Cost of Health-Related Work Productivity Loss among Fly-In Fly-Out Mining Workers in Australia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Survey Instruments and Measures
2.2.1. Sociodemographic and Work Characteristics
2.2.2. Health Conditions
2.2.3. Work Productivity Loss Measures
2.3. Data Analysis and Cost Estimation Plan
- prev = prevalence of a health condition,
- excess loss = excess work productivity loss given by the regression coefficients (due to absenteeism or presenteeism or total productivity loss) attributable to an individual at high risk of a health condition,
- annual salary = average annual salary for full-time mining; AUD $134,323.20
2.3.1. Sensitivity Analysis
2.3.2. Health- and Work-Related Predictors of Work Productivity Loss
3. Results
3.1. Background Characteristics of Study Participants
3.2. Prevalence of Risk of Health Conditions
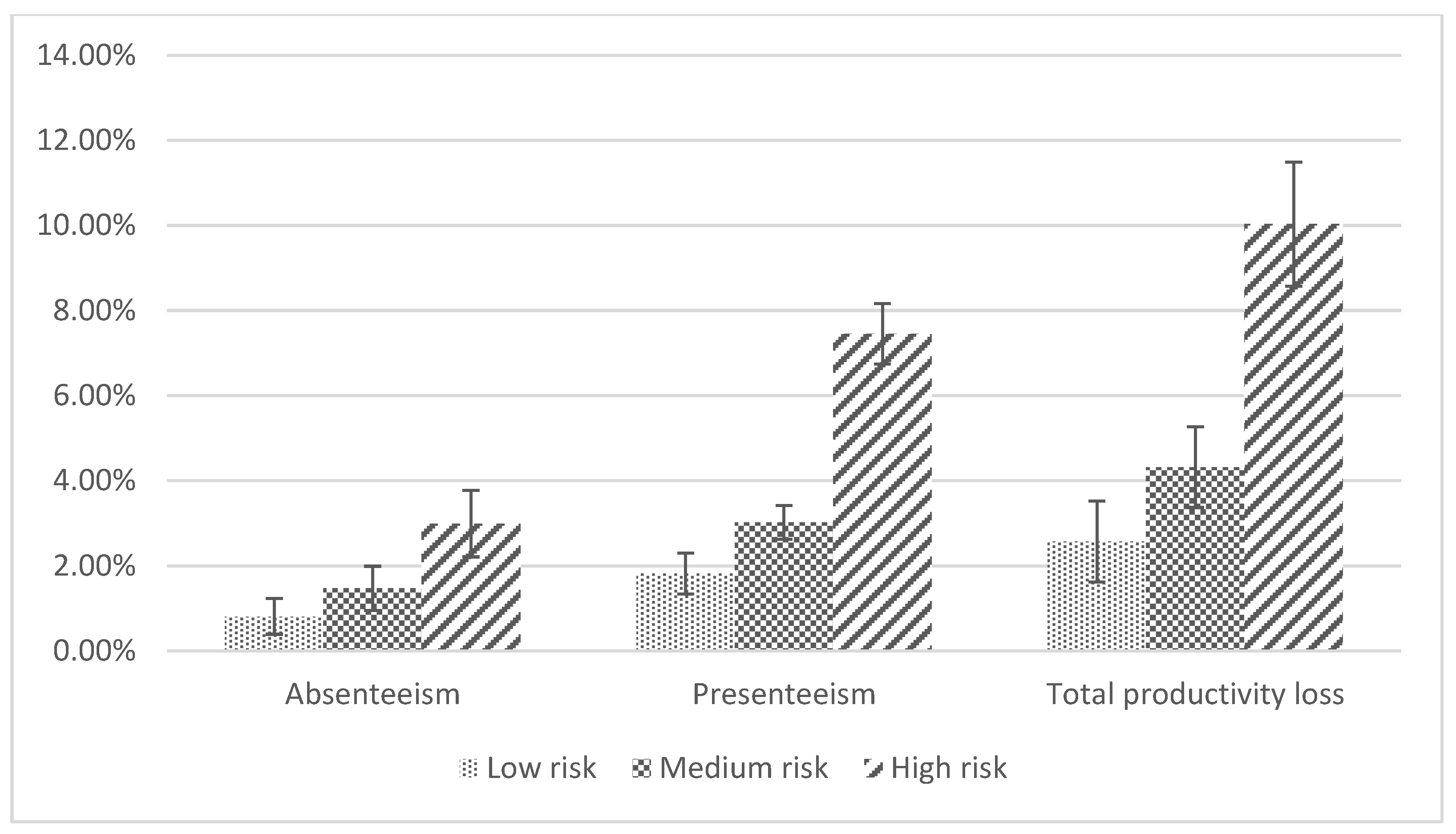
3.3. Productivity Loss in Individuals with High Health Risks
3.4. Productivity Loss in Individuals with High Health Risks
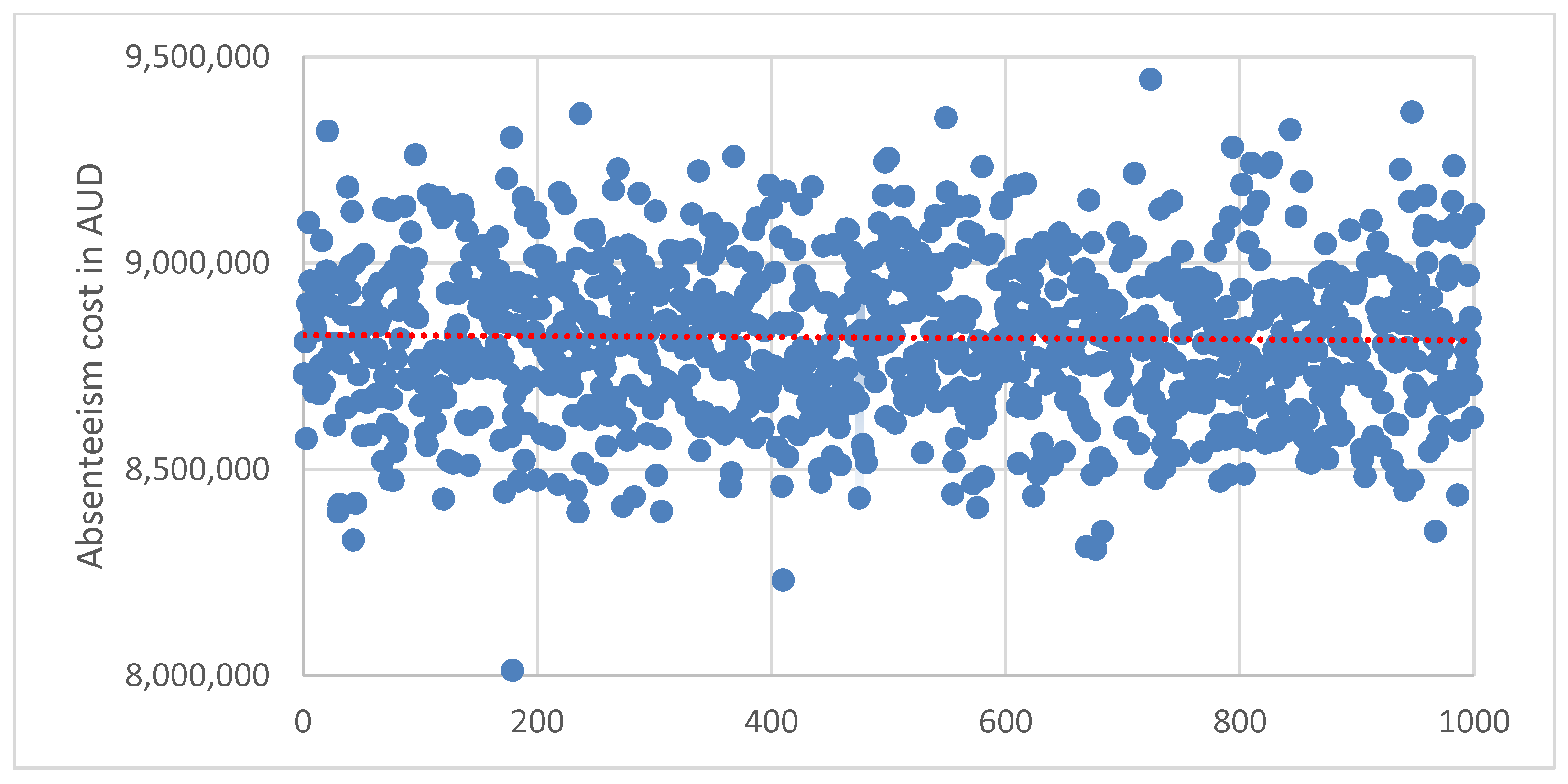
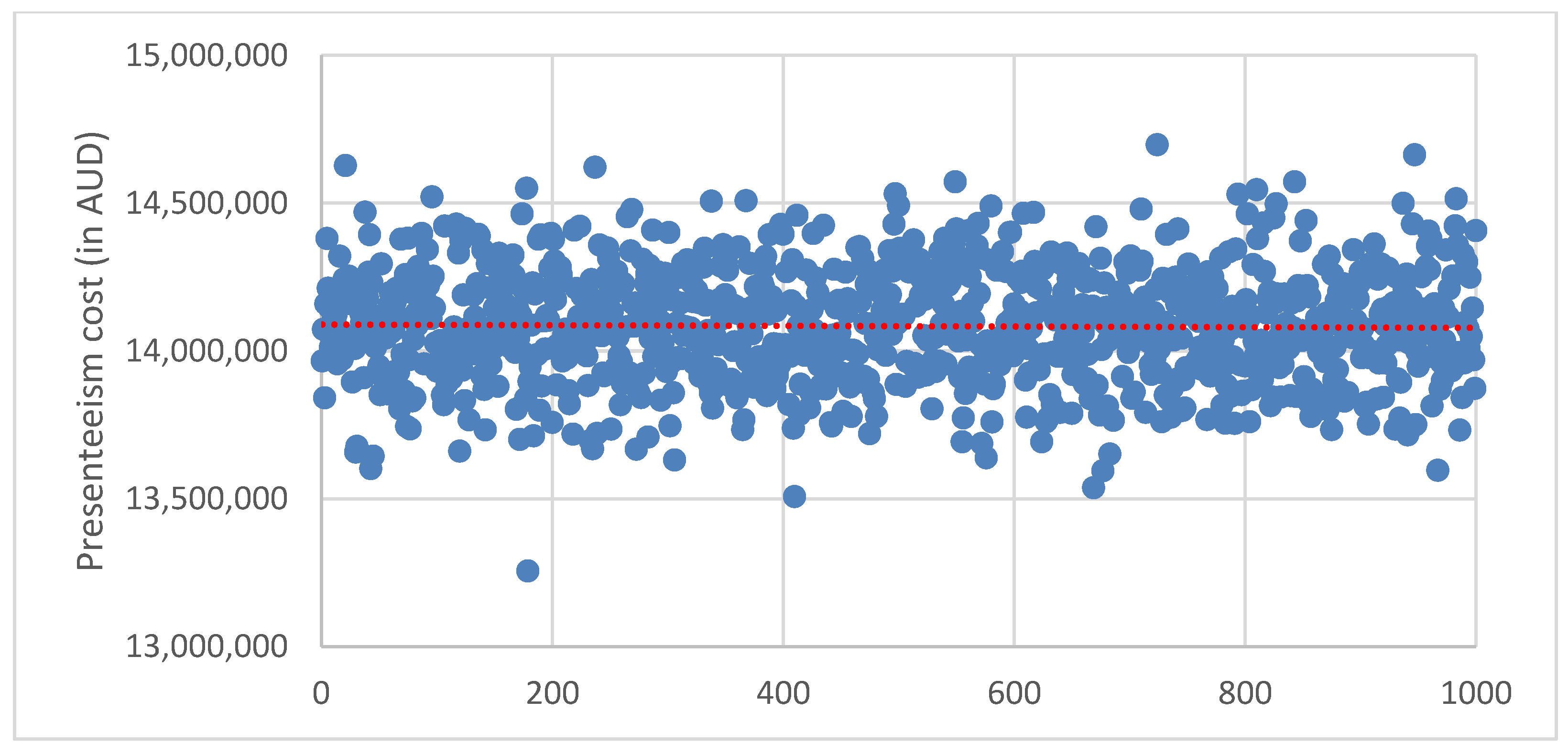
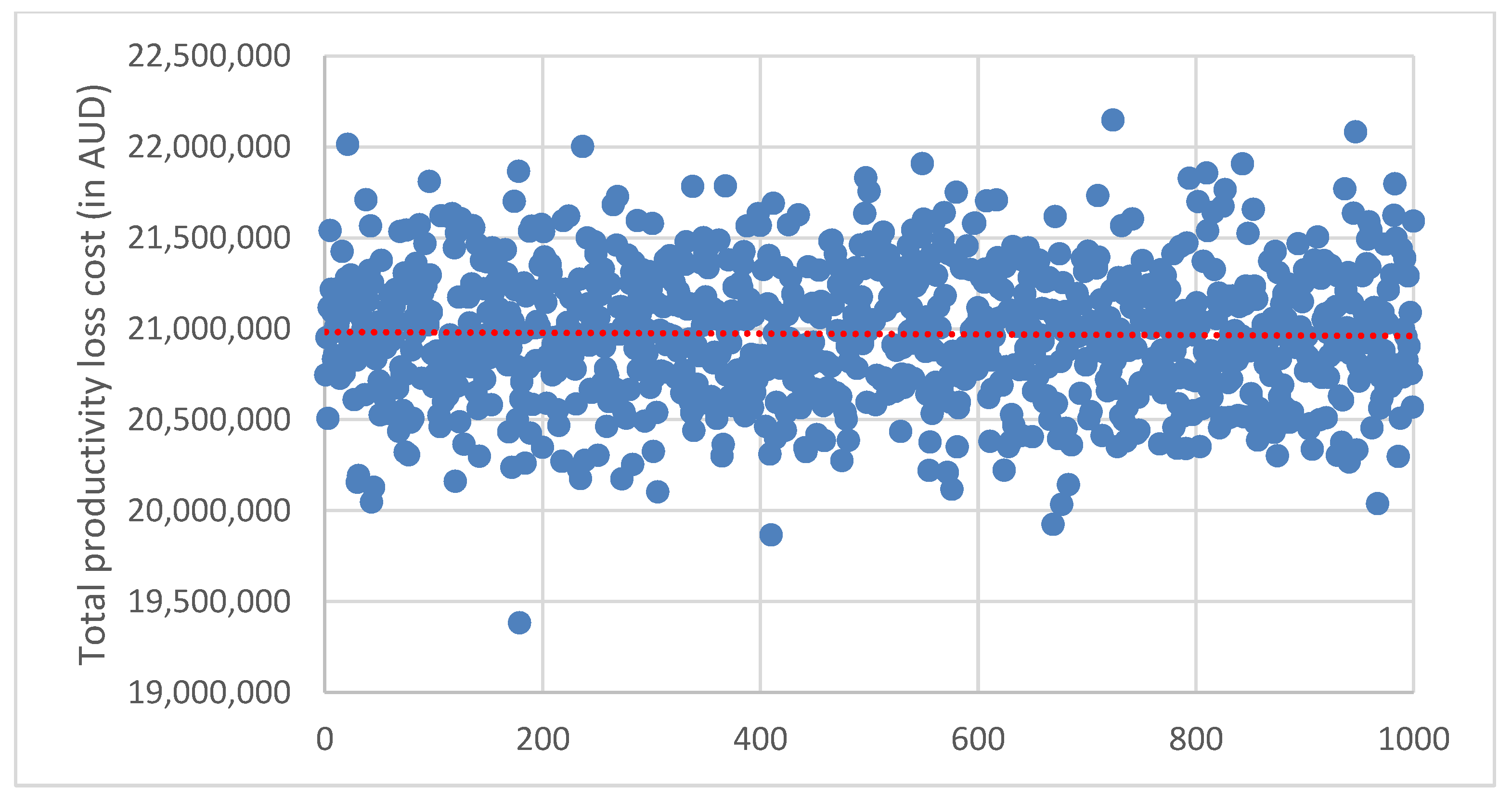
3.5. Sensitivity Analysis
3.6. Health and Work-Related Factors Associated with Productivity Loss Measures
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ling, R.; Kelly, B.; Considine, R.; Tynan, R.; Searles, A.; Doran, C.M. The economic impact of psychological distress in the Australian coal mining industry. J. Occup. Environ. Med. 2016, 58, e171–e176. [Google Scholar] [CrossRef]
- Storey, K. Fly-in/fly-out and fly-over: Mining and regional development in Western Australia. Aust. Geogr. 2001, 32, 133–148. [Google Scholar] [CrossRef]
- Storey, K. The evolution of commute work in the resource sectors in Canada and Australia. Extr. Ind. Soc. 2016, 3, 584–593. [Google Scholar] [CrossRef]
- Mckenzie, F.H. Fly-in fly-out: The challenges of transient populations in rural landscapes. In Demographic Change in Australia’s Rural Landscapes Landscape Series; Luck, G., Black, R., Race, D., Eds.; Springer: Dordrecht, The Netherlands, 2010; pp. 325–374. [Google Scholar]
- Vojnovic, P.; Michelson, G.; Jackson, D.; Bahn, S. Adjustment, well-being and help-seeking among Australian FIFO mining employees. Aust. Bull. Labour 2014, 40, 242–261. [Google Scholar]
- Asare, B.; Kwasnicka, D.; Powell, D.; Robinson, S. Health and well-being of rotation workers in the mining, offshore oil and gas, and construction industry: A systematic review. BMJ Glob. Health 2021, 6, e005112. [Google Scholar] [CrossRef]
