Identifying and Predicting Healthcare Waste Management Costs for an Optimal Sustainable Management System: Evidence from the Greek Public Sector
Abstract
:1. Introduction
2. Healthcare/Medical Wastes Quantities and Generation Rates
2.1. Indicative Evidence from Around the World
2.2. Evidence from Greece
3. Materials and Methods
3.1. Study Design, Sampling
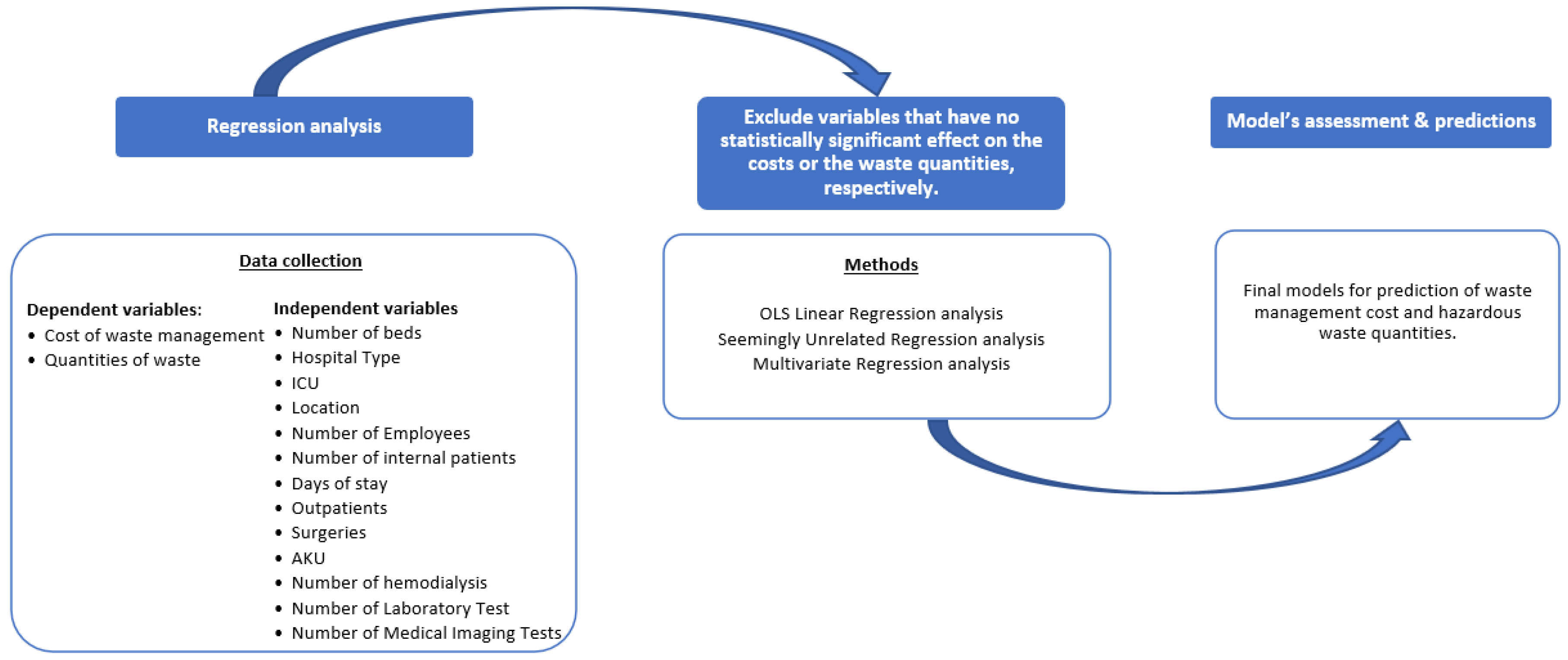
3.2. Methods
4. Results
- A.
- LogWasteCost = 8.013 + 0.024 ∗ Beds + b2 ∗ HospitalType + b3 ∗ HospitalType ∗ Beds + b4 ∗ ICU + 0.0000265 ∗ Inpatients − 0.000006 ∗ Days + 0.0030473 ∗ Employees.
- B.
- LogWasteKilos = 6.711 + 0.0268 ∗ Beds + b2 ∗ HospitalType + b3 ∗ HospitalType ∗ Beds + b4 ∗ ICU + 0.0000337 ∗ Inpatients − 0.0000106 ∗ Days + 0.0024858 ∗ Employees − 0.0000331 ∗ S.Surgeries.
Model Assessment
5. Discussion
- A proper and customize sustainable waste management system should exist and function;
- Proper training regarding the waste management and the occupational safety of healthcare professionals;
- The implementation of a waste management policy and a customized Standard Operational Procedure (SOP);
- A review of the current legislation and relating policymaking;
- The implementation of new medical waste treatment technologies;
- Recycling of materials;
- The need for standardized and mutually accepted guidelines in national and international level of HCWs;
- A minimization of the costs and related risks from HCWs.
