Traditional Heart-Healthy Diet and Medication Adherence in the Norton Sound Region: An 18-Month Telehealth Intervention
Abstract
:1. Introduction
2. Materials and Methods
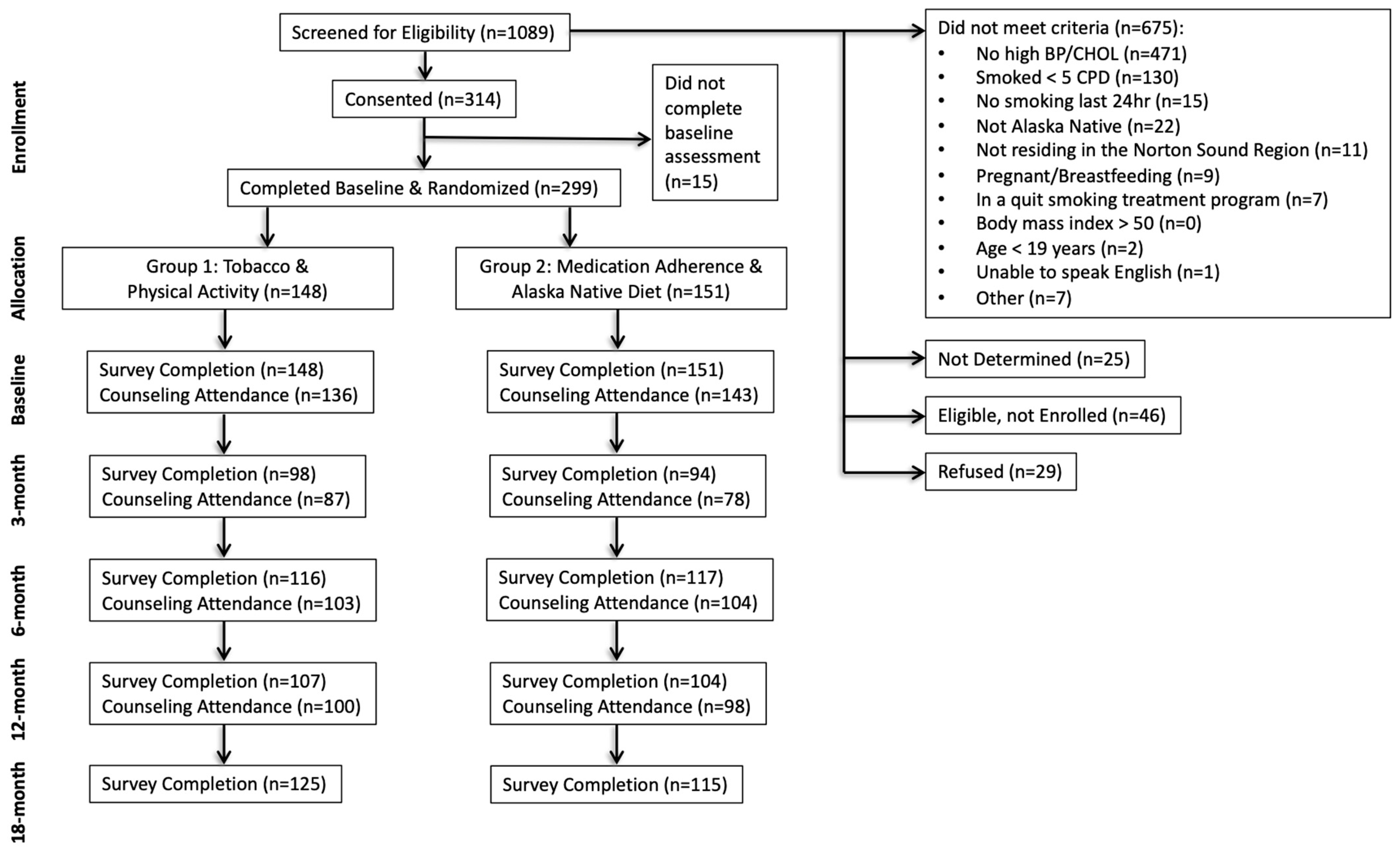
2.1. Sample
2.2. Study Design
2.3. Study Interventions
2.4. Measures
