“All Hands on Deck”: Psychological Characteristics of Women with Experience of Oncological Disease Participating in Sailing Cruise—A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Methods
2.3. Study Organization
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 13 May 2022).
- Lin, L.; Li, Z.; Yan, L.; Liu, Y.; Yang, H.; Li, H. Global, regional, and national cancer incidence and death for 29 cancer groups in 2019 and trends analysis of the global cancer burden, 1990–2019. J. Hematol. Oncol. 2021, 14, 197. [Google Scholar] [CrossRef]
- Religioni, U. Cancer incidence and mortality in Poland. Clin. Epidemiol. Glob. Health 2020, 8, 329–334. [Google Scholar] [CrossRef]
- Fahad Ullah, M. Breast cancer: Current perspectives on the disease status. In Breast Cancer Metastasis and Drug Resistance; Springer: Cham, Switzerland, 2019; pp. 51–64. [Google Scholar]
- Odle, T.G. Adverse effects of breast cancer treatment. Radiol Technol. 2014, 85, 297M–319M. [Google Scholar] [PubMed]
- Fortin, J.; Leblanc, M.; Elgbeili, G.; Cordova, M.J.; Marin, M.F.; Brunet, A. The mental health impacts of receiving a breast cancer diagnosis: A meta-analysis. Br. J. Cancer 2021, 125, 1582–1592. [Google Scholar] [CrossRef] [PubMed]
- Jankowska-Polańska, B.; Świątoniowska-Lonc, N.; Ośmiałowska, E.; Gałka, A.; Chabowski, M. The association between illness acceptance and quality of life in women with breast cancer. Cancer Manag. Res. 2020, 12, 8451. [Google Scholar] [CrossRef] [PubMed]
- Ośmiałowska, E.; Staś, J.; Chabowski, M.; Jankowska-Polańska, B. Illness Perception and Quality of Life in Patients with Breast Cancer. Cancers 2022, 14, 1214. [Google Scholar] [CrossRef]
- Perez-Tejada, J.; Garmendia, L.; Labaka, A.; Vegas, O.; Gómez-Lazaro, E.; Arregi, A. Active and Passive Coping Strategies: Comparing Psychological Distress, Cortisol, and Proinflammatory Cytokine Levels in Breast Cancer Survivors. Clin. J. Oncol. Nurs. 2019, 23, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Sharon-David, H.; Tenenbaum, G. The effectiveness of exercise interventions on coping with stress: Research synthesis. Stud. Sport Humanit. 2017, 22, 19–29. [Google Scholar] [CrossRef]
- Kvam, S.; Kleppe, C.L.; Nordhus, I.H.; Hovland, A. Exercise as a treatment for depression: A meta-analysis. J. Affect. Disord. 2016, 202, 67–86. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, S.; Tiedemann, A.; Sherrington, C.; Curtis, J.; Ward, P.B. Physical activity interventions for people with mental illness: A systematic review and meta-analysis. J. Sci. Med. Sport 2014, 18, e150. [Google Scholar] [CrossRef]
- Wang, D.; Wang, Y.; Wang, Y.; Li, R.; Zhou, C. Impact of physical exercise on substance use disorders: A meta-analysis. PLoS ONE 2014, 9, e110728. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.; Durstine, J.L. Physical activity, exercise, and chronic diseases: A brief review. Sport. Med. Health Sci. 2019, 1, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Henriksson, M.; Wall, A.; Nyberg, J.; Adiels, M.; Lundin, K.; Bergh, Y.; Eggertsen, R.; Danielsson, L.; Kuhn, H.G.; Westerlund, M.; et al. Effects of exercise on symptoms of anxiety in primary care patients: A randomized controlled trial. J. Affect. Disord. 2022, 297, 26–34. [Google Scholar] [CrossRef]