- Carrington, K.; McIntosh, A. A Literature Review of Wellness, Wellbeing and Quality of Life Issues as they Impact upon the Australian Mining Sector; Crime and Justice Research Centre: Brisbane, Australia, 2013. [Google Scholar]
- Howard, K.J.; Howard, J.T.; Smyth, A.F. The Prolem of Abesenteeism and Presenteeism in the Workplace. In Handbook of Occupational Health and Wellness; Gatchel, R., Schultz, I., Eds.; Springer: Boston, MA, USA, 2012; pp. 151–179. [Google Scholar]
- Kowlessar, N.M.; Goetzel, R.Z.; Carls, G.S.; Tabrizi, M.J.; Guindon, A. The relationship between 11 health risks and medical and productivity costs for a large employer. J. Occup. Environ. Med. 2011, 53, 468–477. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Bansback, N.; Anis, A.H. Measuring and valuing productivity loss due to poor health: A critical review. Soc. Sci. Med. 2011, 72, 185–192. [Google Scholar] [CrossRef]
- Kigozi, J.; Jowett, S.; Lewis, M.; Barton, P.; Coast, J. The Estimation and Inclusion of Presenteeism Costs in Applied Economic Evaluation: A Systematic Review. Value Health 2017, 20, 496–506. [Google Scholar] [CrossRef] [PubMed]
- Strömberg, C.; Aboagye, E.; Hagberg, J.; Bergström, G.; Lohela-Karlsson, M. Estimating the Effect and Economic Impact of Absenteeism, Presenteeism, and Work Environment–Related Problems on Reductions in Productivity from a Managerial Perspective. Value Health 2017, 20, 1058–1064. [Google Scholar] [CrossRef] [PubMed]
- Holden, L.; Scuffham, P.A.; Hilton, M.F.; Ware, R.S.; Vecchio, N.; Whiteford, H.A. Which health conditions impact on productivity in working Australians? J. Occup. Environ. Med. 2011, 53, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Yoshimoto, T.; Oka, H.; Fujii, T.; Nagata, T.; Matsudaira, K. The Economic Burden of Lost Productivity due to Presenteeism Caused by Health Conditions Among Workers in Japan. J. Occup. Environ. Med. 2020, 62, 883–888. [Google Scholar] [CrossRef]
- Shiels, C.; Gabbay, M.B.; Ford, F.M. Patient factors associated with duration of certified sickness absence and transition to long-term incapacity. Br. J. Gen. Pract. 2004, 54, 86–91. [Google Scholar]
- Goetzel, R.Z.; Long, S.R.; Ozminkowski, R.J.; Hawkins, K.; Wang, S.; Lynch, W. Health, Absence, Disability, and Presenteeism Cost Estimates of Certain Physical and Mental Health Conditions Affecting U.S. Employers. J. Occup. Environ. Med. 2004, 46, 398–412. [Google Scholar] [CrossRef]
- Kessler, R.C.; Akiskal, H.S.; Ames, M.; Birnbaum, H.; Greenberg, P.; Hirschfeld, R.M.; Jin, R.; Merikangas, K.R.; Simon, G.E.; Wang, P.S. Prevalence and effects of mood disorders on work performance in a nationally representative sample of U.S. workers. Am. J. Psychiatry 2006, 163, 1561–1568. [Google Scholar] [CrossRef]
