How the Cognitive Status of Older People Affects Their Care Dependency Level and Needs: A Cross-Sectional Study
Abstract
:1. Introduction
- To evaluate the functional status of older people with cognitive impairment versus those without cognitive impairment.
- To evaluate the degree and aspects of dependency of older people with cognitive impairment versus those without cognitive impairment.
2. Materials and Methods
2.1. Participants and Setting
2.2. Measurements and Procedure
2.3. Statistical Analysis
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Population Projection 2014–2050. Statistical Analyses and Studies; Central Statistical Office: Warsaw, Poland, 2014. [Google Scholar]
- Rodrigues, R.; Huber, M.; Lamura, G. (Eds.) Facts and Figures on healthy Ageing and Long-Term Care Europe and North America; Occasional Reports Series 8; European Centre: Vienna, Austria, 2012. [Google Scholar]
- Błędowski, P.; Chudek, J.; Grodzicki, T.; Gruchała, M.; Mossakowska, M.; Więcek, A.; Zdrojewski, T. Wyzwania dla polityki zdrowotnej i społecznej. Geneza projektów badawczych Polsenior 1 i Polsenior 2. In Badanie Poszczególnych Obszarów Stanu Zdrowia Osób Starszych, w tym Jakości Życia Związanej ze Zdrowiem; Błędowski, P., Grodzicki, T., Mossakowska, M., Zdrojewski, T., Eds.; Gdański Uniwersytet Medyczny: Gdańsk, Poland, 2021; pp. 19–35. [Google Scholar]
- Czapiński, J.; Panek, T. Social diagnosis 2015: Objective and subjective quality of life in Poland. Contemp. Econ. 2015, 9, 55. [Google Scholar]
- Wieczorowska-Tobis, K. Typowe cechy medycyny geriatrycznej. In Geriatria i Pielęgniarstwo Geriatryczne; Wieczorowska-Tobis, K., Talarska, D., Eds.; PZWL: Warszawa, Poland, 2017; pp. 93–98. [Google Scholar]
- Wizner, B.; Skalska, A.; Klich-Rączka, A.; Piotrowicz, K.; Grodzicki, T. Ocena stanu funkcjonalnego u osób w starszym wieku. In Aspekty Medyczne, Psychologiczne, Socjologiczne i Ekonomiczne Starzenia się Ludzi w Polsce; Mossakowska, M., Więcek, A., Błędowski, P., Eds.; Polsenior, Termedia: Poznań, Poland, 2012; pp. 81–94. [Google Scholar]
- Wizner, B.; Kujawska-Danecka, H.; Hajduk, A.; Wierzba, K.; Jagiełło, K.; Wieczorowska-Tobis, K. Ocena stanu funkcjonalnego. In Badanie Poszczególnych Obszarów Stanu Zdrowia Osób Starszych, w tym Jakości Życia Związanej ze Zdrowiem; Błędowski, P., Grodzicki, T., Mossakowska, M., Zdrojewski, T., Eds.; Gdański Uniwersytet Medyczny: Gdańsk, Poland, 2021; pp. 181–202. [Google Scholar]
- Ćwirlej-Sozańska, A.; Wiśniowska-Szurlej, A.; Wilmowska-Pietruszyńska, A.; Sozański, B. Determinants of ADL and IDAL disability in older adults in southeastern Poland. BMC Geriatr. 2019, 19, 297. [Google Scholar] [CrossRef]
