Abstract
Objective: This study aimed to examine the prevalence of Internet addiction in adolescents, analyze the associations of childhood trauma, systematic family dynamics, and family functioning with Internet addiction, and investigate the mediating chain role of anxiety and depression in the relationship of childhood trauma and family functioning with adolescent Internet addiction. Methods: This was a cross-sectional study in which general sociodemographic data were obtained from 3357 adolescents in grades 6–12 who were assessed using psychometric instruments such as the Childhood Trauma Questionnaire, Young Internet Addiction Test, Systematic Family Dynamics Self-Rating Scale (SSFD), Family Functioning Assessment (FAD), Self-Rating Depression Scale (SDS), and Self-Rating Anxiety Scale (SAS). Results: (1) The prevalence of Internet addiction among adolescents was 26.09% (876/3357). The prevalence of childhood trauma was 54.96% (1845/3357), and the prevalence of Internet addiction was significantly different between adolescents who suffered childhood trauma and those who did not (χ2 = 96.801, ν = 1, p = 0.000). (2) Childhood trauma and various dimensions of systematic family dynamics had a significant negative and positive relationship with poor family functioning and anxiety or depression, respectively. (3) Childhood trauma was a positive predictor of Internet addiction through the chain-mediated effect of anxiety and depression, but there were no direct effects. Poor family functioning was a positive predictor of adolescent Internet addiction, and this positive prediction was augmented by the chain-mediated effect of anxiety and depression. Conclusions: Childhood trauma and poor family functioning or support predicted Internet addiction in adolescents, with anxiety and depression as mediators.
1. Introduction
With the rapid development of the Internet and intelligent electronic devices [1], Internet access has become a part of people’s lives. After the coronavirus disease pandemic 2019 (COVID-19) broke out in China, adolescents spent more time with electronic devices through home online learning. Furthermore, the Internet population is significantly younger [2,3]. The Internet penetration rate of minors reached 94.9% by the end of December 2021, significantly higher than that of the general population, which is 73.0% [3]. In Europe and the United States, adolescents’ Internet use time has similarly increased significantly [4]. Although the Internet has been enormously beneficial to adolescents, the associated damage it has caused cannot be ignored [5]. In clinical practice, parents and adolescents have reported a significant increase in uncontrolled Internet use, thus causing a significant increase in reports of parent–child conflict and adolescent emotional, behavioral, concentration, and learning efficiency problems. Because adolescents are still in a critical stage of mental and physical development, their cognitive function, critical thinking [4], motivation, and impulse control, especially self-control abilities, are immature. The earlier exposure to the Internet using, the more likely it is to affect the processes of transformation and maturation of brain structures, thus interfering with the development of mental dimensions such as anticipation of reward, emotional processing, decision making, and impulse control, leading to a higher risk of Internet Addiction (IA) and more serious psychological and behavioral problems for adolescents [4,6,7,8,9,10,11,12,13,14]. The prevalence of adolescent IA since the beginning of the COVID-19 pandemic was significantly higher than that observed before the pandemic [6,15,16,17,18].
Young and Rogers defined adolescents’ problems as early as 1996 [19], and researchers have found that IA causes significant damage to adolescents, including their mental health, physical health, and social functioning. IA also leads to emotional problems such as anxiety, depression, irritability [16], impaired behavioral control, impaired concentration and execution, personality changes, and negative self-perception [20,21,22]. However, adverse mental states exacerbate adolescent Internet use behavior [23]. IA can also disrupt sleep patterns and damage immature brain structure and function [21,22]. Eventually, IA among adolescents leads to many social function impairments, such as academic failure, interpersonal withdrawal, and further deterioration of interpersonal relationships [24].
The causes of adolescent IA are widespread and complex [2,25]. Among various intrapersonal factors, an individual’s childhood traumatic experience is the highest risk factor for adolescent IA [26]. Childhood trauma is a global phenomenon [27,28], and can cause serious psychological damage to an individual, leading to anxiety, depression, and other emotional and addictive behaviors [21,29,30]. Among external environmental factors, poor family environment and family dynamics may be important risk factors for IA [31,32]. McMaster’s model theory of family functioning states that the role of the family is to provide its members with the appropriate environmental conditions needed for physical, psychological, and social adaptations to growth [33]. Parents’ excessive psychological control over adolescents, poor communication, and rigid relationships with their children, as well as poor emotional relationships among family members, contribute to adolescents’ emotional and behavioral problems [6,11,32,34]. Family dysfunction is strongly associated with childhood trauma [35], which drives adolescents into the virtual world on multiple levels, leading to an increased risk of IA [6,36,37,38,39].
Based on the many causative factors associated with IA, this study aimed to identify the key causative factors and models that cause IA in adolescents to explore effective intervention methods, which will reduce the damage caused by IA and promote the healthy development of the mental, physical, and social functions of adolescents.