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mehra, R.; Sharma, M.K. Measures of Sustainability in Healthcare. Sustain. Anal. Modeling 2021, 1, 100001. [Google Scholar] [CrossRef]
- WHO. Global Spending on Health: Weathering the Storm. 2020. Available online: https://www.who.int/publications/i/item/9789240017788 (accessed on 6 June 2022).
- Khairunnisa, R.A.; Ulfa, M.; Azizi, M.; Setyonugroho, W. A Future Green and Healthy Hospital: A Review Article. Proc. Int. Healthc. Facil. 2021, 1, 82–94. Available online: http://thejournalish.com/ojs/index.php/ichf/article/view/114 (accessed on 6 June 2022).
- Zhu, Q.; Johnson, S.; Sarkis, J. Lean six sigma and environmental sustainability: A hospital perspective. Supply Chain. Forum Int. J. 2018, 19, 25–41. [Google Scholar] [CrossRef]
- Marimuthu, M.; Paulose, H. Emergence of sustainability-based approaches in healthcare: Expanding research and practice. Procedia Soc. Behav. Sci. 2016, 224, 554–561. [Google Scholar] [CrossRef] [Green Version]
- Hensher, M. Incorporating environmental impacts into the economic evaluation of health care systems: Perspectives from ecological economics. Resour. Conserv. Recycl. 2020, 154, 104623. [Google Scholar] [CrossRef]
- Sepetis, A.; Goula, A.; Stasinopoulos, V.; Kastanioti, C.; Stasinopoulos, D. The implementation of Voluntary Environmental Agreements and Sustainable Balanced Scorecard in the Health Care Region of Greece. Int. J. Biol. Biomed. 2020, 5, 1–10. [Google Scholar]
- Karliner, J.; Slotterback, S.; Boyd, R.; Ashby, B.; Steele, K.; Wang, J. Healthcare’s climate footprint: The health sector contribution and opportunities for action. Eur.J. Public Health 2020, 30, ckaa165–ckaa843. [Google Scholar] [CrossRef]
- Health Care without Harm. Our New Road Map for Zero Emissions Health Care. Available online: https://noharm-global.org/articles/news/global/our-new-road-map-zero-emissions-health-care (accessed on 6 June 2022).
- Razzaq, A.; Sharif, A.; Najmi, A.; Tseng, M.L.; Lim, M.K. Dynamic and causality interrelationships from municipal solid waste recycling to economic growth, carbon emissions and energy efficiency using a novel bootstrapping autoregressive distributed lag. Resour. Conserv. Recycl. 2021, 166, 105372. [Google Scholar] [CrossRef]
- Sun, Y.; Duru, O.A.; Razzaq, A.; Dinca, M.S. The asymmetric effect eco-innovation and tourism towards carbon neutrality target in Turkey. J. Environ. Manag. 2021, 299, 113653. [Google Scholar] [CrossRef]
- Chartier, Y.; Emmanuel, J.; Pieper, U.; Pruss, A.; Rushbrook, P.; Stringer, R.; Townend, W.; Wilbum, S.; Zghondi, R. Safe Management of Wastes from Healthcare Activities, 2nd ed.; Chartier, Y., Emmanuel, J., Pieper, U., Eds.; WHO: Geneva, Switzerland, 2014; Volume 2, Available online: https://www.who.int/publications/i/item/9789241548564/ (accessed on 6 June 2022).
- WHO. WHO Calls for Urgent Action to Protect Health from Climate Change—Sign the Call; World Health Organization Publication: Geneva, Switzerland, 2016; Available online: www.who.int/globalchange (accessed on 6 June 2022).
- UNEP. UNEP Finance Initiative’s Annual Overview. 2019. Available online: https://www.unepfi.org/wordpress/wp-content/uploads/2019/09/UNEP-FI-Annual-Overview-2019-.pdf (accessed on 6 June 2022).
- Fuller, R.; Landrigan, P.J.; Balakrishnan, K.; Bathan, G.; Bose-O’Reilly, S.; Brauer, M.; Caravanos, J.; Chiles, T.; Cohen, A.; Corra, L.; et al. Pollution and health: A progress update. Lancet Planet. Health 2022, 6, 5196. [Google Scholar] [CrossRef]
- Khaled, R.; Ali, H.; Mohamed, E.K.A. The Sustainable Development Goals and corporate sustainability performance: Mapping, extent and determinants. J. Clean. Prod. 2021, 311, 127599. [Google Scholar] [CrossRef]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development. Available online: https://sdgs.un.org/2030agenda (accessed on 6 June 2022).
- UN Climate Change The Glasgow Climate Pact—Key Outcomes from COP26. UNFCCC Sites and Platforms, Brazil. 2021. Available online: https://unfccc.int/process-and-meetings/the-paris-agreement/the-glasgow-climate-pact-key-outcomes-from-cop26 (accessed on 6 June 2022).
- UN Climate Change. COP26 Outcomes: Transparency and Reporting. UNFCCC Sites and Platforms, Brazil. 2021. Available online: https://unfccc.int/process-and-meetings/the-paris-agreement/the-glasgow-climate-pact/cop26-outcomes-transparency-and-reporting (accessed on 6 June 2022).
