Utilization of Mental Health Support Systems in the Aftermath of Disasters in Japan: Statistical Data of the Miyagi Disaster Mental Health Care Center
Abstract
:1. Introduction
1.1. Mental Health Needs Depend on Recovery Phases
1.2. The Post-Disaster Mental Health System in Japan
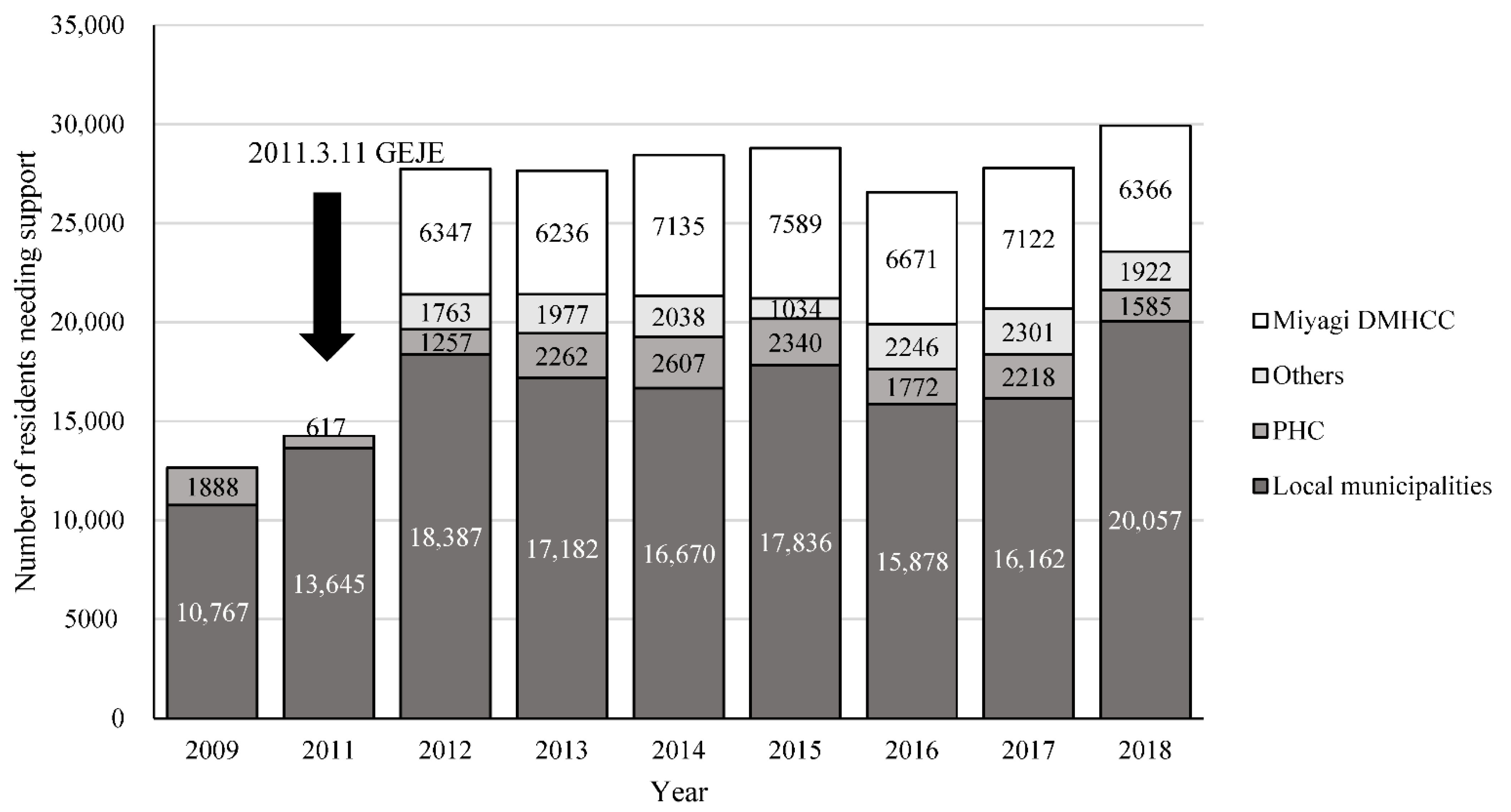
1.3. The GEJE and the Miyagi DMHCC
2. Methods
2.1. Study Design
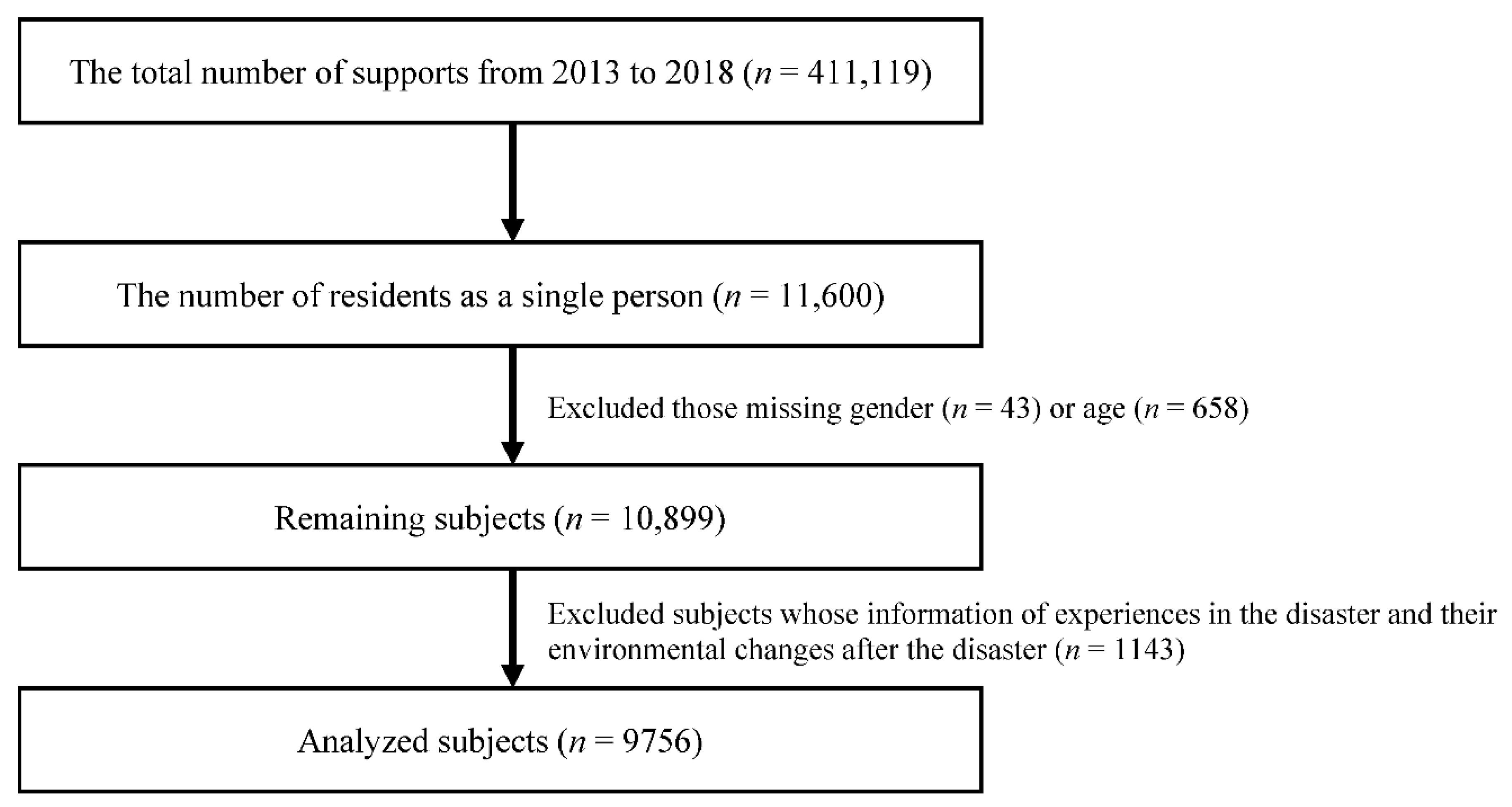
2.2. Participants
2.3. Statistical Analyses
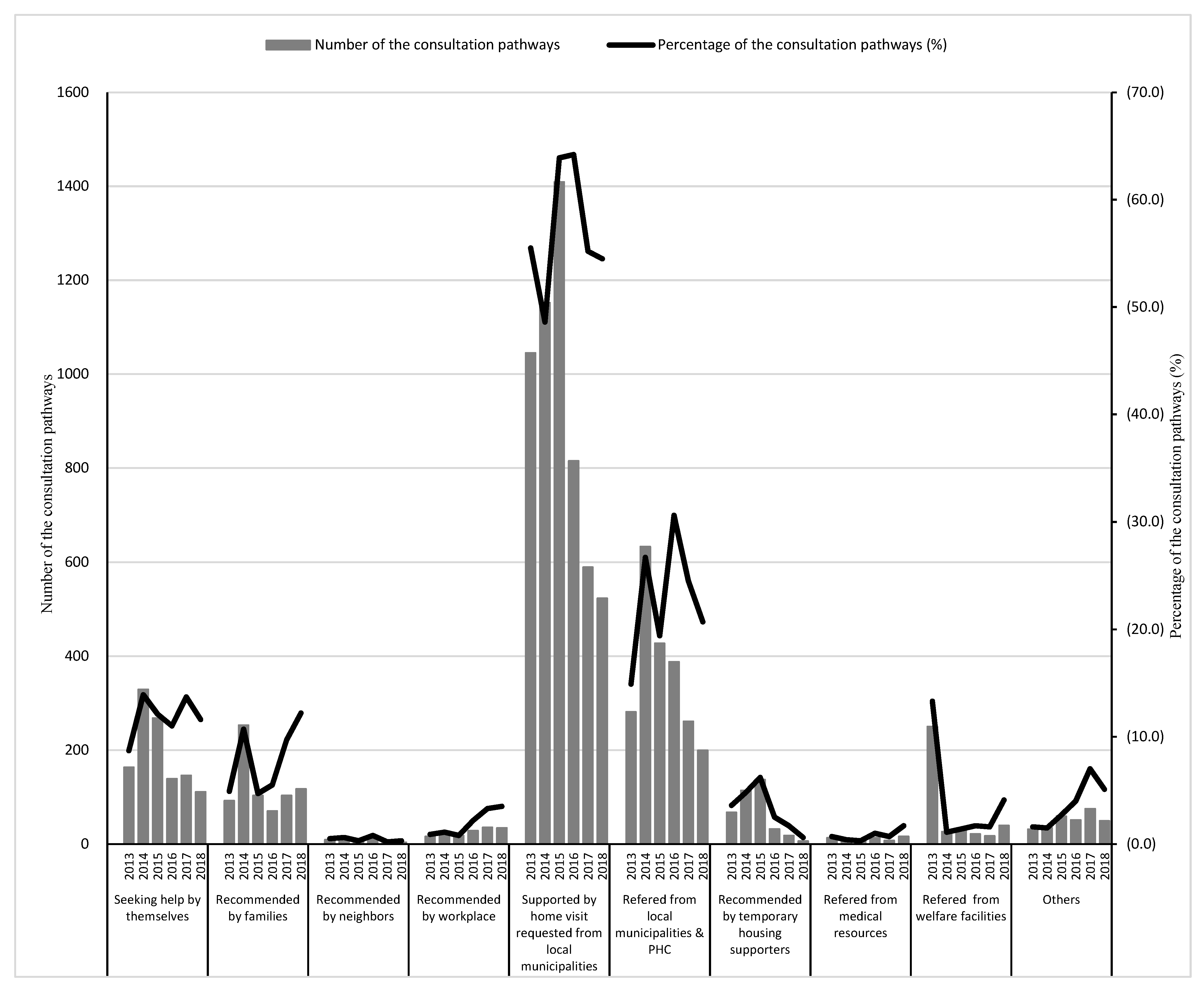
3. Results
4. Discussion
5. Conclusions
Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fergusson, D.M.; Horwood, L.J.; Boden, J.M.; Mulder, R.T. Impact of a Major Disaster on the Mental Health of a Well-Studied Cohort. JAMA Psychiatry 2014, 71, 1025–1031. [Google Scholar] [CrossRef]
- North, C.S.; Pfefferbaum, B. Mental Health Response to Community Disasters: A Systematic Review. JAMA 2013, 310, 507–518. [Google Scholar] [CrossRef] [PubMed]
- Ommeren, M.V.; Saxena, S.; Saraceno, B. Aid after disasters needs a long term public mental health perspective. BMJ Open 2005, 330, 116–1161. [Google Scholar] [CrossRef]
