A Forest Bathing Intervention in Adults with Intellectual Disabilities: A Feasibility Study Protocol
Abstract
1. Introduction
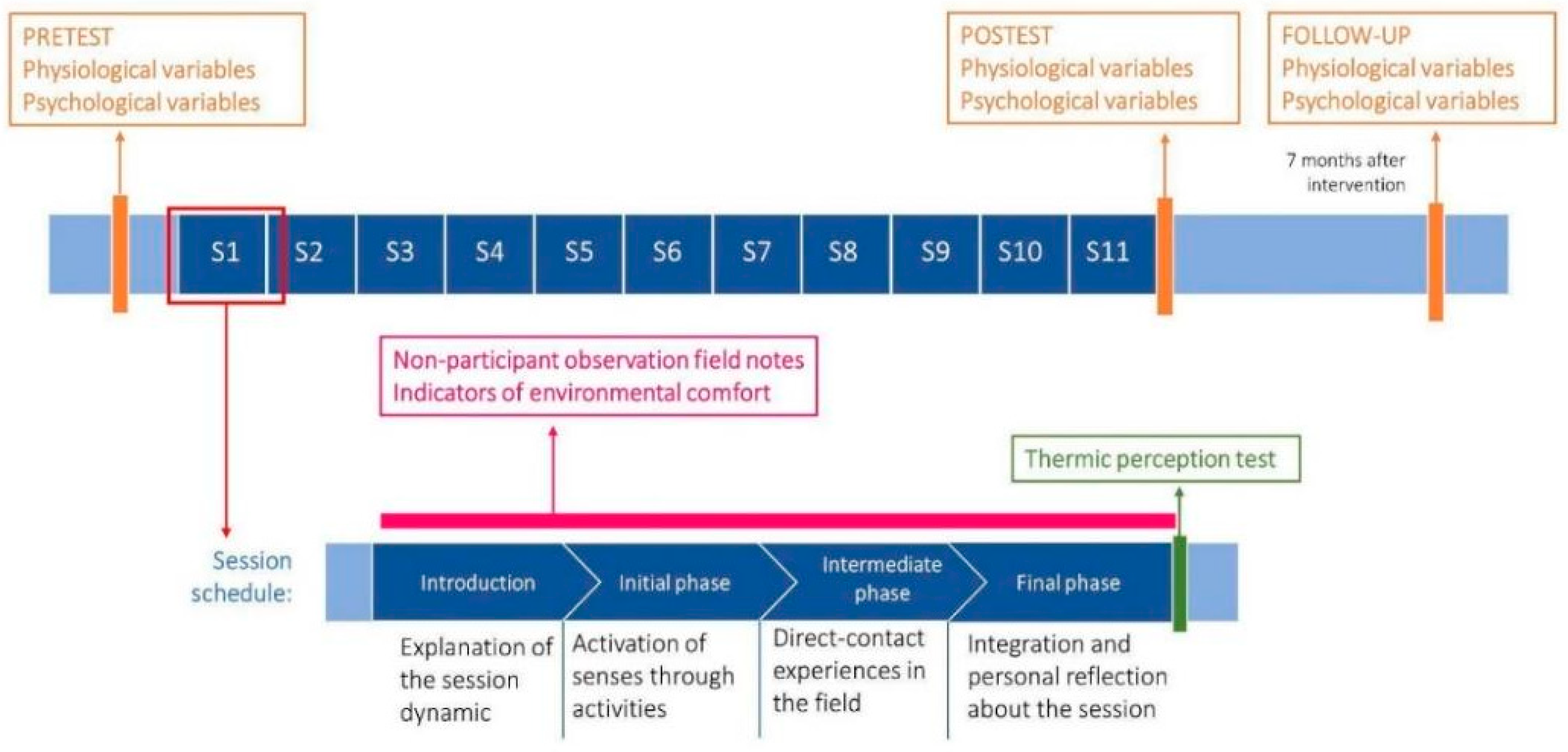
2. Study Design
2.1. Objectives
- Estimate the preliminary efficacy of an 11-session forest bathing intervention on adults with intellectual disability.