2.4.1. Dietary Intake
2.4.2. Medication Adherence
2.4.3. Season
2.4.4. Community Connectedness
2.5. Data Management and Analyses
2.5.1. Missing Data
2.5.2. Data Analyses
3. Results
3.1. Participant Characteristics
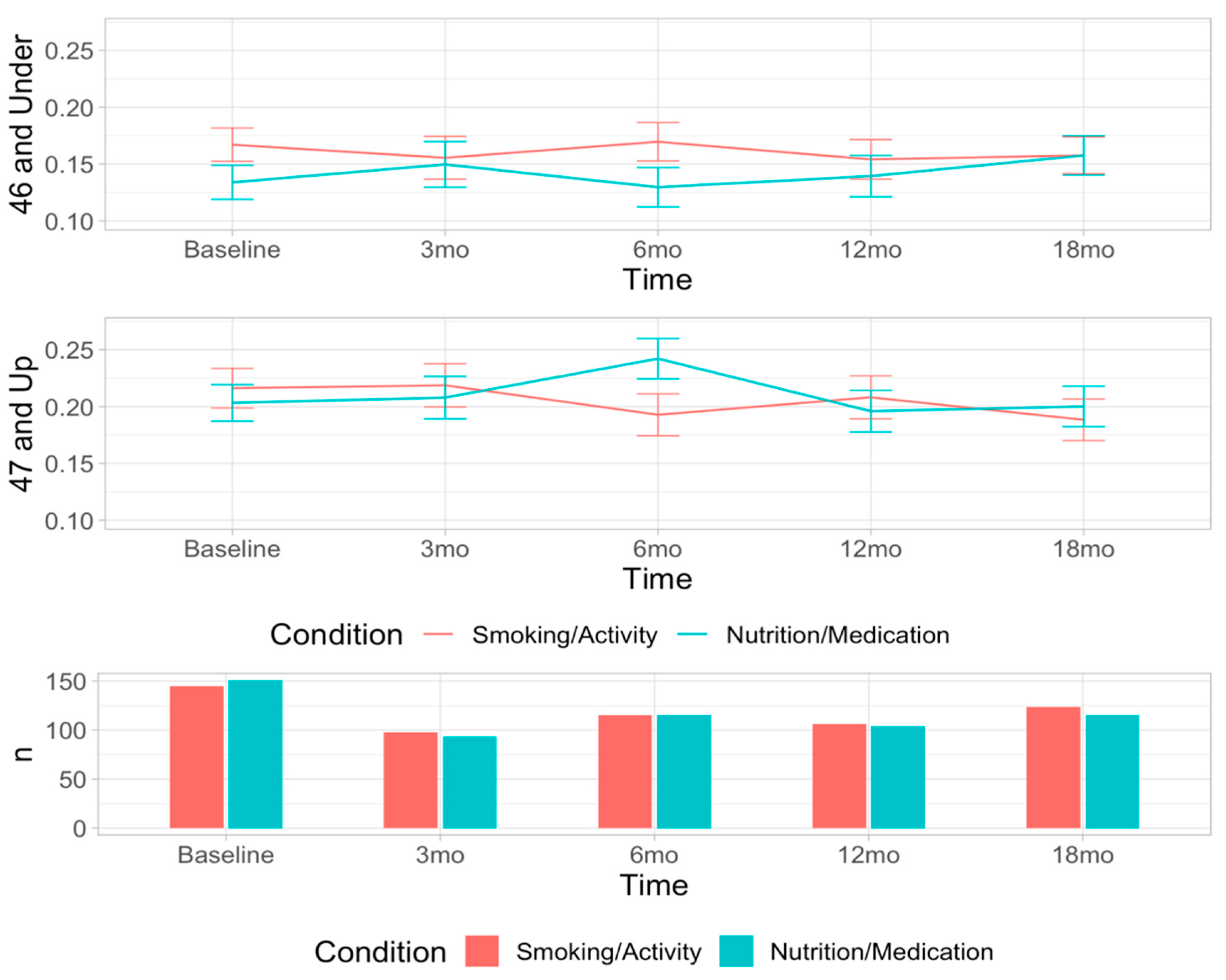
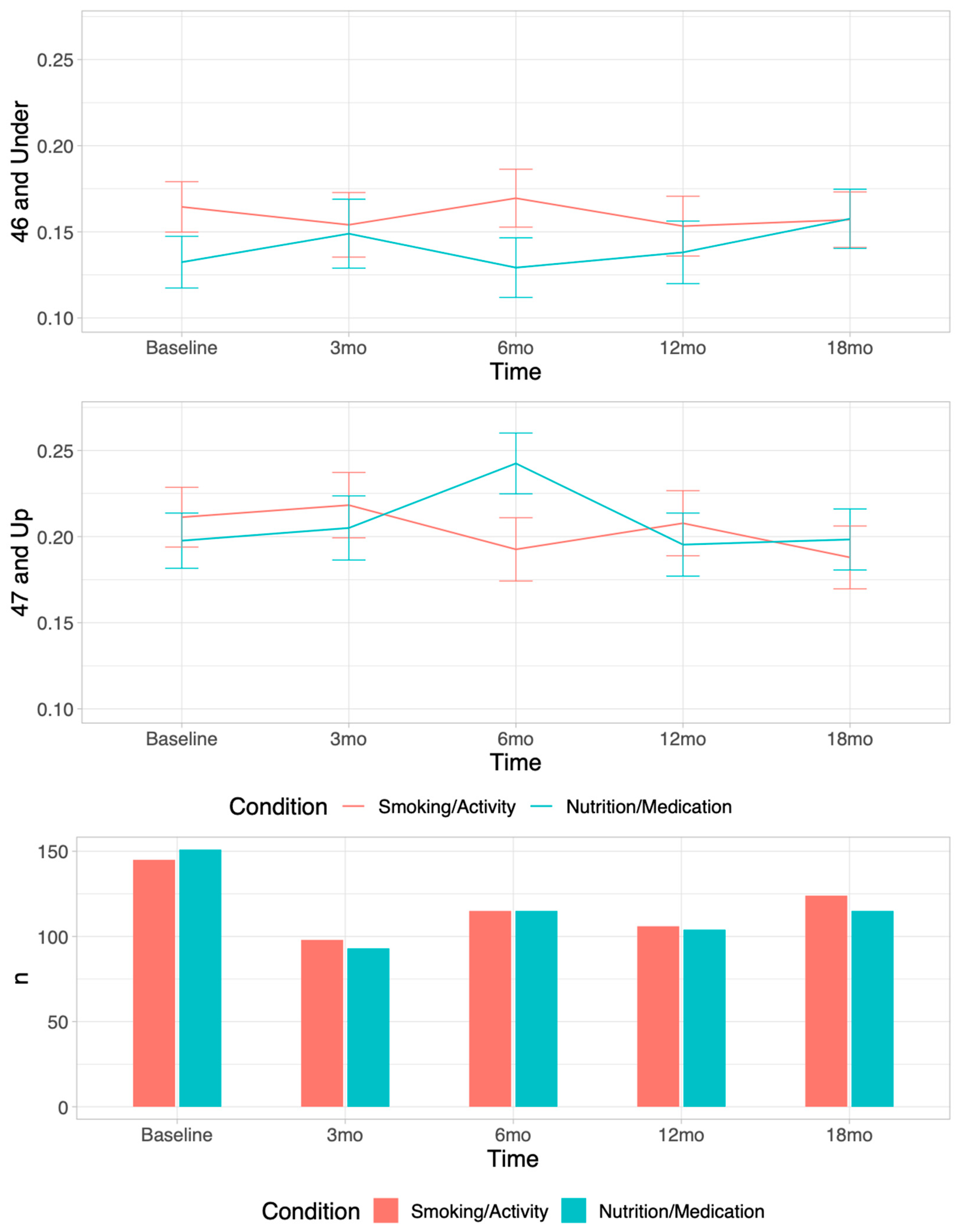
3.2. Nutrition Outcomes
3.3. Medication Adherence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Underlying Cause of Death 1999–2019. 2020 ed.; CDC WONDER ONLINE DATABASE, 1999–2019. Available online: http://wonder.cdc.gov/ucd-icd10.html (accessed on 29 July 2021).