- Ahrenfeldt, L.J.; Lindahl-Jacobsen, R.; Rizzi, S.; Thinggaard, M.; Kaare Christensen, K.; Vaupel, J.W. Comparison of cognitive and physical functioning of Europeans in 2004–05 and 2013. Int. J. Epidemiol. 2018, 47, 1518–1528. [Google Scholar] [CrossRef] [PubMed]
- Klich-Rączka, A.; Siuda, J.; Piotrowicz, K.; Boczarska-Jedynak, M.; Skalska, A.; Krzystanek, E.; Wizner, B.; Świat, M.; Skrzypek, M.; Opala, G.; et al. Zaburzenia funkcji poznawczych u osób w starszym wieku. In Aspekty Medyczne, Psychologiczne, Socjologiczne i Ekonomiczne Starzenia się Ludzi w Polsce; Mossakowska, M., Więcek, A., Błędowski, P., Eds.; Polsenior, Termedia: Poznań, Poland, 2012; pp. 109–121. [Google Scholar]
- Klich-Rączka, A.; Piotrowicz, K.; Kujawska-Danecka, H.; Zagożdżon, P.; Mossakowska, M. Zaburzenia funkcji poznawczych. In Badanie Poszczególnych Obszarów Stanu Zdrowia osób Starszych, w tym Jakości życia Związanej ze Zdrowiem; Błędowski, P., Grodzicki, T., Mossakowska, M., Zdrojewski, T., Eds.; Gdański Uniwersytet Medyczny: Gdański, Poland, 2021; pp. 293–310. [Google Scholar]
- Schüssler, S.; Lohrman, C. Change in care dependency and nursing care problems in nursing home residents with and without dementia: A2-Year Panel Study. PLoS ONE 2015, 10, e0141653. [Google Scholar] [CrossRef] [PubMed]
- Dziechciaż, M.; Chmielewski, J. Cognitive disorders in people over 65 in home environment. J. Neurosci. Nurs. 2021, 10, 65–70. [Google Scholar]
- Janssen, D.J.A.; Wouters, E.F.M.; Schols, J.M.G.A.; Spruit, M.A. Care dependency independently predicts two-year survival in outpatients with advanced chronic organ failure. J. Am. Med. Dir. Assoc. 2013, 14, 194–198. [Google Scholar] [CrossRef]
- Dijkstra, A.; Buist, G.; Moorer, P.; Dassen, T. A reliability and utility study of the care dependency scale. Scand. J. Caring Sci. 2000, 14, 155–161. [Google Scholar] [CrossRef]
- Edjolo, A.; Proust-Lima, C.; Delva, F.; Dartigues, J.F.; Pérès, K. Natural history of dependency in the elderly: A 24-year population-based study using a longitudinal item response theory model. Am. J. Epidemiol. 2016, 183, 277–285. [Google Scholar] [CrossRef]
- Dijkstra, A.; Suzuki, M.; Kazimier, H.; Fujiwara, M.; Saegusa, T. Relationship between care dependency and behavioral symptoms among elderly in-patients with Alzheimer’s disease in Japan and the Netherlands. SAGE Open Med. 2015, 3. [Google Scholar] [CrossRef]
- Henskens, M.; Nauta, I.M.; Drost, K.T.; Milders, M.V.; Scherder, E.J.A. Predictors of care dependency in nursing home residents with moderate to severe dementia: A cross-sectional study. Int. J. Nurs. Stud. 2019, 92, 47–54. [Google Scholar] [CrossRef]