- Examine the feasibility (facilitators, barriers, unforeseen events, and indicators of environmental comfort) of applying the intervention to adults with intellectual disability.
2.2. Sample Size Determination
2.3. Participants and Recruitment
- Inclusion criteria: (1) adults with intellectual disability who are already enrolled in the activities of the participant occupational center; (2) able to read and/or speak in Spanish; and (3) with their own or legal guardian’s informed consent.
- Exclusion criteria: (1) adults with intellectual disability from other associated centers who are not enrolled in the daily activities of the participant occupational center; (2) adults with intellectual disabilities who may require intense and individual supervision from their educators throughout the activity.
3. Data Collection Plan
3.1. Outcomes, Measures and Instruments
3.1.1. Blood Pressure
3.1.2. Psychophysiological Coherence
- Time-domain [40]: to estimate the amount of variability in time intervals between successive interbeat (the standard deviation of all normal NN intervals (SDNN) and the root-mean-square analysis of successive interval differences (RMSSD);
- Frequency-domain: to estimate the distribution of the absolute or relative power (energy) into four frequency bands. High-frequency (HF) bands (0.15 to 0.4 Hz) are mainly affected by respiratory rhythms from 9 to 24 breaths per min (bpm) and reflect the parasympathetic activity. Low-frequency (LF) bands (0.04 to 0.15 Hz) are affected by baroreceptor activity and by respiratory rhythms from ~3 to 9 bpm; they reflect both sympathetic and parasympathetic activities. Very low-frequency (VLF) and ultra-low-frequency (ULF) (VLF, 0.0033 to 0.04 Hz; ULF, ≤0.0033 Hz) bands are spectral components with very low oscillations.
- Non-linear measures: to quantify the non-linear relationship between RR intervals (see [38] for more details).
3.1.3. Quality of Life
3.2. Environmental Comfort
3.3. Fidelity, Barriers, and Facilitators of the Implementation Process
4. Detailed Procedure
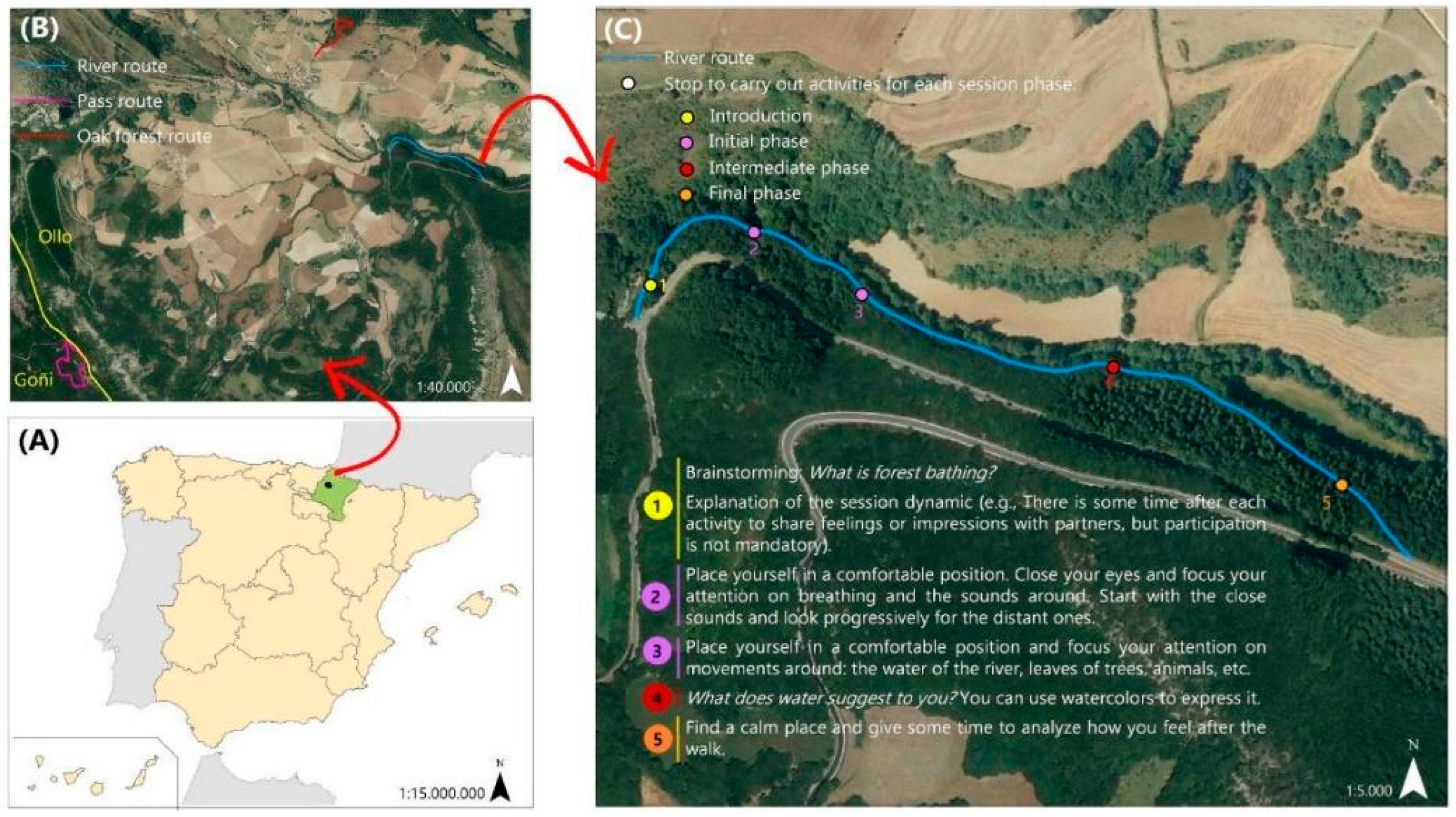
4.1. The Forest Bathing Intervention
4.2. Forest Guide Training
4.3. Ethics
5. Expected Results
- Higher quality of life.
- Reduced levels of blood pressure.
- Improved psycho-physiological coherence parameters.
6. Data Analysis Plan
7. Discussion
Limitations
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations Department of Economic and Social Affairs Population Division. In World Urbanization Prospects: The 2018 Revision (ST/ESA/SER.A/420); United Nations: New York, NY, USA, 2019; Volume 12, ISBN 9789211483192.
