1. Introduction
The extensor hallucis longus (EHL) muscle originates from the middle third of fibula and adjacent anterior surface of the interosseous membrane and is situated between and deep to the tibialis anterior (TA) muscle and the extensor digitorum longus (EDL) muscle. The EHL tendon extends through the inferior retinaculum and then inserts to the distal phalanx of the big toe (hallux). Especially, the EHL tendon reaches its insertion point at the base and dorsal surface of the distal phalanx of the big toe. Thus, the main action of EHL is to extend the big toe (hallux extensor) [
1,
2].
High variability in the anatomical morphology of the EHL has been reported and the most representative variation is the presence of the accessory tendon of the EHL. One or more accessory tendons of the EHL tendon have been well documented, particularly by frequency and insertion site of tendon [
3,
4,
5,
6,
7,
8,
9], and it is presumed that there are regional and/or ethnic differences in the frequency and morphology of variation. Thus, an awareness of this variation has clinical significance to foot and ankle surgeons who always face hallux problems, such as the pathology caused by hallux deformity, and determine usefulness as donor for tendon graft [
3,
8,
9,
10].
Al-Saggaf first distinguished three different types with respect to insertion of the EHL tendon, as follows: single tendon, two tendons (main and medial accessory tendon), and three tendons (main, medial, and lateral accessory tendon) [
3]. Later, Olewnik et al. proposed a systematic classification based on the number and the location of insertion of accessory tendons by adding new types [
9]. Most recently, Zielinska et al. [
11] has updated a new classification system that combines the both the Al-Saggaf [
3] and Olewnik et al. [
9] classification. In our routine dissection of Korean cadavers, however, the new patterns of the EHL tendon variation that were not described at all in the updated classification were observed.
Therefore, the current study was undertaken to ascertain the anatomical characteristics of the EHL tendon variation according to the number and the insertion site of accessory tendons using larger-scale dissection of Korean cadavers and to classify the types along with incidence.
2. Materials and Methods
All cadavers used in this study were donated through the donation program with consent for education and research in medical school. In addition, this study was approved by our institution of Institutional Ethics Committee (Institutional Review Board number: CHUNCHEON NON2021-002).
In this study, a total of 180 feet (90 adult cadavers) were dissected. Among those 180 feet, 158 feet (79 cadavers) were included for this study excluding 22 feet (11 cadavers) with abnormal signs of trauma or surgery, obvious deformities, pathologic lesions, and damage that render the investigation of morphology of structures difficult. Obvious deformities are those that do not have the foot shape in the normal range, but all cases wherein the morphology of structure can be investigated as deformity limited to general diseases (such as hallux valgus) were included.
Of the 158 feet (79 cadavers) dissected from adult formalin-fixed cadavers, 100 feet (63%) were from males and 58 feet (37%) from females. The mean age of the donors at death was 79.9 (range, 44–100) years (
Figure 1).
2.1. Dissection
The lower limb was fixed by a pedestal after formalin-fixed cadavers were placed in the supine position. Dissection started from the anterior aspect of the lower lime to the distal of foot dorsum. After the removal of the skin, the soft tissue was dissected layer by layer to expose the EHL muscle and tendon. Following this, the extensor retinaculum was removed to check the EHL tendon’s course from the ankle toward the hallux. The main and accessory tendons of EHL were carefully checked. Furthermore, the sites of tendon insertions were evaluated.
2.2. Assessment of Morphological Characteristics of the EHL Tendon Variations
Referring of the classification system by Zielinska et al. [
11], authors classified types according to the number of EHL tendon and divided into subtypes according to the sites where the accessory tendons are distally inserted. If the new subtype found only in the current study was not included in the classification system by Zielinska et al. [
11], it was classified as subtype ‘K’. Each independent researcher repeatedly investigated the morphology of the tendon insertion in duplicate. Identical consensus assessments from two researchers were adopted as data for each specimen.
