Respiratory and Otolaryngology Symptoms Following the 2019 Spring Floods in Quebec
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
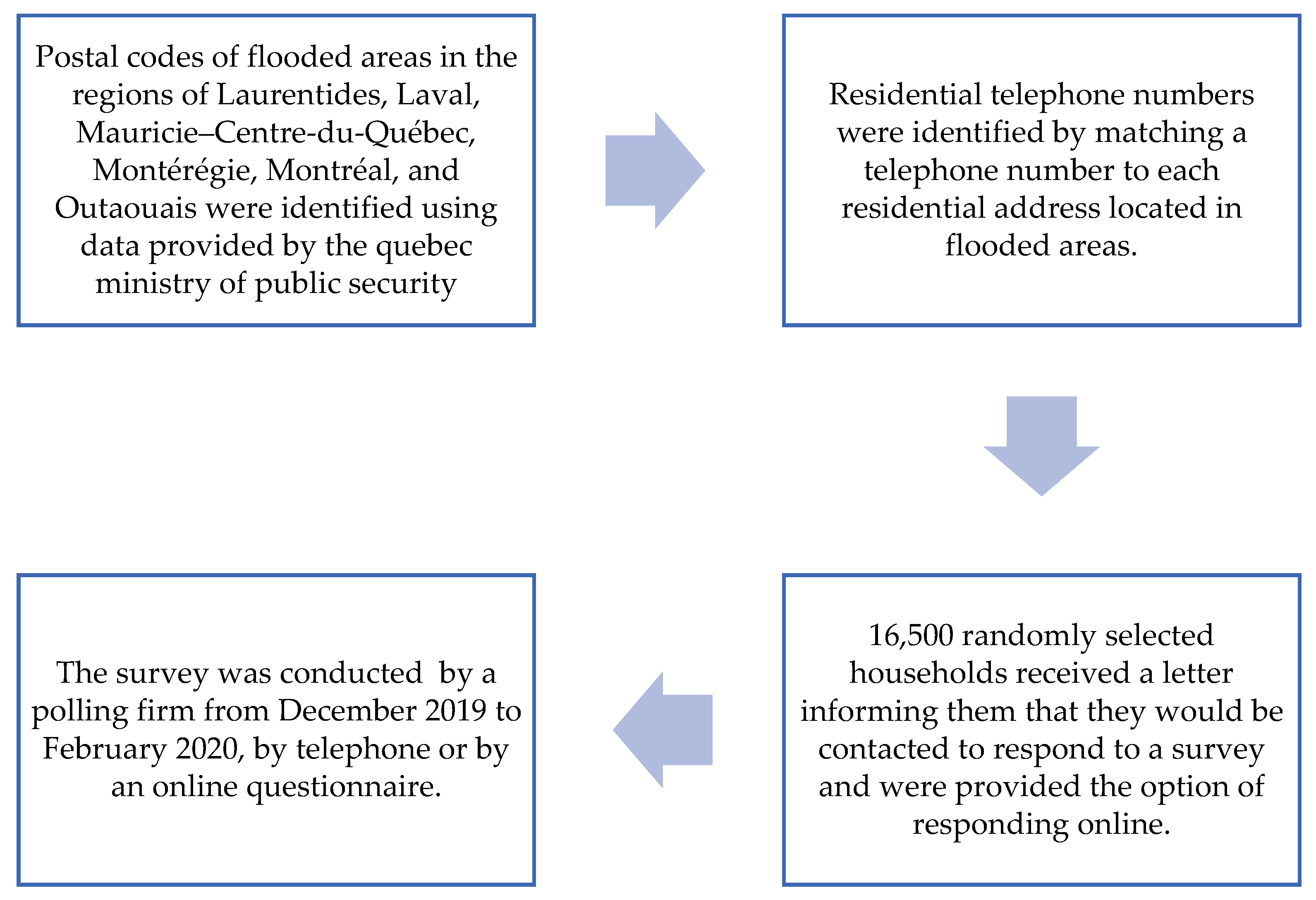
2.2. Recruitment and Participants
2.3. Measurement
2.4. Outcomes
2.5. Exposure to Floods and Stressors
2.6. Analysis
3. Results
3.1. Respondent Characteristics
3.2. Respiratory Health Impacts
3.3. Associated Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Giorgadze, T.; Maisuradze, I.; Japaridze, A.; Utiashvili, Z.; Abesadze, G. Disasters and Their Consequences for Public Health. Georgian Med. News 2011, 194, 59–63. [Google Scholar]
- Kapucu, N. Collaborative Governance and Disaster Recovery: The National Disaster Recovery Framework (NDRF) in the U.S. In Disaster Recovery; Shaw, R., Ed.; Disaster Risk Reduction; Springer: Tokyo, Japan, 2014; pp. 41–59. [Google Scholar] [CrossRef]
- World Health Organization. Climate Change and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health (accessed on 14 July 2022).