- Stier-Jarmer, M.; Throner, V.; Kirschneck, M.; Immich, G.; Frisch, D.; Schuh, A. The Psychological and Physical Effects of Forests on Human Health: A Systematic Review of Systematic Reviews and Meta-Analyses. Int. J. Environ. Res. Public Health 2021, 18, 1770. [Google Scholar] [CrossRef]
- Keniger, L.; Gaston, K.; Irvine, K.; Fuller, R. What Are the Benefits of Interacting with Nature? Int. J. Environ. Res. Public Health 2013, 10, 913–935. [Google Scholar] [CrossRef] [PubMed]
- Rantala, O.; Puhakka, R. Engaging with Nature: Nature Affords Well-Being for Families and Young People in Finland. Child Geogr. 2020, 18, 490–503. [Google Scholar] [CrossRef]
- Tsao, T.-M.; Hwang, J.-S.; Lin, S.-T.; Wu, C.; Tsai, M.-J.; Su, T.-C. Forest Bathing Is Better than Walking in Urban Park: Comparison of Cardiac and Vascular Function between Urban and Forest Parks. Int. J. Environ. Res. Public Health 2022, 19, 3451. [Google Scholar] [CrossRef] [PubMed]
- Zorić, M.; Farkić, J.; Kebert, M.; Mladenović, E.; Karaklić, D.; Isailović, G.; Orlović, S. Developing Forest Therapy Programmes Based on the Health Benefits of Terpenes in Dominant Tree Species in Tara National Park (Serbia). Int. J. Environ. Res. Public Health 2022, 19, 5504. [Google Scholar] [CrossRef]
- Hansen, M.M.; Jones, R.; Tocchini, K. Shinrin-Yoku (Forest Bathing) and Nature Therapy: A State-of-the-Art Review. Int. J. Environ. Res. Public Health 2017, 14, 851. [Google Scholar] [CrossRef]
- Ross, A.M.; Jones, R.J.F. Simulated Forest Immersion Therapy: Methods Development. Int. J. Environ. Res. Public Health 2022, 19, 5373. [Google Scholar] [CrossRef]
- Fu, D.; Serra, N.I.; Mansion, H.; Mansion, E.T.; Blain-Moraes, S. Assessing the Effects of Nature on Physiological States Using Wearable Technologies. Int. J. Environ. Res. Public Health 2022, 19, 1231. [Google Scholar] [CrossRef]
- Oh, B.; Lee, K.J.; Zaslawski, C.; Yeung, A.; Rosenthal, D.; Larkey, L.; Back, M. Health and Well-Being Benefits of Spending Time in Forests: Systematic Review. Environ. Health Prev. Med. 2017, 22, 71. [Google Scholar] [CrossRef]
- Rajoo, K.S.; Karam, D.S.; Abdullah, M.Z. The Physiological and Psychosocial Effects of Forest Therapy: A Systematic Review. Urban For. Urban Green. 2020, 54, 126744. [Google Scholar] [CrossRef]
- Pichler, C.; Freidl, J.; Bischof, M.; Kiem, M.; Weisböck-Erdheim, R.; Huber, D.; Squarra, G.; Murschetz, P.; Hartl, A. Mountain Hiking vs. Forest Therapy: A Study Protocol of Novel Types of Nature-Based Intervention. Int. J. Environ. Res. Public Health 2022, 19, 3888. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Wang, P.; Gao, Y.; Ye, B. Current Development Status of Forest Therapy in China. Healthcare 2020, 8, 61. [Google Scholar] [CrossRef] [PubMed]