- Beaglehole, B.; Mulder, R.T.; Frampton, C.M.; Boden, J.M.; Newton-Howes, G.; Bell, C.J. Psychological Distress and Psychiatric Disorder After Natural Disasters: Systematic Review and Meta-Analysis. Br. J. Psychiatry 2018, 213, 716–722. [Google Scholar] [CrossRef]
- North, C.S.; Oliver, J.; Pandya, A. Examining a Comprehensive Model of Disaster-Related Posttraumatic Stress Disorder in Systematically Studied Survivors of 10 Disasters. Am. J. Public Health 2012, 102, e40–e48. [Google Scholar] [CrossRef] [PubMed]
- McCarroll, J.E.; Ursano, R.J.; Fullerton, C.S.; Liu, X.; Lundy, A. Somatic Symptoms in Gulf War Mortuary Workers. Psychosom. Med. 2002, 64, 29–33. [Google Scholar] [CrossRef]
- Tsuboya, T.; Inoue, M.; Satoh, M.; Asayama, K. Perspectives acquired through long-term epidemiological studies on the Great East Japan Earthquake. Environ. Health Prev. Med. 2017, 22, 3. [Google Scholar] [CrossRef]
- Bosmans, M.W.G.; van der Velden, P.G. The Effect of Employment Status in Post Disaster Recovery: A Longitudinal Comparative Study Among Employed and Unemployed Affected Residents. J. Trauma. Stress 2018, 31, 460–466. [Google Scholar] [CrossRef]