- Sepetis, A. Sustainable Finance in Sustainable Health Care System. Open J. Bus. Manag. 2020, 1, 262–281. [Google Scholar] [CrossRef] [Green Version]
- Jameton, A.; Pierce, J. Environment and health: 8. Sustainable health care and emerging ethical responsibilities. CMAJ 2001, 164, 365–369. [Google Scholar]
- Paci, D. Human Health Impacts of Climate Change in Europe. 2014. Available online: http://europa.eu/ (accessed on 6 June 2022).
- Stenberg, K.; Pierce, J. Financing transformative health systems towards achievement of the health Sustainable Development Goals: A model for projected resource needs in 67 low-income and middle-income countries. Lancet Glob. Health 2017, 9, e875–e887. [Google Scholar] [CrossRef] [Green Version]
- WHO. Safe Management of Wastes from Healthcare Activities. 2017. Available online: https://apps.who.int/iris/handle/10665/259491 (accessed on 6 May 2022).
- WHO. Environmentally Sustainable Health Systems: A Strategic Document. 2017. Available online: https://www.euro.who.int/__data/assets/pdf_file/0004/341239/ESHS_Revised_WHO_web.pdf (accessed on 6 June 2022).
- Namany, S.; Al-Ansari, T.; Govindan, R. Sustainable energy, water and food nexus systems: A focused review of decision-making tools for efficient resource management and governance. J. Clean. Prod. 2019, 225, 610–626. [Google Scholar] [CrossRef]
- Choi, J.K.; Thangamani, D.; Kissock, K. A systematic methodology for improving resource efficiency in small and medium-sized enterprises. Resour. Conserv. Recycl. 2019, 147, 19–27. [Google Scholar] [CrossRef] [Green Version]
- Campion, N.; Thiel, C.L.; Woods, N.C.; Swanzy, L.; Landis, A.E.; Bilec, M.M. Sustainable healthcare and environmental life-cycle impacts of disposable supplies: A focus on disposable custom packs. J. Clean. Prod. 2015, 94, 46–55. [Google Scholar] [CrossRef]
- Leite, H.; Bateman, N.; Radnor, Z. Beyond the ostensible: An exploration of barriers to lean implementation and sustainability in healthcare. Prod. Plan. Control 2020, 31, 1–18. [Google Scholar] [CrossRef]
- Singh, N.; Ogunseitan, O.A.; Tang, Y. Medical waste: Current challenges and future opportunities for sustainable management. Crit. Rev. Environ. Sci. Technol. 2022, 52, 2000–2022. [Google Scholar] [CrossRef]
- Lindsay, C.F.; Kumar, M.; Juleff, L. Operationalising lean in healthcare: The impact of professionalism. Prod. Plan. Control 2020, 31, 629–643. [Google Scholar] [CrossRef]
- Saad, S.G. Integrated environmental management for hospitals. Indoor Built Environ. 2003, 12, 93–98. [Google Scholar] [CrossRef]
- Sherman, J.; Le, C.; Lamers, V.; Eckelman, M.P. Life Cycle Greenhouse Gas Emissions of Anesthetic Drugs. Anesthesia Analg. 2012, 114, 1086–1090. [Google Scholar] [CrossRef] [PubMed]
- Thiel, C.L.; Eckelman, M.; Guido, R.; Huddleston, M.; Landis, A.E.; Sherman, J.; Shrake, S.O.; Copley-Woods, N.; Bilec, M.M. Environmental impacts of surgical procedures: Life cycle assessment of hysterectomy in the United States. Environ. Sci. Technol. 2015, 49, 1779–1786. [Google Scholar] [CrossRef] [PubMed]
- Eckelman, M.J.; Sherman, J. Environmental impacts of the U.S. health care system and effects on public health. PLoS ONE 2016, 11, e0157014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eckelman, M.J.; Sherman, J.D. Estimated Global Disease Burden From US Health Care Sector Greenhouse Gas Emissions Correspondence should be sent to AJPH RESEARCH. AJPH Suppl. 2017, 108, S120–S122. [Google Scholar] [CrossRef] [PubMed]
- McGain, F.N.C. Environmental sustainability in hospitals—A systematic review and research agenda. J. Health Serv. Res. Policy 2014, 19, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Jameton, A.; McGuire, C. Toward sustainable health-care services: Principles, challenges, and a process. Int. J. Sustain. High. Educ. 2002, 3, 113–127. [Google Scholar] [CrossRef]
- Vogt, J.; Nunes, K.R.A. Recycling behaviour in healthcare: Waste handling at work. Ergonomics 2014, 57, 525–535. [Google Scholar] [CrossRef]
- Mackenzie, J. The old care paradigm is dead, long live the new sustainable care paradigm: How can GP commissioning consortia meet the demand challenges of 21st Century healthcare? Lond. J.Prim.Care 2011, 4, 65–69. [Google Scholar] [CrossRef] [Green Version]
- Mosquera, M.; Andrés-Prado, M.J.; Rodríguez-Caravaca, G.; Latasa, P.; Mosquera, M.E.G. Evaluation of an education and training intervention to reduce health care waste in a tertiary hospital in Spain. Am. J. Infect. Control 2014, 42, 894–897. [Google Scholar] [CrossRef]
- Environment Science Center (ESC). Greener Hospitals: Improving Environmental Performance; University Augsburg: Augsburg, Germany, 2007. [Google Scholar]
- Sepeti, A.; Pierrakos, G.; Goula, A. Financial Assessment of Environmental Management Policies in the Operation of Hospitals. In Proceedings of the 21st National Congress of the European Union Decision Making in Health Systems, Athens, Greece, 28–29 May 2009. [Google Scholar]