- Stigsdotter, U.K.; Corazon, S.S.; Sidenius, U.; Refshauge, A.D.; Grahn, P. Forest Design for Mental Health Promotion—Using Perceived Sensory Dimensions to Elicit Restorative Responses. Landsc. Urban Plan 2017, 160, 1–15. [Google Scholar] [CrossRef]
- Lee, J.; Park, B.-J.; Tsunetsugu, Y.; Ohira, T.; Kagawa, T.; Miyazaki, Y. Effect of Forest Bathing on Physiological and Psychological Responses in Young Japanese Male Subjects. Public Health 2011, 125, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Mao, G.-X.; Cao, Y.-B.; Lan, X.-G.; He, Z.-H.; Chen, Z.-M.; Wang, Y.-Z.; Hu, X.-L.; Lv, Y.-D.; Wang, G.-F.; Yan, J. Therapeutic Effect of Forest Bathing on Human Hypertension in the Elderly. J. Cardiol. 2012, 60, 495–502. [Google Scholar] [CrossRef]
- Park, B.J.; Tsunetsugu, Y.; Kasetani, T.; Kagawa, T.; Miyazaki, Y. The Physiological Effects of Shinrin-Yoku (Taking in the Forest Atmosphere or Forest Bathing): Evidence from Field Experiments in 24 Forests across Japan. Environ. Health Prev. Med. 2010, 15, 18–26. [Google Scholar] [CrossRef]
- Jia, B.B.; Yang, Z.X.; Mao, G.X.; Lyu, Y.D.; Wen, X.L.; Xu, W.H.; Lyu, X.L.; Cao, Y.B.; Wang, G.F. Health Effect of Forest Bathing Trip on Elderly Patients with Chronic Obstructive Pulmonary Disease. Biomed. Environ. Sci. 2016, 29, 212–218. [Google Scholar] [CrossRef]
- Morita, E.; Imai, M.; Okawa, M.; Miyaura, T.; Miyazaki, S. A before and after Comparison of the Effects of Forest Walking on the Sleep of a Community-Based Sample of People with Sleep Complaints. Biopsychosoc. Med. 2011, 5, 13. [Google Scholar] [CrossRef]
- Shin, W.S.; Shin, C.S.; Yeoun, P.S. The Influence of Forest Therapy Camp on Depression in Alcoholics. Environ. Health Prev. Med. 2012, 17, 73–76. [Google Scholar] [CrossRef]
- Timko Olson, E.R.; Hansen, M.M.; Vermeesch, A. Mindfulness and Shinrin-Yoku: Potential for Physiological and Psychological Interventions during Uncertain Times. Int. J. Environ. Res. Public Health 2020, 17, 9340. [Google Scholar] [CrossRef]
- Bielinis, E.; Jaroszewska, A.; Łukowski, A.; Takayama, N. The Effects of a Forest Therapy Programme on Mental Hospital Patients with Affective and Psychotic Disorders. Int. J. Environ. Res. Public Health 2020, 17, 118. [Google Scholar] [CrossRef] [PubMed]
- Rosa, C.D.; Larson, L.R.; Collado, S.; Profice, C.C. Forest Therapy Can Prevent and Treat Depression: Evidence from Meta-Analyses. Urban For. Urban Green. 2021, 57, 126943. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Facts about Intellectual Disability. Available online: https://www.cdc.gov/ncbddd/developmentaldisabilities/facts-about-intellectual-disability.html (accessed on 20 August 2022).
