Abstract
The aim of the paper is to present the oral health profile of 12- and 15-year-old schoolchildren in Serbia. Basic Methods for Oral Health Surveys of the WHO were implemented to record: Decayed, Missing, and Filled Teeth/Surfaces Index (DMFT/DMFS), gingival bleeding, enamel fluorosis and other structural anomalies, dental erosion, dental trauma, and oral mucosal lesions. In addition, Silness and Löe plaque index and orthodontic status were assessed. A total of 36% of 12-year-olds and 22% of 15-year-olds in Serbia were caries-free. The mean DMFT was 2.32 ± 2.69 for 12-year-olds and 4.09 ± 3.81 for 15-year-olds. DMFT was made up largely by the decayed component. Gingival bleeding was present in 26% of examined 12-year-old and 18% of 15-year-old children. Dental plaque was observed in 63% of both 12- and 15-year-olds. Fluorosis, structural anomalies, dental erosion, dental trauma, and oral mucosal lesion were rarely detected. Low prevalence of malocclusions was found. Oral disease is still a common public health problem among schoolchildren in Serbia. A significant increase in the prevalence of caries disease between 12- and 15-year-old groups implies that preventive care for adolescents requires special attention. Corrective actions and reforms to the current school-based oral health prevention program are needed to further improve oral health in Serbian children.
1. Introduction
The Republic of Serbia is a European country situated in the West-Central Balkans. According to the latest census from 2011 [1], Serbia (without the Kosovo and Metohija region) has a population of 7,186,862 people. It consists of four administrative regions: (1) the capital—the City of Belgrade (1,659,440 inhabitants), (2) the northern region—Vojvodina (1,931,809 inhabitants), (3) Central and Western Serbia (2,031,697 inhabitants), and (4) Southern and Eastern Serbia (1,563,916 inhabitants).
During previous decades, several national oral health surveys of representative samples were conducted in the Republic of Serbia. During the socialist era in the second half of the 20th century, Serbia had a government-controlled health care system directed to provide equal distribution of health care. All costs, including dental services, were covered by the state [2]. The first national epidemiological study in former SFR Yugoslavia was conducted in 1986 [3]. The study revealed that more than 90% of children in all age groups had caries, and the mean DMFT was 6.1 for 12-year-olds. Subsequently, the first oral health preventive program was established. However, in the 1990s, Serbia was burdened by the financial consequences of the Yugoslav wars and economic sanctions, which had a significant negative impact on implementation and dissemination of the preventive program in the community. Political changes in the beginning of the 21st century brought a restructuring of the health care system. The impact of oral diseases on general health and well-being has not been addressed adequately in Serbian society, even amongst medical professionals. In addition, economic reasons significantly influenced health care policies, and reduced the extent of dental services funded by the public health care system. Nowadays, preventive and restorative oral health care services are funded by the government in public health care institutions for children and adolescents up to 18 years [4].
The latest report on oral health in schoolchildren and adolescents in Serbia was published in 2009 [5]. Since then, new trends in preventive dentistry and cariology have been established, but no science-based modifications and improvements were introduced into the program. A government initiative for updating preventive programs was announced in 2019, intended to develop a modernized program for the prevention of oral diseases in children and adolescents in Serbia. The first step in making a restructured preventive program was to collect epidemiological data in a national oral health survey. The aim of this paper is to present the oral health profile of 12- and 15-year-old schoolchildren in Serbia.
2. Materials and Methods
The present study was part of a national pathfinder survey that aimed to evaluate the oral health status in children and adolescents in Serbia. The survey was designed according to the WHO methodology for oral health surveys [6], approved by the Ethics Committee at the University of Belgrade School of Dental Medicine (document 36/10), and supported by the Ministry of Health of the Republic of Serbia (document 500-01-49-3/2019-07).
According to the WHO [6], in populations where the disease level is known to be high, namely the percentage of caries-free 12-year-olds is less than 20%, the proposed number of subjects in each index age group for each sampling site is approximately 50 subjects. The results of the last epidemiological study in Serbia from 2009 showed that the level of caries-free 12-year-olds was 18% [5]. Therefore, the proposed sample design for oral health survey in Serbia was 50 children of each age group to be examined at the following 14 sampling sites: 4 sites in the capital city (2 urban, 2 periurban), 6 sites in 3 large towns located in 3 administrative regions (1 urban, 1 periurban) and 1 site in 4 rural areas. Such a sample design provides a minimum of 700 participants in each age group.
Prior to the survey, selected schools and health centers were reached for the approval, and written informed institutional consents were obtained. Dental practitioners from 33 pediatric dental services in Serbia were contacted to participate in the national survey, and enter the calibration process. For the purpose of the study, the calibration of examiners was performed at two levels. At the first level, calibration of three principal investigators was completed. Afterwards, experienced pediatric dentists—examiners, completed a two-day training course in oral examination, and calibration of all investigators was performed. Each of three principal investigators supervised and calibrated one group of 11 examiners from one geographical location at one of 33 sampling sites. The results of examiners’ consistency after examinations of permanent teeth are presented in Table 1 and Table 2.

Table 1.
Results of intra-examiner and inter-examiner reproducibility.

Table 2.
Agreement level after examination of permanent teeth (Kappa (Kappa range between examiners)).
Eventually, 24 school dental services were selected to participate in the study, and schoolchildren were evaluated at the following sites: 3 urban and 2 periurban sites in the capital city of Belgrade, 3 urban, 1 periurban, and 2 rural sites in Vojvodina, 3 urban, 1 periurban, and 3 rural sites in Central and Western Serbia, and 3 urban, 1 periurban, and 2 rural sites in Southern and Eastern Serbia.
Informed parent consent was obtained in writing prior to the child’s participation in the study, and informed assent was obtained from the child.
Oral examinations were undertaken in school dental ambulances using a dental mirror and probe between March and July 2019. The WHO Oral Health Assessment Form for Children was translated to Serbian and used in order to record the following: dentition status (Decayed, Missing, and Filed Teeth (DMFT index) and Decayed, Missing, and Filed Teeth Surfaces (DMFS index)), periodontal status (gingival bleeding), presence of enamel fluorosis and other structural anomalies, dental erosion, dental trauma, and oral mucosal lesions [6]. In addition to cavitated caries lesions (ICDAS 3–6 [7]), visual changes in enamel (ICDAS 1–2 [7]) were recorded. Children exhibiting high scores for one or more of the following conditions: DMFT ≥ 5, D ≥ 3, M ≥ 1, and PUFA index [8] ≥ 1, were grouped as those with severe caries [9]. Furthermore, Silness and Löe plaque index (PI) [10] and orthodontic status were assessed.
