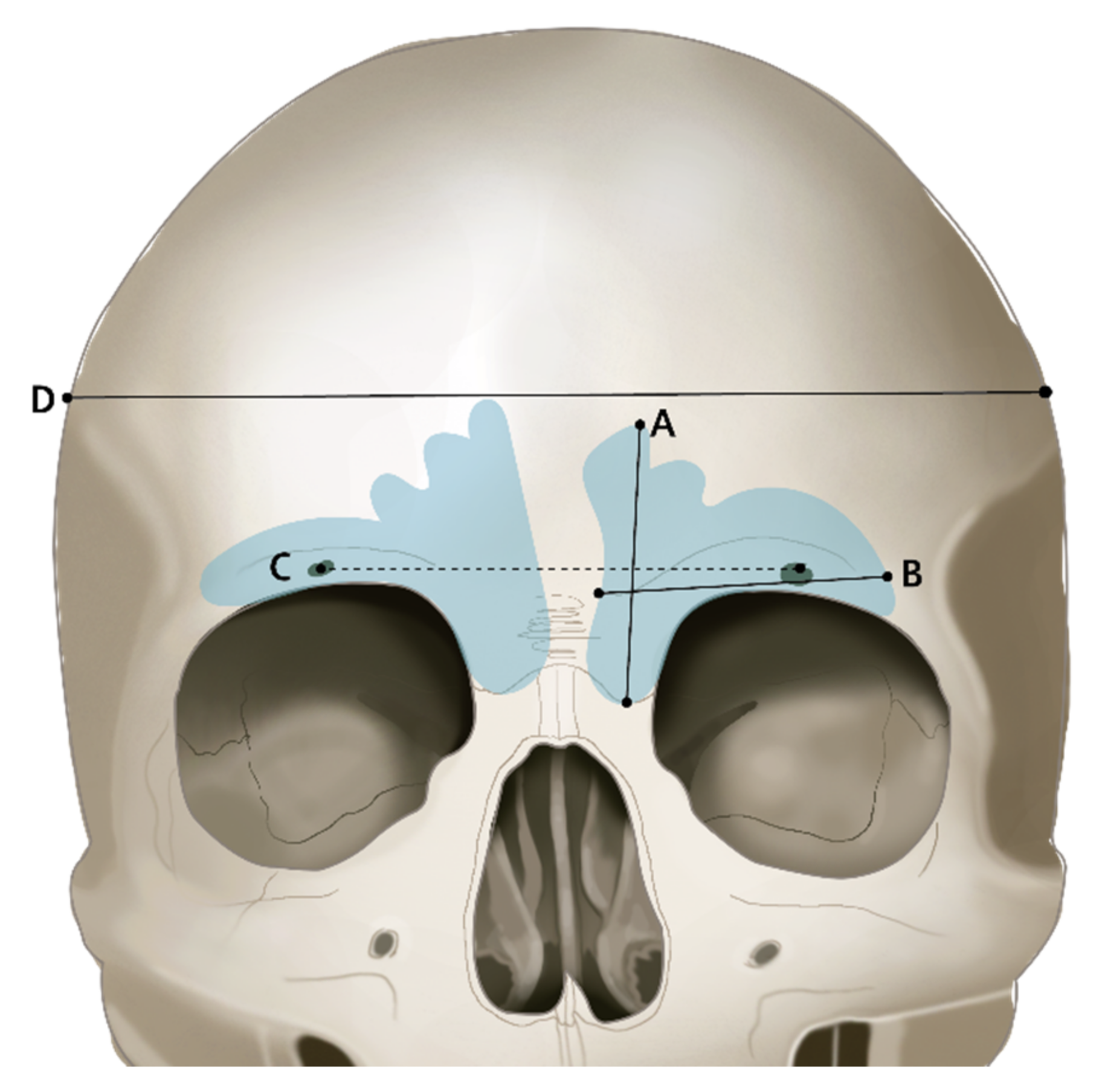



| Parameter | Definition |
|---|---|
| Right frontal sinus width (RXW) | Width of right frontal sinus in a coronal view |
| Left frontal sinus width (LXW) | Width of left frontal sinus in a coronal view |
| Right frontal sinus height (RXH) | Height of right frontal sinus in a coronal view |
| Left frontal sinus height (LXH) | Height of left frontal sinus in a coronal view |
| Frontal sinus width (ZW) | Frontal sinus width in a sagittal view |
| Frontal sinus volume (FSV) | Frontal sinus total volume |
| Parameter | Definition |
|---|---|
| Supraorbital line (SOL) | Distance between supraorbital foramens |
| Cranial bone transversal width (CW) | Full width of cranial bone in a coronal view |
| Measurements | Male (N = 30) | Female (N = 30) | p Value |
|---|---|---|---|
| RXW (mm) | 28.29 (4.76) | 26.30 (5.34) | 0.042 * |
| RXH (mm) | 30.09 (6.03) | 26.31 (3.84) | 0.050 * |
| LXW (mm) | 30.49 (7.15) | 25.41 (7.58) | 0.008 * |
| LXH (mm) | 30.93 (6.69) | 27.42 (7.17) | 0.048 * |
| ZW (mm) | 25.22 (9.08) | 19.69 (5.25) | 0.004 * |
| Volume (mm3) | 9602 (5658) | 5611 (3452) | 0.002 * |
| SOL (mm) | 52.83 (6.21) | 48.08 (3.34) | 0.001 * |
| Cranial bone transversal width (mm) | 151.12 (6.49) | 145.99 (4.54) | 0.002 * |
| RXW (mm) | RXH (mm) | LXW (mm) | LXH (mm) | ZW (mm) | Volume (mm3) | SOL (mm) | Cranial Bone Transversal Width (mm) | |
|---|---|---|---|---|---|---|---|---|
| RXW (mm) | 1 | |||||||
| RXH (mm) | 0.643 ** | 1 | ||||||
| LXW (mm) | NS | NS | 1 | |||||
| LXH (mm) | NS | NS | 0.474 ** | 1 | ||||
| ZW (mm) | 0.230 | 0.228 | 0.335 ** | 0.158 | 1 | |||
| Volume (mm3) | 0.705 ** | 0.710 ** | 0.669 ** | 0.480 ** | 0.341 ** | 1 | ||
| SOL (mm) | 0.368 ** | 0.309 ** | 0.376 ** | 0.188 | 0.339 ** | 0.450 ** | 1 | |
| Cranial bone transversal width (mm) | 0.293 * | 0.333 ** | 0.298 * | 0.055 | 0.289 * | 0.404 ** | 0.421 ** | 1 |