- Anderson, L.L.; Humphries, K.; McDermott, S.; Marks, B.; Sisirak, J.; Larson, S. The State of the Science of Health and Wellness for Adults with Intellectual and Developmental Disabilities. Intellect. Dev. Disabil. 2013, 51, 385–398. [Google Scholar] [CrossRef] [PubMed]
- López-Pousa, S.; Bassets Pagès, G.; Monserrat-Vila, S.; de Gracia Blanco, M.; Hidalgo Colomé, J.; Garre-Olmo, J. Sense of Well-Being in Patients with Fibromyalgia: Aerobic Exercise Program in a Mature Forest—A Pilot Study. Evid. Based Complement. Altern. Med. 2015, 2015, 614783. [Google Scholar] [CrossRef] [PubMed]
- Bach, A.; Ceron, J.J.; Maneja, R.; Llusià, J.; Penuelas, J.; Escribano, D. Evolution of Human Salivary Stress Markers during an Eight-Hour Exposure to a Mediterranean Holm Oak Forest. A Pilot Study. Forests 2021, 12, 1600. [Google Scholar] [CrossRef]
- Muro, A.; Feliu-Soler, A.; Canals, J.; Parrado, E.; Sanz, A. Psychological Benefits of Forest Bathing during the COVID-19 Pandemic: A Pilot Study in a Mediterranean Forest Close to Urban Areas. J. For. Res. 2021, 27, 71–75. [Google Scholar] [CrossRef]
- Muro, A.; Mateo, C.; Parrado, E.; Moya, M.; Sèlvans, C.; Garriga, A.; Muntada, L.; Chamarro, A.; Sanz, A. Forest Bathing and Hiking Benefits for Mental Health during the Covid-19 Pandemic in Mediterranean Regions. Eur. J. For. Res. 2022. under review. [Google Scholar] [CrossRef]
- Skivington, K.; Matthews, L.; Simpson, S.A.; Craig, P.; Baird, J.; Blazeby, J.M.; Boyd, K.A.; Craig, N.; French, D.P.; McIntosh, E.; et al. A New Framework for Developing and Evaluating Complex Interventions: Update of Medical Research Council Guidance. BMJ 2021, 374, n2061. [Google Scholar] [CrossRef]
- Lancaster, G.A.; Dodd, S.; Williamson, P.R. Design and Analysis of Pilot Studies: Recommendations for Good Practice. J. Eval. Clin. Pract. 2004, 10, 307–312. [Google Scholar] [CrossRef]
- McCraty, R. New Frontiers in Heart Rate Variability and Social Coherence Research: Techniques, Technologies, and Implications for Improving Group Dynamics and Outcomes. Front. Public Health 2017, 5, 267. [Google Scholar] [CrossRef]
- McEwan, K.; Giles, D.; Clarke, F.J.; Kotera, Y.; Evans, G.; Terebenina, O.; Minou, L.; Teeling, C.; Basran, J.; Wood, W.; et al. A Pragmatic Controlled Trial of Forest Bathing Compared with Compassionate Mind Training in the UK: Impacts on Self-Reported Wellbeing and Heart Rate Variability. Sustainability 2021, 13, 1380. [Google Scholar] [CrossRef]
- Yu, Y.-M.; Lee, Y.-J.; Kim, J.-Y.; Yoon, S.-B.; Shin, C.-S. Effects of Forest Therapy Camp on Quality of Life and Stress in Postmenopausal Women. Forest. Sci. Technol. 2016, 12, 125–129. [Google Scholar] [CrossRef]