- Weisz, U.; Haas, W.; Pelikan, J.M.; Schmied, H. Sustainable hospitals: A socio-ecological approach. Gaia 2011, 20, 191–198. [Google Scholar] [CrossRef] [Green Version]
- Manupati, V.K.; Ramkumar, M.; Baba, V.; Agarwal, A. Selection of the best healthcare waste disposal techniques during and post COVID-19 pandemic era. J. Clean. Prod. 2020, 281, 125175. [Google Scholar] [CrossRef] [PubMed]
- Salimian, S.; Seyed, M.; Mousavi; Antucheviciene, J. An Interval-Valued Intuitionistic Fuzzy Model Based on Extended VIKOR and MARCOS for Sustainable Supplier Selection in Organ Transplantation Networks for Healthcare Devices. Sustainability 2022, 14, 3795. [Google Scholar] [CrossRef]
- Mir, M.A.; Ghazvinei, P.T.; Sulaiman, N.M.N.; Basri, N.E.A.; Saheri, S.; Mahmood, N.Z.; Aghamohammadi, N. Application of TOPSIS and VIKOR improved versions in a multi criteria decision analysis to develop an optimized municipal solid waste management model. J. Environ. Manag. 2016, 166, 109–115. [Google Scholar] [CrossRef]
- Kenny, C.; Priyadarshini, A. Review of current healthcare waste management methods and their effect on global health. Healthcare 2021, 9, 284. [Google Scholar] [CrossRef]
- Romero, I.; Carnero, M.C. Environmental assessment in health care organizations.Environ. Environ. Sci. Pollut. Res. 2019, 26, 3196–3207. [Google Scholar] [CrossRef]
- WHO. Health-Care Waste. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/health-care-waste (accessed on 6 June 2022).
- Ranjbari, M.; Shams Esfandabadi, Z.; Shevchenko, T.; Chassagnon-Haned, N.; Peng, W.; Tabatabaei, M.; Aghbashlo, M. Mapping healthcare waste management research: Past evolution, current challenges, and future perspectives towards a circular economy transition. J. Hazard. Mater. 2022, 422, 126724. [Google Scholar] [CrossRef]
- Komilis, D.; Fouki, A.; Papadopoulos, D. Hazardous medical waste generation rates of different categories of health-care facilities. Waste Manag. 2012, 32, 1434–1441. [Google Scholar] [CrossRef]
- Thakur, V.; Mangla, S.K.; Tiwari, B. Managing healthcare waste for sustainable environmental development: A hybrid decision approach. Bus. Strat. Environ. 2021, 30, 357–373. [Google Scholar] [CrossRef]
- WHO. Global Analysis of Health Care Waste in the Context of COVID-19. 2022. Available online: https://www.who.int/publications/i/item/9789240039612 (accessed on 6 June 2022).
- Pachauri, A.; Shah, P.; Almroth, B.C.; Sevilla, N.P.; Narasimhan, M. Safe and sustainable waste management of selfcare products. BMJ 2019, 365, 1298. [Google Scholar] [CrossRef] [Green Version]
- Harhay, M.O.; Halpern, S.D.; Harhay, J.S.; Olliaro, P.L. Health care waste management: A neglected and growing public health problem worldwide. Trop. Med. Int. Health 2009, 14, 1414–1417. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.M.; Ahmed, S.A.; Rahman, K.A.; Biswas, T.K. Pattern of medical waste management: Existing scenario in Dhaka City, Bangladesh. BMC Public Health 2008, 8, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khalid, S.; Haq, N.; Sabiha, Z.-U.; Latif, A.; Khan, M.A.; Iqbal, J.; Yousaf, N. Current practices of waste management in teaching hospitals and presence of incinerators in densely populated areas. BMC Public Health 2021, 21, 1340. [Google Scholar] [CrossRef] [PubMed]
- Altin, S.; Altin, A.; Elevli, B.; Cerit, O. Determination of Hospital Waste Composition and Disposal Methods: A Case Study. Pol. J. Environ. Stud. 2003, 12, 251–255. [Google Scholar]
- Wassie, B.; Gintamo, B.; Mekuria, Z.N.; Gizaw, Z. Healthcare Waste Management Practices and Associated Factors in Private Clinics in Addis Ababa, Ethiopia. Environ. Health Insights 2022, 16, 11786302211073383. [Google Scholar] [CrossRef]
- Minoglou, M.; Gerassimidou, S.; Komilis, D. Healthcare Waste Generation Worldwide and Its Dependence on Socio-Economic and Environmental Factors. Sustainability 2017, 9, 220. [Google Scholar] [CrossRef] [Green Version]
- Tesfahun, E.; Kumie, A.; Beyene, A. Developing models for the prediction of hospital healthcare waste generation rate. Waste Manag. Res. 2016, 34, 75–80. [Google Scholar] [CrossRef]
- Etim, M.-A.; Academe, S.; Emenike, P.; Omole, D. Application of Multi-Criteria Decision Approach in the Assessment of Medical Waste Management Systems in Nigeria. Sustainability 2021, 13, 10914. [Google Scholar] [CrossRef]
- Ike, C.C.; Ezeibe, C.C.; Anijiofor, S.C.; Daud, N.N.N. Solid Waste Management in Nigeria: Problems, Prospects, and Policies. J. Solid Waste Technol. Manag. 2018, 44, 163–172. [Google Scholar] [CrossRef]
- BioEnergy Consult. Solid Waste Management in Nigeria. 2021. Available online: https://www.bioenergyconsult.com/solid-waste-nigeria/ (accessed on 6 June 2022).