Depending on data type and distribution, results are presented as count (%), means ± standard deviation, or median. Groups were compared using a non-parametric chi-square, Mann–Whitney U test, or Kruskal–Wallis test. p values lower than 0.05 were considered significant. The data were analyzed using the SPSS 20.0 (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY, USA: IBM Corp.) and R 3.4.2. (R Core Team (2017). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria).
3. Results
The present survey included 1200 12-year-olds and 1220 15-year-olds of both genders.
Thirty-six percent of 12-year-olds and 22% of 15-year-olds in Serbia were caries-free. If only obvious dental decay experience was considered, 47% of 12-year-olds and 28% of 15-year-olds in Serbia were caries-free. Of children diagnosed with caries, 44% of 12-year-olds and 61% of 15-year-olds were diagnosed with severe form.
The mean DMFT was 2.32 ± 2.69 (median 2.00) for 12-year-olds and 4.09 ± 3.81 (median 3.00) for 15-year-olds. For 12-year-olds, mean number of decayed teeth was 1.34 ± 2.12, and mean number of restored teeth was 0.91 ± 1.54. For 15-year-olds, mean number of decayed teeth was 2.08 ± 2.89, and mean number of restored teeth was 1.87±2.49. The mean DMFS was 3.16 ± 4.48 (median 2.00) for 12-year-olds and 5.83 ± 6.42 (median 4.00) for 15-year-olds. The share of surfaces with initial caries was 45% for 12-year-olds and 39% for 15-year-olds.
Dental status according to gender, area, administrative region, and parental employment status is presented in Table 3 for 12-year-olds and Table 4 for 15-year-old Serbian schoolchildren. Twelve-year-old girls had significantly higher DMFT/DMFS scores than boys (p < 0.001, Mann–Whitney test, Table 3). Children who had only one working parent had higher scores than children with both parents working (p < 0.05, Kruskal–Wallis test; Table 3 and Table 4). Children living in urban areas had lower scores compared to suburban and rural sites. Significantly lower DMFT/DMFS values were found in children residing in the capital city of Belgrade (p < 0.001, Kruskal–Wallis test; Table 3 and Table 4).

Table 3.
Prevalence of caries-free and children with severe caries (%), DMFT and DMFS values (mean ± SD (median)) in 12-year-old children in Serbia.

Table 4.
Prevalence of caries-free and children with severe caries (%), DMFT and DMFS values (mean ± SD (median)) in 15-years old children in Serbia.
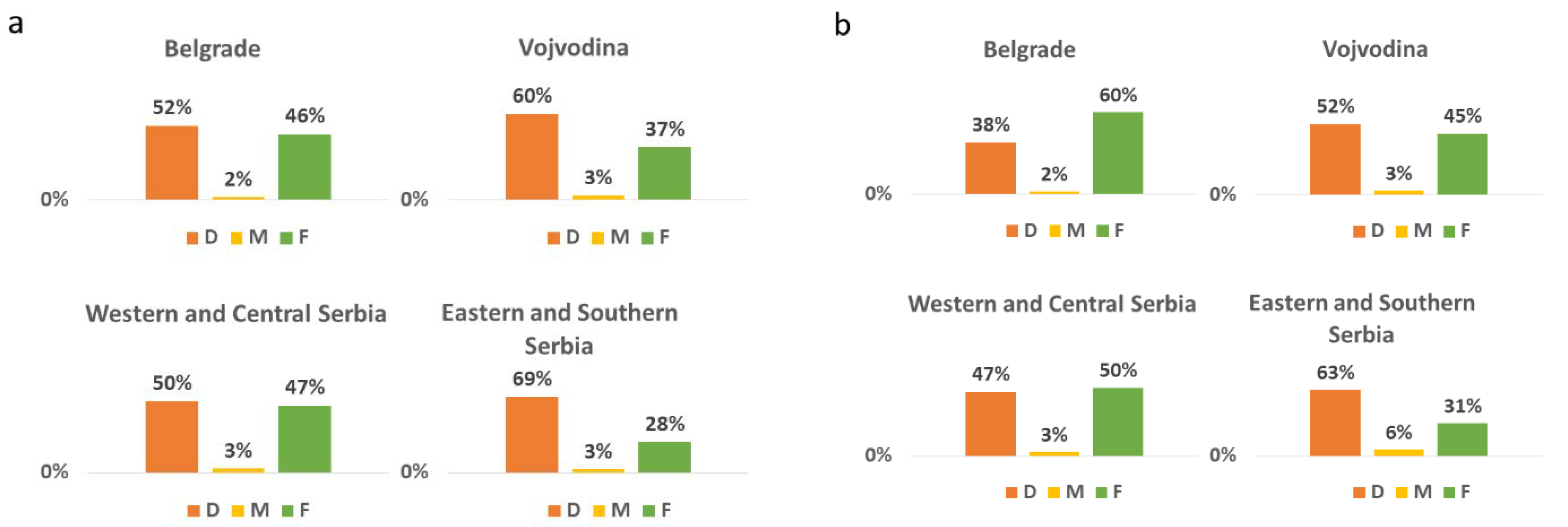
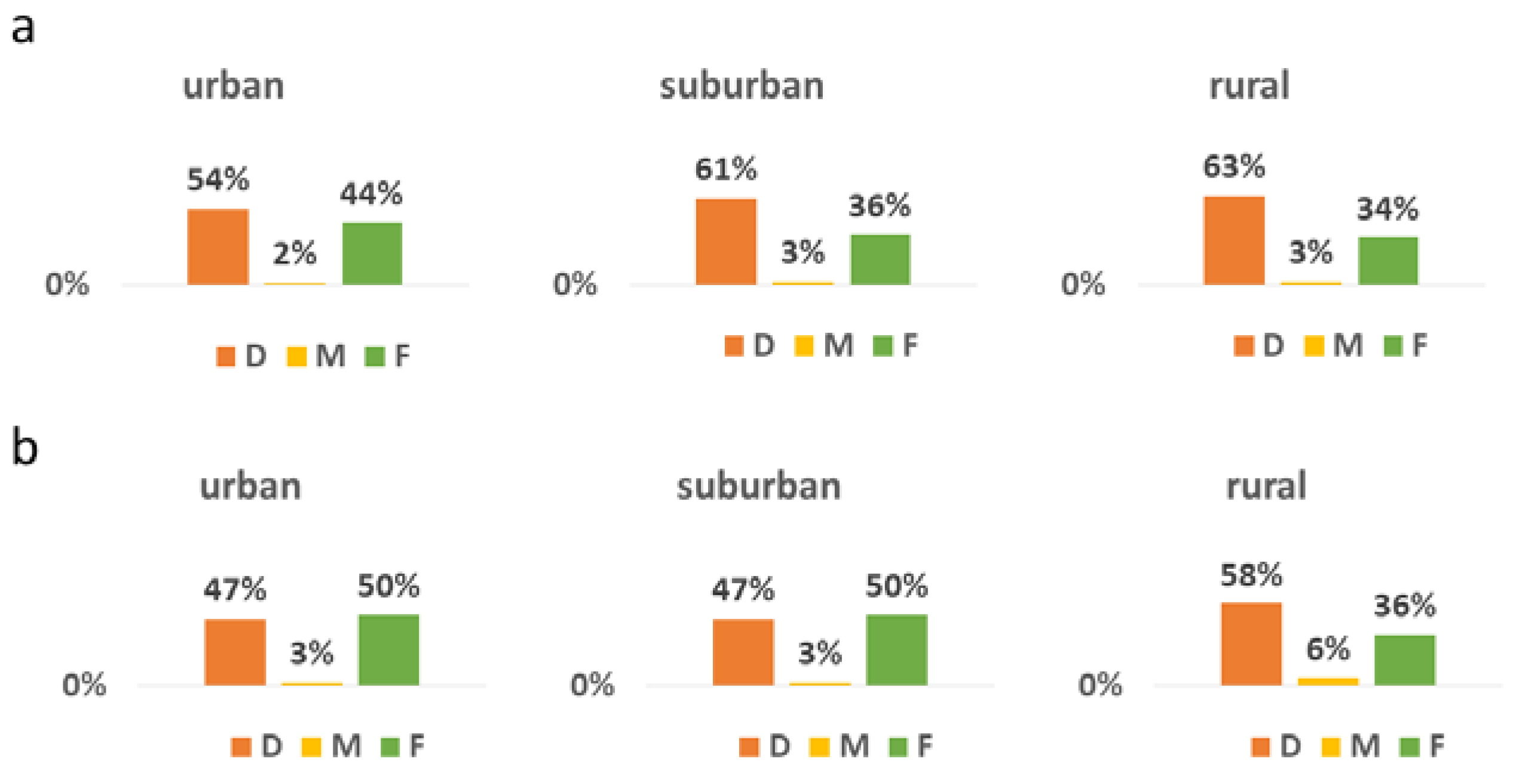
DMFT/DMFS was made up largely by the decayed component (D 58%, M 3%, F 39%; DS 57%, FS 33% for 12-year-olds, and D 51%, M 4%, F 45%; DS 47%, FS 40% for 15-year-olds). There was a significant difference in the distribution of D and F components for both 12- and 15-year-olds between the regions (p < 0.001, Kruskal–Wallis test, Figure 1). In the group of 15-year-olds, children from rural locations had more untreated caries present than children from urban and suburban locations (Figure 2).