- Burton, W.N.; Chen, C.Y.; Conti, D.J.; Schultz, A.B.; Pransky, G.; Edington, D.W. The association of health risks with on-the-job productivity. J. Occup. Environ. Med. 2005, 47, 769–777. [Google Scholar] [CrossRef] [PubMed]
- Hilton, M.F.; Scuffham, P.A.; Vecchio, N.; Whiteford, H.A. Using the interaction of mental health symptoms and treatment status to estimate lost employee productivity. Aust. N. Z. J. Psychiatry 2010, 44, 151–161. [Google Scholar] [CrossRef]
- Evers, K.E.; Castle, P.H.; Prochaska, J.O.; Prochaska, J.M. Examining relationships between multiple health risk behaviors, well-being, and productivity. Psychol. Rep. 2014, 114, 843–853. [Google Scholar] [CrossRef] [PubMed]
- Kirkham, H.S.; Clark, B.L.; Bolas, C.A.; Lewis, G.H.; Jackson, A.S.; Fisher, D.; Duncan, I. Which modifiable health risks are associated with changes in productivity costs? Popul. Health Manag. 2015, 18, 30–38. [Google Scholar] [CrossRef]
- Schultz, A.B.; Edington, D.W. Employee health and presenteeism: A systematic review. J. Occup. Rehabil. 2007, 17, 547–579. [Google Scholar] [CrossRef]
- Goettler, A.; Grosse, A.; Sonntag, D. Productivity loss due to overweight and obesity: A systematic review of indirect costs. BMJ Open 2017, 7, e014632. [Google Scholar] [CrossRef] [PubMed]
- Henke, R.M.; Carls, G.S.; Short, M.E.; Pei, X.; Wang, S.; Moley, S.; Sullivan, M.; Goetzel, R.Z. The relationship between health risks and health and productivity costs among employees at pepsi bottling group. J. Occup. Environ. Med. 2010, 52, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Sears, L.E.; Coberley, C.R.; Pope, J.E. The association between modifiable well-being risks and productivity: A longitudinal study in pooled employer sample. J. Occup. Environ. Med. 2013, 55, 353–364. [Google Scholar] [CrossRef] [PubMed]
- Boles, M.; Pelletier, B.; Lynch, W. The relationship between health risks and work productivity. J. Occup. Environ. Med. 2004, 46, 737–745. [Google Scholar] [CrossRef] [PubMed]
- Musich, S.; Hook, D.; Baaner, S.; Edington, D.W. The association of two productivity measures with health risks and medical conditions in an Australian employee population. Am. J. Health Promot. 2006, 20, 353–363. [Google Scholar] [CrossRef]
- Street, T.D.; Lacey, S.J.; Somoray, K. Employee stress, reduced productivity, and interest in a workplace health program: A case study from the Australian mining industry. Int. J. Env. Res. Public Health 2019, 16, 94. [Google Scholar] [CrossRef]
- Street, T.D.; Lacey, S.J. Accounting for employee health: The productivity cost of leading health risks. Health Promot. J. Aust. 2019, 30, 228–237. [Google Scholar] [CrossRef]