- de Lazzari, N.; Niels, T.; Tewes, M.; Götte, M. A systematic review of the safety, feasibility and benefits of exercise for patients with advanced cancer. Cancers 2021, 13, 4478. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Woo, S.; Larson, J.L. Effects of perioperative exercise interventions on lung cancer patients: An overview of systematic reviews. J. Clin. Nurs. 2020, 29, 4482–4504. [Google Scholar] [CrossRef]
- Klein, P.J.; Schneider, R.; Rhoads, C.J. Qigong in cancer care: A systematic review and construct analysis of effective Qigong therapy. Support. Care Cancer 2016, 24, 3209–3222. [Google Scholar] [CrossRef]
- Zeng, Y.; Xie, X.; Cheng, A.S.K. Qigong or Tai Chi in cancer care: An updated systematic review and meta-analysis. Curr. Oncol. Rep. 2019, 21, 48. [Google Scholar] [CrossRef]
- Denieffe, S.; Castineira, C.; Denny, M. The impact of dragon boating for fatigue in cancer survivors. J. Nurse Pract. 2021, 17, 1019–1022. [Google Scholar] [CrossRef]
- McDonough, M.H.; Patterson, M.C.; Weisenbach, B.B.; Ullrich-French, S.; Sabiston, C.M. The difference is more than floating: Factors affecting breast cancer survivors’ decisions to join and maintain participation in dragon boat teams and support groups. Disabil. Rehabil. 2019, 41, 1788–1796. [Google Scholar] [CrossRef]
- Mirandola, D.; Franchi, G.; Maruelli, A.; Vinci, M.; Muraca, M.G.; Miccinesi, G.; Manetti, M.; Marini, M. Tailored sailing experience to reduce psychological distress and improve the quality of life of breast cancer survivors: A survey-based pilot study. Int. J. Environ. Res. Public Health 2020, 17, 4406. [Google Scholar] [CrossRef]
- STS Fryderyk Chopin. Available online: https://www.fryderykchopin.pl (accessed on 15 May 2022).
- Onkorejs.pl. Available online: http://onkorejs.pl (accessed on 10 May 2022).
- Carta, M.G.; Maggiani, F.; Pilutzu, L.; Moro, M.F.; Mura, G.; Sancassiani, F.; Vellante, V.; Migliaccio, G.M.; Machado, S.; Nardi, A.E.; et al. Sailing can improve quality of life of people with severe mental disorders: Results of a cross over randomized controlled trial. Clin. Pract. Epidemiol. Ment. Health 2014, 10, 80. [Google Scholar] [CrossRef]
- Carta, M.G.; Maggiani, F.; Pilutzu, L.; Moro, M.F.; Mura, G.; Cadoni, F.; Sancassiani, F.; Vellante, M.; Machado, S.; Preti, A. Sailing for rehabilitation of patients with severe mental disorders: Results of a cross over randomized controlled trial. Clin. Pract. Epidemiol. Ment. Health 2014, 10, 73–79. [Google Scholar] [CrossRef]
- Blaschke, S. The role of nature in cancer patients’ lives: A systematic review and qualitative meta-synthesis. BMC Cancer 2017, 17, 370. [Google Scholar] [CrossRef] [PubMed]
- McVeigh, J.; MacLachlan, M.; Stilz, R.; Cox, H.; Doyle, N.; Fraser, A.; Dyer, M. Positive psychology and well-being at sea. In Maritime Psychology; MacLachan, M., Ed.; Springer: Cham, Switzerland, 2017; pp. 19–47. [Google Scholar]
- McCrae, R.R.; Costa, P.T. Validation of the five-factor model of personality across instruments and observers. J. Pers. Soc. Psychol. 1987, 52, 81. [Google Scholar] [CrossRef] [PubMed]
- Lai, H.L.; Chen, C.I.; Lu, C.Y.; Yao, Y.C.; Huang, C.Y. Relationships among personality, coping, and concurrent health-related quality of life in women with breast cancer. Breast Cancer 2019, 26, 544–551. [Google Scholar] [CrossRef]
- Zimbardo, P.G.; Boyd, J.N. Putting Time in Perspective: A Valid, Reliable Individual-Differences Metric. J. Personal. Soc. Psychol. 1999, 17, 1271–1288. [Google Scholar] [CrossRef]
- Nozari, M.; Janbabai, G.; Dousti, Y. Time perspective in healthy individuals and patients suffering from cancer and diabetes. In Annales Universitatis Paedagogicae Cracoviensis Studia Psychologica VI; Uniwersytet Pedagogiczny w Krakowie: Kraków, Poland, 2013; Volume 152, pp. 157–165. [Google Scholar]