Figure 1.
The distribution of DMFT according to the region in (a) 12-year-olds and (b) 15-year-olds in Serbia. Significant differences in the distribution of D and F components were found between the regions (p < 0.001, Kruskal–Wallis test).

Figure 2.
The distribution of DMFT according to the area in (a) 12-year-olds and (b) 15-year-olds in Serbia.
Overall, 15% of 12-year-old children and 16% of 15-year-olds had fissure sealants present. The occurrence of fissure sealing was significantly lower in Eastern and Southern Serbia (p < 0.001, chi-square test). There were no differences in DMFT values between 12-year-old children who had fissure sealants present (2.40 ± 2.78, median 2.00) and those who had not (1.85 ± 2.09, median 1.00) (p > 0.05, Mann–Whitney test). However, DMFT scores were significantly lower in 15-year-olds with sealants (3.15 ± 3.21 (median 2.00)), in comparison to children without sealants (4.27 ± 3.88 (median 4.00)) (p < 0.05, Mann–Whitney test).
Gingival bleeding was present in 26% of examined 12-year-old and 18% of 15-year-old children. Dental plaque was observed in 63% of both 12-year-olds (PI = 0.71 ± 0.78) and 15-year-olds (PI = 0.61 ± 0.72) (Table 5).

Table 5.
Gingival health and oral hygiene.
Fluorosis, structural anomalies, dental erosion, and oral mucosal lesion were rarely detected (<1%), while dental trauma was noted in 2% of children. Orthodontic status is shown in Table 6.

Table 6.
Orthodontic findings.
4. Discussion
This was the first study in Serbia, under the umbrella of the WHO, to provide a better insight into all aspects of oral health, including oral hygiene and orthodontic status in 12- and 15-year-old schoolchildren. The importance of this study in the country that has had many challenges in past decades is enormous. Even in high-income countries with great funding for national research projects, pathfinder surveys are rare [11].
The investigation of oral health trends in young population is a powerful instrument in monitoring efficacy of preventive measures. In comparison to the findings of previous epidemiological studies, there was a noticeable reduction in carious disease in schoolchildren and adolescents in Serbia. According to the latest report on oral health published in 2009 [5], 18% of 12-year-olds and 7.8% of 15-year-olds were caries-free, and the mean DMFT was 3.3 and 5.5, respectively. Findings of the present survey show that 36% of 12-year-olds and 22% of 15-year-olds in Serbia are caries-free (47% of 12-year-olds and 28% of 15-year-olds, if only obvious decay is considered). The number of caries-free children in the last 10 years has doubled, which is a good sign of progress in the prevention of oral diseases in Serbia. The positive trend could be attributed to easier access to dental care, better education, and improved socio-economic status in the country. Significant improvements of oral health awareness, knowledge, and attitudes were also reported in previous studies during the last decades [12].