The length of the main EHL tendon was measured from the point where it could be divided into the muscle belly and tendon to the distal insertion of tendon. Then, the width was measured at the midpoint of the main tendon. Furthermore, the length and width of accessory tendon were measured only in Type 2 (two tendons: main and one accessory tendon). For the length of the accessory tendon, the distance from the bifurcation of the main EHL tendon to the distal insertion point was measured. Next, the width of the accessory tendon was measured at the midpoint of the accessory tendon. An electronic digital caliper (Sincon Corporation, Seoul, Korea) with an accuracy of up to 0.1 mm was used for all measurements. For all measurements, two researchers each independently measured the width, and one researcher measured each once and the average was adopted as the measurement value.
2.3. Statistical Analysis
Intra- and interobserver reliability for all measurements were assessed by intraclass correlation coefficient (ICC). Data were analyzed using IBM SPSS Statistics version 23.0 for Windows (IBM Co., Armonk, NY, USA), and a p-value of less than 0.05 was considered statistically significant. The Fisher’s exact test was used to assess the distribution of types between gender and side. The mean comparison of length and width of tendons according to gender was analyzed by independent samples t-test, and the mean comparison between left and right was analyzed by paired t-test.
3. Results
The intraclass correlation coefficient for all measurements generated a result of 0.9 or higher. All measurements were higher than the accepted reliability (0.8) and were employed in the study.
The EHL tendon variation could be classified into three main types based on the number of tendons.
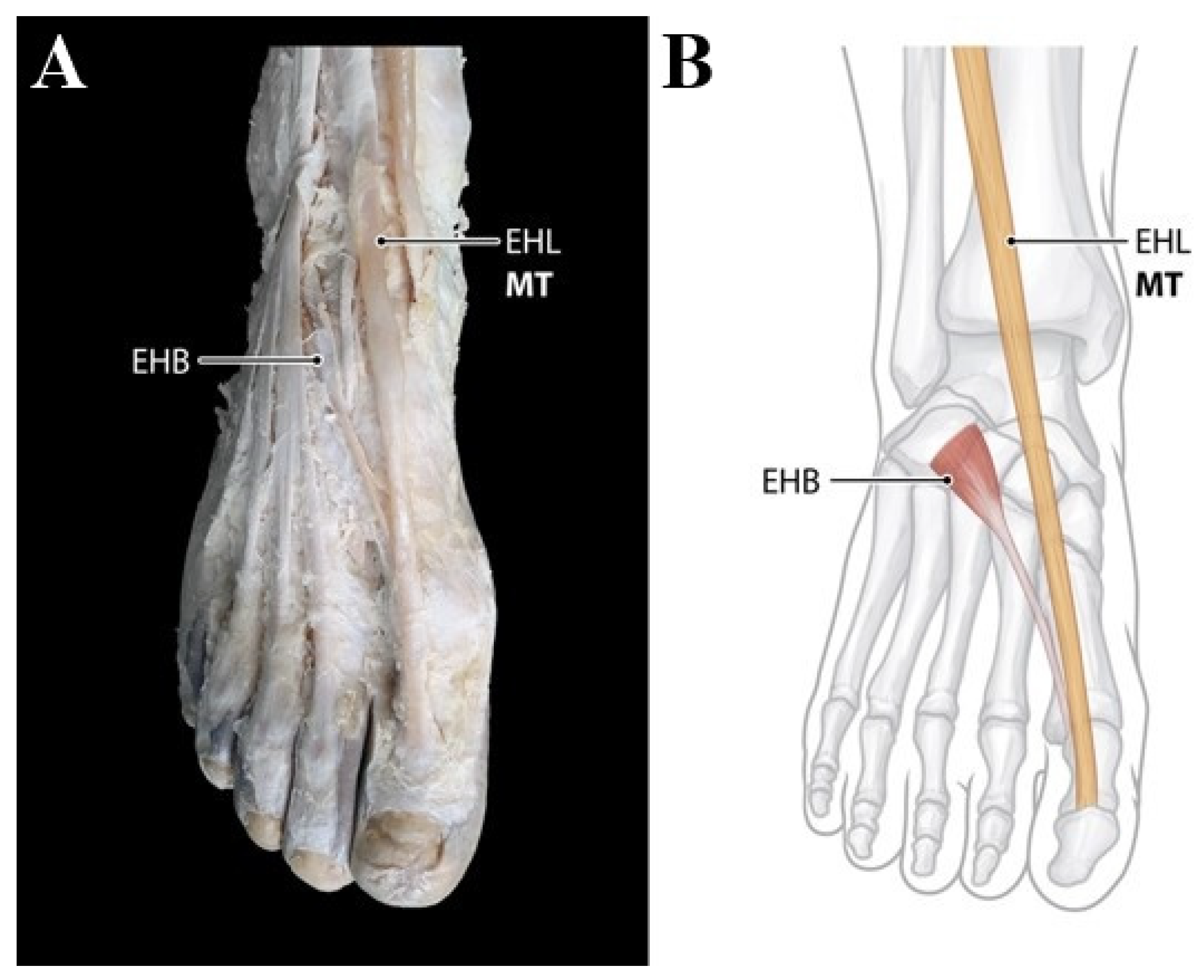
Type 1 (single insertion) consists of single tendon. The main tendon only inserts to the base of distal phalanx of the big toe (hallux). This type was observed in 49 feet (31.0%) (
Figure 2).