- Mirzania, A.; Firoozi, M.; Saberi, A. The Efficacy of Time Perspective Therapy in Reducing Symptoms of Post-traumatic Stress, Anxiety, and Depression in Females with Breast Cancer. Int. J. Cancer Manag. 2021, 14, e112915. [Google Scholar] [CrossRef]
- Wallston, K.A.; Strudler Wallston, B.; DeVellis, R. Development of the multidimensional health locus of control (MHLC) scales. Health Educ. Monogr. 1978, 6, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Gruszczyńska, M.; Bąk-Sosnowska, M.; Szemik, S. Selected psychological aspects and medication adherence in oncological patients. Cancer Med. 2020, 9, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Marchand, W.R.; Klinger, W.; Block, K.; VerMerris, S.; Herrmann, T.S.; Johnson, C.; Shubin, E.; Sheppard, S. Safety and psychological impact of sailing adventure therapy among Veterans with substance use disorders. Complement. Ther. Med. 2018, 40, 42–47. [Google Scholar] [CrossRef]
- Jeżewska, M.; Leszczyńska, I.; Grubman-Nowak, M. Personality and temperamental features vs. quality of life of Polish seafarers. Int. Marit. Health 2013, 64, 101–105. [Google Scholar] [PubMed]
- Zawadzki, B.; Strelau, J.; Szczepaniak, P.; Śliwińska, M. NEO-FFI; Inwentarz Osobowości Paula T. Costy Jr i Roberta R. McCrae. Adaptacja Polska; Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego: Warszawa, Poland, 2010; pp. 12–24. [Google Scholar]
- Cybis, N.; Rowinski, T.; Paul, J. Development of the Polish version of Zimbardo Time Perspective Inventory. In Proceedings of the 1st International Conference of Time Perspective, Coimbra, Portugal, 5–8 September 2012. [Google Scholar]
- Juczyński, Z. Narzędzia Pomiaru w Promocji Psychologii Zdrowia; Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego: Warszawa, Poland, 2012; pp. 81–88. [Google Scholar]
- Zimbardo, P.; Boyd, J. The Time Paradox: The New Psychology of Time That Will Change Your Life; Free Press: New York, NY, USA, 2008. [Google Scholar]
- Zhang, J.W.; Howell, R.T.; Stolarski, M. Comparing Three Methods to Measure a Balanced Time Perspective: The Relationship Between a Balanced Time Perspective and Subjective Well-Being. J. Happiness Stud. 2013, 14, 169–184. [Google Scholar] [CrossRef]
- McCrae, R.R.; John, O.P. An introduction to the five-factor model and its applications. J. Pers. 1992, 60, 175–215. [Google Scholar] [CrossRef]
- Neeme, M.; Aavik, A.; Aavik, T.; Punab, M. Personality and utilization of prostate cancer testing: Evidence for the influence of neuroticism and conscientiousness. SAGE Open 2015, 5, 2158244015593324. [Google Scholar] [CrossRef]
- Perry, L.M.; Hoerger, M.; Silberstein, J.; Sartor, O.; Duberstein, P. Understanding the distressed prostate cancer patient: Role of personality. Psycho-Oncol. 2018, 27, 810–816. [Google Scholar] [CrossRef]
- de Moor, M.H.M.; Beem, A.L.; Stubbe, J.H.; Boomsma, D.I.; de Geus, E.J.C. Regular exercise, anxiety, depression and personality: A population-based study. Prev. Med. 2006, 42, 273–279. [Google Scholar] [CrossRef]
- Chang, H.J.; Chen, W.X.; Lin, E.C.L.; Tung, Y.Y.; Fetzer, S.; Lin, M.F. Delay in seeking medical evaluations and predictors of self-efficacy among women with newly diagnosed breast cancer: A longitudinal study. Int. J. Nurs. Stud. 2014, 51, 1036–1047. [Google Scholar] [CrossRef]