According to the WHO caries severity criteria [6], Serbian schoolchildren currently belong to the low-risk group (mean DMFT in 12-year-olds: 1.2–2.6), compared to the moderate-risk group (mean DMFT in 12-year-olds: 2.7–4.4) in the past. Conversely, the increase in mean DMFT/DMFS between 12- and 15-year-old groups is a worrying trend. Adolescence is a period of numerous behavioral shifts [13], including change in dietary habits, negligence of oral hygiene, and possible adoption of nicotine, alcohol, and drugs addiction. Although adolescents may be perceived as responsible and capable of taking care of their oral health, it does not seem to be so. It has been shown that sugar consumption was higher during adolescence [14], and motivation for brushing teeth and using proper brushing technique may vary greatly [15]. Thus, prevention and treatment programs for adolescents should be emphasized and designed with special care.
Nowadays, initial changes in enamel are considered a disease requiring therapeutic response. This approach reflects changes in diagnosis and clinical practice towards preventive and minimum intervention approach to caries management [9]. Therefore, in the present study, besides identifying obvious cavitated lesions, non-cavitated caries lesions were also noted. Of all recorded decayed tooth surfaces, 45% in 12-year-olds, and 39% in 15-year-olds were initial caries lesions. These data clearly show that more rigorous preventive measures could further improve the caries status in Serbian children. One of the most effective prophylactic measures is fissure sealing. The present study revealed that the presence of fissure sealants was related to lower DMFT values. This finding is in accordance with the results of previous studies, which identified fissure sealing as a strong predictor for good oral health [16,17,18].
Significant share of severe caries has been noted among children with caries. Perhaps even more worrying is a larger proportion of untreated teeth with decay rather than restored teeth. This finding is in line with the conclusions of Kassebaum et al. [19], who showed that the burden of untreated caries was higher in Eastern and Central Europe compared to Western Europe. The mean DMFT value in Western European countries was lower, probably due to well-organized public oral health services for children, and high socio-economic status of the population, which enable widespread use of fluoridated and other oral hygiene products [20,21]. On the contrary, results of recent epidemiological studies from other parts of the world, such as Eastern European countries, Latin America, Africa, and Asia are not very encouraging, showing no improvement in caries experience [22,23,24,25,26,27,28,29,30,31,32,33,34]. When it comes to the epidemiological studies performed in the Western Balkan Region, i.e., countries constituted after the Yugoslavia breakup, data on oral health are scarce. To the best of our knowledge, the only oral health survey at the national level was conducted in Bosnia and Herzegovina in 2004 [35]. Similar to the findings of the present study, the D component was the major part of the DMFT index in 12-year-old Bosnian children. That was also the finding from the pathfinder survey in the neighboring Romania, especially in children from rural areas [36].
The present survey revealed that the capital city of Serbia, Belgrade had significantly more caries-free children and lower DMFT/DMFS values compared to other regions. The distribution of D and F components was balanced in all regions, except for Eastern and Southern Serbia where the prevalence of untreated and severe caries was significantly higher. In addition, the share of decayed and extracted teeth increased from urban to rural locations. The capital city of Belgrade is the most developed region in the country with the highest proportion of highly educated people [1]. On the contrary, Southern Serbia is less developed region, with low socio-economic status, which might affect oral health, provision of dental care, and implementation of preventive measures. The same may be the reason for differences in the oral health of children residing in urban, suburban, and rural sites. It has been emphasized that oral health knowledge, attitudes, and practices differ between urban and rural populations, as well as between privileged and underprivileged people [37]. Additional problems may be a limited access to dental health care in rural areas, and less opportunity for adequate provision of preventive measures and dental services [13,38,39,40,41]. Another reason for the high prevalence of severe and untreated caries might be the distribution of working dental professionals in the public dental system. According to 2019 annual reports, Serbia has 1,276,654 children aged 0–18 years [42], and the number of pediatric dentists in public health institutions is 322 [43]. That means that each pediatric dentist provides dental care for an average of 3965 children, which is not in accordance with good practice recommendations (one pediatric dentist per maximum 1500 children).
As previously shown [13], children’s oral health was influenced by parental employment status. Higher caries incidence, higher DMFT/DMFS scores, and worse oral hygiene were observed in children with only one working parent compared to children with both working parents. Lower socio-economic status might determine poor oral health [44,45], probably due to the unaffordable oral hygiene products and high-sugar diets. Interestingly, the findings of the present study showed that the level of oral health in children whose parents were both unemployed was similar to children with both working parents.
The present study showed that gingival bleeding was observed in every fourth 12-year-old, and every fifth 15-year-old in Serbia, which was in accordance with the findings of previous studies in Europe [20]. The incidence of gingivitis varies globally [46] due to differences in oral habits and availability of oral hygiene products. In addition, methodological differences between the studies might influence the results. The community periodontal index (CPI) proposed by the WHO [6] has been widely used because it is simple and fast to use, but it has its limitations [47]. The CPI only shows whether gingivitis exists, but does not show the severity of the disease. Findings of the present study showed that oral hygiene in Serbian children was not adequate, as noticeable dental plaque was observed in two-thirds of schoolchildren. Similar findings [44] show the need for consistency in public health work to raise children’s awareness of the importance of maintaining oral hygiene.
Non-carious dental lesions, such as developmental defects and erosive tooth wear, have been the subject of growing interest [48]. Numerous studies investigated the prevalence of abnormalities in tooth size, shape, number, position, and structure in various countries and different ethnic groups. However, those studies showed methodological variations in sampling and choice of diagnostic methods, which led to inconsistent and incomparable results [49]. A recent study [50] reported higher prevalence of anomalies in tooth position and shape compared to the anomalies of the tooth structure. The overall prevalence of structural abnormalities was 0.2%, which corresponds to the findings of the present study.
Low incidences of fluorosis were found in previous [3] and present national surveys in Serbia in comparison to similar studies in Europe [51] and America [48]. Fluoride concentration in soil and water varies among the regions in Serbia. In some areas, the average level of fluoride in wells is more than 10 times higher than the recommended value. The first law on community water fluoridation in Serbia was created in 1971. Water fluoridation was implemented in several towns (Pancevo, Uzice, Krusevac, Cacak), but it was discontinued during the 1990s due to a lack of funding [2]. Nowadays, the majority of inhabitants in Serbia are drinking tap water, which is not fluoridated.