- Yabe, Y.; Hagiwara, Y.; Sekiguchi, T.; Sugawara, Y.; Tsuchiya, M.; Itaya, N.; Yoshida, S.; Sogi, Y.; Yano, T.; Onoki, T.; et al. Musculoskeletal Pain and New-Onset Poor Physical Function in Elderly Survivors of a Natural Disaster: A Longitudinal Study After the Great East Japan Earthquake. BMC Geriatr. 2019, 19, 274. [Google Scholar] [CrossRef]
- Schoenbaum, M.; Butler, B.; Kataoka, S.; Norquist, G.; Springgate, B.; Sullivan, G.; Duan, N.; Kessler, R.C.; Wells, K. Promoting Mental Health Recovery After Hurricanes Katrina and Rita: What Can Be Done at What Cost. Arch. Gen. Psychiatry 2009, 66, 906–914. [Google Scholar] [CrossRef]
- McFarlane, A.C.; Williams, R. Mental Health Services Required After Disasters: Learning From the Lasting Effects of Disasters. Depress. Res. Treat. 2012, 2012, 970194. [Google Scholar] [CrossRef] [PubMed]
- Houston, J.B.; Spialek, M.L.; Stevens, J.; First, J.; Mieseler, V.L.; Pfefferbaum, B. 2011 Joplin, Missouri Tornado Experience, Mental Health Reactions, and Service Utilization: Cross-Sectional Assessments at Approximately 6 Months and 2.5 Years Post-Event. PLoS Curr. 2015, 7, PMC4639320. [Google Scholar] [CrossRef]