| Measurements | B | SE | β | T (p) | F (p) | R2 |
|---|---|---|---|---|---|---|
| Constant | 129.168 | 8.477 | 15.238 | 2.931 | 0.283 | |
| RXW (mm) | 0.068 | 0.225 | 0.058 | 0.301 | ||
| RXH (mm) | 0.184 | 0.215 | 0.161 | 0.856 | ||
| LXW (mm) | 0.058 | 0.138 | 0.074 | 0.422 | ||
| LXH (mm) | −0.216 | 0.136 | −0.251 | −1.590 | ||
| ZW (mm) | 0.088 | 0.101 | 0.113 | 0.870 | ||
| Volume (mm3) | 0.021 | 0.026 | 0.174 | 0.795 | ||
| SOL (mm) | 0.267 | 0.154 | 0.240 | 1.741 |
| Measurements | Class I (N = 20) | Class II (N = 20) | Class III (N = 20) | p Value |
|---|---|---|---|---|
| RXW (mm) | 27.83 (5.46) | 25.56 (5.11) | 27.00 (5.14) | 0.976 |
| RXH (mm) | 29.07 (5.75) | 28.28 (5.58) | 27.26 (4.84) | 0.430 |
| LXW (mm) | 29.32 (9.54) | 25.66 (6.39) | 28.87 (6.77) | 0.591 |
| LXH (mm) | 28.81 (7.13) | 29.45 (7.23) | 29.26 (7.29) | 0.294 |
| ZW (mm) | 23.48 (5.85) | 23.22 (11.27) | 20.68 (5.07) | 0.901 |
| Volume (mm3) | 8068 (5378.99) | 7664 (5144.70) | 7088 (4868.17) | 0.004 * |
| SOL (mm) | 51.91 (5.38) | 51.47 (4.14) | 47.98 (6.15) | 0.479 |
| Cranial bone trans-versal Width (mm) | 148.89 (5.42) | 146.95 (5.00) | 149.82 (7.58) | 0.287 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-H.; Park, J.-T. Three-Dimensional Evaluation of the Frontal Sinus in Koreans. Int. J. Environ. Res. Public Health 2022, 19, 9605. https://doi.org/10.3390/ijerph19159605
Lee J-H, Park J-T. Three-Dimensional Evaluation of the Frontal Sinus in Koreans. International Journal of Environmental Research and Public Health. 2022; 19(15):9605. https://doi.org/10.3390/ijerph19159605
Chicago/Turabian StyleLee, Jeong-Hyun, and Jong-Tae Park. 2022. "Three-Dimensional Evaluation of the Frontal Sinus in Koreans" International Journal of Environmental Research and Public Health 19, no. 15: 9605. https://doi.org/10.3390/ijerph19159605