Erosive tooth wear has become a growing public health problem [52]. It has been estimated that the worldwide prevalence of dental erosion in permanent teeth in children and adolescents is 30.4%, and in Europe 33.1% [53]. However, tooth erosion was found in less than 1% of Serbian schoolchildren in the present study. The reason might be that Serbian schoolchildren are less exposed to risk factors (acidic ingredients) than their peers in other countries. However, an explanation that is more possible is that the assessment protocol for diagnosis of tooth erosion used in the present study (WHO criteria) [6] is different from more precise tooth erosion criteria used in previous studies. Erosive tooth wear is a relatively new condition in pediatric dentistry, and it cannot be noticed easily, especially at the very beginning of its development. Uniform criteria for diagnosis of tooth erosion should be determined and used.
Traumatic tooth injuries are common during childhood. It was reported that 25% of all schoolchildren experience dental trauma [54]. Our data showed that the prevalence of dental injuries was 2% in both 12- and 15-year-olds. A higher prevalence (6.3–14%) of dental injuries in the same age groups was recently reported [30,55,56]. However, the finding from the present study should be considered with caution. Due to study design, only visible outcomes of previous tooth injuries (untreated or restored crown fractures) were recorded.
A high prevalence of malocclusions is a global oral health problem [57]. Malocclusions could pose functional, aesthetic, psychological, or social problems. Nationwide oral health surveys have the potential to provide information on dental needs of the population [58]. Quite a large number of studies on the prevalence of malocclusions in different populations were published. However, information on the prevalence of malocclusion in the Serbian population is scarce [5,59].
In the present study, oro-facial functions showed a slight improvement in 15-year-old children in comparison to 12-year-olds. Neutrocclusion was found in the majority of children, which is in accordance with global prevalence of Class I occlusion [60,61]. Findings of the previous epidemiological study in Serbia [5] also indicated high percentage of children with neutrocclusion (60.3% and 58.5% of 12-year-old and 15-year-old children, respectively). Similar results were presented in a national pathfinder survey in Greece [62]. Authors reported an Angle Class I molar relationship in 49.4% and 52.3% of 12-year-old and 15-year-old children, respectively. The difference in prevalence of sagittal malocclusions between neighboring countries may be attributed to ethnic differences and sample composition. Crowding, deep bite, and posterior crossbite were dominant malocclusion traits found in the present study, which is in accordance with the findings in the Greek survey [62]. Crowding was the most frequently reported malocclusion in Serbian children, as well as globally [61]. The prevalence of posterior crossbite in Serbia was slightly higher than in European countries, but within the global range [61]. Greek children showed similar prevalence of posterior crossbite with almost identical percentages in both age groups [62]. The prevalence of deep bite was higher in Serbian children in comparison to their peers in Europe [60]. Anterior crossbite and open bite had the lowest prevalence of all malocclusion traits, which is consistent with worldwide findings [60]. The lower prevalence of malocclusion in the present study, in comparison to the other parts of the world [61,63], could be either due to the composition of the sample or the growing trend of early initiation of orthodontic prevention and treatment in Serbia in recent years. The orthodontic findings from the present study could assist in providing orthodontic status from this part of the world, as well as in determining steps required for further improvement of measures in regards to preventive and treatment approaches.
The strengths of the present study should be highlighted. At the population level, this was the first epidemiological survey in the last fifteen years that evaluated oral health in Serbian children based on WHO methodology. Prevalence and severity of caries lesions were assessed using not only commonly used DMFT/DMFS indices to characterize cavitated caries lesions, but also recognizing initial enamel caries lesions, which increased the validity of the caries profile. The study provided valuable age- and area-specific indicators of oral health, which could give a foundation for future implementation of targeted preventive interventions.
There are a few limitations of the present study. Only healthy children were recruited for the survey, while children with disabilities were not examined. The organization and administration of community oral health services in Serbia differ among regions, thus influencing the available preventive measures and treatment modalities. Despite the limitations, the present study provides valuable oral health profile of Serbian schoolchildren, which can be used for updating and refining current preventive oral health care program.
5. Conclusions
Dental caries is still a common public health problem among schoolchildren in Serbia. The level of caries experience in 12-year-olds is low. However, a significant increase in prevalence of caries disease between 12- and 15-year-old groups was found. Given the specific needs and health-compromising behaviors of adolescents, prevention efforts need to be tailored very diligently. Improvement of oral hygiene habits is a priority to get better dental and gingival health. The existing school-based prevention program for oral health promotion needs additional attention. Corrective actions and reforms to the current oral health prevention program in Serbia are necessary to deliver strategies for addressing the specific challenges in schoolchildren.
Author Contributions
All authors contributed substantially to this work. Conceptualization, T.P. and D.M.; methodology, D.M., T.P., G.C., E.M. and A.V.; formal analysis, I.S., J.V. and J.M.; investigation, T.P., E.M., B.P., A.V., J.V. and J.M.; data curation, T.P., E.M. and B.P.; writing—original draft preparation, T.P., E.M., B.P. and B.K.; writing—review and editing, T.P., D.M., G.C., E.M., B.P., B.K., A.V., I.S., J.V. and J.M.; supervision, D.M. and G.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Ministry of Health of the Republic of Serbia (document 500-01-49-3/2019-07).
Institutional Review Board Statement
The study was approved by the Ethics Committee at the University of Belgrade School of Dental Medicine (document 36/10).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Datasets generated and/or analyzed during the study are available from the first author on reasonable request.
Acknowledgments
The authors would like to express sincere appreciation to the WHO Country Office for Serbia and the WHO Collaborating Center for Epidemiology and Community Dentistry at the University of Milan. We are particularly grateful for the assistance given by: Marija Igić, Tatjana Kanjevac, Zoraida Milojkovic, Tatjana Aleksic, Zorica Andjelic, Vladica Ciric, Jovanka Drazic, Marija Djurkovic, Naida Hamzagic, Maja Jakoviljevic, Marko Jeremic, Milena Jovanovic, Milica Javor, Jelena Jovicic, Sanda Koncar, Sonja Krdzovic, Jasmina Lapcevic, Jasera Ljajic, Katarina Madic, Ivana Maksimovic, Eleonora Marjanovic, Nada Marjanovic Stefanovic, Marijana Matovic, Sanja Mijatovic, Gabrijela Milanović Stefanović, Jelena Nikolic Ivosevic, Samela Pasovic, Dusan Petrovic, Almera Planic, Vanja Radjen, Maida Skrijelj, Milica Stamenkovic, Marko Stevanovic, Maja Tadic, Biljana Takić, and Katarina Untenecker.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Statistical Office of the Republic of Serbia. Municipalities and Regions of the Republic of Serbia, 2020; Statistical Office of the Republic of Serbia: Belgrade, Serbia, 2020. Available online: https://publikacije.stat.gov.rs/G2020/PdfE/G202013047.pdf (accessed on 20 July 2020).