Therefore, this study proposed the following hypotheses related to IA.
- Adolescents’ childhood trauma and dysfunctional family are high-risk causative factors of IA.
- Adolescents’ anxiety and depression are associated with childhood trauma and family dysfunction.
- Anxiety and depression mediate the relationship between childhood trauma and poor family functioning with IA.
2. Methods
2.1. Participants
This cross-sectional study was conducted in Shanghai, China, from October to December 2020. To estimate the sample size, 189 samples were pre-tested. The prevalence of IA (π) obtained from the pretest was approximately 23.4%; a 6% relative error was allowed in this study. The absolute error was calculated as δ = 0.06π = 0.06 × 23.4%. A 95% confidence interval (CI) was adopted, and μa was 1.96. The sample size was determined using the following equation: n = [1.962 × 23.4% × (1–23.4%)]/(0.06 × 23.4%)2, which was ≈ 3493. Considering the possibility of invalid cases, the sample size must be increased by 15%; therefore, the final sample size was calculated as 3493/(1–15%), which was ≈ 4109.
After determining the sample size, the multi-stage stratified whole-group sampling method, in which two districts were randomly selected among 17 communities and counties in Shanghai, three junior high schools and three high schools were chosen in each section, and two classes were randomly selected in each grade, was used. All students in the selected classes were surveyed with the consent of their guardians, and after both, the guardians and students signed informed consent forms. A total of 4109 questionnaires were distributed, and finally, excluding incomplete questionnaires, a total of 3357 (81.7%) valid questionnaires were retrieved.
Inclusion criteria: (1) adolescents who were enrolled in public schools at the junior high and high school levels at the time of the study and (2) adolescents who voluntarily participated in the psychological assessment survey and with their guardians signed an informed consent form.
Exclusion criteria: (1) adolescents who were enrolled in school at the time of the study but had suspended their studies for various reasons and (2) adolescents who were unwilling to participate in this psychological assessment survey.
2.2. Measures
2.2.1. Demographic Information Sheet
A demographic information sheet, which collected information including sex, age, schooling grade, number of siblings, mode of living, parents’ generation, parents’ education level, parents’ marital quality, and self-assessment of family economic satisfaction (with a score of 0 to 10, 0 being little dissatisfaction and 10 being the maximal satisfaction) was distributed to the participants.
2.2.2. Childhood Trauma Questionnaire-Short Form
The Childhood Trauma Questionnaire-Short Form (CTQ-28) is a retrospective self-report questionnaire developed by Bernstein et al. [8,40], which asks questions about traumatic experiences in early childhood and adolescence and is rated from 1 (never) to 5 (very often). For each type of trauma, scores ranged from 5 to 25, and for the total trauma score, scores ran from 25 to 125. The questionnaire assesses five types of childhood trauma, including emotional abuse (EA), physical abuse (PA), sexual abuse (SA), emotional neglect (EN), and physical neglect (PN). Three additional items were used for validity ratings. An individual who experienced childhood trauma was considered to have experienced EA if the dimension scores were ≥13, PA if scores were ≥10, SA if scores were ≥8, EN if scores were ≥15, and PN if scores were ≥10. Zhao et al. (2005) [40] translated and revised the Chinese version of the CTQ-28 scale and confirmed that it has been used in clinical studies successfully with good reliability, validity, and internal consistency and Cronbach α coefficient of 0.64 and re-measuring reliability of 0.75.
2.2.3. Young-Internet Addiction Test
A Chinese version of Young’s Internet Addiction Test (IAT-20) was used to measure IA [41,42]. In total, 20 items were rated on a 5-point scale, with one being “rarely” and five being “always,” and a final score was determined; the higher the total scores, the more prone an adolescent is to IA. The questionnaire is assessed based on the evaluation criteria of domestic researchers. A total score of <50 indicated no IA, and a total score of ≥50 indicated IA. The Cronbach’s α coefficient for this questionnaire was 0.90 [41,43].
2.2.4. The Self-Rating Scale of Systematic Family Dynamics, Revised Version
The Self-rating Scale of Systematic Family Dynamics, revised version (SSFD), was compiled by Zhao et al. [44], based on Heidelberg’s systematic family dynamics theory combined with the Chinese cultural background. The self-assessment questionnaire was revised and republished in 2014 [44]. This questionnaire includes the following four dimensions: family atmosphere (FA, eight items), individualized (IN, six items), systematic logic (SL, five items), and illness concept (IC, four items), totaling 23 items. Each item was scored on a 5-point scale: 1 = completely disagree; 2 = very much disagree; 3 = partially agree; 4 = very much agree; and 5= completely agree. There were both positive and negative items on the scale. The higher the positive item score, the more positive the item; the higher the negative item score, the less positive the item. Cronbach’s α and split-half correlation coefficients were 0. 79 and 0. 84, respectively [44].