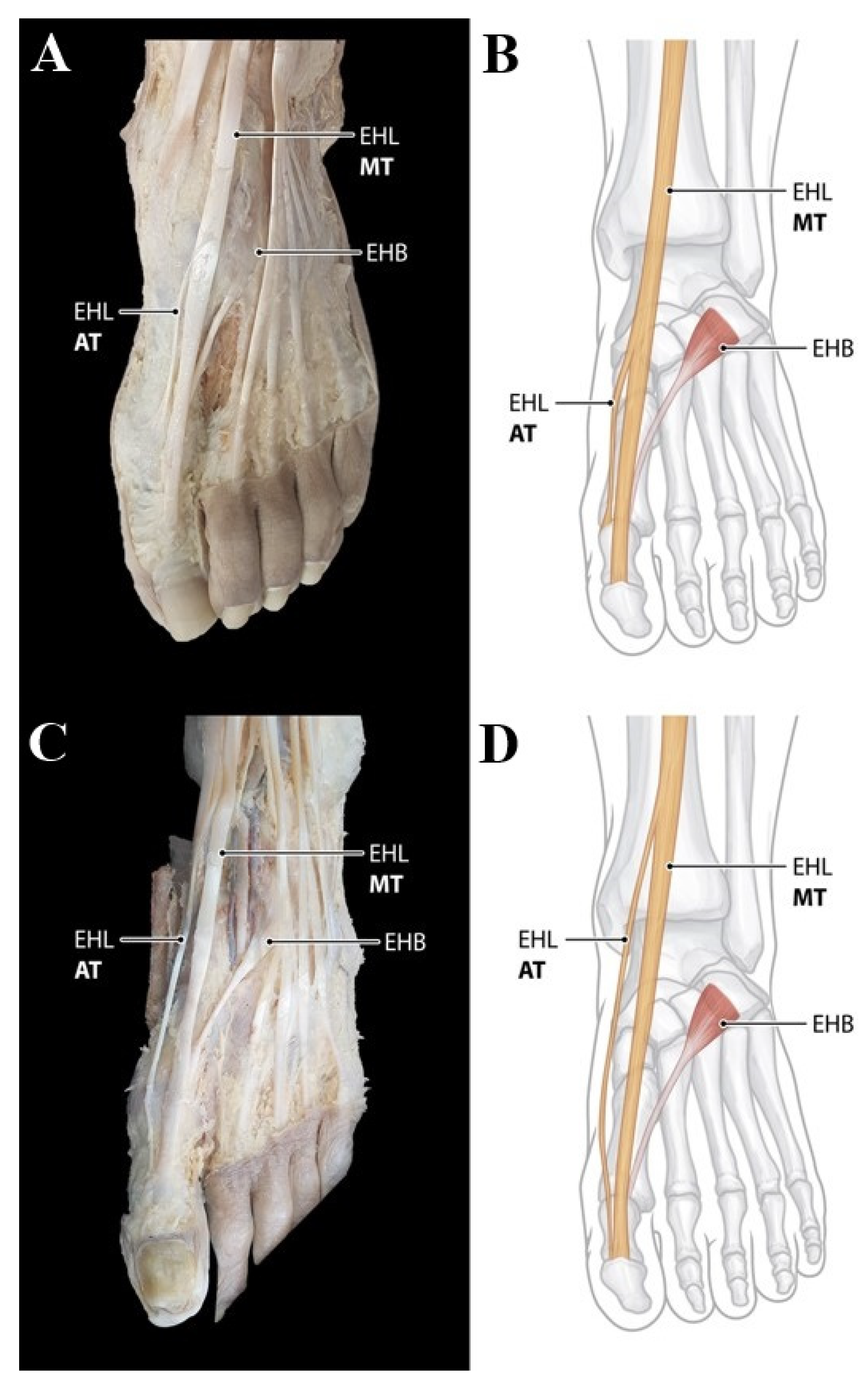
Type 2 (double insertions) consists of two tendons, including the main tendon and one accessory tendon. The main tendon inserts as in Type 1; however, the following subtypes were divided according to the different insertion of the accessory tendons. Type 2 was observed in the 106 feet (67.1%). In Subtype 2A, described in the classification by Zielinska et al. observed in the 94 feet (59.5%), the medial accessory tendon inserts to the dorsal aspect of the proximal phalanx base of the hallux (
Figure 3A,B). Subtype 2C of classification by Zielinska et al. was observed in only one foot (0.6%) and the lateral accessory tendon inserts to the dorsal aspect of the first metatarsal base. However, Subtype 2B, 2C, and 2E were not observed in our study. In addition, it is noteworthy that new subtype not mentioned in the classification by Zielinska et al. was founded in 11 feet (7.0%) of our study. In this subtype named ‘2K’, the medial accessory tendon inserts onto the first interphalangeal joint capsule (
Figure 3C,D).
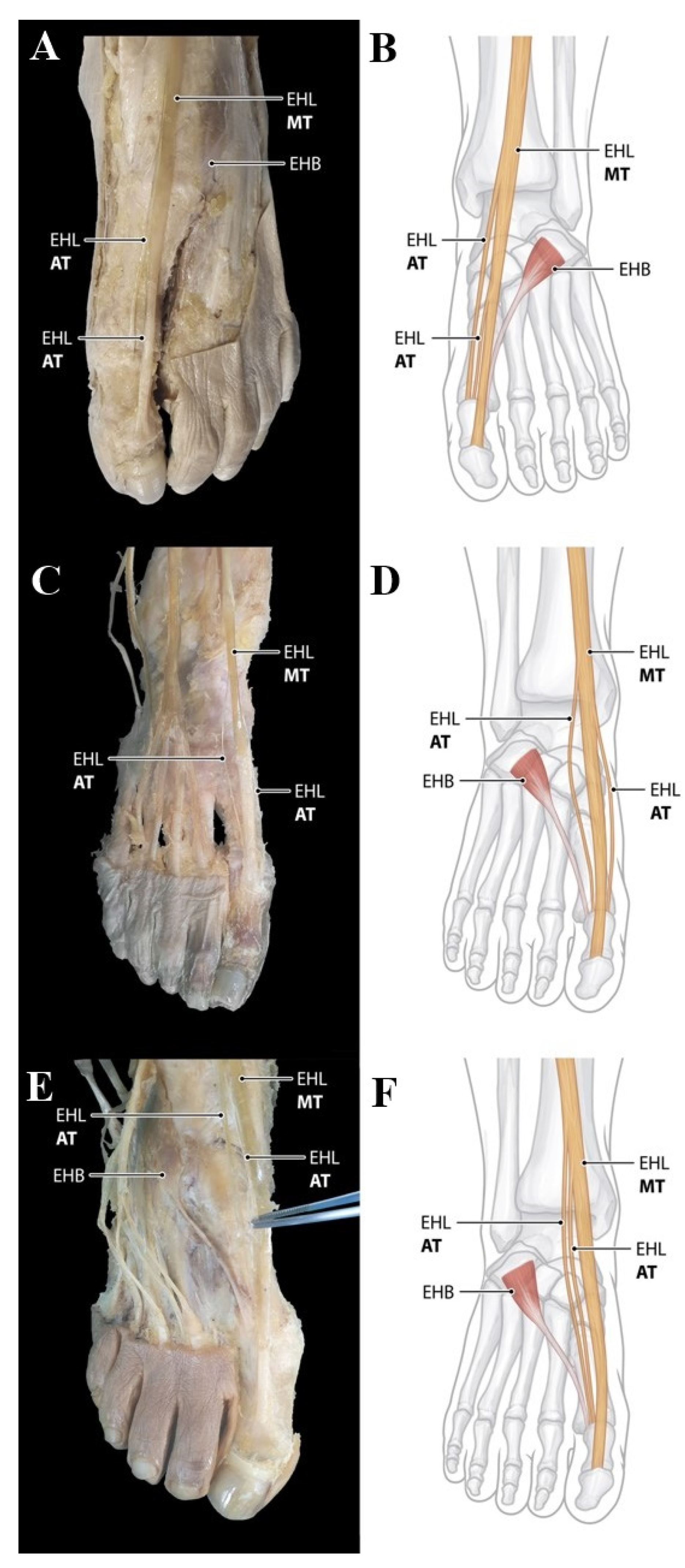
Type 3 (triple insertions) consists of three tendons including main tendon and two accessory tendon The main tendon inserts as in Type 1; with the following subtypes divided according to the different insertion of the accessory tendons. Type 3 was observed in the 3 feet (1.9%). Subtype 3B and 3C described in the classification by Zielinska et al. were observed in the 1 foot (0.6%), respectively. Subtype 3B showed that two