- Carevic, M.; Vulovic, M. National program for prevention of oral diseases on caries distribution in population of Serbia 1996–2001. In Scientific Thought and Clinical Practice—10 Years of Balkan Stomatological Society; Markovic, D., Ed.; Faculty of Dentistry: Belgrade, Serbia, 2005; pp. 119–125. [Google Scholar]
- Vrbic, V.; Vulović, M.; Rajić, Z.; Topić, B.; Tatić, E.; Malić, M.; Milić, D.; Aurer-Kozelj, J.; Neceva, L.; Redzepagić, S. Oral health in SFR Yugoslavia in 1986. Community Dent. Oral. Epidemiol. 1988, 16, 286–288. [Google Scholar] [CrossRef] [PubMed]
- Government of Serbia, Ministry of Health. Policy of Healthcare Rights under Compulsory National Health Insurance Fund, Including Scope and Funding of Provision of Health Care Services for 2020. Službeni Glasnik RS 25/19. Available online: https://www.rfzo.rs/download/pravilnici/obim-sadrzaj/sadrzaj%20i%20obim%20od%2020.06.2020.godine.pdf (accessed on 10 June 2020). (In Serbian).
- Government of Serbia, Ministry of Health. National Program for Prevention of Oral Diseases in Republic of Serbia. Službeni Glasnik RS 22/2009. Available online: http://demo.paragraf.rs/demo/combined/Old/t/t2009_04/t04_0044.htm (accessed on 17 June 2017). (In Serbian).
- World Health Organization. Oral Health Surveys. Basic Methods, 5th ed.; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Pitts, N. “ICDAS”—An international system for caries detection and assessment being developed to facilitate caries epidemiology, research and appropriate clinical management. Community Dent. Health 2004, 21, 193–198. [Google Scholar] [PubMed]
- Monse, B.; Heinrich-Weltzien, R.; Benzian, H.; Holmgren, C.; van Palenstein Helderman, W. PUFA—An index of clinical consequences of untreated dental caries. Community Dent. Oral. Epidemiol. 2010, 38, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Vernazza, C.R.; Rolland, S.L.; Chadwick, B.; Pitts, N. Caries experience, the caries burden and associated factors in children in England, Wales and Northern Ireland 2013. Br. Dent. J. 2016, 221, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Silness, J.; Loe, H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol. Scand. 1964, 22, 121–135. [Google Scholar] [CrossRef] [PubMed]
- Lavigne, S.E.; Allison, P.J. A Canadian national oral health survey—Coming soon! Can. J. Dent. Hyg. 2022, 56, 3–6. [Google Scholar]
- Zhu, L.; Petersen, P.E.; Wang, H.Y.; Bian, J.Y.; Zhang, B.X. Oral health knowledge, attitudes and behaviour of children and adolescents in China. Int. Dent. J. 2003, 53, 289–298. [Google Scholar] [CrossRef]
- Bombert, F.; Manso, A.C.; Sousa Ferreira, C.; Nogueira, P.; Nunes, C. Sociodemographic factors associated with oral health in 12-year-old adolescents: Hygiene behaviours and health appointments. A cross-sectional national study in Portugal. Int. Dent. J. 2018, 68, 327–335. [Google Scholar] [CrossRef]
- Hall-Scullin, E.; Goldthorpe, J.; Milsom, K.; Tickle, M. A qualitative study of the views of adolescents on their caries risk and prevention behaviours. BMC Oral Health 2015, 15, 141. [Google Scholar] [CrossRef]
- Rouxel, P.; Chandola, T. Socioeconomic and ethnic inequalities in oral health among children and adolescents living in England, Wales and Northern Ireland. Community Dent. Oral Epidemiol. 2018, 46, 426–434. [Google Scholar] [CrossRef]
- Oulis, C.J.; Berdouses, E.D.; Mamai-Homata, E.; Polychronopoulou, A. Prevalence of sealants in relation to dental caries on the permanent molars of 12 and 15-year-old Greek adolescents. A national pathfinder survey. BMC Public Health 2011, 11, 100. [Google Scholar] [CrossRef] [PubMed]
- Jablonski-Momeni, A.; Winter, J.; Petrakakis, P.; Schmidt-Schäfer, S. Caries prevalence (ICDAS) in 12-year-olds from low caries prevalence areas and association with independent variables. Int. J. Paediatr. Dent. 2014, 24, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Berna, K.; Ece, E.; Nese, G. Clinical success of fluoride-releasing fissure sealant in permanent first molars: 5-year retrospective atudy. Balk. J. Dent. Med. 2022. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.; Marcenes, W. Global burden of untreated caries: A systematic review and metaregression. J. Dent. Res. 2015, 94, 650–658. [Google Scholar] [CrossRef] [PubMed]
- Campus, G.; Solinas, G.; Cagetti, M.G.; Senna, A.; Minelli, L.; Majori, S.; Montagna, M.T.; Reali, D.; Castiglia, P.; Strohmenger, L. National Pathfinder survey of 12-year-old Children’s Oral Health in Italy. Caries Res. 2007, 41, 512–517. [Google Scholar] [CrossRef] [PubMed]
- Jordan, R.A.; Bodechtel, C.; Hertrampf, K.; Hoffmann, T.; Kocher, T.; Nitschke, I.; Schiffner, U.; Stark, H.; Zimmer, S.; Micheelis, W.; et al. The Fifth German Oral Health Study (Fünfte Deutsche Mundgesundheitsstudie, DMS V)—Rationale, design, and methods. BMC Oral Health 2014, 14, 161. [Google Scholar] [CrossRef] [PubMed]
- El-Nadeef, M.A.; Al Hussani, E.; Hassab, H.; Arab, I.A. National survey of the oral health of 12- and 15-year-old schoolchildren in the United Arab Emirates. East Mediterr. Health J. 2009, 15, 993–1004. [Google Scholar] [CrossRef]