2.2.5. Family Assessment Device
According to the McMaster family function model, the Family Assessment Device (FAD) scale includes seven subscales. This study used the general function subscale (GF) and behavior control subscale (BC). The GF consists of 12 self-report items, and the BC consists of 9 items. Each item is rated as strongly agree, agree, disagree, or completely disagree. The corresponding scores range from 1 to 4, and the Starred items were reversely scored. In this study, the higher the scale score, the less healthy the family function. Additionally, the FAD has demonstrated good reliability and validity in Chinese children over 12 years old [45]. The Cronbach’s α coefficient of BC is 0.71, and the correlation coefficient is greater than 0.5 [45].
2.2.6. Self-Rating Anxiety Scale
The self-rating anxiety scale (SAS) compiled by Zung in 1971 reflects subjective feelings of anxiety, with a total of 20 items. The scores are summed to obtain a raw score, standardized to a cut-off of 50. Individuals with scores ≥50 were considered anxious, and those with scores <50 had no anxiety [45]. The Cronbach’s α and correlation coefficients of SAS were 0.697 and 0.777, respectively [46].
2.2.7. Self-Rating Depression Scale
The self-rating depression scale (SDS) was developed by Zung (1965) [45]. The questionnaire has 20 items that are scored using a 4-point Likert scale to evaluate depression. The sum of the raw scores ranges from 20 to 80. The cut-off after standardization is 53 points; therefore, scores more than or equal to 53 points indicate depression and those less than 53 points indicate no depression [45]. The Cronbach’s α and correlation coefficients of the SDS are r.73 and 0.84, respectively [45].
2.3. Statistical Analyses
Data were analyzed using IBM SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, NY, USA). First, we coded the options for each categorical variable in Table 1. Second, Pearson’s chi-square test was used to analyze the differences in IA rates between the groups. Third, Pearson’s bivariate correlation analysis was used to analyze the correlation between IA and other variables. Finally, a regression analysis of the chain-mediation model was performed using PROCESS Macro for SPSS 3.3 [47], using Model 6 with 5000 bias-corrected bootstrap samples. Statistical significance was determined using a p-value of 0.05. Indirect effects were analyzed at a significance level of 0.05. If the bootstrap 95% confidence intervals (Cis) that do not include zero indicate significant effects at α = 0.05 [47].

Table 1.
Comparison of the differences in the prevalence of Internet addiction between groups.
2.4. Ethics
The present study was approved by the Ethical Committee of the Mental Health Center affiliated with Tongji University in Shanghai (No. PDJWLL2019008). Informed consent was obtained from all participants, including those younger than 18.
3. Results
3.1. Differences in the Prevalence of Internet Addiction among Adolescents according to Their Demographic Characteristics
The descriptive statistics of all participants with or without IA and their respective p values were presented in Table 1. The average age of 3357 young adults was 13.69 years (SD = 2.06). The prevalence of IA among adolescents was 26.2%. The following variables showed statistically significant intergroup differences in the prevalence of IA: whether the adolescent was a single-child or not, grades, parental preference for children, parental education level, parental marital quality, self-assessment of whether internet use is out of control, presence or absence of childhood trauma, and presence or absence of anxiety and depression. There were significant correlations between IA and the following variables: being a single child or not, schooling grade, parental preference of children, parental education level, parental marital quality, and satisfaction with family economic status, which were subsequently used as control variables for the regression analysis.