- Brown, L.M.; Framingham, J.L.; Frahm, K.A.; Wolf, L.D. Crisis Counselors’ Perceptions and Assessment of Suicidal Behavior Among Hurricane Survivors Receiving Crisis Counseling Services. Disaster Med. Public Health Prep. 2015, 9, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.; Hameed, A. Mental Health and Psychosocial Response After the Worst Natural Disaster in the History of the Maldives. Int. Rev. Psychiatry 2006, 18, 567–572. [Google Scholar] [CrossRef] [PubMed]
- Contreras, C.; Aguilar, M.; Eappen, B.; Guzmán, C.; Carrasco, P.; Millones, A.K.; Galea, J.T. Community Strengthening and Mental Health System Linking After Flooding in Two Informal Human Settlements in Peru: A Model for Small-Scale Disaster Response. Glob. Ment. Health 2018, 5, e11. [Google Scholar] [CrossRef]
- Raviola, G.; Rose, A.; Fils-Aimé, J.R.; Thérosmé, T.; Affricot, E.; Valentin, C.; Daimyo, S.; Coleman, S.; Dubuisson, W.; Wilson, J.; et al. Development of a comprehensive, sustained community mental health system in post-earthquake Haiti, 2010–2019. Global Mental Health. 2020, 11, e6. [Google Scholar] [CrossRef]
- Fire Disaster Management Agency. The Damage Situation Caused by the Great East Japan Earthquake in 2011. Available online: https://www.fdma.go.jp/disaster/higashinihon/items/159.pdf (accessed on 1 February 2022).