- Cerveny, R.S.; Bessemoulin, P.; Burt, C.C.; Cooper, M.A.; Cunjie, Z.; Dewan, A.; Finch, J.; Holle, R.L.; Kalkstein, L.; Kruger, A.; et al. WMO Assessment of Weather and Climate Mortality Extremes: Lightning, Tropical Cyclones, Tornadoes, and Hail. Weather Clim. Soc. 2017, 9, 487–497. [Google Scholar] [CrossRef]
- Mostofi Zadeh, S.; Burn, D.H.; O’Brien, N. Detection of Trends in Flood Magnitude and Frequency in Canada. J. Hydrol. Reg. Stud. 2020, 28, 100673. [Google Scholar] [CrossRef]
- Burn, D.H.; Whitfield, P.H. Changes in Floods and Flood Regimes in Canada. Can. Water Res. J. Rev. Can. Res. Hydrol. 2016, 41, 139–150. [Google Scholar] [CrossRef]
- Buttle, J.M.; Allen, D.M.; Caissie, D.; Davison, B.; Hayashi, M.; Peters, D.L.; Pomeroy, J.W.; Simonovic, S.; St-Hilaire, A.; Whitfield, P.H. Flood Processes in Canada: Regional and Special Aspects. Can. Water Res. J. Rev. Can. Res. Hydrol. 2016, 41, 7–30. [Google Scholar] [CrossRef]
- Bonsal, B.; Shrestha, R.R.; Dibike, Y.; Peters, D.L.; Spence, C.; Mudryk, L.; Yang, D. Western Canadian Freshwater Availability: Current and Future Vulnerabilities. Environ. Rev. 2020, 28, 528–545. [Google Scholar] [CrossRef]
- Lowe, D.; Ebi, K.L.; Forsberg, B. Factors Increasing Vulnerability to Health Effects before, during and after Floods. Int. J. Environ. Res. Public Health 2013, 10, 7015–7067. [Google Scholar] [CrossRef]
- Zhong, S.; Yang, L.; Toloo, S.; Wang, Z.; Tong, S.; Sun, X.; Crompton, D.; FitzGerald, G.; Huang, C. The Long-Term Physical and Psychological Health Impacts of Flooding: A Systematic Mapping. Sci. Total Environ. 2018, 626, 165–194. [Google Scholar] [CrossRef]
- Vanasse, A.; Cohen, A.; Courteau, J.; Bergeron, P.; Dault, R.; Gosselin, P.; Blais, C.; Bélanger, D.; Rochette, L.; Chebana, F. Association between Floods and Acute Cardiovascular Diseases: A Population-Based Cohort Study Using a Geographic Information System Approach. Int. J. Environ. Res. Public Health 2016, 13, 168. [Google Scholar] [CrossRef]
- Sahni, V.; Scott, A.N.; Beliveau, M.; Varughese, M.; Dover, D.C.; Talbot, J. Public Health Surveillance Response Following the Southern Alberta Floods, 2013. Can. J. Public Health 2016, 107, e142–e148. [Google Scholar] [CrossRef]
- Maltais, D.; Gilbert, S.; Généreux, M. Les Conséquences à Court, à Moyen et à Long Terme Des Inondations Sur La Santé Globale Des Adultes Exposées à Des Inondations: Résultats d’une Recension Des Écrits. In Les Inondations au Québec: Connaissances du Risque, Aménagement du Territoire, Impacts Socioéconomiques et Transformation des Vulnérabilités; Presse de l’Université du Québec: Quebec City, QC, Canada, 2022; [Manuscript submitted for publication]. [Google Scholar]
- Saulnier, D.D.; Hanson, C.; Ir, P.; Mölsted Alvesson, H.; Von Schreeb, J. The Effect of Seasonal Floods on Health: Analysis of Six Years of National Health Data and Flood Maps. Int. J. Environ. Res. Public Health 2018, 15, 665. [Google Scholar] [CrossRef] [PubMed]
- Maltais, D. Catastrophes En Milieu Rural; Éditions JCL: Chicoutimi, QC, Canada, 2003. [Google Scholar]
- Fisk, W.J.; Eliseeva, E.A.; Mendell, M.J. Association of Residential Dampness and Mold with Respiratory Tract Infections and Bronchitis: A Meta-Analysis. Environ. Health 2010, 9, 72. [Google Scholar] [CrossRef] [PubMed]