- Hamoda, H.M.; El-Tomi, H.N.; Bahman, Q.Y. Variations in Hospital Waste Quantities and Generation Rates. J. Environ. Sci. Health Part A 2005, 40, 467–476. [Google Scholar] [CrossRef]
- Anicetus, H.; Saria, J.; Mohamed, H. Estimation of Different Categories of Healthcare Waste Generated at Two Different Hospital Categories in Four Hospitals in Dar es Salaam City. J. Environ. Prot. 2020, 11, 872–888. [Google Scholar] [CrossRef]
- Maamari, O.; Brandam, C.; Lteif, R.; Salameh, D. Health CareWaste generation rates and patterns: The case of Lebanon. Waste Manag. 2015, 43, 550–554. [Google Scholar] [CrossRef] [Green Version]
- Sadar, G. Assessment of Medical Waste Management Practices: A Case Study in Gopalganj Sadar, Bangladesh. Eur. J. Med. Health Sci. 2022, 62–71. [Google Scholar] [CrossRef]
- Dardi, C.K.; Pandey, A.; Tekwani, D.; Bedekar, M.Y.; Pai, M.; Agarwal, M. Awareness of Bio-medical waste management among the health care workers in rural area. Indian J. Basic Appl. Med. Res. 2015, 4, 351–357. [Google Scholar]
- Voudrias, E.A. Healthcare waste management from the point of view of circular economy. Waste Manag. 2018, 75, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Dietl, H.; Li, J. Identifying key factors influencing sustainable element in healthcare waste management using the interval-valued fuzzy DEMATEL method. J. Mater. Cycles Waste Manag. 2021, 23, 1777–1790. [Google Scholar] [CrossRef]
- Amariglio, A.; Depaoli, D. Waste management in an Italian Hospital’s operating theatres: An observational study. Am. J. Infect. Control 2021, 49, 184–187. [Google Scholar] [CrossRef]
- United Nations Environment Programme, International Environmental Technology Centre, IGES Center Collaborating with UNEP on Environmental Technologies. Waste Management during the COVID-19 Pandemic: From Response to Recovery. Nairobi: United Nations Environment Programme. 2020. Available online: https://www.unep.org/ietc/resources/report/waste-management-during-covid-19-pandemic-response-recovery (accessed on 6 June 2022).
- Greek National Waste Management Plan, Including Hazardous Waste 2022–2030. Available online: http://www.opengov.gr/minenv/wp-content/uploads/downloads/2020/08/%CE%95%CE%A3%CE%94%CE%91-%CE%94%CE%99%CE%91%CE%92%CE%9F%CE%A5%CE%9B%CE%95%CE%A5%CE%A3%CE%97-6-8-2020.pdf (accessed on 6 June 2022).