- Bonsaksen, T.; Lerdal, A.; Heir, T.; Ekeberg, Ø.; Skogstad, L.; Grimholt, T.K.; Schou-Bredal, I. General self-efficacy in the Norwegian population: Differences and similarities between sociodemographic groups. Scand. J. Public Health 2019, 47, 695–704. [Google Scholar] [CrossRef]
- İzci, F.; Erdogan, Z.İ.; İlgün, A.S.; Çelebi, E.; Alço, G.; Kocaman, N.; Ordu, Ç.; Öztürk, A.; Duymaz, T.; Pilavcı, K.N.; et al. Impact of personality traits, anxiety, depression and hopelessness levels on quality of life in the patients with breast cancer. Eur. J. Breast Health 2018, 14, 105. [Google Scholar] [CrossRef]
- Macía, P.; Gorbeña, S.; Gómez, A.; Barranco, M.; Iraurgi, I. Role of neuroticism and extraversion in the emotional health of people with cancer. Heliyon 2020, 6, e04281. [Google Scholar] [CrossRef]
- van der Steeg, A.F.W.; de Vries, J.; Roukema, J.A. Anxious personality and breast cancer: Possible negative impact on quality of life after breast-conserving therapy. World J. Surg. 2010, 34, 1453–1460. [Google Scholar] [CrossRef] [PubMed]
- Hampson, S.E.; Goldberg, L.R.; Vogt, T.M.; Dubanoski, J.P. Mechanisms by which childhood personality traits influence adult health status: Educational attainment and healthy behaviors. Health Psychol. 2007, 26, 121. [Google Scholar] [CrossRef] [PubMed]
- Hirsh, J.B.; Kang, S.K.; Bodenhausen, G.V. Personalized persuasion: Tailoring persuasive appeals to recipients’ personality traits. Psychol. Sci. 2012, 23, 578–581. [Google Scholar] [CrossRef] [PubMed]
- Bogg, T.; Roberts, B.W. Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychol. Bull. 2004, 130, 887. [Google Scholar] [CrossRef]
- Wortman, C.B.; Dunkel-Schetter, C. Interpersonal relationships and cancer: A theoretical analysis. J. Soc. Issues 1979, 35, 120–155. [Google Scholar] [CrossRef]
- Jensen-Campbell, L.A.; Gleason, K.A.; Adams, R.; Malcolm, K.T. Interpersonal conflict, agreeableness, and personality development. J. Pers. 2003, 71, 1059–1086. [Google Scholar] [CrossRef]
- Shigemoto, Y. Moderating Effect of Agreeableness on Coping Among Cancer Survivors: A Longitudinal Analysis. J. Loss Trauma 2018, 23, 588–599. [Google Scholar] [CrossRef]
- Flynn, K.E.; Smith, M.A. Personality and health care decision-making style. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2007, 62, P261–P267. [Google Scholar] [CrossRef]
- Kamen, C.; Mustian, K.M.; Heckler, C.; Janelsins, M.C.; Peppone, L.J.; Mohile, S.; McMahon, J.M.; Lord, R.; Flynn, P.J.; Weiss, M.; et al. The association between partner support and psychological distress among prostate cancer survivors in a nationwide study. J. Cancer Surviv. 2015, 9, 492–499. [Google Scholar] [CrossRef]
- Wyszomirska, J.; Gajda, M.; Janas, J.; Gomulski, M.; Wydmański, J. Evaluation of the impact of social support on mental adjustment to cancer during palliative or radical treatment. Psychoonkologia 2014, 18, 89–96. [Google Scholar]
- Jaarsma, T.A.; Pool, G.; Sanderman, R.; Ranchor, A.V. Psychometric properties of the Dutch version of the posttraumatic growth inventory among cancer patients. Psycho-Oncol. J. Psychol. Soc. Behav. Dimens. Cancer 2006, 15, 911–920. [Google Scholar] [CrossRef] [PubMed]
- Strelau, J. Różnice Indywidualne: Historia, Determinanty, Zastosowania, 2nd ed.; Wydawnictwo Naukowe “Scholar”; Szkoła Wyższa Psychologii Społecznej: Warszawa, Poland, 2016; pp. 345–467. [Google Scholar]
- Hamidou, Z.; Auquier, P.; Leroy, T.; Barlesi, F.; Salas, S.; Chinot, O.; Baumstarck, K. Dyadic effects of coping strategies, time perspectives, and personality on the quality of life of cancer patients and their caregivers. Psycho-Oncol. 2018, 27, 590–599. [Google Scholar] [CrossRef] [PubMed]