- Cummings, K.J.; Cox-Ganser, J.; Riggs, M.A.; Edwards, N.; Hobbs, G.R.; Kreiss, K. Health Effects of Exposure to Water-Damaged New Orleans Homes Six Months after Hurricanes Katrina and Rita. Am. J. Public Health 2008, 98, 869–875. [Google Scholar] [CrossRef]
- Mulder, A.C.; Pijnacker, R.; de Man, H.; van de Kassteele, J.; van Pelt, W.; Mughini-Gras, L.; Franz, E. “Sickenin’ in the Rain”—Increased Risk of Gastrointestinal and Respiratory Infections after Urban Pluvial Flooding in a Population-Based Cross-Sectional Study in the Netherlands. BMC Infect. Dis. 2019, 19, 377. [Google Scholar] [CrossRef]
- Burton, H.; Rabito, F.; Danielson, L.; Takaro, T.K. Health Effects of Flooding in Canada: A 2015 Review and Description of Gaps in Research. Can. Water Res. J. Rev. Can. Res. Hydrol. 2016, 41, 238–249. [Google Scholar] [CrossRef]
- Gargano, L.M.; Locke, S.; Jordan, H.T.; Brackbill, R.M. Lower Respiratory Symptoms Associated with Environmental and Reconstruction Exposures After Hurricane Sandy. Disaster Med. Public Health Prep. 2018, 12, 697–702. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, A.M.; Collins, T.W.; Grineski, S.E. Intra-Ethnic Disparities in Respiratory Health Problems among Hispanic Residents Impacted by a Flood. J. Asthma 2013, 50, 463–471. [Google Scholar] [CrossRef]
- Quansah, R.; Jaakkola, M.S.; Hugg, T.T.; Heikkinen, S.A.M.; Jaakkola, J.J.K. Residential Dampness and Molds and the Risk of Developing Asthma: A Systematic Review and Meta-Analysis. PLoS ONE 2012, 7, e47526. [Google Scholar] [CrossRef]
- Kanchongkittiphon, W.; Mendell, M.J.; Gaffin, J.M.; Wang, G.; Phipatanakul, W. Indoor Environmental Exposures and Exacerbation of Asthma: An Update to the 2000 Review by the Institute of Medicine. Environ. Health Perspect. 2015, 123, 6–20. [Google Scholar] [CrossRef]
- Jaakkola, M.S.; Quansah, R.; Hugg, T.T.; Heikkinen, S.A.M.; Jaakkola, J.J.K. Association of Indoor Dampness and Molds with Rhinitis Risk: A Systematic Review and Meta-Analysis. J. Allergy Clin. Immunol. 2013, 132, 1099–1110.e18. [Google Scholar] [CrossRef]
- Rando, R.J.; Lefante, J.J.; Freyder, L.M.; Jones, R.N. Respiratory Health Effects Associated with Restoration Work in Post-Hurricane Katrina New Orleans. J. Environ. Public Health 2012, 2012, 462478. [Google Scholar] [CrossRef] [PubMed]
- Lanthier-Veilleux, M.; Baron, G.; Généreux, M. Respiratory Diseases in University Students Associated with Exposure to Residential Dampness or Mold. Int. J. Environ. Res. Public Health 2016, 13, 1154. [Google Scholar] [CrossRef] [PubMed]
- Tempest, E.L.; English National Study on Flooding and Health Study Group; Carter, B.; Beck, C.R.; Rubin, G.J. Secondary Stressors Are Associated with Probable Psychological Morbidity after Flooding: A Cross-Sectional Analysis. Eur. J. Public Health 2017, 27, 1042–1047. [Google Scholar] [CrossRef] [PubMed]
- Généreux, M.; Lansard, A.-L.; Maltais, D.; Gachon, P. Impacts Des Inondations Sur La Santé Mentale Des Québécois: Pourquoi Certains Citoyens Sont-Ils plus Affectés Que d’autres? Mon Clim. Ma St. 2020. Available online: http://www.monclimatmasante.qc.ca/impacts-des-inondations-sur-la-sante-mentale-des-quebecois (accessed on 15 September 2022).
