Barriers and Expectations of Adolescents Regarding the Identification and Management of Their Psychoactive Substance Use by Their General Practitioner
Abstract
:1. Introduction
2. Methods
2.1. Type of Study
2.2. Population Concerned
2.3. Method of Investigation
- -
- Number of times adolescents had visited their GP in the year.
- -
- Consumption of different PASs by adolescents and their consequences according to the screening scale for problematic alcohol and drug use among adolescents (DEP-ADO) [16].
- -
- An ad hoc multiple-choice questionnaire exploring adolescents’ expectations of their relationship with their GP, particularly regarding PAS, the various possible contacts for PAS consumption, their point of view on the use of a questionnaire as a tool for identifying PAS consumption, their point of view on the place of parents during a GP consultation, and, last, their knowledge of associations providing assistance to young people and adolescents.
- -
- Sociodemographic data and the adolescents’ lifestyle: gender, age, level of education, and urban or rural habitat.
- -
- This study was approved by the ethics commission of the academic department of general medicine of the Midi-Pyrénées region, France, under number 2018-009.
2.4. Screening Scale for Problematic Alcohol and Drug Use among Adolescents: DEP-ADO
2.5. Statistical Analysis
3. Results
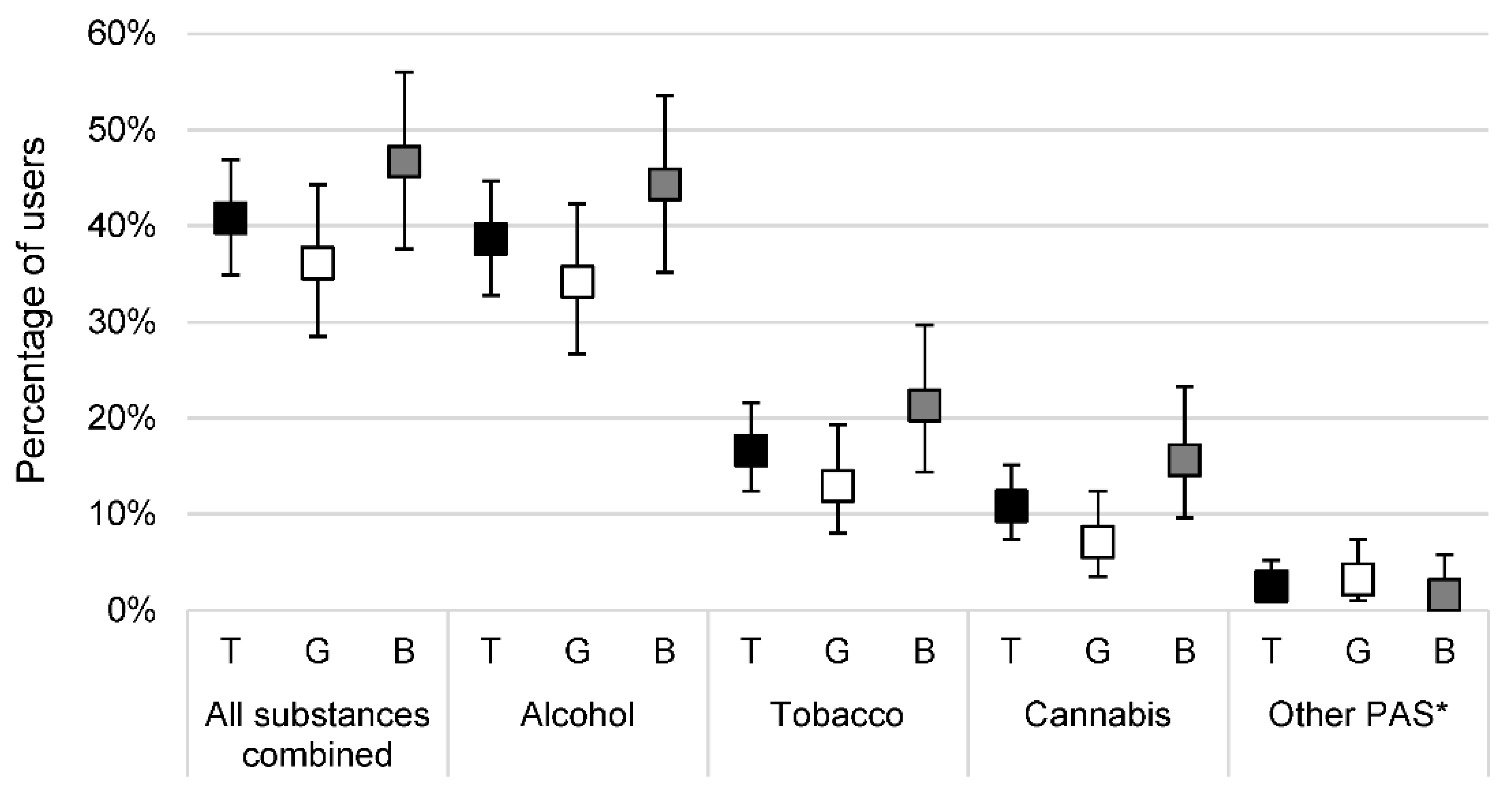
3.1. Analysis of Consumption by Gender and PAS Consumed
3.2. Users’ Analysis
3.3. Multiple Correspondence Analysis (MCA)
3.4. Analysis of the Relationship with Their GP according to the Adolescents’ Use Profiles
4. Discussion
5. Implications and Contribution
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Spilka, S.; Le Nézet, O.; Janssen, E.; Brissot, A.; Philippon, A.; Shah, J.; Chyderiotis, S. Les drogues à 17 ans: Analyse de L’enquête ESCAPAD 2017. Observatoire Français des Drogues et des Toxicomanies; 2018; p. 8. (Tendances). Report No.: 123. Available online: https://www.ofdt.fr/publications/collections/periodiques/lettre-tendances/les-drogues-17-ans-analyse-de-lenquete-escapad-2017-tendances-123-fevrier-2018/ (accessed on 5 March 2020).