accessory tendons arise from the medial side of the main tendon and insert into the capsule of first metatarsophalangeal joint, whereas two accessory tendons arise from the medial and lateral side of the main tendon and insert into the capsule of first metatarsophalangeal joint in Subtype 3C (
Figure 4A–D). However, Subtype 3A was not observed in our study. In addition, it is noteworthy that new subtype not mentioned in the classification by Zielinska et al. was founded in 1 foot (0.6%) of our study. In the subtype named ‘3K’, the two accessory tendons arise from the lateral side of the main tendon and insert into the capsule of first metatarsophalangeal joint (
Figure 4E,F).
The significant difference regarding the distribution of types can be found between gender (
p = 0.016) which is presented in
Table 1. However, there was no significant difference in the distribution of types between the left and right (
p = 0.205) (
Table 2).
The length and width of the main tendon of EHL were measured in 158 feet, while the measurement of the length and width of the accessory tendon of EHL were evaluated in 106 feet of Type 2. The mean values of these measurements are presented in
Table 3. These measurements did not differ significantly between genders.
4. Discussion
Although recently updated classification of the EHL tendon variation to clarify presentation of morphologic characteristics of the accessory tendon of the EHL has been proposed, the contribution of current study is to suggest morphological characteristics of the EHL tendon variation in Korean population, while complementing the previous classification system by observing new types of variation. Additionally, by emphasizing the high morphological variability of the EHL tendons, the current study reinforces the possibility of differences in the morphological variability by race or ethnicity and gender.
In the literature review of incidence rates of an accessory tendon of the EHL, the incidence rate of an accessory tendon of the EHL is relatively low in Saudi Arabia (35.0%) [
3], Greece (26.5%) [
8], and Poland (42.5%) [
9]; whereas in Turkey (78.4%) [
5] and the United States (75%) [
4], the incidence is high. In particular, two recent studies of the Asian population [
6,
7] reported that 47 out of 48 feet (97.92%) of a Taiwanese sample and all 50 feet of a Chinese sample had accessory tendons of EHL. The current study was conducted on the largest number of samples to date (158 feet), and the incidence rate of the accessory tendons of EHL was 67.1%. This may mean a high incidence of the accessory tendons of EHL in Asian populations, but it also means that there is high variability in frequency according to region and ethnicity in same Asian populations. Furthermore, a noteworthy point in comparing the frequency of the accessory tendons of EHLs among studies is that there is a wide range of frequencies among adults, from 26.5% to 100% (
Table 4). This clearly reinforces a difference in the morphology of the EHL tendon variation by region and race or ethnicity.