- Hellenic Governmental Ministerial Decision on Medical Waste Management. In Measures and Terms for the Management of Medical Wastes from Health-Care Facilities; No. 37591/2031/1419; Hellenic Printing Office: Athens, Greece, 2003. (In Greek)
- Voudrias, E.A. Technology selection for infectious medical waste treatment using the analytic hierarchy process. J. Air Waste Manag. Assoc. 2016, 66, 663–672. [Google Scholar] [CrossRef] [Green Version]
- Voudrias, E.; Graikos, A. Infectious MedicalWaste Management System at the Regional Level. J. Hazard. Toxic Radioact. Waste 2014, 18, 04014020. [Google Scholar] [CrossRef]
- Mantzaras, G.; Voudrias, E.A. An optimization model for collection, haul, transfer, treatment and disposal of infectious medical waste: Application to a Greek region. Waste Manag. 2017, 69, 518–534. [Google Scholar] [CrossRef]
- Giakoumakis, G.; Politi, D.; Sidiras, D. MedicalWaste Treatment Technologies for Energy, Fuels, and Materials Production: A Review. Energies 2021, 14, 8065. [Google Scholar] [CrossRef]
- Sepetis, A. Sustainable Health Care Management in the Greek Health Care Sector. Open J. Soc. Sci. 2019, 7, 386–402. [Google Scholar] [CrossRef] [Green Version]
- Komilis, D.; Katsafaros, N. Statistical predictors of hazardous medical waste generation rates in a 40-bed general hospital. Glob. Nest J. 2011, 13, 170–175. [Google Scholar]
- Komilis, D.; Katsafaros, N.; Vassilopoulos, P. Hazardous medical waste generation in Greece: Case studies from medical facilities in Attica and from a small insular hospital. Waste Manag. Res. 2011, 29, 807–814. [Google Scholar] [CrossRef] [PubMed]
- Sanida, G.; Karagiannidis, A.; Mavidou, F.; Vartzopoulos, D.; Moussiopoulos, N.; Chatzopoulos, S. Assessing generated quantities of infectious medicalwastes: A case study for a health region administration in Central Macedonia, Greece. Waste Manag. 2010, 30, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Tsakona, M.; Anagnostopoulou, E.; Gidarakos, E. Hospital waste managementand toxicity evaluation: A case study. Waste Manag. 2007, 27, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Idowu, I.; Alo, B.; Atherton, W. Profile of medical waste management in two healthcare facilities in Lagos, Nigeria: A case study. Waste Manag. Res. 2013, 31, 494–501. [Google Scholar] [CrossRef]
- Kougemitrou, I.; Godelitsas, A.; Tsabaris, C.; Stathopoulos, V.; Papandreou, A.; Gamaletsos, P.; Economou, G.; Papadopoulos, D. Characterization and management of ash produced in the hospital waste incinerator of Athens, Greece. J. Hazard. Mater. 2011, 187, 421–432. [Google Scholar] [CrossRef]
- Salimian, S.; Mousavi, S.M. The selection of healthcare waste treatment technologies by a multi-criteria group decision-making method with intuitionistic fuzzy sets. J. Ind. Syst. Eng. 2022, 14, 205–220. [Google Scholar]
- Mavromatis, S.; Milioreli, K.; Christophorou, S.; Drouza, A.; Despotidou, M.; Special Secretariat for the Environment and Energy Inspectorate (Sseei) Management of Hazardous Waste of Health Units. Reality through the Inspections by the Hellenic Environmental Inspectorate. 2012. Available online: http://www.ypeka.gr/linkclick.aspx?Fileticket=Dh9kb02jku0%3D&tabid=400&language=el-GR (accessed on 6 June 2022).
- Zamparas, M.; Kapsalis, V.C.; Kyriakopoulos, G.L.; Aravossis, K.G.; Kanteraki, A.E.; Vantarakis, A.; Kalavrouziotis, I.K. Medical waste management and environmental assessment in the Rio University Hospital, Western Greece. Sustain. Chem. Pharm. 2019, 13, 100163. [Google Scholar] [CrossRef]
- Health Care without Harm, Greece Health Sector Emissions Fact Sheet. Available online: https://healthcareclimateaction.org/fact-sheets/en/English%20-%20Greece (accessed on 6 June 2022).
- Price Observatory of the Greek Ministry of Health. Available online: https://www.moh.gov.gr›parathrhthrio-timwn (accessed on 6 June 2022).
- Afriyanto; Pitaksanurat, S.; Junggoth, R.; Setiyadi, N.A. Factors Affecting the Infectious Waste Management System on Practice Disposal Waste Among Health Workers in Bengkulu Hospital. In Proceedings of the 2nd Sriwijaya International Conference of Public Health (SICPH 2019), Palembang, Indonesia, 6–7 November 2019; Atlantis Press: Amsterdam, The Netherlands, 2019; Volume 25, pp. 101–109. [Google Scholar] [CrossRef]
- Manyele, S.V.; Lyasenga, T.J. Factors Affecting Medical Waste Management in Low- Level Health Facilities in Tanzania. Afr. J. Environ. Sci. Technol. 2010, 4, 304–318. Available online: http://www.academicjournals.org/AJEST (accessed on 6 June 2022).