- Lock, S.; Rubin, G.J.; Murray, V.; Rogers, M.B.; Amlôt, R.; Williams, R. Secondary Stressors and Extreme Events and Disasters: A Systematic Review of Primary Research from 2010–2011. PLoS Curr. 2012, 4. [Google Scholar] [CrossRef] [PubMed]
- Stanke, C.; Murray, V.; Amlôt, R.; Nurse, J.; Williams, R. The Effects of Flooding on Mental Health: Outcomes and Recommendations from a Review of the Literature. PLoS Curr. 2012, 4. [Google Scholar] [CrossRef]
- Ministère de l’Environnement. et de la Lutte Contre les Changements Climatiques. Crue printanière 2019: Un Apport en eau Record en 57 ans au Sud-Ouest du Québec. Available online: https://www.environnement.gouv.qc.ca/climat/Faits-saillants/2019/crue-printaniere.htm (accessed on 11 May 2022).
- Marin, S. Étudier l’inondation de Sainte-Marthe-sur-le-Lac pour Prévenir de Futures Catastrophes. Le Devoir. Available online: https://www.ledevoir.com/societe/578116/sainte-marthe-sur-le-lac-des-recommandations-pour-prevenir-les-inondations-catastrophes (accessed on 11 May 2022).
- United Nations Office for Disaster Risk Reduction. Sendai Framework for Disaster Risk Reduction 2015–2030. Available online: https://www.undrr.org/publication/sendai-framework-disaster-risk-reduction-2015-2030 (accessed on 14 July 2022).
- United Nations Office for Disaster Risk Reduction. Global Assessment Report on Disaster Risk Reduction 2022: Our World at Risk; United Nations: New York, NY, USA, 2022.
- Waite, T.D.; Chaintarli, K.; Beck, C.R.; Bone, A.; Amlôt, R.; Kovats, S.; Reacher, M.; Armstrong, B.; Leonardi, G.; Rubin, G.J.; et al. The English National Cohort Study of Flooding and Health: Cross-Sectional Analysis of Mental Health Outcomes at Year One. BMC Public Health 2017, 17, 129. [Google Scholar] [CrossRef]
- FitzGerald, G.; Toloo, G.; Baniahmadi, S.; Crompton, D.; Tong, S. Long-Term Consequences of Flooding: A Case Study of the 2011 Queensland Floods. Aust. J. Emerg. Manag. 2019, 34, 35–40. [Google Scholar] [CrossRef]
- Vardoulakis, S.; Dimitroulopoulou, C.; Thornes, J.; Lai, K.-M.; Taylor, J.; Myers, I.; Heaviside, C.; Mavrogianni, A.; Shrubsole, C.; Chalabi, Z.; et al. Impact of Climate Change on the Domestic Indoor Environment and Associated Health Risks in the UK. Environ. Int. 2015, 85, 299–313. [Google Scholar] [CrossRef]
- Brandt, M.; Brown, C.; Burkhart, J.; Burton, N.; Cox-Ganser, J.; Damon, S.; Falk, H.; Fridkin, S.; Garbe, P.; McGeehin, M.; et al. Mold Prevention Strategies and Possible Health Effects in the Aftermath of Hurricanes and Major Floods. In Morbidity and Mortality Weekly Report: Recommendations and Reports; Centers for Disease Control & Prevention (CDC): Atlanta, GA, USA, 2006; Volume 55, pp. 1–27, CE-1–CE-4. [Google Scholar]
- Metts, T.A. Addressing Environmental Health Implications of Mold Exposure after Major Flooding. AAOHN J. 2008, 56, 115–122. [Google Scholar] [CrossRef]