- Miller, P.; Brook, L.; Stomski, N.J.; Ditchburn, G.; Morrison, P. Depression, suicide risk, and workplace bullying: A comparative study of fly-in, fly-out and residential resource workers in Australia. Aust. Health Rev. 2019, 44, 3–8. [Google Scholar] [CrossRef]
- Velander, F.; Schineanu, A.; Liang, W.; Midford, R. Digging for gold and coming up blue: A health survey in the mining industry. J. Health Saf. Environ. 2010, 26, 389–401. [Google Scholar]
- Tynan, R.J.; Considine, R.; Wiggers, J.; Lewin, T.J.; James, C.; Inder, K.; Kay-Lambkin, F.; Baker, A.L.; Skehan, J.; Perkins, D.; et al. Alcohol consumption in the Australian coal mining industry. Occup. Env. Med. 2017, 74, 259–267. [Google Scholar] [CrossRef]
- Nielsen, M.B.; Tvedt, S.D.; Matthiesen, S.B. Prevalence and occupational predictors of psychological distress in the offshore petroleum industry: A prospective study. Int. Arch. Occup. Env. Health 2013, 86, 875–885. [Google Scholar] [CrossRef]
- Pereira, M.J.; Coombes, B.K.; Comans, T.A.; Johnston, V. The impact of onsite workplace health-enhancing physical activity interventions on worker productivity: A systematic review. Occup. Environ. Med. 2015, 72, 401–412. [Google Scholar] [CrossRef] [PubMed]
- Mineral Councils of Australia. Independent Mining Statistics Should Be Used Accurately. Available online: https://www.minerals.org.au/news/independent-mining-statistics-should-be-used-accurately#:~:text=Mining%20employment%20has%20trebled%20from,above%2Daward%20wages%20and%20conditions (accessed on 10 July 2022).
- KPMG. Analysis of Long Distance Commuter Workforce Across Australia; Minerals Council of Australia: Canberra, Australia, 2013. [Google Scholar]
- Meredith, V.; Rush, P.; Robinson, E. Fly-in fly-out workforce practices in Australia: The effects on children and family relationships. In Child, Family, Community Australia; Information Exchange (CFCA PAPER NO. 19 2014); Australian Institute of Family Studies: Melbourne, Australia, 2014. [Google Scholar]
- Australian Bureau of Statistics. Fly-In Fly-Out (FIFO) Workers No. 6105.0; Australian Institute of Health and Welfare: Canberra, Australia, 2014. [Google Scholar]
- Education and Health Standing Committee. The Impact of FIFO Work Practices on Mental Health: Final Report; Report 5; Parliament of Western Australia: Perth, Australia, 2015; pp. 1–167. [Google Scholar]
- Rebar, A.L.; Alfrey, K.L.; Gardner, B.; Vandelanotte, C. Health behaviours of Australian fly-in, fly-out workers and partners during on-shift and off-shift days: An ecological momentary assessment study. BMJ Open 2018, 8, e023631. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, F.H.M.; Hoath, A. The socio-economic impact of mine industry commuting labour force on source communities. Resour. Policy 2014, 42, 45–52. [Google Scholar] [CrossRef]