- Alaska Division of Public Health. Alaska Health Analytics and Vital Records Section. In Heart Disease Mortality; Alaska Native Tribal Health Consortium: Anchorage, AK, USA, 2021; Available online: http://anthctoday.org/epicenter/healthData/factsheets/2022%20Factsheets/Heart-Disease-Mortality.pdf (accessed on 29 July 2021).
- Jernigan, V.B.B.; Duran, B.; Ahn, D.; Winkleby, M. Changing Patterns in Health Behaviors and Risk Factors Related to Cardiovascular Disease Among American Indians and Alaska Natives. Am. J. Public Health 2010, 100, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.J.; Prochaska, J.O. A Review of Multiple Health Behavior Change Interventions for Primary Prevention. Am. J. Lifestyle Med. 2011, 5, 208–221. [Google Scholar] [CrossRef] [PubMed]
- Bersamin, A.; Zidenberg-Cherr, S.; Stern, J.S.; Luick, B.R. Nutrient intakes are associated with adherence to a traditional diet among Yup‘ik Eskimos living in remote Alaska Native communities: The CANHR Study. Int. J. Circumpolar Health 2007, 66, 62–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Redwood, D.G.; Ferucci, E.D.; Schumacher, M.C.; Johnson, J.S.; Lanier, A.P.; Helzer, L.J.; Tom-Orme, L.; Murtaugh, M.A.; Slattery, M.L. Traditional foods and physical activity patterns and associations with cultural factors in a diverse Alaska Native population. Int. J. Circumpolar Health 2008, 67, 335–348. [Google Scholar] [CrossRef] [Green Version]
- Bersamin, A.; Izumi, B.T.; Nu, J.; O’Brien, D.M.; Paschall, M. Strengthening adolescents’ connection to their traditional food system improves diet quality in remote Alaska Native communities: Results from the Neqa Elicarvigmun Pilot Study. Transl. Behav. Med. 2019, 9, 952–961. [Google Scholar] [CrossRef] [PubMed]
- Howard, B.V.; Devereux, R.D.; Cole, S.A.; Davidson, M.; Dyke, B.; Ebbesson, S.O.E.; Epstein, S.E.; Robinson, D.R.; Jarvis, B.; Kaufman, D.J.; et al. A genetic and epidemiologic study of cardiovascular disease in Alaska Natives (GOCADAN): Design and methods. Int. J. Circumpolar Health 2005, 64, 206–221. [Google Scholar] [CrossRef] [PubMed]
- Koller, K.R.; Flanagan, C.A.; Nu, J.; Lee, F.R.; Desnoyers, C.; Walch, A.; Alexie, L.; Bersamin, A.; Thomas, T.K. Storekeeper perspectives on improving dietary intake in 12 rural remote western Alaska communities: The “Got Neqpiaq?” project. Int. J. Circumpolar Health 2021, 80, 1961393. [Google Scholar] [CrossRef] [PubMed]
- Meter, K.; Goldenberg, M.P. Building Food Security in Alaska; Crossroads Resource Center: Minneapolis, MN, USA, 2014. [Google Scholar]
- Adler, A.I.; Boyko, E.J.; Schraer, C.D.; Murphy, N.J. Lower Prevalence of Impaired Glucose Tolerance and Diabetes Associated With Daily Seal Oil or Salmon Consumption among Alaska Natives. Diabetes Care 1994, 17, 1498–1501. [Google Scholar] [CrossRef] [PubMed]
- Ebbesson, S.O.E.; Adler, A.I.; Risica, P.M.; Ebbesson, L.O.E.; Yeh, J.-L.; Go, O.T.; Doolittle, W.; Ehlert, G.; Swenson, M.; Robbins, D.C. Cardiovascular disease and risk factors in three Alaskan Eskimo populations: The Alaska-Siberia project. Int. J. Circumpolar Health 2005, 64, 365–386. [Google Scholar] [CrossRef]