- Shinfuku, N. Disaster Mental Health: Lessons Learned From the Hanshin Awaji Earthquake. World Psychiatry 2002, 1, 158–159. [Google Scholar]
- Disaster Psychiatric Assistance Team. Outline of the DPAT. Available online: https://www.dpat.jp/images/dpat_documents/2.pdf (accessed on 1 February 2022).
- Takahashi, S.; Takagi, Y.; Fukuo, Y.; Arai, T.; Watari, M.; Tachikawa, H. Acute mental health needs duration during major disasters: A phenomenological experience of disaster psychiatric assistance teams (DPATs) in Japan. Int. J. Environ. Res. Public Health 2020, 17, 1530. [Google Scholar] [CrossRef]
- Takagi, Y.; Takahashi, S.; Fukuo, Y.; Arai, T.; Tachikawa, H. Acute-Stage Mental Health Symptoms by Natural Disaster Type: Consultations of Disaster Psychiatric Assistance Teams (DPATs) in Japan. Int. J. Environ. Res. Public Health 2021, 18, 12409. [Google Scholar] [CrossRef]
- Nomura, S.; Parsons, A.J.Q.; Hirabayashi, M.; Kinoshita, R.; Liao, Y.; Hodgson, S. Social determinants of mid- to long-term disaster impacts on health: A systematic review. Int. J. Disaster Risk Reduct. 2016, 16, 53–67. [Google Scholar] [CrossRef]
- Kayano, R.; Lin, M.; Shinozaki, Y.; Nomura, S.; Kim, Y. Long-term mental health support after natural hazard events: A report from an online survey among experts in Japan. Int. J. Environ. Res. Public Health 2022, 19, 3022. [Google Scholar] [CrossRef] [PubMed]
- Kato, H. Posttraumatic Symptoms Among Victims of the Great Hanshin-Awaji Earthquake in Japan. Psychiatry Clin. Neurosci. 1998, 52, S19–S25. [Google Scholar] [CrossRef]
- The Office of the 10th Year Restoration Committee. The Great Hanshin-Awaji Earthquake: The Report of the 10-Year Reconstruction Overall Verification and Recommendations; The Great Hanshin-Awaji Earthquake Memorial Research Institute: Kobe, Japan, 2004. [Google Scholar]
- Ministry of Health, Labour and Welfare Japan. Status of Suicide in 2020. Available online: https://www.npa.go.jp/safetylife/seianki/jisatsu/R03/R02_jisatuno_joukyou.pdf (accessed on 1 February 2022). (In Japanese)
- Miyagi Prefectural Government. Health and Welfare. Available online: https://www.pref.miyagi.jp/life/5/index.html (accessed on 1 February 2022). (In Japanese)
- Otsuka, K.; Sakai, S.; Nakamura, H.; Akahira, M. Mental health activities following the Great East Japan Earthquake in the stricken coastal area of Iwate Prefecture. Seishin Shinkeigaku Zasshi 2013, 115, 485–491. [Google Scholar] [PubMed]
- Uchida, T.; Matsumoto, K.; Takahashi, Y.; Koshimichi, R.; Sakuma, A.; Katsura, M.; Sato, H.; Ueda, I.; Matsuoka, H. Activity to prevent mental diseases after the Great East Japan Earthquake. Seishin Shinkeigaku Zasshi 2014, 116, 203–208. [Google Scholar]
- Weiss, R.S.; Bass, S.A.; Heimovitz, H.K.; Oka, M. Japan’s Silver Human Resource Centers and Participant Well-Being. J. Cross-Cult. Gerontol. 2005, 20, 47–66. [Google Scholar] [CrossRef]