- Le Borgès, E.; Quatremère, G.; Andler, R.; Arwidson, P.; Nguyen-Thanh, V.; Spilka, S.; Spilka, S.; le Nézet, O.; Janssen, E.; Brissot, A.; et al. Consommation de substances psychoactives chez les jeunes en France et dans certains pays à revenus élevés. In État des Lieux des Modes et Niveaux de Consommation et Facteurs Associés; Santé Publique France: Saint-Maurice, France, 2019. [Google Scholar]
- Com-Ruelle, L.; Le Guen, N. Les Jeunes et l’alcool: Évolution des Comportements, Facteurs de Risque et Eléments Protecteurs. Quest Déconomie Santé 2013. Available online: https://www.irdes.fr/recherche/questions-d-economie-de-la-sante/192-les-jeunes-et-l-alcool-evolution-des-comportements-facteurs-de-risque-et-elements-protecteurs.pdf (accessed on 12 September 2022).
- Kraus, L.; Nociar, A. ESPAD Report 2015: Results from the European School Survey Project on Alcohol and Other Drugs. European Monitoring Centre for Drugs and Drug Addiction. 2016. Available online: http://www.espad.org/report/summary (accessed on 12 September 2022).
- Beck, F.; Dervaux, A.; Roscoät, E.D.; Gallopel-Morvan, K.; Grall-Bronnec, M.; Kern, L.; Marie-Odile Krebs, S.L.; Legleye , S.; Melchior, M.; Naassila, M.; et al. Conduites Addictives Chez les Adolescents: Usages, Prévention et Accompagnement. Institut National de la Santé et de la Recherche médicale (INSERM); 2014 avr. p. Paris: Inserm: Éditions EDP Sciences (ISSN: 1264-1782)/500p. Available online: https://www.hal.inserm.fr/inserm-02102920 (accessed on 15 September 2020).
- Reynaud, M.; Santé FD Générale de, la. Usage Nocif de Substances Psychoactives: Identification des Usages à Risque, Outils de Repérage, Conduites à tenir. La Documentation Française; 2002. Available online: https://www.vie-publique.fr/sites/default/files/rapport/pdf/024000138.pdf (accessed on 12 September 2022).