- Ministerio de Trabajo y Asuntos Sociales. Real Decreto 1971/1999, de 23 de Diciembre, de Procedimiento Para El Reconocimiento, Declaración y Calificación Del Grado de Discapacidad (Texto Consolidado). 2000. Available online: https://www.boe.es/eli/es/rd/1999/12/23/1971/con (accessed on 19 August 2022).
- Kang, M.-J.; Kim, H.-S.; Kim, J.-Y. Effects of Forest-Based Interventions on Mental Health: A Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2022, 19, 4884. [Google Scholar] [CrossRef]
- Yeon, P.-S.; Jeon, J.-Y.; Jung, M.-S.; Min, G.-M.; Kim, G.-Y.; Han, K.-M.; Shin, M.-J.; Jo, S.-H.; Kim, J.-G.; Shin, W.-S. Effect of Forest Therapy on Depression and Anxiety: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 12685. [Google Scholar] [CrossRef]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed]
- McCraty, R.; Atkinson, M.; Tomasino, D.; Bradley, R.T. The Coherent Heart Heart–Brain Interactions, Psychophysiological Coherence, and the Emergence of System-Wide Order. Integral. Rev. 2009, 5, 11–115. [Google Scholar]
- Tinello, D.; Kliegel, M.; Zuber, S. Does Heart Rate Variability Biofeedback Enhance Executive Functions Across the Lifespan? A Systematic Review. J. Cogn. Enhanc. 2022, 6, 126–142. [Google Scholar] [CrossRef] [PubMed]
- Verdugo Alonso, M.Á.; Gómez Sánchez, L.E.; Arias Martínez, B.; Santamaría Domínguez, M.; Clavero Herrero, D.; Tamarit Cuadrado, J. Escala INICO-FEAPS Evaluación Integral de La Calidad de Vida de Personas Con Discapacidad Intelectual o Del Desarrollo; Instituto Universitario de Integración en la Comunidad: Salamanca, Spain, 2013. [Google Scholar]
- Höppe, P. The Physiological Equivalent Temperature—A Universal Index for the Biometeorological Assessment of the Thermal Environment. Int. J. Biometeorol. 1999, 43, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.-P.; Matzarakis, A.; Hwang, R.-L. Shading Effect on Long-Term Outdoor Thermal Comfort. Build. Environ. 2010, 45, 213–221. [Google Scholar] [CrossRef]
- Teli, D.; Jentsch, M.F.; James, P.A.B. Naturally Ventilated Classrooms: An Assessment of Existing Comfort Models for Predicting the Thermal Sensation and Preference of Primary School Children. Energy Build. 2012, 53, 166–182. [Google Scholar] [CrossRef]
- Trebilcock, M.; Soto-Muñoz, J.; Yañez, M.; Figueroa-San Martin, R. The Right to Comfort: A Field Study on Adaptive Thermal Comfort in Free-Running Primary Schools in Chile. Build. Environ. 2017, 114, 455–469. [Google Scholar] [CrossRef]
- Forest Therapy Hub. Available online: https://foresttherapyhub.com/ (accessed on 14 October 2022).