- Strathman, A.; Gleicher, F.; Boninger, D.S.; Edwards, C.S. The consideration of future consequences: Weighing immediate and distant outcomes of behavior. J. Pers. Soc. Psychol. 1994, 66, 742. [Google Scholar] [CrossRef]
- Drake, L.; Duncan, E.; Sutherland, F.; Abernethy, C.; Henry, C. Time perspective and correlates of wellbeing. Time Soc. 2008, 17, 47–61. [Google Scholar] [CrossRef]
- Henson, J.M.; Carey, M.P.; Carey, K.B.; Maisto, S.A. Associations among health behaviors and time perspective in young adults: Model testing with boot-strapping replication. J. Behav. Med. 2006, 29, 127–137. [Google Scholar] [CrossRef]
- Wakefield, C.E.; Homewood, J.; Taylor, A.; Mahmut, M.; Meiser, B. Time perspective in hereditary cancer: Psychometric properties of a short form of the Zimbardo Time Perspective Inventory in a community and clinical sample. Genet. Test. Mol. Biomark. 2010, 14, 617–627. [Google Scholar] [CrossRef]
- Lefèvre, H.K.; Mirabel-Sarron, C.; Docteur, A.; Leclerc, V.; Laszcz, A.; Gorwood, P.; Bungener, C. Time perspective differences between depressed patients and non-depressed participants, and their relationships with depressive and anxiety symptoms. J. Affect. Disord. 2019, 246, 320–326. [Google Scholar] [CrossRef]
- McKay, M.T.; Cole, J.C. The relationship between balanced and negative time perspectives, and symptoms of anxiety and depression. Psychiatry Res. 2020, 293, 113383. [Google Scholar] [CrossRef]
- Stolarski, M.; Matthews, G. Time Perspectives Predict Mood States and Satisfaction with Life over and above Personality. Curr. Psychol. 2016, 35, 516–526. [Google Scholar] [CrossRef]
- Bitsko, M.J.; Stern, M.; Dillon, R.; Russell, E.C.; Laver, J. Happiness and time perspective as potential mediators of quality of life and depression in adolescent cancer. Pediatr. Blood Cancer 2008, 50, 613–619. [Google Scholar] [CrossRef]
- Bettencourt, B.A.; Talley, A.E.; Molix, L.; Schlegel, R.; Westgate, S.J. Rural and urban breast cancer patients: Health locus of control and psychological adjustment. Psycho-Oncol. J. Psychol. Soc. Behav. Dimens. Cancer 2008, 17, 932–939. [Google Scholar] [CrossRef] [PubMed]
- Bourjolly, J.N. Locus of control among black and white women with breast cancer: A preliminary study. J. Psychosoc. Oncol. 1999, 17, 21–31. [Google Scholar] [CrossRef]
- Iskandarsyah, A.; de Klerk, C.; Suardi, D.R.; Sadarjoen, S.S.; Passchier, J. Health locus of control in Indonesian women with breast cancer: A comparison with healthy women. Asian Pac. J. Cancer Prev. 2014, 15, 9191–9197. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Naz, R.; Kamal, A.; Mahmood, A. Relationship of emotional intelligence and health locus of control among female breast cancer patients in pakistan. PAFMJ 2016, 66, 903–908. [Google Scholar]
- Heiser, C. What a Day at the Beach Does to Your Brain. Available online: https://www.nbcnews.com/better/health/what-beach-does-your-brain-ncna787231 (accessed on 29 June 2022).
- Murphy, N.A.; Carbone, P.S. Disabilities C on C with. Promoting the participation of children with disabilities in sports, recreation, and physical activities. Pediatrics 2008, 121, 1057–1061. [Google Scholar] [CrossRef]
- Health Fitness Revolution. Top 10 Health Benefits of Sailing. Available online: http://www.healthfitnessrevolution.com/top-10-benefits-sailing (accessed on 13 June 2022).