- Makhoul, Z.; Kristal, A.R.; Gulati, R.; Luick, B.; Bersamin, A.; Boyer, B.; Mohatt, G.V. Associations of very high intakes of eicosapentaenoic and docosahexaenoic acids with biomarkers of chronic disease risk among Yup’ik Eskimos. Am. J. Clin. Nutr. 2010, 91, 777–785. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parkinson, A.J.; Cruz, A.L.; Heyward, W.L.; Bulkow, L.R.; Hall, D.; Barstaed, L.; Connor, W.E. Elevated concentrations of plasma ω-3 polyunsaturated fatty acids among Alaskan Eskimos. Am. J. Clin. Nutr. 1994, 59, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Ruscica, M.; Sirtori, C.R.; Carugo, S.; Calder, P.C.; Corsini, A. Omega-3 and cardiovascular prevention—Is this still a choice? Pharmacol. Res. 2022, 182, 106342. [Google Scholar] [CrossRef] [PubMed]
- Boyer, B.B.; Hopkins, S.E.; Wiener, H.W.; Purnell, J.Q.; O’Brien, D.M.; Zhang, C.X.; Aslan, J.E.; Aliwarga, T.; Pomeroy, J.J.; Thummel, K.E.; et al. Habitual Intake of Marine-Derived n-3 PUFAs is Inversely Associated with a Cardiometabolic Inflammatory Profile in Yup’ik Alaska Native People. J. Nutr. 2022, 152, 844–855. [Google Scholar] [CrossRef] [PubMed]
- Crouch, M.C.; Skan, J.; David, E.J.R.; Lopez, E.D.S.; Prochaska, J.J. Indigenizing Quality of Life: The Goodness of Life for Every Alaska Native Research Study. Appl. Res. Qual. Life 2021, 16, 1123–1143. [Google Scholar] [CrossRef]
- Henson, M.; Sabo, S.; Trujillo, A.; Teufel-Shone, N. Identifying Protective Factors to Promote Health in American Indian and Alaska Native Adolescents: A Literature Review. J. Prim. Prev. 2017, 38, 5–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Utsey, S.O.; Chae, M.H.; Brown, C.F.; Kelly, D. Effect of ethnic group membership on ethnic identity, race-related stress, and quality of life. Cult. Divers. Ethn. Minor. Psychol. 2002, 8, 366–377. [Google Scholar] [CrossRef]
- Tomaszewski, M.; White, C.; Patel, P.; Masca, N.; Damani, R.; Hepworth, J.; Samani, N.J.; Gupta, P.; Madira, W.; Stanley, A.; et al. High rates of non-adherence to antihypertensive treatment revealed by high-performance liquid chromatography-tandem mass spectrometry (HP LC-MS/MS) urine analysis. Heart 2014, 100, 855–861. [Google Scholar] [CrossRef] [Green Version]
- Huser, M.A.; Evans, T.S.; Berger, V. Medication adherence trends with statins. Adv. Ther. 2005, 22, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Fung, V.; Graetz, I.; Reed, M.; Jaffe, M.G. Patient-reported adherence to statin therapy, barriers to adherence, and perceptions of cardiovascular risk. PLoS ONE 2018, 13, e0191817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ebrahim, S.; Taylor, F.; Ward, K.; Beswick, A.; Burke, M.; Smith, G.D. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database Syst. Rev. 2011, 1, CD001561. [Google Scholar] [CrossRef] [Green Version]
- Atkins, D.; Clancy, C. Multiple risk factors interventions: Are we up to the challenge? Am. J. Prev. Med. 2004, 27 (Suppl. S2.), 102–103. [Google Scholar] [CrossRef] [PubMed]
- Orleans, C.T. Addressing multiple behavioral health risks in primary care: Broadening the focus of health behavior change research and practice. Am. J. Prev. Med. 2004, 27, 1–3. [Google Scholar] [CrossRef] [PubMed]
- PAR-11-346: Interventions for Health Promotion and Disease Prevention in Native American Populations (R01). Available online: https://grants.nih.gov/grants/guide/pa-files/PAR-11-346.html (accessed on 1 January 2015).