- Schüssler, S.; Dassen, T.; Lohrman, C. Care dependency and nursing care problems in nursing home residents with and without dementia: A cross-sectional study. Aging Clin. Exp. Res. 2016, 28, 973–982. [Google Scholar] [CrossRef] [PubMed]
- Cohen, C.; Pereira, F.; Kampel, T.; Bélanger, L. Integration of family caregivers in delirium prevention care for hospitalized older adults: A case study analysis. J. Adv. Nurs. 2021, 77, 318–330. [Google Scholar] [CrossRef] [PubMed]
- Doroszkiewicz, H.; Sierakowska, M.; Muszalik, M. Utility of the care dependency scale in predicting care needs and health risk of elderly patients admitted to a geriatric unit: A cross-sectional study of 200 consecutive patients. Clin. Interv. Aging 2018, 13, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Rubenstein, L.Z.; Wieland, D.; Bernabei, R. Geriatric assessment technology: International research perspectives. Aging 1995, 7, 153–158. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index. Md State Med. J. 1965, 14, 61–65. [Google Scholar]
- Fillenbaum, C.G.; Smyer, M.A. The development, validity and reliability of OARS multidimensional functional assessment questionnaire. J. Gerontol. 1981, 36, 428–434. [Google Scholar] [CrossRef]
- Tinetti, M.E. Performance-oriented assessment of mobility problems in elderly patients. J. Am. Geriatr. Soc. 1986, 34, 119–126. [Google Scholar] [CrossRef]
- Norton, D.; McLaren, R.; Exton-Smith, A.N. An Investigation of Geriatric Nursing Problems in Hospital; Churchill Livingstone: London, UK, 1962. [Google Scholar]
- Sheikh, J.I.; Yesavage, J.A. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clin. Gerontol. 1986, 5, 165–173. [Google Scholar]
- Dijkstra, A.; Muszalik, M.; Kędziora-Kornatowska, K.; Kornatowski, T. Care Dependency Scale—psychometric testing of the Polish version. Scand. J. Caring Sci. 2010, 24, 62–66. [Google Scholar] [CrossRef]
- Skalska, A. Kompleksowa ocena geriatryczna. In Geriatria z Elementami Gerontologii Ogólnej; Grodzicki, T., Kocemba, J., Skalska, A., Eds.; Via Medica: Gdańsk, Poland, 2006; pp. 68–75. [Google Scholar]
- Kim, E.J. Factors influencing care dependency in patients with dementia. Taehan Kanho Hakhoe Chi 2003, 33, 705–712. [Google Scholar] [CrossRef]
- Henskens, M.; Nauta, I.M.; Vrijkotte, S.; Drost, K.T.; Milders, M.V.; Scherder, E.J.A. Mood and behavioral problems are important predictors of quality of life of nursing home residents with moderate to severe dementia: A cross-sectional study. PLoS ONE 2019, 14, e0223704. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.; Pachana, N.A.; Beattie, E.; Fielding, E.; Ramis, M.A. Effectiveness of interventions to improve family-staff relationships in the care of people with dementia in residential aged care: A systematic review protocol. JBI Database Syst. Rev. Implemen. Rep. 2015, 13, 52–63. [Google Scholar] [CrossRef] [PubMed]