- Kusama, T.; Aida, J.; Sugiyama, K.; Matsuyama, Y.; Koyama, S.; Sato, Y.; Yamamoto, T.; Igarashi, A.; Tsuboya, T.; Osaka, K. Does the Type of Temporary Housing Make a Difference in Social Participation and Health for Evacuees of the Great East Japan Earthquake and Tsunami? A Cross-Sectional Study. J. Epidemiol. 2019, 29, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Matsuyama, Y.; Aida, J.; Hase, A.; Sato, Y.; Koyama, S.; Tsuboya, T.; Osaka, K. Do Community- and Individual-Level Social Relationships Contribute to the Mental Health of Disaster Survivors?: A Multilevel Prospective Study After the Great East Japan Earthquake. Soc. Sci. Med. 2016, 151, 187–195. [Google Scholar] [CrossRef]
- Ministry of Health, Labor and Welfare. Efforts for the Great East Japan Earthquake and Employment Situation in the Affected Areas; The white paper on Labor and Economy 2012 Labor. Available online: https://www.mhlw.go.jp/wp/hakusyo/roudou/12/ (accessed on 1 February 2022).
- Bromet, E.; Dew, M.A. Review of psychiatric epidemiologic research on disasters. Epidemiol. Rev. 1995, 17, 113–119. [Google Scholar] [CrossRef]
- McMurray, L.; Steiner, W. Natural disasters and service delivery to individuals with severe mental illness—Ice storm 1998. Can. J. Psychiatry 2000, 45, 383–385. [Google Scholar] [CrossRef]
- Sakuma, A.; Ueda, I.; Rengi, S.; Shingai, T.; Matsuoka, H.; Matsumoto, K. Increase in the number of admissions to psychiatric hospitals immediately after the Great East Japan Earthquake. Asia Pac. Psychiatry 2018, 10, e12307. [Google Scholar] [CrossRef]
- DiGangi, J.A.; Gomez, D.; Mendoza, L.; Jason, L.A.; Keys, C.B.; Koenen, K.C. Pretrauma risk factors for posttraumatic stress disorder: A systematic review of the literature. Clin. Psychol. Rev. 2013, 33, 728–744. [Google Scholar] [CrossRef] [PubMed]
- Maguen, S.; Neira, Y.; Conoscenti, L.M.; Litz, B.T. Depression and prolonged grief in the wake of disasters. In Mental health and disasters; Neira, Y., Galea, S., Norris, F.H., Eds.; Cambridge University Press: New York, NY, USA, 2009; pp. 116–130. [Google Scholar]
- Van der Velden, P.G.; Kleber, R.J. Substance use and misuse after disaster. In Mental Health and Disasters; Neira, Y., Galea, S., Norris, F.H., Eds.; Cambridge University Press: New York, NY, USA, 2009; pp. 94–115. [Google Scholar]
| 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 1882) | (n = 2372) | (n = 2206) | (n = 1269) | (n = 1067) | (n = 960) | |||||||||
| No | % | No | % | No | % | No | % | No | % | No | % | p-Value | χ2 | |
| No | ||||||||||||||
| Male | 729 | (38.7) | 1084 | (45.7) | 994 | (45.1) | 563 | (44.4) | 476 | (44.6) | 480 | (50.0) | <0.001 | 38.7 |
| Female | 1153 | (61.3) | 1288 | (54.3) | 1212 | (54.9) | 706 | (55.6) | 591 | (55.4) | 480 | (50.0) | ||
| Age group | ||||||||||||||
| Less than 20 years old | 37 | (2.0) | 70 | (3.0) | 57 | (2.6) | 55 | (4.3) | 79 | (7.4) | 106 | (11.0) | <0.001 | 4193.1 |