- Windle, M.; Mun, E.Y.; Windle, R.C. Adolescent-to-Young Adulthood Heavy Drinking Trajectories and Their Prospective Predictors. J. Stud. Alcohol. 2005, 66, 313–322. Available online: http://www.jsad.com/doi/10.15288/jsa.2005.66.313 (accessed on 1 October 2020). [CrossRef] [PubMed]
- Welch, K.A.; Carson, A.; Lawrie, S.M. Brain Structure in Adolescents and Young Adults with Alcohol Problems: Systematic Review of Imaging Studies. Alcohol Alcohol. 2013, 48, 433–444. Available online: https://academic.oup.com/alcalc/article/48/4/433/534074 (accessed on 1 October 2020). [CrossRef]
- Quinn, P.D.; Harden, K.P. Differential Changes in Impulsivity and Sensation Seeking and the Escalation of Substance Use from Adolescence to Early Adulthood. Dev. Psychopathol. 2013, 25, 223–239. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3967723/ (accessed on 22 September 2020). [CrossRef] [PubMed] [Green Version]
- Costanza, A.; Rothen, S.; Achab, S.; Thorens, G.; Baertschi, M.; Weber, K.; Canuto, A.; Richard-Lepouriel, H.; Perroud, N.; Zullino, D. Impulsivity and Impulsivity-Related Endophenotypes in Suicidal Patients with Substance Use Disorders: An Exploratory Study. Int. J. Ment. Health Addict. 2021, 19, 1729–1744. [Google Scholar] [CrossRef] [Green Version]
- Assemblée mondiale de la Santé 64. Risques pour la Santé des Jeunes: Rapport du Secrétariat. 2011. Available online: https://apps.who.int/iris/handle/10665/4393 (accessed on 10 September 2020).
- Gautier, A.; Berra, N. Baromètre Santé Médecins Généralistes 2009. St-Denis Inpes Coll Baromètres Santé. 2011. Available online: https://sites.uclouvain.be/reso/opac_css/doc_num.php?explnum_id=2523 (accessed on 12 September 2022).
- Teoli, R.; Haller, D.M.; Ingrand, P.; Binder, P. Comparaison des Représentations et Comportements des Médecins Généralistes du Canton de Genève et du Poitou-Charentes. Sante Publique 2016, 28, 187–195. Available online: https://www.cairn.info/revue-sante-publique-2016-2-page-187.htm (accessed on 17 September 2020). [CrossRef] [PubMed] [Green Version]
- Choquet, M.; Ledoux, S. Attentes et Comportements des Adolescents; INSERM: Paris, France, 1998. [Google Scholar]
- Binder, P. Intervenir sur les Addictions en Médecine Générale. Exerc. Rev. Fr. Médecine Générale 2017, 24–31. Available online: https://www.exercer.fr/sommaire/51 (accessed on 17 September 2020).
- Gosselin, M.; Bergeron, J. RISQ Recherche et Intervention sur les Substances Psychoactives, Fédération Québécoise des Centres de Réadaptation Pour Personnes Alccoliques et Autres Toxicomanies, Université de Montréal; Centre Dollard-Cormier 950, rue de Louvain Est, Montréal (Québec) 1993. Available online: https://oraprdnt.uqtr.uquebec.ca/pls/public/docs/FWG/GSC/Publication/4242/60/5333/1/61296/5/F801751859_1993_Evaluation_SCL.pdf (accessed on 12 September 2022).
- Spilka, S.; Godeau, E.; Le Nézet, O.; Ehlinger, V.; Janssen, E.; Brissot, A.; Philippon, A.; Chyderiotis, S. Usages d’alcool, de tabac et de cannabis chez les adolescents du secondaire en 2018. Tendances 2019, 132, 4. [Google Scholar]
- Godeau, E.; Ehlinger, V.; Spilka, S. EnCLASS: An innovative project merging 2 international surveys (HBSC/ESPAD) among French students. Eur. J. Public Health 2019, 29 (Suppl. 4), ckz187. [Google Scholar] [CrossRef]
- Spilka, S.; Ehlinger, V.; Le Nézet, O.; Pacoricona, D.; Ngantcha, M.; Godeau, E. Alcool, Tabac et Cannabis en 2014, Durant les «Années Collège». Observatoire Français des Drogues et des Toxicomanies; 2015; p. 6. (Tendances). Report No.: 126. Available online: https://www.ofdt.fr/publications/collections/periodiques/lettre-tendances/alcool-tabac-et-cannabis-en-2014-durant-les-annees-college-tendances-106-decembre-2015 (accessed on 5 March 2020).