- Risco, E.; Cabrera, E.; Jolley, D.; Stephan, A.; Karlsson, S.; Verbeek, H.; Saks, K.; Hupli, M.; Sourdet, S.; Zabalegui, A. The association between physical dependency and the presence of neuropsychiatric symptoms, with the admission of people with dementia to a long-term care institution: A prospective observational cohort study. Int. J. Nurs. Stud. 2015, 52, 980–987. [Google Scholar] [CrossRef]
- Rocha, V.; Marques, A.; Pinto, M.; Sousa, L.; Figueiredo, D. People with dementia in long-term care facilities: An exploratory study of their activities and participation. Disabil. Rehabil. 2013, 35, 1501–1508. [Google Scholar] [CrossRef]
| Characteristics | Severe Cognitive Impairment | Moderate Cognitive Impairment | No Impairment | p-Value |
|---|---|---|---|---|
| n = 49 | n = 53 | n = 98 | ||
| Age in years | ||||
| Mean ± SD | 83.6 ± 5.9 | 82.3 ± 6.0 | 80.6 ± 7.0 | 0.011 |
| Min. | 66 | 68 | 65 | |
| Max. | 92 | 93 | 101 | |
| Female (%) | 61.2 | 79.2 | 67.3 | 0.128 |
| Marital status (%) | ||||
| married | 45.8 | 28.6 | 32.4 | 0.310 |
| widowed | 54.2 | 69.1 | 60.8 | |
| divorced | 0.0 | 2.3 | 6.8 | |
| Dwelling (%) | ||||
| alone | ||||
| with a mate | 35.4 | 47.6 | 33.3 | |
| with children | 41.7 | 21.4 | 30.7 | 0.333 |
| in an institution | 22.9 | 31 | 32 | |
| 0.0 | 0.0 | 4.0 | ||
| Does the person feel lonely? | ||||
| often | 63.2 | 84.9 | 65.3 | 0.087 |
| Health self-assessment (%) | ||||
| very good/good | 24.5 | 45.3 | 50.0 | 0.007 |
| poor/very poor | 75.5 | 54.7 | 50.0 | |
| Problem with locomotion (%) | 83.7 | 62.3 | 65.3 | 0.001 |
| Risk of fall (%) | 75.6 | 56.6 | 48.0 | 0.019 |
| Use of glasses (yes) (%) | 42.9 | 41.5 | 37.8 | 0.930 |
| Use of hearing aid (yes) (%) | 53.1 | 37.8 | 40.8 | 0.207 |
| Barthel Index, mean ± SD | ||||
| (0–100) | 67.7 ± 30.2 | 75.8 ± 26.6 | 82.3 ± 23.6 | 0.001 |
| I-ADL, | ||||
| mean ± SD (0–12) | 4.7 ± 3.4 | 5.8 ± 3.9 | 7.6 ± 3.4 | 0.000 |
| GDS, | ||||
| mean ± SD (0–15) | 7.3 ± 3.7 | 6.3 ± 3.6 | 5.3 ± 3.7 | 0.013 |
| AMTS, | ||||
| mean ± SD (0–10) | 2.3 ± 0.8 | 5.4 ± 0.8 | 8.8 ± 1.1 | 0 |
| Norton scale, mean ± SD (0–20) | 15.4 ± 3.3 | 16.3 ± 3.1 | 17.3 ± 2.7 | 0.001 |
| Characteristics | Severe Cognitive Impairment | Moderate Cognitive Impairment | No Impairment | p-Value |
|---|---|---|---|---|
| n = 49 | n = 53 | n = 98 | ||
| Care Dependency Scale, | ||||
| mean ± SD (15–75) | 46.3 (±16.1) | 53.6 (±14.3) | 60.8 (±12.6) | 0.0000 |
| Severity level of care dependency, | ||||
| n (%) | ||||
| 1 = completely care dependent | 6 (12.2) | 3 (5.7) | 1 (1.0) | 0.0001 |
| 2 = to a great extent care dependent | 15 (30.6) | 10 (18.9) | 13 (13.3) | |