- Qualtrics Online Data Collection Software. Available online: https://www.qualtrics.com/au/ (accessed on 21 May 2021).
- Barclay, M.A.; Harris, J.; Everingham, J.A.; Kirsch, P.; Arend, S.; Shi, S.; Kim, J. Factors Linked to the Well-Being of Fly-In-Fly-Out (FIFO) Workers; Centre for Social Responsibility in Mining, Minearls Industry Safety and Health Centre, The University of Queensland: Brisbane, Australia, 2014; pp. 40–43. [Google Scholar]
- James, C.; Tynan, R.; Roach, D.; Leigh, L.; Oldmeadow, C.; Rahman, M.; Kelly, B. Correlates of psychological distress among workers in the mining industry in remote Australia: Evidence from a multi-site cross-sectional survey. PLoS ONE 2018, 13, e0209377. [Google Scholar] [CrossRef] [PubMed]
- Parker, S.; Fruhen, L.; Burton, C.; McQuade, S.; Loveny, J.; Griffin, M.; Page, A.; Chikritzhs, T.; Crock, S.; Jorritsma, K.; et al. Impact of FIFO Work Arrangements on the Mental Health and Wellbeing of FIFO Workers; Centre for Transformative Work Design: Perth, Australia, 2018. [Google Scholar]
- Lenneman, J.; Schwartz, S.; Giuseffi, D.L.; Wang, C. Productivity and health: An application of three perspectives to measuring productivity. J. Occup. Environ. Med. 2011, 53, 55–61. [Google Scholar] [CrossRef]
- Kessler, R.; Andrews, G.; Colpe, L.; Hiripi, E.; Mroczek, D.; Normand, S.L.T.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Dewey, J.E.; Gandek, B. How to Score and Interpret Single-Item Health Status Measures: A Manual for Users of the SF-8 Health Survey; QualityMetric Incorporated: Lincoln, RI, USA, 2001; Volume 15, p. 5. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Bradley, K.A.; Debenedetti, A.F.; Volk, R.J.; Williams, E.C.; Frank, D.; Kivlahan, D.R. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin. Exp. Res. 2007, 31, 1208–1217. [Google Scholar] [CrossRef]
- Craig, C.; Marshall, A.; Sjostrom, M.; Bauman, A.; Lee, P.; Macfarlane, D.; Lam, T.; Stewart, S. International physical activity questionnaire-short form. J. Am. Coll. Health 2017, 65, 492–501. [Google Scholar]
- IPAQ Research Committee. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ)-short and long forms. 2005. Available online: http://www.ipaq.ki.se/scoring.pdf (accessed on 21 May 2021).
- Australian Bureau of Statistics. National Health Survey 2011-12 Questionnaire. 2011. Available online: https://www.abs.gov.au/AUSSTATS/abs@.nsf/39433889d406eeb9ca2570610019e9a5/9f4d8e85b3aab3b7ca257a9a00790bea/$FILE/National%20Health%20Survey%202011-12%20questionnaire.pdf (accessed on 21 May 2021).