- Dewi, O.; Sukendi, S.; Ikhwan, Y.S.; Nazrianti, E. Characteristics and Factors Associated with Medical Waste Management Behaviour in Private Dental Health Services in Pekanbaru City, Indonesia. Open Access Maced. J. Med. Sci. 2019, 7, 157–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huda, N.; Hailemariam, T.G.; Hossain, S.Z.; Malo, J.S.; Khan, S.; Hadisuyatmana, S.; Ferdous, A. Medical waste management-related factors affecting health and experiences of health risks among medical waste handlers in low and middle-income countries: A systematic review protocol of qualitative studies. BMJ Open 2022, 12, e056037. [Google Scholar] [CrossRef] [PubMed]
- Vaccari, M.; Tudor, T.; Perteghella, A. Costs associated with the management of waste from healthcare facilities: An analysis at national and site level. Waste Manag. Res. 2018, 36, 39–47. [Google Scholar] [CrossRef]
- Bdour, A.; Altrabsheh, B.; Hadadin, N.; Al-Shareif, M. Assessment of medical wastes management practice: A case study of the northern part of Jordan. Waste Manag. 2007, 27, 746–759. [Google Scholar] [CrossRef]
- Hamburger, W. A Heteroskedasticity-Consistent Covariance Matrix Estimator and a Direct Test for Heteroskedasticity. Econometrica 2016, 23, 1–17. [Google Scholar] [CrossRef]
- White, H. Maximum Likelihood Estimation of Misspecified Models. Econometrica 1983, 51, 513. [Google Scholar] [CrossRef] [Green Version]
- Zellner, A. An Efficient Method of Estimating Seemingly Unrelated Regressions and Tests for Aggregation Bias. J. Am. Stat. Assoc. 1962, 57, 348. [Google Scholar] [CrossRef]
- StataCorp. Stata: Release 13. Statistical Software; StataCorp LP: College Station, TX, USA, 2013. [Google Scholar]
- Alhumoud, J.M.; Alhumoud, H.M. An analysis of trends related to hospital solid wastes management in Kuwait. Manag. Environ. Qual. Int. J. 2007, 18, 502–513. [Google Scholar] [CrossRef]
- Katoch, S.; Kumar, V. Modelling seasonal variation in biomedical waste generation at healthcare facilities. Waste Manag. Res. 2007, 26, 241–246. [Google Scholar] [CrossRef]






| Health District | Small Hospitals | General Hospitals | University Hospitals | Specialized Type I Hospitals | Specialized Type II Hospitals |
|---|---|---|---|---|---|
| 1st | 1 | 11 | 0 | 7 | 3 |
| 2nd | 6 | 9 | 2 | 2 | 2 |
| 3rd | 0 | 14 | 0 | 1 | 0 |
| 4th | 1 | 10 | 2 | 0 | 1 |
| 5th | 2 | 10 | 1 | 0 | 0 |
| 6th | 6 | 19 | 2 | 1 | 0 |
| 7th | 3 | 4 | 1 | 0 | 0 |
| Health District | Average Annual Cost of Hazardous Waste per Bed (€) | Total Average Waste Cost per Bed (€) |
|---|---|---|
| 1st | 718 | 571.3 |
| 2nd | 630 | |
| 3rd | 355 | |
| 4th | 395 | |
| 5th | 467 | |
| 6th | 449 | |
| 7th | 601 |
| Health District | Average Cost of Hazardous Waste per Patient (€) | Total Average Waste Cost per Patient (€) |
|---|---|---|
| 1st | 10.6 | 7.6 |
| 2nd | 10.7 | |
| 3rd | 4.4 | |
| 4th | 5.3 | |
| 5th | 6.1 | |
| 6th | 8.2 | |
| 7th | 9.0 |
| Hospital Type | Average Kilos of Hazardous Waste per Bed per Day | Total Average Kilos of Hazardous Waste per Bed per Day |
|---|---|---|
| Small Hospital | 0.33 | 0.84 |
| General Hospital | 0.75 | |
| University Hospital | 0.99 | |
| Specialized Hospital I | 0.34 | |
| Specialized Hospital II | 1.00 |
| Pairwise Correlations | LogWaste Cost | LogWaste Kilos | Beds | Hospital Type | ICU | Inpatients | Days of Stay | Employees |
|---|---|---|---|---|---|---|---|---|
| LogWaste Cost | 1.0000 | |||||||
| LogWaste Kilos | 0.9492 | 1.0000 | ||||||
| Beds | 0.6084 | 0.6790 | 1 | |||||
| Hospital Type | 0.2557 | 0.3017 | 0.3784 | 1.0000 | ||||
| ICU | 0.7271 | 0.7326 | 0.5579 | 0.1627 | 1.0000 | |||
| Inpatients | 0.7544 | 0.7712 | 0.8005 | 0.3044 | 0.6509 | 1.0000 | ||
| Days of stay | 0.6586 | 0.6961 | 0.9078 | 0.3149 | 0.5753 | 0.899 | 1.0000 | |
| Employees | 0.7759 | 0.799 | 0.924 | 0.3154 | 0.6436 | 0.8798 | 0.9217 | 1.0000 |
| Dependent Variables | YEAR 2018 | |||||
|---|---|---|---|---|---|---|
| Seemingly Unrelated Regression | Multivariate Regression | Linear Regression | ||||
| Number of Obs = 121 | Number of Obs = 121 | Number of Obs = 121 | ||||
| R2 | Independent Variables | R2 | Independent Variables | R2 | Independent Variables | |
| Cost of hazardous waste | 0.8522 | Beds, Hosptype, Beds#Hosptype Icu, Inpatients, Days, Employees | 0.8603 | Beds, Hosptype, Beds#Hosptype Icu, Inpatients, Days, Employees | 0.8522 | Beds, Hosptype, Beds#Hosptype Icu, Inpatients, Days, Employees |