- Besseling, S.; Ngonephady, S.; van Wijk, A.J. Pilot survey on dental health in 5–12-year-old school children in Laos. J. Investig. Clin. Dent. 2013, 4, 44–48. [Google Scholar] [CrossRef]
- Mafuvadze, B.T.; Mahachi, L.; Mafuvadze, B. Dental caries and oral health practice among 12 year old school children from low socio-economic status background in Zimbabwe. Pan. Afr. Med. J. 2013, 14, 164. [Google Scholar] [CrossRef]
- Monse, B.; Benzian, H.; Araojo, J.; Holmgren, C.; van Palenstein Helderman, W.; Naliponguit, E.C.; Heinrich-Weltzien, R. A silent public health crisis: Untreated caries and dental infections among 6- and 12-year-old children in the Philippine National Oral Health Survey 2006. Asia Pac. J. Public Health 2015, 27, NP2316–NP2325. [Google Scholar] [CrossRef]
- Zhang, S.; Xu, B.; Liu, J.; Lo, E.C.; Chu, C.H. Dental and periodontal status of 12-year-old Dai school children in Yunnan Province, China: A cross-sectional study. BMC Oral Health 2015, 15, 117. [Google Scholar] [CrossRef] [PubMed]
- Elias-Boneta, A.R.; Toro, M.J.; Rivas-Tumanyan, S.; Murillo, M.; Orraca, L.; Encarnacion, A.; Cernigliaro, D.; Toro-Vizcarrondo, C.; Psoter, W.J. Persistent oral health disparity in 12-year-old Hispanics: A cross-sectional study. BMC Oral Health 2016, 16, 10. [Google Scholar] [CrossRef]
- Rybarczyk-Townsend, E.; Hilt, A.; Szczepanska, J. Dentition status in 12-year-old children in Lodzkie province in 2014. Przegl. Epidemiol. 2016, 70, 47–51. [Google Scholar] [PubMed]
- Yin, W.; Yang, Y.M.; Chen, H.; Li, X.; Wang, Z.; Cheng, L.; Yin, Q.D.; Fang, H.Z.; Fei, W.; Mi, F.L.; et al. Oral health status in Sichuan Province: Findings from the oral health survey of Sichuan, 2015–2016. Int. J. Oral Sci. 2017, 9, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Bilder, L.; Stepco, E.; Uncuta, D.; Aizenbud, D.; Machtei, E.; Bilder, A.; Sgan-Cohen, H.D. The pathfinder study among schoolchildren in the Republic of Moldova: Dental caries experience. Int. Dent. J. 2018, 68, 344–347. [Google Scholar] [CrossRef]
- Karki, S.; Laitala, M.L.; Humagain, M.; Seppänen, M.; Päkkila, J.; Anttonen, V. Oral health status associated with sociodemographic factors of Nepalese schoolchildren: A population-based study. Int. Dent. J. 2018, 68, 348–358. [Google Scholar] [CrossRef]
- Ballouk, M.A.; Dashash, M. Caries prevalence and dental health of 8-12 year-old children in Damascus city in Syria during the Syrian Crisis; a cross-sectional epidemiological oral health survey. BMC Oral Health 2019, 19, 16. [Google Scholar] [CrossRef]
- Du, A.; Zhang, H.; Chen, C.; Zhang, F.; Liu, X.; Zhang, Z.; Wang, R. Oral health of 12-year-old children in Jilin province, China: A population-based epidemiological survey. Medicine 2019, 98, e18463. [Google Scholar] [CrossRef]
- Ghotane, S.G.; Challacombe, S.J.; Don-Davis, P.; Kamara, D.; Gallagher, J.E. Unmet need in Sierra Leone: A national oral health survey of schoolchildren. BDJ Open 2022, 8, 16. [Google Scholar] [CrossRef]
- Markovic, N.; Muratbegovic, A.; Kobaslija, S.; Bajric, A.; Huseinbegovic, A.; Selimovic-Dragas, M. Caries prevalence in Bosnia and Herzegovina schoolchildren—Findings of first national survey. Stomatol. Vjesn. 2013, 2, 9–15. [Google Scholar]
- Ondine Lucaciu, P.; Mester, A.; Constantin, I.; Orban, N.; Cosma, L.; Candrea, S.; Sava-Rosianu, R.; Mesaros, A.S. A WHO pathfinder survey of dental caries in 6 and 12-year old Transylvanian children and the possible correlation with their family background, oral-health behavior, and the intake of sweets. Int. J. Environ. Res. Public Health 2020, 17, 4180. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E. Inequality in oral health: The social context for oral health. In Community Oral Health; Harris, R., Pine, C., Eds.; Quintessence Publ.: Copenhagen, Danemark, 2005. [Google Scholar]
- Ha, D.H.; Crocombe, L.A.; Mejia, G.C. Clinical oral health of Australia’s rural children in a sample attending school dental services. Aust. J. Rural Health 2014, 22, 316–322. [Google Scholar] [CrossRef] [PubMed]
- Shen, A.; Zeng, X.; Cheng, M.; Tai, B.; Huang, R.; Bernabé, E. Inequalities in dental caries among 12-year-old Chinese children. J. Public Health Dent. 2015, 75, 210–217. [Google Scholar] [CrossRef]
- Quan, J.K.; Wang, X.Z.; Sun, X.Y.; Yuan, C.; Liu, X.N.; Wang, X.; Feng, X.P.; Tai, B.J.; Hu, Y.; Lin, H.C.; et al. Permanent Teeth Caries Status of 12- to 15-year-olds in China: Findings from the 4th National Oral Health Survey. Chin. J. Dent. Res. 2018, 21, 181–193. [Google Scholar] [CrossRef] [PubMed]
- Bonev, B.; Avramova, N.; Yaneva, K.; Filchev, D. Dental caries and associated socio-demographic factors in adult people in Bulgaria. Balk. J. Dent. Med. 2015, 19, 33–37. [Google Scholar] [CrossRef]
- Statistical Office of the Republic of Serbia. Estimates of Population by Age and Sex; Statistical Office of the Republic of Serbia: Belgrade, Serbia, 2019. Available online: https://data.stat.gov.rs/Home/Result/18010403?languageCode=en-US (accessed on 20 July 2020).