- Australian Bureau of Statistics. Dietary Behaviour. Dietary Behaviour, 2017–2018 Financial Year. 2018. Available online: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/dietary-behaviour/latest-release (accessed on 4 November 2021).
- Reilly, M.C.; Zbrozek, A.S.; Dukes, E.M. The Validity and Reproducibility of a Work Productivity and Activity Impairment Instrument. Pharmacoeconomics 1993, 4, 353–365. [Google Scholar] [CrossRef]
- Lee, D.W.; Lee, J.; Kim, H.R.; Kang, M.Y. Health-related productivity loss according to health conditions among workers in South Korea. Int. J. Environ. Res. Public Health 2021, 18, 7589. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Employee Earnings and Hours, Australia, May 2021. Earnings and work hours. 2021. Available online: https://www.abs.gov.au/statistics/labour/earnings-and-work-hours/employee-earnings-and-hours-australia/latest-release (accessed on 7 February 2022).
- Kozak, M.; Piepho, H.P. What’s normal anyway? Residual plots are more telling than significance tests when checking ANOVA assumptions. J. Agro. Crop. Sci. 2018, 204, 86–98. [Google Scholar] [CrossRef]
- Bolge, S.L.; Doan, J.F.; Kannan HBaran, R.W. Association of insomnia with quality of life, work productivity, and activity impairment. Qual. Life Res. 2009, 18, 415–422. [Google Scholar] [CrossRef]
- d’Errico, M.; Pavlova, M.; Spandonaro, F. The economic burden of obesity in Italy: A cost-of-illness study. Eur. J. Health Econ. 2022, 23, 177–192. [Google Scholar] [CrossRef] [PubMed]
- Farrance, I.; Frenkel, R. Uncertainty in Measurement: A Review of Monte Carlo Simulation Using Microsoft Excel for the Calculation of Uncertainties Through Functional Relationships, Including Uncertainties in Empirically Derived Constants. Clin. Biochem. Rev. 2014, 35, 37–61. [Google Scholar] [PubMed]
- Belotti, F.; Deb, P.; Manning, W.G.; Norton, E.C. twopm: Two-part models. Stata J. 2015, 15, 3–20. [Google Scholar] [CrossRef]
- Johnston, D.A.; Harvey, S.B.; Glozier, N.; Calvo, R.A.; Christensen, H.; Deady, M. The relationship between depression symptoms, absenteeism and presenteeism. J. Affect. Disord. 2019, 256, 536–540. [Google Scholar] [CrossRef]
- Baptista, M.C.; Burton, W.N.; Nahas, A.K.; Wang, Y.P.; Viana, M.C.; Andrade, L.H. Absenteeism and Presenteeism Associated with Common Health Conditions in Brazilian Workers. J. Occup. Environ. Med. 2019, 61, 303–313. [Google Scholar] [CrossRef]
- Hilton, M.F.; Scuffham, P.A.; Sheridan, J.; Cleary, C.M.; Whiteford, H.A. Mental ill-health and the differential effect of employee type on absenteeism and presenteeism. J. Occup. Environ. Med. 2008, 50, 1228–1243. [Google Scholar] [CrossRef]
- Lerner, D.; Adler, D.A.; Chang, H.; Berndt, E.R.; Irish, J.T.; Lapitsky, L.; Hood, M.Y.; Reed, J.; Rogers, W.H. The clinical and occupational correlates of work productivity loss among employed patients with depression. J. Occup. Environ. Med. 2004, 46, 46–55. [Google Scholar] [CrossRef]
- Cuijpers, P.; Smit, F.; Oostenbrink, J.; De Graaf, R.; Ten Have, M.; Beekman, A. Economic costs of minor depression: A population-based study. Acta Psychiatr. Scand. 2007, 115, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Wee, L.H.; Yeap, L.L.L.; Chan, C.M.H.; Wong, J.E.; Jamil, N.A.; Swarna Nantha, Y.; Ching, S.S. Anteceding factors predicting absenteeism and presenteeism in urban area in Malaysia. BMC Public Health 2019, 19, 540. [Google Scholar] [CrossRef] [PubMed]
- Evans-Lacko, S.; Knapp, M. Global patterns of workplace productivity for people with depression: Absenteeism and presenteeism costs across eight diverse countries. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 1525–1537. [Google Scholar] [CrossRef] [PubMed]
- Ebert, A.; Strehlow, K. Does on-site chaplaincy enhance the health and well being of fly-in, fly-out (FIFO) personnel? Health Promot. J. Aust. 2017, 28, 118–122. [Google Scholar] [CrossRef]
- Merrill, R.M.; Aldana, S.G.; Pope, J.E.; Anderson, D.R.; Coberley, C.R.; Whitmer, R.W. Presenteeism according to healthy behaviors, physical health, and work environment. Popul. Health Manag. 2012, 15, 293–301. [Google Scholar] [CrossRef]
- Van den Heuvel, S.G.; Geuskens, G.A.; Hooftman, W.E.; Koppes, L.L.; Van den Bossche, S.N. Productivity loss at work; health-related and work-related factors. J. Occup. Rehabil. 2010, 20, 331–339. [Google Scholar] [CrossRef]
- Ishibashi, Y.; Shimura, A. Association between work productivity and sleep health: A cross-sectional study in Japan. Sleep Health 2020, 6, 270–276. [Google Scholar] [CrossRef]
- Rosekind, M.R.; Gregory, K.B.; Mallis, M.M.; Brandt, S.L.; Seal, B.; Lerner, D. The cost of poor sleep: Workplace productivity loss and associated costs. J. Occup. Environ. Med. 2010, 52, 91–98. [Google Scholar] [CrossRef]