- Kotte, D.; Li, Q.; Shin, W.S.; Michalsen, A. International Handbook of Forest Therapy; Cambridge Scholars Publishing: Newcastle upon Tyne, UK, 2019; ISBN (13)978-1-5275-3955-6. [Google Scholar]
- Miyazaki, Y. Shinrin-Yoku: Baños Curativos de Bosque; Blume: Barcelona, Spain, 2018; ISBN 978-84-17254-83-4. [Google Scholar]
- Shah, P.B. Intention-to-Treat and per-Protocol Analysis. Can. Med. Assoc. J. 2011, 183, 696. [Google Scholar] [CrossRef]
- Li, T.; Hutfless, S.; Scharfstein, D.O.; Daniels, M.J.; Hogan, J.W.; Little, R.J.A.; Roy, J.A.; Law, A.H.; Dickersin, K. Standards Should Be Applied in the Prevention and Handling of Missing Data for Patient-Centered Outcomes Research: A Systematic Review and Expert Consensus. J. Clin. Epidemiol. 2014, 67, 15–32. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Erlbaum: New York, NY, USA, 1988; ISBN 0203771583. [Google Scholar]
- Mayring, P. Qualitative Content Analysis: Theoretical Foundation, Basic Procedures and Software Solution; Social Science Open Access Repository (SSOAR): Klagenfurt, Austria, 2014. [Google Scholar]
- AVIFES. Baños de Bosque. Impacto en la Salud de las Personas con Enfermedad Mental; AVIFES: Bilbao, Spain, 2019. [Google Scholar]
- Kaiserbäder Insel Usedom. Available online: https://www.heilwald-heringsdorf.de/en (accessed on 14 October 2022).
- Forest Europe. Human Health and Sustainable Forest Management; Marušáková, Ľ., Sallmannshofer, M., Eds.; Forest Europe: Bratislava, Slovakia, 2019; ISBN 978-80-8093-266-4. [Google Scholar]
- Shogren, K.A.; Singh, N.N. Intervening from the “Inside Out”: Exploring the Role of Self-Determination and Mindfulness-Based Interventions for People with Intellectual and Developmental Disabilities. Adv. Neurodev. Disord. 2022, 6, 147–156. [Google Scholar] [CrossRef]
- Baer, R.A. Mindfulness Training as a Clinical Intervention: A Conceptual and Empirical Review. Clin. Psychol. Sci. Pract. 2003, 10, 125–143. [Google Scholar] [CrossRef]
- Chiesa, A.; Serretti, A. A Systematic Review of Neurobiological and Clinical Features of Mindfulness Meditations. Psychol Med. 2010, 40, 1239–1252. [Google Scholar] [CrossRef]
- Fjorback, L.O.; Arendt, M.; Ørnbøl, E.; Fink, P.; Walach, H. Mindfulness-Based Stress Reduction and Mindfulness-Based Cognitive Therapy—A Systematic Review of Randomized Controlled Trials. Acta. Psychiatr. Scand. 2011, 124, 102–119. [Google Scholar] [CrossRef]
- Chapman, M.J.; Hare, D.J.; Caton, S.; Donalds, D.; McInnis, E.; Mitchell, D. The Use of Mindfulness with People with Intellectual Disabilities: A Systematic Review and Narrative Analysis. Mindfulness 2013, 4, 179–189. [Google Scholar] [CrossRef]
- Clarke, C.; Kellett, S.; Beail, N. Systematic Review of Systematic Reviews on Psychological Therapies for People Who Have Intellectual Disabilities: 1. Quality Appraisal. Adv. Ment. Health Intellect. Disabil. 2022. ahead-of-print. [Google Scholar] [CrossRef]