| 3 = partially care dependent | 17 (34.8) | 18 (34.0) | 17 (17.4) | |
| 4 = to a limited extent care dependent | 5 (10.2) | 17 (32.0) | 39 (39.7) | |
| 5 = almost independent | 6 (12.2) | 5 (9.4) | 28 (28.6) | |
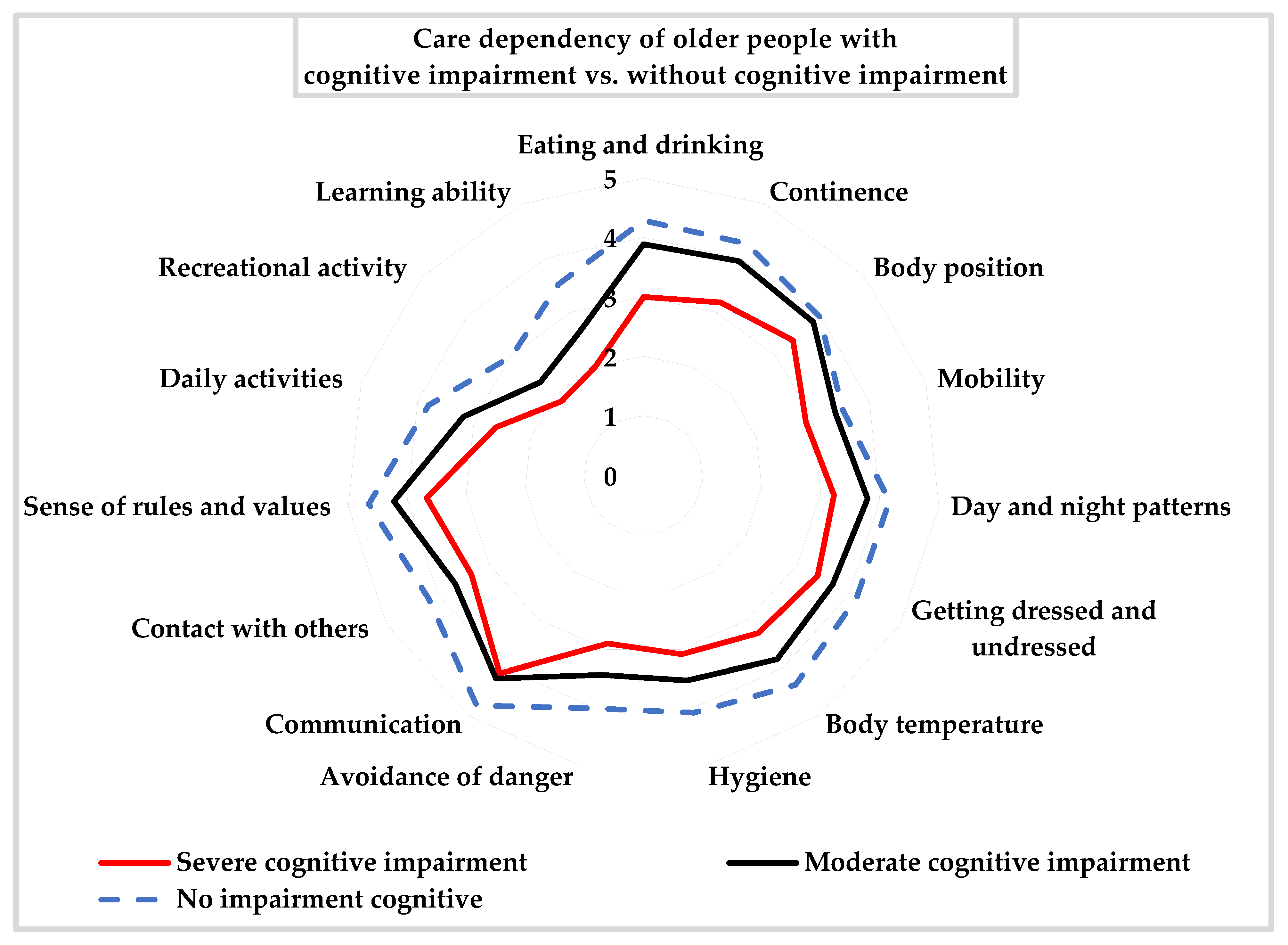
| Care Dependency Scale, | ||||
| mean ± SD | ||||
| Eating and drinking | 3.4 ± 1.5 | 3.9 ± 1.3 | 4.3 ± 1.1 | 0.0004 |
| mean ± SD (1–5) | ||||
| Continence, mean ± SD (1–5) | 3.2 ± 1.4 | 3.9 ± 1.3 | 4.3 ± 1.2 | 0.0000 |
| Body posture, mean ± SD (1–5) | 3.4 ± 1.3 | 3.8 ± 1.1 | 4.0 ± 1.1 | 0.0129 |
| Mobility, mean ± SD (1–5) | 2.9 ± 1.4 | 3.4 ± 1.4 | 3.5 ± 1.3 | 0.0248 |
| Day/night pattern, mean ± SD (1–5) | 3.2 ± 1.4 | 3.8 ± 1.1 | 4.2 ± 1.0 | 0.0001 |
| Getting dressed and undressed, mean ± SD (1–5) | 3.4 ± 1.4 | 3.7 ± 1.3 | 4.1 ± 1.2 | 0.0009 |
| Body temperature, | 3.3 ± 1.2 | 3.8 ± 1.2 | 4.4 ± 0.9 | 0.0000 |
| mean ± SD (1–5) | ||||
| Hygiene, mean ± SD (1–5) | 3.1 ± 1.5 | 3.5 ± 1.3 | 4.1 ± 1.2 | 0.0001 |
| Avoidance of danger, | 2.9 ± 1.3 | 3.4 ± 1.3 | 4.0 ± 1.2 | 0.0000 |
| mean ± SD (1–5) | ||||
| Communications, mean ± SD (1–5) | 4.1 ± 1.0 | 4.2 ± 1.0 | 4.8 ± 0.5 | 0.0000 |
| Contact with others, mean ± SD (1–5) | 3.3 ± 1.3 | 3.7 ± 1.3 | 4.2 ± 1.1 | 0.0004 |
| Sense of rules and values, mean ± SD (1–5) | 3.6 ± 1.4 | 4.2 ± 0.9 | 4.7 ± 0.7 | 0.0000 |
| Daily activities, mean ± SD (1–5) | 2.6 ± 1.3 | 3.2 ± 1.2 | 3.8 ± 1.3 | 0.0000 |
| Recreational activities, mean ± SD (1–5) | 1.9 ± 1.3 | 2.3 ± 1.5 | 3.0 ± 1.6 | 0.0001 |
| Learning activities, mean ± SD (1–5) | 2.0 ± 1.0 | 2.6 ± 1.1 | 3.5 ± 1.0 | 0.0000 |
| Number of care needs CDS, mean ± SD | ||||
| Physical care needs | 4.7 ± 3.2 | 3.2 ± 3.2 | 2.3 ± 2.9 | 0.0000 |
| Psychological care needs | 1.7 ± 0.7 | 1.5 ± 0.7 | 0.9 ± 0.8 | 0.0000 |
| Social care needs | 1.7 ± 1.5 | 1.2 ± 1.4 | 0.6 ± 1.0 | 0.0000 |
| Sum score of biopsychological care needs, CDS, mean ± SD | 8.0 ± 4.9 | 5.9 ± 4.8 | 3.8 ± 4.3 | 0.0000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doroszkiewicz, H. How the Cognitive Status of Older People Affects Their Care Dependency Level and Needs: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 10257. https://doi.org/10.3390/ijerph191610257
Doroszkiewicz H. How the Cognitive Status of Older People Affects Their Care Dependency Level and Needs: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(16):10257. https://doi.org/10.3390/ijerph191610257
Chicago/Turabian StyleDoroszkiewicz, Halina. 2022. "How the Cognitive Status of Older People Affects Their Care Dependency Level and Needs: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 16: 10257. https://doi.org/10.3390/ijerph191610257