- Cheng, C.; Zhang, T.; Su, K.; Gao, P.; Shen, S. Assessing the Intensity of the Population Affected by a Complex Natural Disaster Using Social Media Data. ISPRS Int. J. Geo-Inf. 2019, 8, 358. [Google Scholar] [CrossRef] [Green Version]
- Rubin, C.B. Long Term Recovery from Disasters—The Neglected Component of Emergency Management. J. Homel. Secur. Emerg. Manag. 2009, 6, 1–2. [Google Scholar] [CrossRef]
- Comfort, L.K.; Birkland, T.A.; Cigler, B.A.; Nance, E. Retrospectives and Prospectives on Hurricane Katrina: Five Years and Counting. Public Adm. Rev. 2010, 70, 669–678. [Google Scholar] [CrossRef]
| Flooded | Disrupted | Non-Affected | |
|---|---|---|---|
| Regions | n (%) | n (%) | n (%) |
| Laurentides (excluding Sainte-Marthe-sur-le-Lac) | 42 (5.0) | 209 (25.0) | 585 (70.0) |
| Sainte-Marthe-sur-le-Lac | 178 (30.3) | 335 (57.1) | 74 (12.6) |
| Laval | 22 (16.4) | 86 (64.2) | 26 (19.4) |
| Outaouais | 67 (8.4) | 320 (40.3) | 407 (51.3) |
| Mauricie-Centre du Québec | 20 (3.1) | 115 (17.9) | 508 (79.0) |
| Montérégie | 8 (2.5) | 101 (31.0) | 217 (66.6) |
| Montréal | 12 (10.3) | 64 (54.7) | 41 (35.0) |
| All regions affected by floods | 349 (10.2) | 1230 (35.8) | 1858 (54.1) |
| Sainte-Marthe-sur-le-Lac | All Regions (Excluding Sainte-Marthe) | All Regions | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Primary Stressors (Among All Respondents) | |||
| Level of exposure | |||
| Flooded | 178 (30.3) | 171 (6.0) | 349 (10.2) |
| Disrupted | 335 (57.1) | 895 (31.4) | 1230 (35.8) |
| Unaffected | 74 (12.6) | 1784 (62.6) | 1858 (54.1) |
| Water level (at the first floor) | |||
| No water | 404 (69.3) | 2617 (92.0) | 3021 (88.2) |
| Less than 30 cm | 36 (6.2) | 129 (4.5) | 165 (4.8) |
| 30 to 100 cm | 48 (8.2) | 49 (1.7) | 97 (2.8) |
| More than 100 cm | 95 (16.3) | 49 (1.7) | 144 (4.2) |
| Extent of material losses | |||
| No loss | 369 (63.3) | 2437 (86.1) | 2806 (82.2) |
| Less than $25,000 | 52 (8.9) | 304 (10.7) | 356 (10.4) |
| 25,000 to $49,999 | 63 (10.8) | 39 (1.4) | 102 (3.0) |
| $50,000 or more | 99 (17.0) | 51 (1.8) | 150 (4.4) |
| Recurrence of floods | |||
| Never flooded | 355 (60.7) | 2200 (77.6) | 2555 (74.7) |
| Flooded in 2019 only | 200 (34.2) | 157 (5.5) | 357 (10.4) |
| Flooded in 2019 and before 2019 | 30 (5.1) | 479 (16.9) | 14.9 (14.9) |
| Secondary stressors (among flooded or disrupted) | |||
| Perception about concrete or moral help received | |||
| More than expected | 41 (18.8) | 80 (22.1) | 121 (20.9) |
| As much as expected | 121 (55.5) | 152 (42.0) | 273 (47.1) |
| Less than expected | 56 (25.7) | 130 (35.9) | 186 (32.1) |
| Financial sum received to meet costs | |||
| All or most of the costs | 78 (34.5) | 125 (46.8) | 203 (41.2) |
| About half the costs | 78 (34.5) | 71 (26.6) | 149 (30.2) |