- Johnson, S.S.; Driskell, M.-M.; Johnson, J.L.; Dyment, S.J.; Prochaska, J.O.; Prochaska, J.M.; Bourne, L. Transtheoretical Model Intervention for Adherence to Lipid-Lowering Drugs. Dis. Manag. 2006, 9, 102–114. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.S.; Driskell, M.-M.; Johnson, J.L.; Prochaska, J.M.; Zwick, W.; Prochaska, J.O. Efficacy of a Transtheoretical Model-Based Expert System For Antihypertensive Adherence. Dis. Manag. 2006, 9, 291–301. [Google Scholar] [CrossRef]
- Knox, M.; Skan, J.; Benowitz, N.L.; Schnellbaecher, M.; Prochaska, J.J. Recruitment best practices of a cardiovascular risk reduction randomised control trial in rural Alaska Native communities. Int. J. Circumpolar Health 2020, 79, 1806639. [Google Scholar] [CrossRef]
- Prochaska, J.J.; Epperson, A.; Skan, J.; Oppezzo, M.; Barnett, P.; Delucchi, K.; Schnellbaecher, M.; Benowitz, N.L. The Healing and Empowering Alaskan Lives Toward Healthy-Hearts (HEALTHH) Project: Study protocol for a randomized controlled trial of an intervention for tobacco use and other cardiovascular risk behaviors for Alaska Native People. Contemp. Clin. Trials 2018, 71, 40–46. [Google Scholar] [CrossRef] [Green Version]
- Renner, C.C.; Lanier, A.P.; Lindgren, B.; Jensen, J.; Patten, C.A.; Parascandola, M.; Benowitz, N.L.; Tyndale, R.F.; Hatsukami, D.K. Tobacco Use Among Southwestern Alaska Native People. Nicotine Tob. Res. 2013, 15, 401–406. [Google Scholar] [CrossRef] [Green Version]
- Vidyo. Available online: https://www.vidyo.com/ (accessed on 25 May 2022).
- Prochaska, J.O.; DiClemente, C.C. Stages and processes of self-change of smoking: Toward an integrative model of change. J. Consult. Clin. Psychol. 1983, 51, 390–395. [Google Scholar] [CrossRef]
- Benowitz, N.L.; Renner, C.C.; Lanier, A.P.; Tyndale, R.F.; Hatsukami, D.K.; Lindgren, B.; Stepanov, I.; Watson, C.H.; Sosnoff, C.S.; Jacob, P., 3rd. Exposure to Nicotine and Carcinogens among Southwestern Alaskan Native Cigarette Smokers and Smokeless Tobacco Users. Cancer Epidemiol. Biomark. Prev. 2012, 21, 934–942. [Google Scholar] [CrossRef] [Green Version]
- Binnington, M.J.; Zhu, A.Z.X.; Renner, C.C.; Lanier, A.P.; Hatsukami, D.K.; Benowitz, N.L.; Tyndale, R.F. CYP2A6 and CYP2B6 genetic variation and its association with nicotine metabolism in South Western Alaska Native people. Pharmacogenet. Genom. 2012, 22, 429–440. [Google Scholar] [CrossRef] [Green Version]
- Alaska Native Tribal Health Consortium. Traditional Food Guide for the Alaska Native People, 2nd ed.; Alaska Native Tribal Health Consortium: Anchorage, AK, USA, 2015. [Google Scholar]
- U.S. Department of Health and Human Services; U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans, 8th ed.; December 2015. Available online: https://health.gov/our-work/food-nutrition/previous-dietary-guidelines/2015 (accessed on 1 January 2020).