- Beck, F.; Guignard, R.; Obradovic, I.; Gautier, A.; Karila, L. Le Développement du Repérage des Pratiques Addictives en Médecine Générale en France. Rev. Dépidémiologie St. Publique 2011, 59, 285–294. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0398762011003099 (accessed on 12 November 2020). [CrossRef] [PubMed]
- Rost, K.; Burnam, M.A.; Smith, G.R. Development of screeners for depressive disorders and substance disorder history. Med. Care 1993, 31, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Svanum, S.; McGrew, J. Prospective screening of substance dependence: The advantages of directness. Addict. Behav. 1995, 20, 205–213. [Google Scholar] [CrossRef]


| Total (N = 277) | Users * (N = 113) | Nonusers † (N = 164) | p Value | |
|---|---|---|---|---|
| Female gender | 155 (56%) | 56 (50%) | 99 (60%) | 0.08 |
| Age (years) | 14.5 ± 1.7 | 15.6 ± 1.4 | 13.8 ± 1.4 | <0.001 |
| Housing with parents or family | 273 (99%) | 110 (97%) | 163 (99%) | 0.31 |
| Urban localization | 260 (94%) | 104 (92%) | 156 (95%) | 0.29 |
| Level of education | <0.001 | |||
| Middle school | 161 (58%) | 32 (28%) | 129 (79%) | |
| General high school | 57 (21%) | 37 (33%) | 20 (12%) | |
| Vocational school | 32 (12%) | 22 (19%) | 10 (6%) | |
| Technical school | 18 (6%) | 13 (12%) | 5 (3%) | |
| Apprentice training center | 5 (2%) | 5 (4%) | 0 (0%) | |
| Other ‡ | 4 (1%) | 4 (4%) | 0 (0%) |
| Total (N = 113) | Girls (N = 56) | Boys (N = 57) | p Value | |
|---|---|---|---|---|
| Age of first use of any PAS (years) | 13.7 ± 1.8 | 13.8 ± 1.9 | 13.6 ± 1.8 | 0.44 |
| Age of regular use of any PAS (years) (n = 35) | 14.1 ± 2.0 | 13.4 ± 2.5 | 14.6 ± 1.4 | 0.20 |
| PAS use in the last 30 days | 49 (43%) | 22 (39%) | 27 (47%) | 0.39 |
| Number of alcohol use of ≥5 drinks on the same occasion during the last 12 months | 0 [0; 3] | 0 [0; 1] | 1 [0; 6] | 0.02 |
| DEP-ADO score | 0.21 | |||
| ≤13 | 95/112 (85%) | 49 (87%) | 46/56 (82%) | |
| 14–19 | 9/112 (8%) | 2 (4%) | 7/56 (13%) | |
| ≥20 | 8/112 (7%) | 5 (9%) | 3/56 (5%) |
| 1 PAS * (N = 68) | 2 PAS * (N = 20) | 3 PAS * (N = 25) | p Value | |
|---|---|---|---|---|
| Female gender | 38 (56%) | 8 (40%) | 10 (40%) | 0.26 |
| Age of first use of any PAS (years) | 14.0 ± 1.8 | 13.7 ± 1.6 | 12.9 ± 1.9 | 0.03 |
| Age of regular use of any PAS (years) (n = 35) | 15.5 ± 0.7 | 14.3 ± 2.6 | 13.8 ± 1.6 | 0.16 |
| Use of another PAS † | 0 (0%) | 0 (0%) | 7 (28%) | <0.001 |
| PAS use in the last 30 days | 19 (28%) | 9 (45%) | 21 (84%) | <0.001 |
| Number of binge drinking ‡ during the last 12 months | 0 [0; 1] | 1 [0; 1] | 6 [3; 18] | <0.001 |
| DEP-ADO score | <0.001 | |||
| ≤13 | 66/67 (99%) | 20 (100%) | 9 (36%) | |
| 14–19 | 1/67 (1%) | 0 (0%) | 8 (32%) | |