| Less than half the costs | 70 (31.0) | 71 (26.6) | 141 (28.6) |
| Insurance covering floods | |||
| Yes | 245 (55.4) | 478 (51.8) | 723 (53.0) |
| No | 197 (44.6) | 444 (48.2) | 641 (47.0) |
| Bank loan to meet expenses | |||
| Yes | 49 (16.9) | 56 (8.5) | 105 (11.1) |
| No | 241 (83.1) | 601 (91.5) | 842 (88.9) |
| Normal reuse of all rooms | |||
| Yes | 426 (83.2) | 993 (93.4) | 1419 (90.1) |
| No | 86 (16.8) | 70 (6.6) | 156 (9.9) |
| Sainte-Marthe-sur-le-Lac | All Regions (Excluding Sainte-Marthe) | All Regions | ||||
|---|---|---|---|---|---|---|
| ENT Symptoms | Respiratory Symptoms | ENT Symptoms | Respiratory Symptoms | ENT Symptoms | Respiratory Symptoms | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Flooded | 61 (34.3) a | 35 (19.7) a | 60 (35.1) a | 34 (19.9) a | 121 (34.7) a | 69 (19.8) a |
| Disrupted | 64 (19.1) b | 20 (6.0) b | 203 (22.7) b | 88 (9.8) b | 267 (21.7) b | 108 (8.8) b |
| Unaffected | 13 (17.6) b | 5 (6.8) b | 259 (14.5) c | 123 (6.9) c | 272 (14.6) c | 128 (6.9) b |
| ENT Symptoms | Respiratory Symptoms | |||||
|---|---|---|---|---|---|---|
| Flooded | Disturbed | Unaffected | Flooded | Disturbed | Unaffected | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Sex | ||||||
| Men | 38 (30.2) a | 85 (18.3) a | 92 (11.9) a | 22 (17.5) a | 42 (9.1) a | 46 (6.0) a |
| Women | 83 (37.2) a | 182 (23.8) b | 180 (16.5) b | 47 (21.1) a | 66 (8.6) a | 82 (7.5) a |
| Age | ||||||
| 18–44 years old | 20 (32.2) a | 43 (15.4) a | 27 (8.8) a | 12 (19.4) a | 12 (4.3) a | 11 (3.6) a |
| 45–64 years old | 62 (32.6) a | 134 (23.2) b | 98 (12.0) a | 36 (18.9) a | 59 (10.2) b | 54 (6.6) a,b |
| More than 65 years old | 39 (40.2) a | 90 (24.1) b | 147 (20.0) b | 21 (21.6) a | 37 (9.9) b | 63 (8.6) b |
| Education | ||||||
| High school or less | 56 (37.1) a | 116 (29.1) a | 134 (16.0) a | 31 (20.5) a | 64 (16.1) a | 77 (9.2) a |
| College | 22 (27.5) a | 64 (19.2) b | 55 (12.6) a | 14 (17.5) a | 19 (5.7) b | 25 (5.7) b |
| University | 39 (35.1) a | 85 (17.8) b | 81 (14.4) a | 23 (20.7) a | 25 (5.2) b | 25 (4.4) b |
| Annual household income | ||||||
| Less than $29,999 | 17 (42.5) a | 47 (31.8) a | 79 (22.3) a | 9 (22.5) a | 27 (18.2) a | 41 (11.5) a |
| 30,000$ to $79,999 | 50 (35.2) a | 108 (25.4) a | 111 (16.1) b | 32 (22.5) a | 41 (9.6) b | 45 (6.5) b |
| More than $80,000 | 33 (29.5) a | 6 (15.5) b | 53 (11.6) c | 21 (18.8) a | 22 (5.0) c | 25 (5.5) b |
| Smoking status | ||||||
| Yes | 29 (39.2) a | 51 (26.2) a | 57 (20.7) a | 21 (28.4) a | 39 (20.0) a | 47 (17.0) a |
| No | 92 (33.6) a | 216 (20.9) a | 214 (13.6) b | 48 (17.5) b | 69 (6.7) b | 81 (5.1) b |
| ENT Symptoms | Crude Odds Ratios | Adjusted Odds Ratios | |||
| Primary Stressors | n(%) | OR | [95% CI] | OR | [95% CI] |
| Level of exposure | |||||