- Institute of Public Health of Serbia “Dr. Milan Jovanovic Batut”. Health Statistical Yearbook of Republic of Serbia 2019; Institute of Public Health of Serbia “Dr. Milan Jovanovic Batut”: Belgrade, Serbia, 2020; Available online: http://www.batut.org.rs/download/publikacije/pub2019a.pdf (accessed on 7 December 2020).
- Vadiakas, G.; Oulis, C.J.; Tsinidou, K.; Mamai-Homata, E.; Polychronopoulou, A. Oral hygiene and periodontal status of 12 and 15-year-old Greek adolescents. A national pathfinder survey. Eur. Arch. Paediatr. Dent. 2012, 13, 11–20. [Google Scholar] [CrossRef]
- Zumpe, L.; Bensel, T.; Wienke, A.; Mtaya-Mlangwa, M.; Hey, J. The Oral Health Situation of 12-Year-Old School Children in the Rural Region of Ilembula in Southwestern Tanzania: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 12237. [Google Scholar] [CrossRef] [PubMed]
- Elias-Boneta, A.R.; Ramirez, K.; Rivas-Tumanyan, S.; Murillo, M.; Toro, M.J. Prevalence of gingivitis and calculus in 12-year-old Puerto Ricans: A cross-sectional study. BMC Oral Health 2018, 18, 13. [Google Scholar] [CrossRef]
- Leroy, R.; Eaton, K.A.; Savage, A. Methodological issues in epidemiological studies of periodontitis—How can it be improved? BMC Oral Health 2010, 10, 8. [Google Scholar] [CrossRef]
- Martignon, S.; Bartlett, D.; Manton, D.J.; Martinez-Mier, E.A.; Splieth, C.; Avila, V. Epidemiology of Erosive Tooth Wear, Dental Fluorosis and Molar Incisor Hypomineralization in the American Continent. Caries Res. 2021, 55, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Shokri, A.; Poorolajal, J.; Khajeh, S.; Faramarzi, F.; Kahnamoui, H.M. Prevalence of dental anomalies among 7- to 35-year-old people in Hamadan, Iran in 2012–2013 as observed using panoramic radiographs. Imaging Sci. Dent. 2014, 44, 7–13. [Google Scholar] [CrossRef]
- Bilge, N.H.; Yeşiltepe, S.; Törenek Ağırman, K.; Çağlayan, F.; Bilge, O.M. Investigation of prevalence of dental anomalies by using digital panoramic radiographs. Folia Morphol. 2018, 77, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Whelton, H.P.; Ketley, C.E.; McSweeney, F.; O’Mullane, D.M. A review of fluorosis in the European Union: Prevalence, risk factors and aesthetic issues. Community Dent. Oral Epidemiol. 2004, 32 (Suppl. 1), 9–18. [Google Scholar] [CrossRef] [PubMed]
- Bilder, L.; Margvelashvili, V.; Sgan-Cohen, H.; Kalandadze, M.; Levin, L.; Ivanishvili, R.; Machtei, E.E. Traumatic dental injuries among 12- and 15-year-old adolescents in Georgia: Results of the pathfinder study. Dent. Traumatol. 2016, 32, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Eltair, M.; Pitchika, V.; Standl, M.; Lang, T.; Krämer, N.; Hickel, R.; Kühnisch, J. Prevalence of traumatic crown injuries in German adolescents. Clin. Oral Investig. 2020, 24, 867–874. [Google Scholar] [CrossRef] [PubMed]
- Schlueter, N.; Luka, B. Erosive tooth wear—A review on global prevalence and on its prevalence in risk groups. Br. Dent. J. 2018, 224, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Salas, M.M.; Nascimento, G.G.; Huysmans, M.C.; Demarco, F.F. Estimated prevalence of erosive tooth wear in permanent teeth of children and adolescents: An epidemiological systematic review and meta-regression analysis. J. Dent. 2015, 43, 42–50. [Google Scholar] [CrossRef]
- Levin, L.; Day, P.F.; Hicks, L.; O’Connell, A.; Fouad, A.F.; Bourguignon, C.; Abbott, P.V. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: General introduction. Dent. Traumatol. 2020, 36, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Enzo, B. Malocclusion in orthodontics and oral health: Adopted by the General Assembly: September 2019, San Francisco, United States of America. Int. Dent. J. 2020, 70, 11–12. [Google Scholar] [CrossRef] [PubMed]
- Adanero, A.; Baquero, L.; Berasategui, M.; Velayos, L.; Espí, M.; Piñeiro, M.; Miegimolle, M. Oral health status of 6- to 12-year-old children in Madrid, Spain: A cross-sectional study. Heliyon 2022, 8, e09557. [Google Scholar] [CrossRef] [PubMed]
- Markovic, E.; Vukovic, A.; Peric, T.; Kuzmanovic-Pficer, J.; Petrovic, B. Prevalence of developmental dental anomalies in Serbian orthodontic patients. Srp. Arh. Celok. Lek. 2020, 148, 17–23. [Google Scholar] [CrossRef]
- Alhammadi, M.S.; Halboub, E.; Fayed, M.S.; Labib, A.; El-Saaidi, C. Global distribution of malocclusion traits: A systematic review. Dental. Press. J. Orthod. 2018, 23, 40.e1–40.e10. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, G.; Vena, F.; Negri, P.; Pagano, S.; Barilotti, C.; Paglia, L.; Colombo, S.; Orso, M.; Cianetti, S. Worldwide prevalence of malocclusion in the different stages of dentition: A systematic review and meta-analysis. Eur. J. Paediatr. Dent. 2020, 21, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Mylonopoulou, I.-M.; Sifakakis, I.; Berdouses, E.; Kavvadia, K.; Arapostathis, K.; Oulis, C.J. Orthodontic Status and Orthodontic Treatment Need of 12- and 15-Year-Old Greek Adolescents: A National Pathfinder Survey. Int. J. Environ. Res. Public Health 2021, 18, 11790. [Google Scholar] [CrossRef] [PubMed]
- De Ridder, L.; Aleksieva, A.; Willems, G.; Declerck, D.; Cadenas de Llano-Pérula, M. Prevalence of Orthodontic Malocclusions in Healthy Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 7446. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).