| Kilos of hazardous waste | 0.8594 | Beds, Hosptype, Beds#Hosptype Icu, Inpatients, Days, Employees, S.Surgeries | 0.8642 | Beds, Hosptype, Beds#Hosptype Icu, Inpatients, Days, Employees | 0.8471 | Beds, Hosptype, Beds#Hosptype Inpatients, Days, Employees |
| Seemingly Unrelated Regression for the Cost of Hazardous Waste Management | R2 = 0.8522 | ||
|---|---|---|---|
| Number of Obs = 121 | |||
| Coefficient | (SE) | ||
| Constant | b0 | 8.013451 | (0.2663484) |
| Number of Beds | b1 | 0.0246254 | (0.0053255) |
| Hospital Type | |||
| General Hospital | b2 | 2.118334 | (0.2903447) |
| University Hospital | 5.640858 | (1.147168) | |
| Specialized Hospital Type I | 1.613669 | (0.3829162) | |
| Specialized Hospital Type II | 1.867596 | (0.6772875) | |
| Hospital Type # Beds | |||
| General Hospital | b3 | −0.0287761 | (0.0052831) |
| University Hospital | −0.0352248 | (0.0055343) | |
| Specialized Hospital Type I | −0.0278102 | (0.005303) | |
| Specialized Hospital Type II | −0.0276302 | (0.0057483) | |
| Intensive Care Unit | b4 | 0.4388912 | (0.1553799) |
| Total Internal Patients | b5 | 0.0000265 | (6.85 × 10−6) |
| Days of Stay | b6 | −0.00000633 | (2.83 × 10−6) |
| Total Number of Employees | b7 | 0.0030473 | (0.0003703) |
| Seemingly Unrelated Regression for the Kilos of Hazardous Waste | R2 = 0.8594 | ||
|---|---|---|---|
| Number of Obs = 121 | |||
| Coefficient | (SE) | ||
| Constant | b0 | 6.711418 | (0.293857) |
| Number of Beds | b1 | 0.0268199 | (0.0058768) |
| Hospital Type | |||
| General Hospital | b2 | 2.482767 | (0.3203334) |
| University Hospital | 5.751815 | (1.26892) | |
| Specialized Hospital Type I | 1.803676 | (0.4244299) | |
| Specialized Hospital Type II | 2.805956 | (0.7482615) | |
| Hospital Type # Beds | |||
| General Hospital | b3 | −0.027856 | (0.0058301) |
| University Hospital | −0.0341217 | (0.0061111) | |
| Specialized Hospital Type I | −0.027567 | (0.0058515) | |
| Specialized Hospital Type II | −0.0285752 | (0.006342) | |
| Intensive Care Unit | b4 | 0.3689101 | (0.1717678) |
| Total Internal Patients | b5 | 0.0000337 | (7.68 × 10−6) |
| Days of Stay | b6 | −0.0000106 | (3.19 × 10−6) |
| Total Number of Employees | b7 | 0.0024858 | (0.0004086) |
| Scheduled Surgeries | b8 | −0.0000331 | (0.293857) |
| Hospital Type | b2 | b3 |
|---|---|---|
| Small Hospital/Health Center | 0 | 0 |
| General Hospital | 2.118334 | −0.0287761 |
| University Hospital | 5.640858 | −0.0352248 |
| Specialized Hospital Type I | 1.613669 | −0.0278102 |
| Specialized Hospital Type II | 1.867596 | −0.0276302 |
| Hospital Type | b2 | b3 |
|---|---|---|
| Small Hospital/ Health Center | 0 | 0 |
| General Hospital | 2.482767 | −0.027856 |
| University Hospital | 5.751815 | −0.0341217 |
| Specialized Hospital I | 1.803676 | −0.027567 |
| Specialized Hospital II | 2.805956 | −0.0285752 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sepetis, A.; Zaza, P.N.; Rizos, F.; Bagos, P.G. Identifying and Predicting Healthcare Waste Management Costs for an Optimal Sustainable Management System: Evidence from the Greek Public Sector. Int. J. Environ. Res. Public Health 2022, 19, 9821. https://doi.org/10.3390/ijerph19169821
Sepetis A, Zaza PN, Rizos F, Bagos PG. Identifying and Predicting Healthcare Waste Management Costs for an Optimal Sustainable Management System: Evidence from the Greek Public Sector. International Journal of Environmental Research and Public Health. 2022; 19(16):9821. https://doi.org/10.3390/ijerph19169821
Chicago/Turabian StyleSepetis, Anastasios, Paraskevi N. Zaza, Fotios Rizos, and Pantelis G. Bagos. 2022. "Identifying and Predicting Healthcare Waste Management Costs for an Optimal Sustainable Management System: Evidence from the Greek Public Sector" International Journal of Environmental Research and Public Health 19, no. 16: 9821. https://doi.org/10.3390/ijerph19169821
APA StyleSepetis, A., Zaza, P. N., Rizos, F., & Bagos, P. G. (2022). Identifying and Predicting Healthcare Waste Management Costs for an Optimal Sustainable Management System: Evidence from the Greek Public Sector. International Journal of Environmental Research and Public Health, 19(16), 9821. https://doi.org/10.3390/ijerph19169821