- Sorokowska, A.; Słowińska, A.; Zbieg, A.; Sorokowski, P. Polska Adaptacja Testu Ten Item Personality Inventory (TIPI)–TIPI-PL–Wersja Standardowa i Internetowa; WrocLab: Wrocław, Poland, 2014. [Google Scholar]
| Variable | N | % |
|---|---|---|
| Dwelling-place | ||
| Village | 10 | 17.85 |
| City with up to 100,000 inhabitants | 18 | 32.14 |
| City with over 100,000 inhabitants | 28 | 50.0 |
| Education | ||
| Primary | 0 | 0 |
| Vocational | 4 | 7.14 |
| Secondary | 9 | 16.07 |
| Higher | 43 | 76.78 |
| Employment | ||
| Currently working | 40 | 71.42 |
| Currently on sick leave/rehabilitation benefit | 6 | 10.71 |
| Pensioner | 5 | 8.92 |
| Retiree | 4 | 7.14 |
| Unemployed | 1 | 1.78 |
| Partner status | ||
| In relationship | 40 | 71.42 |
| Single | 16 | 28.57 |
| Faith | ||
| Practicing believer | 24 | 42.85 |
| Non-practicing believer | 21 | 37.50 |
| Doubter | 7 | 12.50 |
| Non-believer | 4 | 7.14 |
| Variable | N | % |
|---|---|---|
| Oncological diagnosis | ||
| Breast cancer | 35 | 62.50 |
| Ovarian cancer | 7 | 12.50 |
| Cervical cancer | 4 | 7.14 |
| Hodgkin’s lymphoma | 3 | 5.35 |
| Thyroid cancer | 3 | 5.35 |
| Other | 9 | 16.07 |
| Previous oncological treatment | ||
| No recommendation or only observation | 0 | 0.0 |
| Surgical treatment | 50 | 89.28 |
| Chemotherapy | 39 | 69.64 |
| Radiotherapy | 34 | 60.71 |
| Hormone therapy | 26 | 46.42 |
| Other | 10 | 17.85 |
| Current oncological treatment | ||
| No recommendation or only observation | 27 | 48.21 |
| Surgical treatment | 0 | 0.0 |
| Chemotherapy | 4 | 7.14 |
| Radiotherapy | 2 | 3.57 |
| Hormone therapy | 23 | 41.07 |