- Ailey, S.H.; Heller, T.; Brown, H.E. Mental Health of Older Adults with Intellectual Disability. J. Psychosoc. Nurs. Ment. Health Serv. 2022, 60, 10–14. [Google Scholar] [CrossRef]
- Hassiotis, A.; Rudra, S. Behaviours That Challenge in Adults with Intellectual Disability: Overview of Assessment and Management. BJPsych. Adv. 2022, 1–8. [Google Scholar] [CrossRef]
- Farrow, M.R.; Washburn, K. A Review of Field Experiments on the Effect of Forest Bathing on Anxiety and Heart Rate Variability. Glob. Adv. Health Med. 2019, 8, 216495611984865. [Google Scholar] [CrossRef] [PubMed]
- Palix, J.; Akselrod, M.; Cungi, C.; Giuliani, F.; Favrod, J. Changes in Heart Rate Variability Recorded in Natural Situation with T-Shirt Integrated Sensors and Level of Observed Behavioral Excitation: A Pilot Study of Patients with Intellectual Disabilities and Psychiatric Disorders. Front. Psychiatry 2017, 8, 4. [Google Scholar] [CrossRef] [PubMed]
- Meule, A.; Fath, K.; Real, R.G.; Sütterlin, S.; Vögele, C.; Kübler, A. Quality of Life, Emotion Regulation, and Heart Rate Variability in Individuals with Intellectual Disabilities and Concomitant Impaired Vision. Psychol. Well-Being Theory Res. Pract. 2013, 3, 1–14. [Google Scholar] [CrossRef]
- Farkic, J.; Isailovic, G.; Taylor, S. Forest Bathing as a Mindful Tourism Practice. Ann. Tour. Res. Empir. Insights 2021, 2, 100028. [Google Scholar] [CrossRef]
- Hertzog, M.A. Considerations in Determining Sample Size for Pilot Studies. Res. Nurs. Health 2008, 31, 180–191. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bermejo-Martins, E.; Pueyo-Garrigues, M.; Casas, M.; Bermejo-Orduna, R.; Villarroya, A. A Forest Bathing Intervention in Adults with Intellectual Disabilities: A Feasibility Study Protocol. Int. J. Environ. Res. Public Health 2022, 19, 13589. https://doi.org/10.3390/ijerph192013589
Bermejo-Martins E, Pueyo-Garrigues M, Casas M, Bermejo-Orduna R, Villarroya A. A Forest Bathing Intervention in Adults with Intellectual Disabilities: A Feasibility Study Protocol. International Journal of Environmental Research and Public Health. 2022; 19(20):13589. https://doi.org/10.3390/ijerph192013589
Chicago/Turabian StyleBermejo-Martins, Elena, María Pueyo-Garrigues, María Casas, Raúl Bermejo-Orduna, and Ana Villarroya. 2022. "A Forest Bathing Intervention in Adults with Intellectual Disabilities: A Feasibility Study Protocol" International Journal of Environmental Research and Public Health 19, no. 20: 13589. https://doi.org/10.3390/ijerph192013589
APA StyleBermejo-Martins, E., Pueyo-Garrigues, M., Casas, M., Bermejo-Orduna, R., & Villarroya, A. (2022). A Forest Bathing Intervention in Adults with Intellectual Disabilities: A Feasibility Study Protocol. International Journal of Environmental Research and Public Health, 19(20), 13589. https://doi.org/10.3390/ijerph192013589