| Flooded | 121 (34.7) | 3.09 | [2.40; 3.99] | 3.18 | [2.45; 4.14] |
| Disturbed | 267 (21.7) | 1.62 | [1.34; 1.95] | 1.76 | [1.45; 2.14] |
| Unaffected | 272 (14.6) | 1 | Reference | 1 | Reference |
| Water Level (at first floor) | |||||
| No water | 520 (17.2) | 1 | Reference | 1 | Reference |
| Less than 30 cm | 49 (29.7) | 2.03 | [1.44; 2.88] | 1.96 | [1.38; 2.79] |
| 30 to 100 cm | 24 (24.7) | 1.58 | [1.00; 2.53] | 1.54 | [0.96; 2.49] |
| More than 100 cm | 62 (43.1) | 3.64 | [2.58; 5.13] | 3.56 | [2.51; 5.04] |
| Extent of material losses | |||||
| No loss | 453 (16.1) | 1 | Reference | 1 | Reference |
| Less than $25,000 | 108 (30.3) | 2.26 | [1.77; 2.90] | 2.15 | [1.67; 2.77] |
| 25,000 to $49,999 | 30 (29.4) | 2.16 | [1.40; 3.35] | 2.06 | [1.32; 3.20] |
| More than $50,000 $ | 62 (41.3) | 3.66 | [2.60; 5.14] | 3.86 | [2.72; 5.47] |
| Recurrence of floods | |||||
| Never flooded | 407 (15.9) | 1 | Reference | 1 | Reference |
| Flooded in 2019 only | 407 (28.3) | 2.08 | [1.62; 2.68] | 2.05 | [1.58; 2.65] |
| Flooded in 2019 and before 2019 | 148 (29.1) | 2.16 | [1.74; 2.69] | 2.08 | [1.67; 2.60] |
| Respiratory Symptoms | Crude Odds Ratio | Adjusted Odds Ratio | |||
| n (%) | OR | [IC 95%] | OR | [IC 95%] | |
| Level of exposure | |||||
| Flooded | 69 (19.8) | 3.33 | [2.42; 4.58] | 3.41 | [2.45; 4.75] |
| Disturbed | 108 (8.8) | 1.30 | [1.00; 1.70] | 1.45 | [1.10; 1.91] |
| Unaffected | 128 (6.9) | 1 | Reference | 1 | Reference |
| Water Level (at first floor) | |||||
| No water | 222 (7.3) | 1 | Reference | 1 | Reference |
| Less than 30 cm | 30 (18.2) | 2.80 | [1.84; 4.26] | 2.58 | [1.68; 3.98] |
| 30 to 100 cm | 15 (15.5) | 2.31 | [1.31; 4.07] | 2.02 | [1.13; 3.62] |
| More than 100 cm | 34 (23.6) | 3.90 | [2.59; 5.86] | 3.48 | [2.28; 5.31] |
| Extent of material losses | |||||
| No loss | 198 (7.1) | 1 | Reference | 1 | Reference |
| Less than $25,000 | 53 (14.9) | 2.30 | [1.66; 3.19] | 2.08 | [1.49; 2.91] |
| 25,000 to $49,999 | 19 (18.6) | 3.02 | [1.79; 5.07] | 2.67 | [1.57; 4.54] |
| More than $50,000 | 30 (20.0) | 3.29 | [2.15; 5.04] | 3.64 | [2.34; 5.66] |
| Recurrence of floods | |||||
| Never flooded | 179 (7.0) | 1 | Reference | 1 | Reference |
| Flooded in 2019 only | 61 (17.1) | 2.74 | [2.00; 3.75] | 2.74 | [1.98; 3.78] |
| Flooded in 2019 and before 2019 | 64 (12.6) | 1.91 | [1.41; 2.58] | 1.79 | [1.31; 2.44] |
| ENT Symptoms | Crude Odds Ratios | Adjusted Odds Ratios | |||
| Secondary Stressors (Among Flooded or Disrupted) | n(%) | RC | [IC 95%] | RC | [IC 95%] |
| Level of satisfaction about concrete or moral help received | |||||
| More than expected | 31 (25.6) | 1 | Reference | 1 | Reference |
| As much as expected | 81 (29.7) | 1.23 | [0.76; 1.99] | 1.23 | [0.75; 2.01] |
| Less than expected | 70 (37.6) | 1.75 | [1.06; 2.90] | 1.87 | [1.11; 3.13] |