A classification system is necessary to clarify the morphology of the EHL tendon variations, and Al-Saggaf [
3] created the first accurate classification. This systematic classification was based on the number and the location of insertion of accessory tendons of the EHL. Additionally, Olewnik et al. [
9] suggested a systematic classification based on the same criteria but added new subtypes different from the previous one. Most recently, Zielinska et al. [
11] proposed a new, detailed classification system which is merely a combination of subtypes from the previous two classifications. In the current study, a subtype in which the medial accessory EHL tendon is inserted into the first interphalangeal joint capsule near the attachment site of the main EHL tendon was observed in 11 cases (7%) and this pattern could be suggested as a new subtype (named ‘Type 2K’). In addition, another new subtype (named ‘Type 3K’) in which two accessory EHL tendons run laterally relative to the major EHL tendon was also suggested (
Table 3). Therefore, it is clear that the morphology of the EHL tendon is highly variable. For this reason, the current study suggests a newly updated classification by supplementing the subtypes not presented in the recently updated classification system through dissection of the larger samples.
In addition, in our study, cadaveric dissections were made for 158 cases—a very generous sample size—allowing paired analysis of the feet of each of 79 patients. A variant of the EHL tendon could be obtained with the result that even one patient could show different morphologies between their two sides. These results are noteworthy as they imply that variability of the EHL tendon can occur even within the same individual.
Since the EHL tendon variants are mainly attached to the metatarsophalangeal and interphalangeal joints, hallux deformity—such as hallux valgus—may be developed secondary to imbalance with the action of other tendons around the joint of the big toe. In the literature review, the relationship between EHL tendon variation and hallux valgus is controversial. Many researchers have failed to find any significant correlation between the presence of an accessary EHL tendon and that of hallux valgus [
4,
5,
8]. Natsis et al. [
8] even mentioned that the action of the accessory EHL tendon against the axis of deformity force in the varus direction might rather prevent the deformity. Conversely, some authors have thought that an accessory tendon of EHL may influence the development of hallux valgus [
3,
12]. Our results showed that the frequency of the accessory EHL tendon was significantly higher among females. As a result of a systematic review and meta-analysis of the prevalence of hallux valgus [
13], it is clear that hallux valgus is prevalent in women. Therefore, the contribution of the accessory tendon of EHL related to HV deformity seems to remain unclear, and a biomechanical study will be required to determine what direction of force the accessary EHL tendon acts on the hallux according to the classification system.
It has been suggested that the accessory EHL tendon could be used as tendon graft in various reconstructive surgeries such as tendon repairs, small ligament transfers, and interpositional arthroplasty [
5,
10]. However, its usefulness as donor for tendon graft would depend on its width and length, although tendon length may be less important than width and volume with respect to autogenous grafting. Boyd et al. [
14] found that the average length of an accessory EHL tendon in Type 2 was 10.8 cm; and in our results, it was 9.44 cm. Additionally, Boyd et al. [
14] suggested that 12 out of 81 feet (14%), when the accessory EHL tendon had a width of 2 mm or more, that it could be used as a donor for tendon graft. Similarly, our results showed that 16 out of 106 feet (15%) had a width of 2 mm or more and the average of the accessory EHL tendon was 1.39 mm. It is considered necessary to check the tendon width using imaging tests such as magnetic resonance imaging (MRI) or ultrasound before surgery in order to determine suitability for grafting, and the newly updated classification of the EHL tendon variation may be helpful to foot and ankle surgeons.
There were some limitations in this study. Fixed cadavers were used to evaluate tendon structure, so there may be differences comparing a live person due to post-mortem changes. Furthermore, as the mean age of cadavers was 79.9 years, the presence of tendon pathology may not be completely ruled out, because the past medical histories of the corpse specimens donated for research are uncertain.