| 20–30 years old | 110 | (5.8) | 102 | (4.3) | 117 | (5.3) | 71 | (5.6) | 73 | (6.8) | 61 | (6.4) | ||
| 30–40 years old | 189 | (10.0) | 193 | (8.1) | 199 | (9.0) | 150 | (11.8) | 135 | (12.7) | 86 | (9.0) | ||
| 40–50 years old | 283 | (15.0) | 304 | (12.8) | 295 | (13.4) | 163 | (12.8) | 159 | (14.9) | 127 | (13.2) | ||
| 50–60 years old | 313 | (16.6) | 334 | (14.1) | 322 | (14.6) | 175 | (13.8) | 145 | (13.6) | 146 | (15.2) | ||
| 60–70 years old | 434 | (23.1) | 636 | (26.8) | 529 | (24.0) | 292 | (23.0) | 230 | (21.6) | 205 | (21.4) | ||
| 70 years old or more | 516 | (27.4) | 733 | (30.9) | 687 | (31.1) | 363 | (28.6) | 246 | (23.1) | 229 | (23.9) | ||
| Life backgrounds before the disaster | ||||||||||||||
| Lived alone Yes (vs. No) | 1495 | (79.4) | 1742 | (73.4) | 1623 | (73.6) | 926 | (73.0) | 790 | (74.0) | 705 | (73.4) | <0.001 | 28.8 |
| Had a history of visiting psychiatric facilities Yes (vs. No) | 335 | (17.8) | 814 | (34.3) | 380 | (17.2) | 211 | (16.6) | 198 | (18.6) | 176 | (18.3) | <0.001 | 297.2 |
| Experiences that could be a psychological burden during the disaster | ||||||||||||||
| Lost loved ones Yes (vs. No) | 276 | (14.7) | 393 | (16.6) | 250 | (11.3) | 157 | (12.4) | 102 | (9.6) | 107 | (11.1) | <0.001 | 50.5 |
| Had been injured Yes (vs. No) | 46 | (2.4) | 145 | (6.1) | 87 | (3.9) | 24 | (1.9) | 11 | (1.0) | 12 | (1.3) | <0.001 | 102.8 |
| Had a near-death experience Yes (vs. No) | 394 | (20.9) | 545 | (23.0) | 335 | (15.2) | 191 | (15.1) | 102 | (9.6) | 105 | (10.9) | <0.001 | 155.0 |
| Lost of their community Yes (vs. No) | 421 | (22.4) | 726 | (30.6) | 335 | (30.6) | 322 | (25.4) | 234 | (21.9) | 241 | (25.1) | <0.001 | 68.1 |
| Lost their job Yes (vs. No) | 171 | (9.1) | 287 | (12.1) | 335 | (5.7) | 65 | (5.1) | 44 | (4.1) | 44 | (4.6) | <0.001 | 128.1 |
| Seeking Help by Themselves (n = 1156) | Others (n = 8600) | ||||||
|---|---|---|---|---|---|---|---|
| No | % | No | % | p-Value | OR | 95%CI | |
| Male | 411 | (35.6) | 745 | (64.4) | <0.01 | 1.55 | (1.38–1.80) |
| Year | 0.05 | 1.04 | (1.00–1.09) | ||||
| 20–30 years old | 142 | (12.3) | 1014 | (87.7) | <0.01 | 3.39 | (2.27–5.07) |
| 30–40 years old | 203 | (17.6) | 953 | (82.4) | <0.01 | 2.48 | (1.69–3.65) |
| 40–50 years old | 221 | (19.1) | 935 | (80.9) | 0.01 | 1.63 | (1.11–2.40) |
| 50–60 years old | 158 | (13.7) | 998 | (86.3) | 0.55 | 1.13 | (0.76–1.67) |
| 60–70 years old | 219 | (18.9) | 937 | (81.1) | 0.79 | 0.95 | (0.65–1.39) |
| 70 years old or more | 178 | (15.4) | 978 | (84.6) | 0.10 | 0.72 | (0.49–1.06) |
| Lived alone | 834 | (72.1) | 322 | (27.9) | <0.01 | 0.75 | (0.65–0.87) |
| Had a history of visiting psychiatric facilities | 427 | (36.9) | 729 | (63.1) | <0.01 | 2.04 | (1.77–2.34) |
| Lost loved ones | 111 | (9.6) | 1045 | (90.4) | 0.05 | 0.80 | (0.64–1.00) |
| Had been injured | 18 | (1.6) | 1138 | (98.4) | 0.01 | 0.51 | (0.31–0.86) |