| ≥20 | 0/67 (0%) | 0 (0%) | 8 (32%) |
| Group 1 | Group 2 | Group 3 | p Value | |
|---|---|---|---|---|
| (n = 134) | (n = 71) | (n = 38) | ||
| Female gender | 77 (57%) | 46 (65%) | 13 (34%) | 0.008 |
| Age (years) | <0.001 | |||
| 12 | 33 (25%) | 0 (0%) | 0 (0%) | |
| 13 | 45 (34%) | 1 (1%) | 1 (3%) | |
| 14 | 37 (28%) | 1 (1%) | 8 (21%) | |
| 15 | 18 (13%) | 19 (27%) | 5 (13%) | |
| 16 | 0 (0%) | 31 (44%) | 2 (5%) | |
| 17 | 1 (1%) | 19 (27%) | 22 (58%) | |
| Level of education | <0.001 | |||
| Middle school | 126 (94%) | 6 (8%) | 10 (26%) | |
| General high school | 3 (2%) | 38 (54%) | 8 (21%) | |
| Other * | 5 (4%) | 27 (38%) | 20 (53%) | |
| Alcohol use in the last 12 months | 9 (7%) | 51 (72%) | 37 (97%) | <0.001 |
| Tobacco use in the last 12 months | 3 (2%) | 4 (6%) | 35 (92%) | <0.001 |
| Cannabis use in the last 12 months | 0 (0%) | 1 (1%) | 26 (68%) | <0.001 |
| Other PAS use † in the last 12 months | 0 (0%) | 0 (0%) | 6 (16%) | <0.001 |
| Polydrug use of PAS in the last 12 months | 0 (0%) | 3 (4%) | 38 (100%) | <0.001 |
| Age of first use of any PAS (years) | <0.001 | |||
| ≤14 | 12 (9%) | 18 (25%) | 30 (79%) | |
| ≥15 | 0 (0%) | 35 (49%) | 8 (21%) | |
| Not concerned | 122 (91%) | 18 (25%) | 0 (0%) | |
| Binge drinking ‡ | 0 (0%) | 17 (24%) | 26 (68%) | <0.001 |
| DEP-ADO score ≥ 14 | 0 (0%) | 1 (1%) | 15 (39%) | <0.001 |
| Talk to their parents about their PAS use | 79 (59%) | 46 (65%) | 14 (37%) | 0.02 |
| Talk to another family member about their PAS use | 45 (34%) | 35 (49%) | 8 (21%) | 0.009 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fortin, F.; Roche, S.; Dupouy, J.; Bernard, P.; Lachal, J.; Lambert, C.; Laporte, C. Barriers and Expectations of Adolescents Regarding the Identification and Management of Their Psychoactive Substance Use by Their General Practitioner. Int. J. Environ. Res. Public Health 2022, 19, 13231. https://doi.org/10.3390/ijerph192013231
Fortin F, Roche S, Dupouy J, Bernard P, Lachal J, Lambert C, Laporte C. Barriers and Expectations of Adolescents Regarding the Identification and Management of Their Psychoactive Substance Use by Their General Practitioner. International Journal of Environmental Research and Public Health. 2022; 19(20):13231. https://doi.org/10.3390/ijerph192013231
Chicago/Turabian StyleFortin, Frédéric, Stéphanie Roche, Julie Dupouy, Pierre Bernard, Jonathan Lachal, Céline Lambert, and Catherine Laporte. 2022. "Barriers and Expectations of Adolescents Regarding the Identification and Management of Their Psychoactive Substance Use by Their General Practitioner" International Journal of Environmental Research and Public Health 19, no. 20: 13231. https://doi.org/10.3390/ijerph192013231