- Dorrian, J.; Baulk, S.D.; Dawson, D. Work hours, workload, sleep and fatigue in Australian Rail Industry employees. Appl. Ergon. 2011, 42, 202–209. [Google Scholar] [CrossRef]
- Mulgrew, A.T.; Ryan, C.F.; Fleetham, J.A.; Cheema, R.; Fox, N.; Koehoorn, M.; Fitzgerald, J.M.; Marra, C.; Ayas, N.T. The impact of obstructive sleep apnea and daytime sleepiness on work limitation. Sleep Med. 2007, 9, 42–53. [Google Scholar] [CrossRef]
- Doi, Y.; Minowa, M.; Tango, T. Impact and correlates of poor sleep quality in Japanese white-collar employees. Sleep 2003, 26, 467–471. [Google Scholar] [CrossRef] [PubMed]
- Kerner, I.; Rakovac, M.; Lazinica, B. Leisure-time physical activity and absenteeism. Arh. Za Hig. Rada I Toksikol. 2017, 8, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Cancelliere, C.; Cassidy, J.D.; Ammendolia, C.; Côté, P. Are workplace health promotion programs effective at improving presenteeism in workers? A systematic review and best evidence synthesis of the literature. BMC Public Health 2011, 11, 395. [Google Scholar] [CrossRef] [PubMed]
- Stults-Kolehmainen, M.A.; Sinha, R. The effects of stress on physical activity and exercise. Sports Med. 2014, 44, 81–121. [Google Scholar] [CrossRef]
- Masi, D.A.; Jacobson, J.M. Outcome measurements of an integrated employee assistance and work-life program. Res. Soc. Work Pract. 2003, 13, 451–467. [Google Scholar] [CrossRef]
- Pitt-Catsouphes, M.; James, J.B.; Matz-Costa, C. Workplace-based health and wellness programs: The intersection of aging, work, and health. Gerontologist 2015, 55, 262–270. [Google Scholar] [CrossRef]
- Plaisier, I.; de Graaf, R.; de Bruijn, J.; Smit, J.; van Dyck, R.; Beekman, A.; Penninx, B. Depressive and anxiety disorders on-the-job: The importance of job characteristics for good work functioning in persons with depressive and anxiety disorders. Psychiatry Res. 2012, 200, 382–388. [Google Scholar] [CrossRef]
| Health Condition | High-Risk Criteria | Low-Risk Criteria |
|---|---|---|
| Psychological distress | K10 scores of 22–29 (high) and 30–50 (very high) levels | K10 scores of 10–15 (low) and 16–21 (medium) levels |
| Poor physical health | Scores of less than 50 on the PCS of SF-8 Health scale | Scores of less than 50 on the PCS of SF-8 Health scale |
| Poor sleep condition | Sleep duration less than 7 h and/or poor sleep quality | Sleep duration of 7 or more hours and/or better sleep quality |
| Risky alcohol use | AUDIT-C score of ≥4 among men and ≥3 among women | AUDIT-C score of <4 among men and <3 among women |
| Smoking | Currently smoking | Non-or ex-smokers |
| Insufficient physical activity | Metabolic equivalent minutes (MET minutes) of less than 600 per week | Metabolic equivalent minutes (MET minutes) of ≥ 600 per week |
| Weight problem | BMI < 18.5(underweight), BMI = 25–29.9 (overweight) and BMI ≥ 30 (obese) | BMI = 18.5–24.9 |
| Poor diet/nutrition | Intake of less than 2 servings of fruits and/or less than 5 servings of vegetables | Intake of more than 2 servings of fruits and/or 5 servings of vegetables |
| Personal Characteristics | Frequency (n) | Percent (%) |
|---|---|---|
| Age in year | ||
| ≤34 | 82 | 38.0 |
| 35–44 | 67 | 31.0 |
| ≥45 | 67 | 31.0 |
| Gender | ||
| Male | 143 | 66.2 |
| Female | 73 | 33.8 |
| Ethnicity | ||
| Caucasian/white | 183 | 84.7 |
| Other | 33 | 15.3 |
| Relationship status | ||
| Single/never married | 43 | 19.9 |
| Married | 93 | 43.1 |
| Separated/divorced/widowed | 25 | 11.6 |
| De-facto/co-habiting/civil partnership | 52 | 23.0 |
| Other | 3 | 1.4 |
| Educational status | ||
| Primary/secondary education and equivalent | 70 | 32.4 |
| Trade/apprentice | 45 | 20.8 |
| TAFE/college | 60 | 27.8 |
| Bachelor’s degree | 30 | 13.9 |
| Postgraduate degree | 11 | 5.1 |
| FIFO role | ||
| Management/administration/services | 54 | 25.0 |
| Professional | 27 | 12.5 |
| Maintenance/technician | 39 | 18.1 |
| Production/drilling/construction/labourer | 45 | 20.8 |
| Machinery operator and driver | 35 | 16.2 |
| Catering | 10 | 4.6 |
| Other | 6 | 2.8 |
| Shift patterns | ||
| Rotation shift (mixture of day/night shift) | 124 | 57.4 |
| Regular shift (fixed day/night) | 92 | 42.6 |
| Shift length | ||
| <12 h | 30 | 13.9 |
| ≥12 h | 186 | 86.1 |
| Consecutive days spent at work | ||
| <8 days | 43 | 19.9 |
| 8–14 days | 156 | 72.2 |
| 15+ days | 17 | 7.9 |
| Consecutive days spent at home | ||
| <8 days | 187 | 86.6 |
| 8–14 days | 29 | 13.4 |
| FIFO duration | ||
| <5 yrs | 87 | 40.3 |
| 5–9 yrs | 46 | 21.3 |
| 10+ yrs | 83 | 38.4 |
| Health Condition | High-Risk Frequency (n) | Percent (%) |