| Other | 4 | 7.14 |
| Planned oncological treatment | ||
| No recommendation or only observation | 35 | 62.50 |
| Surgical treatment | 3 | 5.35 |
| Chemotherapy | 4 | 7.14 |
| Radiotherapy | 0 | 0.0 |
| Hormone therapy | 15 | 26.78 |
| Other | 0 | 0.0 |
| Chronic diseases | ||
| Hypertension | 14 | 25.00 |
| Hashimoto disease/hypothyroidism | 9 | 16.07 |
| Diabetes | 2 | 3.57 |
| Asthma | 2 | 3.57 |
| Depressive disorders | 13 | 23.21 |
| Anxiety disorders | 13 | 23.21 |
| Other | 5 | 8.92 |
| Medications treatment | ||
| Tamoxifen | 13 | 23.21 |
| Levothyroxine | 12 | 21.42 |
| Selective serotonin reuptake inhibitors | 7 | 12.50 |
| Bisoprolol | 3 | 5.35 |
| Other | 33 | 58.92 |
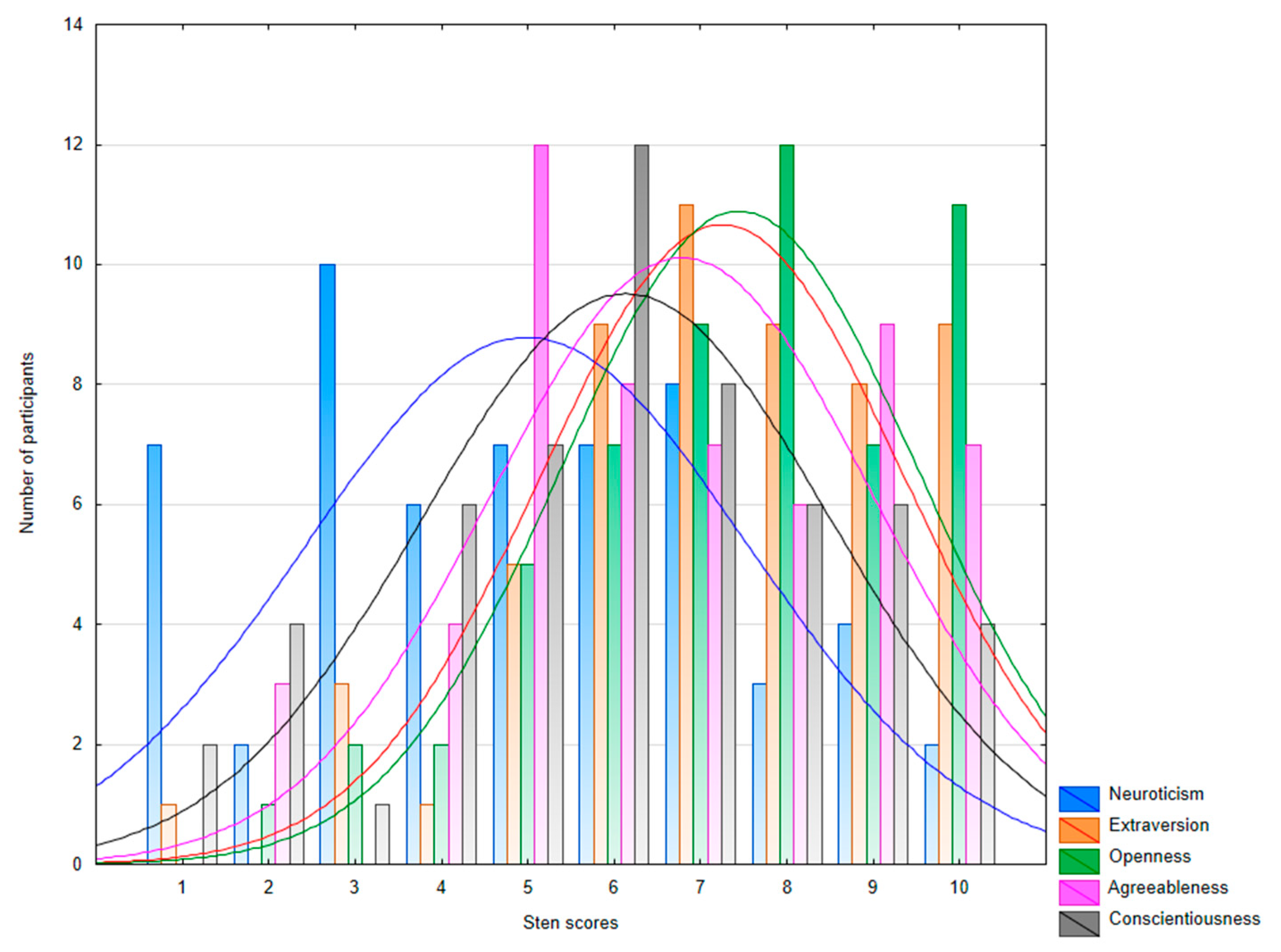
| Variable | M | SD | Me | Mo | Min. | Max. |
|---|---|---|---|---|---|---|
| NEO Five-Factor Inventory (NEO-FFI) | ||||||
| Neuroticism | 21.62 | 9.33 | 22.00 | 23.00 | 2.00 | 42.00 |
| Extraversion | 32.48 | 7.02 | 33.00 | 33.00 | 14.00 | 47.00 |
| Openness | 31.50 | 6.31 | 32.00 | 33.00 | 18.00 | 44.00 |
| Agreeableness | 34.53 | 5.74 | 35.00 | 33.00 | 20.00 | 48.00 |
| Conscientiousness | 34.57 | 7.82 | 35.50 | 35.00 | 12.00 | 48.00 |
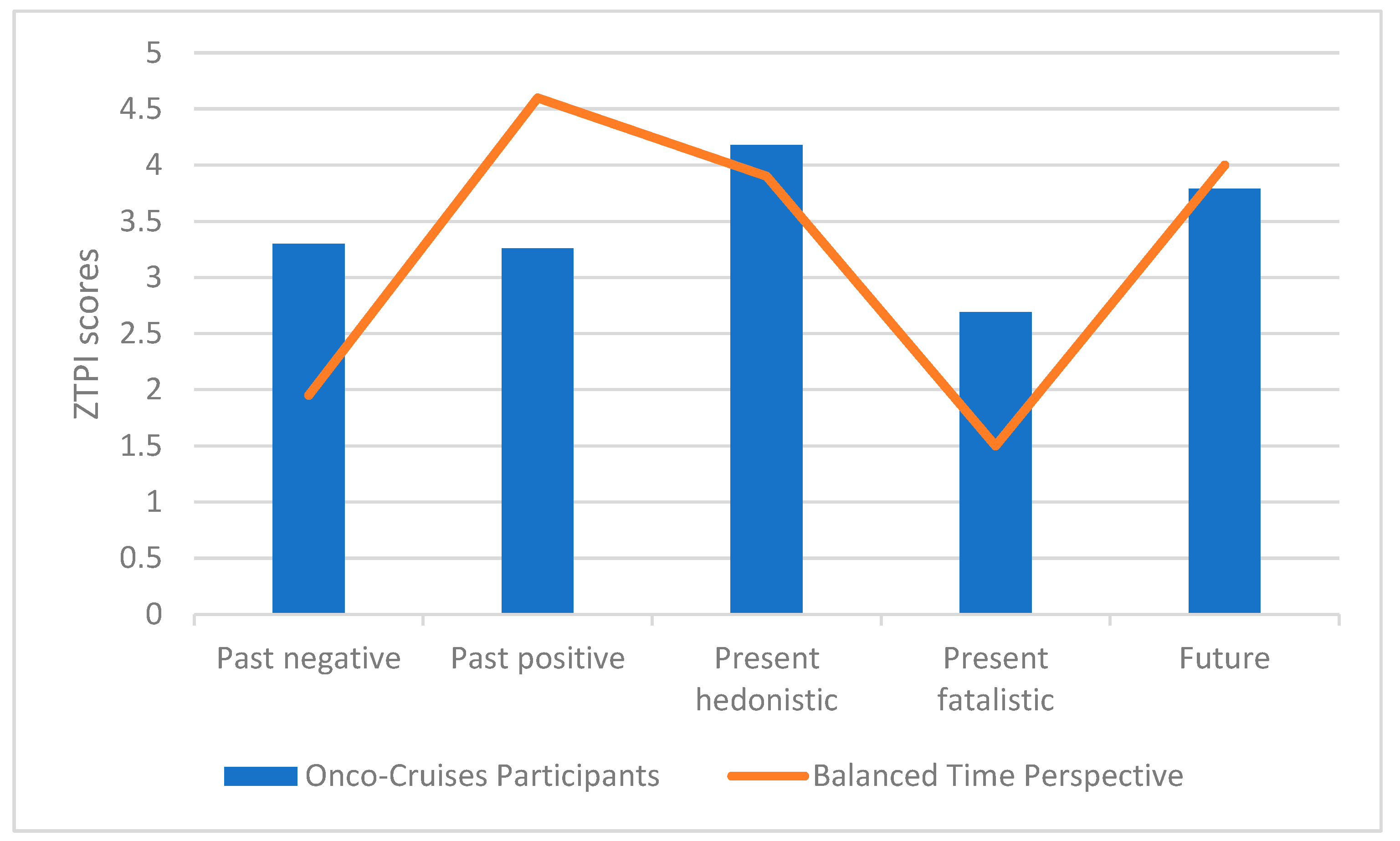
| Zimbardo Time Perspective Inventory (ZTPI) | ||||||
| Past negative | 9.92 | 3.49 | 10.00 | 13.00 | 3.00 | 15.00 |
| Future | 11.39 | 2.67 | 12.00 | 12.00 | 4.00 | 15.00 |
| Present hedonistic | 12.55 | 1.46 | 13.00 | 13.00 | 9.00 | 15.00 |
| Present fatalistic | 8.08 | 3.03 | 8.00 | 8.00 | 3.00 | 15.00 |
| Past positive | 9.80 | 2.95 | 10.00 | 10/11/12 | 3.00 | 15.00 |