- Slattery, M.L.; Murtaugh, M.A.; Schumacher, M.C.; Johnson, J.; Edwards, S.; Edwards, R.; Benson, J.; Tom-Orme, L.; Lanier, A.P. Development, Implementation, and Evaluation of a Computerized Self-Administered Diet History Questionnaire for Use in Studies of American Indian and Alaskan Native People. J. Am. Diet. Assoc. 2008, 108, 101–109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinberg, D.; Bennett, G.G.; Svetkey, L. The DASH Diet, 20 Years Later. JAMA 2017, 317, 1529–1530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morisky, D.E.; Green, L.W.; Levine, D.M. Concurrent and Predictive Validity of a Self-reported Measure of Medication Adherence. Med. Care 1986, 24, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Adler, N.E.; Epel, E.S.; Castellazzo, G.; Ickovics, J.R. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy, White women. Health Psychol. 2000, 19, 586–592. [Google Scholar] [CrossRef]
- Walch, A.; Bersamin, A.; Loring, P.; Johnson, R.; Tholl, M. A scoping review of traditional food security in Alaska. Int. J. Circumpolar Health 2018, 77, 1419678. [Google Scholar] [CrossRef]
- Skan, J.; Benowitz, N.L.; Prochaska, J.J. Acceptability of a Telemedicine Cardiovascular Disease Prevention Intervention for Alaska Native Men and Women Who Smoke Cigarettes. In Proceedings of the 2018 Annual Meeting of the Society for Research on Nicotine and Tobacco, Baltimore, MD, USA, 21–24 February 2018. [Google Scholar]
- Centers for Disease Control and Prevention. PRS Efficacy Criteria for Best-Evidence (Tier I) Risk Reduction (RR) Indivdiual-Level and Group-Level Interventions (ILIs/GLIs). Available online: https://www.cdc.gov/hiv/pdf/research/interventionresearch/compendium/rr/RR_Chapter_Best_Efficacy_Criteria_ILI_GLI_CPLs.pdf (accessed on 28 November 2012).
- Osler, M.; Heitmann, B.L. The Validity of a Short Food Frequency Questionnaire and its Ability to Measure Changes in Food Intake: A Longitudinal Study. Int. J. Epidemiology 1996, 25, 1023–1029. [Google Scholar] [CrossRef] [PubMed]
- Yuan, C.; Spiegelman, D.; Rimm, E.B.; Rosner, B.A.; Stampfer, M.J.; Barnett, J.B.; Chavarro, J.E.; Rood, J.C.; Harnack, L.J.; Sampson, L.K.; et al. Relative Validity of Nutrient Intakes Assessed by Questionnaire, 24-Hour Recalls, and Diet Records as Compared With Urinary Recovery and Plasma Concentration Biomarkers: Findings for Women. Am. J. Epidemiol. 2018, 187, 1051–1063. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Treatment Component | Condition 1: Smoking Cessation + Physical Activity | Condition 2: Nutrition and Medication Adherence |
|---|---|---|
| Manual 1 | Provided at baseline | Provided at baseline |
| 30-min Counseling 1 Telehealth, computerized Tailored to condition and participant | Baseline, 3-mo, 6-mo, 12-mo | Baseline, 3-mo, 6-mo, 12-mo |
| Prochange report (mailed) | After Baseline, 3-mo, 6-mo, 12-mo | After Baseline, 3-mo, 6-mo, 12-mo |
| Swag | Provided at baseline. Items: Pedometer; 12-weeks of NRT | Provided at baseline. Items: Cookbook; Medication bag |
| Nutrition + Medication Adherence (N = 151) | Tobacco + Physical Activity (N = 148) | Full Sample (N = 299) | |
|---|---|---|---|
| M (SD)/N (%) | M (SD)/N (%) | M (SD)/N (%) | |
| Age (M/SD) | 47.0 (13.4) | 45.5 (14.7) | 46.3 (14.0) |
| Gender (N/%) | |||
| Male | 77 (51.0%) | 77 (52.0%) | 154 (51.5%) |
| Female | 74 (49.0%) | 71 (48.0%) | 145 (48.5%) |
| Highest Education Level (N/%) | |||
| Elementary/some high school | 38 (25.2%) | 23 (15.5%) | 61 (20.4%) |