| Financial sum received to cover damages | |||||
| All or most of the costs | 50 (24.6) | 1 | Reference | 1 | Reference |
| About half the cost | 46 (30.9) | 1.37 | [0.85; 2.19] | 1.42 | [0.88; 2.30] |
| Less than half the costs | 60 (42.6) | 2.27 | [1.43; 3.60] | 2.44 | [1.51; 3.93] |
| Insurance covering floods | |||||
| Yes | 172 (23.8) | 1 | Reference | 1 | Reference |
| No | 173 (27.0) | 1.18 | [0.93; 1.51] | 1.15 | [0.90; 1.48] |
| Bank loan to meet expenses | |||||
| Yes | 48 (45.7) | 2.34 | [1.55; 3.53] | 2.54 | [1.66; 3.89] |
| No | 223 (26.5) | 1 | Reference | 1 | Reference |
| Normal reuse of all rooms | |||||
| Yes | 316 (22.3) | 1 | Reference | 1 | Reference |
| No | 70 (44.9) | 2.84 | [2.02; 3.99] | 2.77 | [1.96; 3.91] |
| Respiratory symptoms | Crude Odds Ratios | Adjusted Odds Ratios | |||
| Secondary Stressors (among Flooded or Disrupted) | n(%) | OR | [IC 95%] | OR | [IC 95%] |
| Level of satisfaction about Concrete or moral help received | |||||
| More than expected | 15 (12.5) | 1 | Reference | 1 | Reference |
| As much as expected | 38 (13.9) | 1.14 | [0.60; 2.17] | 1.10 | [0.58; 2.01] |
| Less than expected | 35 (18.8) | 1.64 | [0.85; 3.15] | 1.61 | [0.82; 3.13] |
| Financial sum received to cover damages | |||||
| All or most of the costs | 25 (12.3) | 1 | Reference | 1 | Reference |
| About half the costs | 21 (14.1) | 1.17 | [0.63; 2.18] | 1.15 | [0.61; 2.17] |
| Less than half the costs | 33 (23.4) | 2.18 | [1.23; 3.86] | 2.20 | [1.24; 3.98] |
| Insurance covering floods | |||||
| Yes | 67 (9.3) | 1 | Reference | 1 | Reference |
| No | 94 (14.7) | 1.68 | [1.20; 2.35] | 1.56 | [1.12; 2.21] |
| Bank loan to meet expenses | |||||
| Yes | 26 (24.8) | 2.24 | [1.37; 3.64] | 2.48 | [1.50; 4.10] |
| No | 108 (12.8) | 1 | Reference | 1 | Reference |
| Normal reuse of all rooms | |||||
| Yes | 134 (9.4) | 1 | Reference | 1 | Reference |
| No | 41 (26.3) | 3.42 | [2.30; 5.09] | 3.41 | [2.27; 5.13] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Landaverde, E.; Généreux, M.; Maltais, D.; Gachon, P. Respiratory and Otolaryngology Symptoms Following the 2019 Spring Floods in Quebec. Int. J. Environ. Res. Public Health 2022, 19, 11738. https://doi.org/10.3390/ijerph191811738
Landaverde E, Généreux M, Maltais D, Gachon P. Respiratory and Otolaryngology Symptoms Following the 2019 Spring Floods in Quebec. International Journal of Environmental Research and Public Health. 2022; 19(18):11738. https://doi.org/10.3390/ijerph191811738
Chicago/Turabian StyleLandaverde, Elsa, Mélissa Généreux, Danielle Maltais, and Philippe Gachon. 2022. "Respiratory and Otolaryngology Symptoms Following the 2019 Spring Floods in Quebec" International Journal of Environmental Research and Public Health 19, no. 18: 11738. https://doi.org/10.3390/ijerph191811738