| Had a near-death experience | 187 | (16.2) | 969 | (83.8) | 0.55 | 0.94 | (0.78–1.14) |
| Lost their community | 250 | (21.6) | 906 | (78.4) | 0.53 | 0.95 | (0.81–1.12) |
| Lost their job | 117 | (10.1) | 1039 | (89.9) | <0.01 | 1.53 | (1.21–1.93) |
| Supported by Home Visits (n = 5533) | Others (n = 4223) | ||||||
|---|---|---|---|---|---|---|---|
| No | % | No | % | p-Value | OR | 95%CI | |
| Male | 2918 | (52.7) | 2615 | (47.3) | <0.01 | 0.71 | (0.64–0.77) |
| Year | <0.01 | 1.07 | (1.04–1.10) | ||||
| Less than 20 years old | 36 | (0.7) | 5497 | (99.3) | <0.01 | 0.03 | (0.02–0.04) |
| 20–30 years old | 191 | (3.5) | 5342 | (96.5) | <0.01 | 0.25 | (0.21–0.31) |
| 30–40 years old | 434 | (7.8) | 5099 | (92.2) | <0.01 | 0.39 | (0.33–0.46) |
| 40–50 years old | 633 | (11.4) | 4900 | (88.6) | <0.01 | 0.52 | (0.45–0.60) |
| 50–60 years old | 808 | (14.6) | 4725 | (85.4) | <0.01 | 0.67 | (0.58–0.77) |
| 60–70 years old | 1475 | (26.7) | 4058 | (73.3) | 0.01 | 0.83 | (0.73–0.95) |
| Lived alone | 4214 | (76.2) | 1319 | (23.8) | <0.01 | 1.41 | (1.27–1.56) |
| Had a history of visiting psychiatric facilities | 515 | (9.3) | 5018 | (90.7) | <0.01 | 0.19 | (0.17–0.21) |
| Lost loved ones | 703 | (12.7) | 4830 | (87.3) | 0.07 | 0.88 | (0.76–1.01) |
| Had been injured | 107 | (1.9) | 5426 | (98.1) | <0.01 | 0.33 | (0.25–0.44) |
| Had a near-death experience | 882 | (15.9) | 4651 | (84.1) | 0.50 | 0.95 | (0.83–1.09) |
| Lost their community | 1719 | (31.1) | 3814 | (68.9) | <0.01 | 1.54 | (1.38–1.73) |
| Lost their job | 393 | (7.1) | 5140 | (92.9) | 0.58 | 0.95 | (0.79–1.14) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fukuchi, N.; Chiba, S. Utilization of Mental Health Support Systems in the Aftermath of Disasters in Japan: Statistical Data of the Miyagi Disaster Mental Health Care Center. Int. J. Environ. Res. Public Health 2022, 19, 10856. https://doi.org/10.3390/ijerph191710856
Fukuchi N, Chiba S. Utilization of Mental Health Support Systems in the Aftermath of Disasters in Japan: Statistical Data of the Miyagi Disaster Mental Health Care Center. International Journal of Environmental Research and Public Health. 2022; 19(17):10856. https://doi.org/10.3390/ijerph191710856
Chicago/Turabian StyleFukuchi, Naru, and Shusaku Chiba. 2022. "Utilization of Mental Health Support Systems in the Aftermath of Disasters in Japan: Statistical Data of the Miyagi Disaster Mental Health Care Center" International Journal of Environmental Research and Public Health 19, no. 17: 10856. https://doi.org/10.3390/ijerph191710856
APA StyleFukuchi, N., & Chiba, S. (2022). Utilization of Mental Health Support Systems in the Aftermath of Disasters in Japan: Statistical Data of the Miyagi Disaster Mental Health Care Center. International Journal of Environmental Research and Public Health, 19(17), 10856. https://doi.org/10.3390/ijerph191710856