| High school graduate | 83 (55.0%) | 95 (64.2%) | 178 (59.5%) |
| Some college | 26 (17.2%) | 26 (17.2%) | 52 (17.4%) |
| College degree or higher | 3 (2.0%) | 4 (2.7%) | 7 (2.3%) |
| Community Connectedness (M/SD) | 5.7 (2.5) | 5.6 (2.6) | 5.3 (2.1) |
| Residence (N/%) | |||
| Nome | 31 (20.5%) | 38 (25.7%) | 69 (23.1%) |
| Another Norton Sound community | 120 (79.5%) | 110 (74.4%) | 230 (76.9%) |
| Nutrition Measures (M/SD) | |||
| Heart-healthy foods ratio (%) | 40% (19) | 42% (20) | 41% (20) |
| Traditional healthy foods ratio 1 | 17% (13) | 19% (15) | 18% (14) |
| Total servings heart-healthy foods 2 | 19.9 (15.2) | 21.5(20.4) | 20.7 (18.0) |
| Total servings traditional heart-healthy foods | 8.5 (9.3) | 9.5 (11.0) | 9.0 (10.1) |
| Total servings unhealthy foods | 27.9 (18.1) | 27.7 (21.8) | 27.8 (20.0) |
| Medication Adherence 3 | |||
| Recent medication adherent | 55/71 (77%) | 49/67 (73%) | 104/138 (75%) |
| Typical medication adherent | 36/72 (50%) | 33/67 (49%) | 69/139 (50%) |
| Action 4: Blood pressure medication | 44/57 (77%) | 48/67 (72%) | 92/124 (74%) |
| Action 4: Cholesterol medication | 33/40 (83%) | 24/38 (63%) | 57/78 (73%) |
| M (SD) Servings per Week | |||||
|---|---|---|---|---|---|
| Group | Baseline | 3-mo | 6-mo | 12-mo | 18-mo |
| Nutrition/Medication Adherence | |||||
| Unhealthy foods | 27.9 | 27.8 | 26.5 | 24.4 | 26.0 |
| (18.1) | (16.6) | (17.1) | (17.7) | (21.2) | |
| Heart healthy foods | 19.9 | 20.2 | 21.9 | 19.2 | 20.2 |
| (15.2) | (13.0) | (15.5) | (15.0) | (16.5) | |
| Traditional heart-healthy foods, age ≤ 46 years 1 | 5.5 | 7.2 | 5.9 | 5.6 | 6.9 |
| (6.3) | (6.4) | (4.8) | (4.9) | (5.9) | |
| Traditional heart-healthy foods, age ≥ 47 years 1 | 11.1 | 9.5 | 12.0 | 9.7 | 9.8 |
| (10.8) | (8.8) | (9.6) | (9.7) | (9.9) | |
| Tobacco/Physical Activity | |||||
| Unhealthy foods | 27.7 | 26.2 | 26.9 | 25.9 | 26.0 |
| (21.8) | (17.0) | (16.9) | (16.2) | (13.4) | |
| Heart healthy foods | 21.5 | 20.1 | 20.9 | 20.8 | 20.7 |
| (20.4) | (13.9) | (16.3) | (15.8) | (14.0) | |
| Traditional heart-healthy foods, age ≤ 46 years 1 | 8.3 | 6.7 | 7.9 | 7.8 | 7.9 |
| (8.4) | (5.6) | (7.2) | (8.3) | (8.3) | |
| Traditional heart-healthy foods, age ≥ 47 years 1 | 10.8 | 10.0 | 9.8 | 8.8 | 7.1 |
| (13.1) | (8.2) | (8.8) | (7.4) | (5.6) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oppezzo, M.; Knox, M.; Skan, J.; Chieng, A.; Crouch, M.; Aikens, R.C.; Benowitz, N.L.; Schnellbaecher, M.; Prochaska, J.J. Traditional Heart-Healthy Diet and Medication Adherence in the Norton Sound Region: An 18-Month Telehealth Intervention. Int. J. Environ. Res. Public Health 2022, 19, 9885. https://doi.org/10.3390/ijerph19169885
Oppezzo M, Knox M, Skan J, Chieng A, Crouch M, Aikens RC, Benowitz NL, Schnellbaecher M, Prochaska JJ. Traditional Heart-Healthy Diet and Medication Adherence in the Norton Sound Region: An 18-Month Telehealth Intervention. International Journal of Environmental Research and Public Health. 2022; 19(16):9885. https://doi.org/10.3390/ijerph19169885
Chicago/Turabian StyleOppezzo, Marily, Mariah Knox, Jordan Skan, Amy Chieng, Maria Crouch, Rachael C. Aikens, Neal L. Benowitz, Matthew Schnellbaecher, and Judith J. Prochaska. 2022. "Traditional Heart-Healthy Diet and Medication Adherence in the Norton Sound Region: An 18-Month Telehealth Intervention" International Journal of Environmental Research and Public Health 19, no. 16: 9885. https://doi.org/10.3390/ijerph19169885