|---|---|---|
| Poor sleep condition | 139 | 64.4 |
| Risky alcohol use | 74 | 34.3 |
| Currently smoking | 57 | 26.4 |
| Poor diet | 208 | 96.3 |
| Weight problem | 161 | 74.5 |
| Insufficient physical activity | 58 | 26.9 |
| Poor physical health | 19 | 8.8 |
| Psychological distress | 72 | 33.3 |
| How many health conditions reported | ||
| 1 | 5 | 2.3 |
| 2 | 39 | 18.1 |
| 3 | 67 | 31.0 |
| 4 | 53 | 24.5 |
| 5 or more | 52 | 24.1 |
| Measures | Frequency (n), Mean ± SD | Percent (%) |
|---|---|---|
| Absenteeism | ||
| Yes | 44 | 20.4 |
| No | 172 | 79.6 |
| Work hours missed per 4 weeks | 16.07 ± 20.34 h (range 1–96) | |
| Average absenteeism rate (per week) | 1.70 ± 5.36% (range 0–33.3) | |
| Presenteeism | ||
| Yes | 116 | 53.7 |
| No | 100 | 46.3 |
| Reduced work productivity (ranked 0–10) per 4 weeks | ||
| 0 | 100 | 46.3 |
| 1–2 | 64 | 29.6 |
| 3–4 | 32 | 14.8 |
| ≥5 | 20 | 9.3 |
| Average presenteeism rate (per week) | 3.84 ± 5.33% (range 0–22.5) | |
| Average total productivity loss rate (per week) | 7.48 ± 10.20% (range 0–40) |
| Percent Absenteeism Due to Health | Percent Presenteeism Due to Health | Percent Total Productivity Loss | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Health Conditions | High Risk | Low Risk | Excess | Cost Per Year | High Risk | Low Risk | Excess | Cost per year | High Risk | Low Risk | Excess | Cost Per Year |
| Poor sleep condition | 2.07 | 1.04 | 1.03 | 1383.53 | 4.64 | 2.40 | 2.24 ** | 3008.84 | 6.43 | 3.36 | 3.07 * | 4123.72 |
| Risky alcohol use | 1.75 | 1.68 | 0.07 | 94.03 | 4.12 | 3.70 | 0.42 | 564.16 | 5.71 | 5.14 | 0.57 | 765.64 |
| Current smoking | 1.99 | 1.60 | 0.39 | 523.86 | 5.70 | 3.18 | 2.52 ** | 3384.94 | 7.37 | 4.61 | 2.77 * | 3720.75 |
| Poor diet | 1.77 | 0.07 | 1.70 | 2283.49 | 3.92 | 1.88 | 2.04 | 2740.19 | 5.47 | 1.94 | 3.53 | 4741.61 |
| Weight problems | 1.77 | 1.51 | 0.26 | 349.24 | 4.02 | 3.32 | 0.70 | 940.26 | 5.56 | 4.69 | 0.86 | 1155.18 |
| Insufficient physical activity | 2.73 | 1.32 | 1.41 * | 1893.96 | 5.13 | 3.37 | 1.76 | 2364.09 | 7.52 | 4.54 | 2.98 * | 4002.83 |
| Poor physical health | 4.23 | 1.46 | 2.77 * | 3720.75 | 11.71 | 3.08 | 8.63 *** | 11,592.09 | 15.11 | 4.40 | 10.71 *** | 14,386.01 |
| Psychological distress | 3.08 | 1.01 | 2.07 ** | 2789.49 | 7.01 | 2.26 | 4.75 *** | 6380.35 | 9.64 | 3.19 | 6.45 *** | 8663.85 |
| Health Conditions | Prevalence of High Risk (%) | Excess Absenteeism (%) | Lost Productivity Cost Per 1000 (AUD) | Excess Presenteeism (%) | Lost Productivity Cost Per 1000 (AUD) | Excess Total Productivity Loss (%) | Lost Productivity Cost per 1000 (AUD) |
|---|---|---|---|---|---|---|---|
| Poor sleep condition | 64.4 | 1.41 | 1,219,708.39 | 2.17 * | 1,877,139.86 | 3.28 * | 2,837,335.82 |
| Risky alcohol use | 34.3 | 0.93 | 428,477.58 | 1.48 | 681,878.29 | 2.26 | 1,041,246.58 |
| Smoking | 26.4 | −0.07 | - | 1.26 | 446,812.69 | 1.03 | 365,251.65 |
| Poor diet | 96.3 | 3.20 | 4,139,303.73 | 4.26 * | 5,510,448.09 | 6.85 * | 8,860,697.05 |
| Weight problems | 74.5 | 1.00 | 1,000,707.84 | 1.50 | 1,501,061.76 | 2.21 | 2,211,564.33 |
| Insufficient physical activity | 26.9 | 1.64 | 592,580.23 | 2.54 ** | 917,776.70 | 3.88 ** | 1,401,958.10 |
| Poor physical health | 8.8 | 2.79 | 329,790.32 | 9.05 *** | 1,069,749.96 | 11.10 *** | 1,312,069.02 |
| Psychological distress | 33.3 | 2.47 * | 1,104,821.75 | 4.64 *** | 2,075,454.63 | 6.56 *** | 2,934,263.44 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asare, B.Y.-A.; Makate, M.; Powell, D.; Kwasnicka, D.; Robinson, S. Cost of Health-Related Work Productivity Loss among Fly-In Fly-Out Mining Workers in Australia. Int. J. Environ. Res. Public Health 2022, 19, 10056. https://doi.org/10.3390/ijerph191610056
Asare BY-A, Makate M, Powell D, Kwasnicka D, Robinson S. Cost of Health-Related Work Productivity Loss among Fly-In Fly-Out Mining Workers in Australia. International Journal of Environmental Research and Public Health. 2022; 19(16):10056. https://doi.org/10.3390/ijerph191610056
Chicago/Turabian StyleAsare, Bernard Yeboah-Asiamah, Marshall Makate, Daniel Powell, Dominika Kwasnicka, and Suzanne Robinson. 2022. "Cost of Health-Related Work Productivity Loss among Fly-In Fly-Out Mining Workers in Australia" International Journal of Environmental Research and Public Health 19, no. 16: 10056. https://doi.org/10.3390/ijerph191610056
APA StyleAsare, B. Y.-A., Makate, M., Powell, D., Kwasnicka, D., & Robinson, S. (2022). Cost of Health-Related Work Productivity Loss among Fly-In Fly-Out Mining Workers in Australia. International Journal of Environmental Research and Public Health, 19(16), 10056. https://doi.org/10.3390/ijerph191610056