| Multidimensional Health Locus of Control Scale (MHLC) | ||||||
| Internal | 23.25 | 5.43 | 24.00 | 26.00 | 9.00 | 34.00 |
| Powerful Others | 20.57 | 5.33 | 20.00 | 19.00 | 9.00 | 32.00 |
| Chance | 20.19 | 5.76 | 19.50 | 18.00 | 9.00 | 36.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wyszomirska, J.; Bąk-Sosnowska, M.; Modrzejewska, A. “All Hands on Deck”: Psychological Characteristics of Women with Experience of Oncological Disease Participating in Sailing Cruise—A Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 13133. https://doi.org/10.3390/ijerph192013133
Wyszomirska J, Bąk-Sosnowska M, Modrzejewska A. “All Hands on Deck”: Psychological Characteristics of Women with Experience of Oncological Disease Participating in Sailing Cruise—A Pilot Study. International Journal of Environmental Research and Public Health. 2022; 19(20):13133. https://doi.org/10.3390/ijerph192013133
Chicago/Turabian StyleWyszomirska, Julia, Monika Bąk-Sosnowska, and Adriana Modrzejewska. 2022. "“All Hands on Deck”: Psychological Characteristics of Women with Experience of Oncological Disease Participating in Sailing Cruise—A Pilot Study" International Journal of Environmental Research and Public Health 19, no. 20: 13133. https://doi.org/10.3390/ijerph192013133
APA StyleWyszomirska, J., Bąk-Sosnowska, M., & Modrzejewska, A. (2022). “All Hands on Deck”: Psychological Characteristics of Women with Experience of Oncological Disease Participating in Sailing Cruise—A Pilot Study. International Journal of Environmental Research and Public Health, 19(20), 13133. https://doi.org/10.3390/ijerph192013133