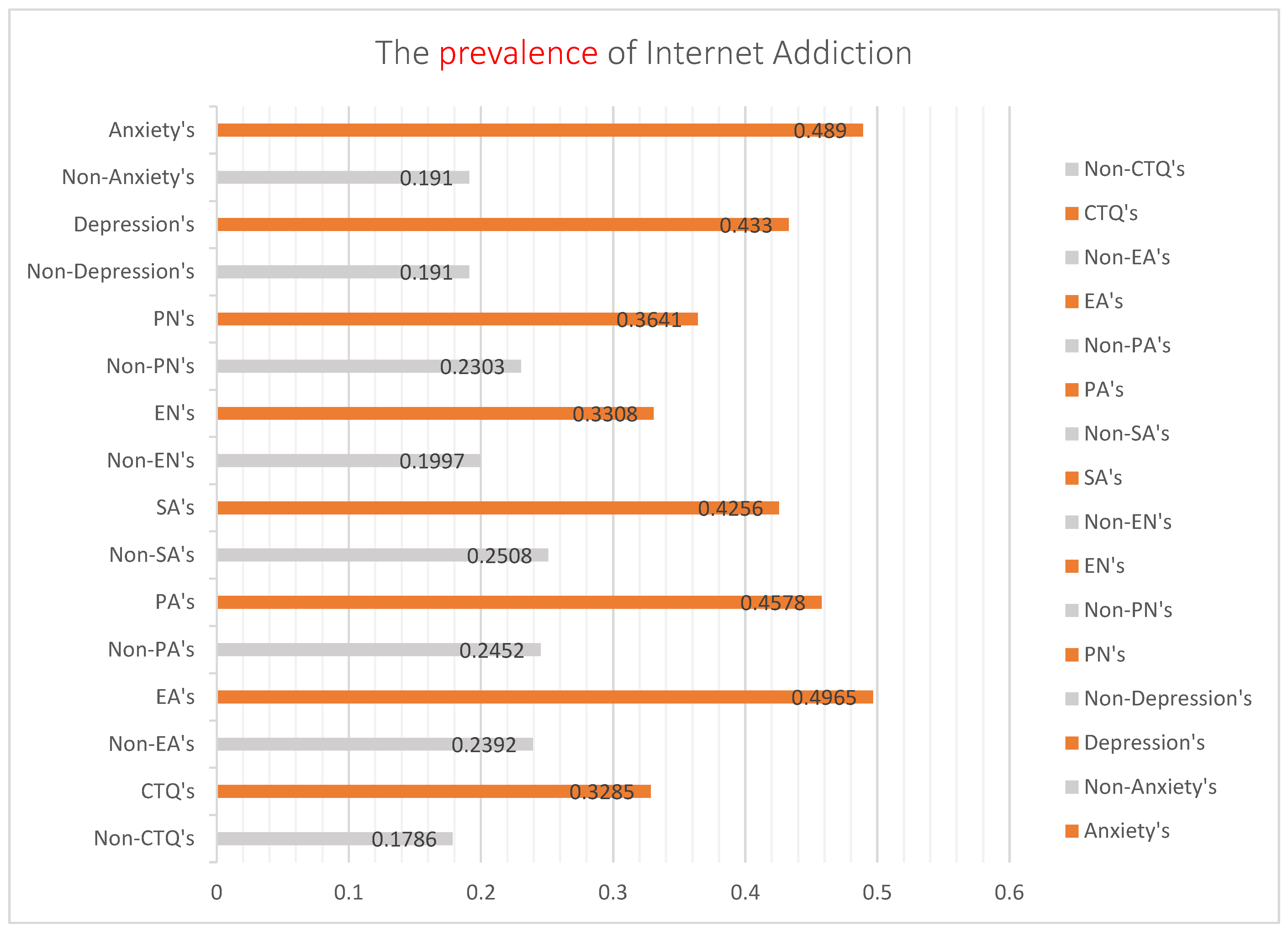
3.2. Internet Addiction in Adolescents with Childhood Trauma, Anxiety, or Depression
In this study, the prevalence of childhood trauma was 55.0% (59.1% of boys and 51.0% of girls), and the difference between the sexes was statistically significant (χ2 = 22.012, ν = 1, p = 0.000). However, the difference in IA prevalence was not statistically significant (χ2 = 0.105, ν = 1, p = 0.746). The prevalence of IA among adolescents with childhood trauma was 32.85%, significantly different from that among adolescents without childhood trauma (17.86%; χ2 = 96.801, ν = 1, p = 0.025 > 0.05). The prevalence of depression and anxiety in adolescents was 29.1% and 23.7%, respectively. The prevalence of IA in adolescents with childhood trauma according to the five types of traumas and negative emotions shown in Figure 1. The prevalence of IA or adverse emotions in adolescents with childhood trauma was significantly higher than the those without childhood trauma or emotional disorders.
Figure 1.
Cluster bar graph analysis of the prevalence of Internet addiction among adolescents with or without childhood trauma, anxiety, or depression. Note: Non-CTQ’s = None childhood trauma. CTQ’s = With childhood trauma. Non-EA’s = None emotion abuse. EA’s = With emotion abuse. Non-PA’s = None physical abuse. PA’s = With physical abuse. Non-SA’s = None Sexual abuse. SA’s = With Sexual abuse. Non-EN’s = None emotion neglect. EN’s = With emotion neglect. Non-PN’s = None physical neglect. PN’s = With physical neglect.
3.3. Correlations between Internet Addiction in Adolescents and Other Variables
Pearson’s correlation analysis showed a significant positive correlation between the IAT-20 scores and the SAS, SDS, the five CTQ-28 subscales, GF, and BC scores (Table 2). There was a significant negative correlation between the IAT-20 scores and all the SSFD dimension scores, except the IC scores. The correlation coefficients were more than 0.7 for the following variables: SAS and SDS, FA and IN or SSFD, IN and SSFD, and IC and IN or SSFD, 0.708, 0.703, 0.793, 0.825, and 0.720, respectively.

Table 2.
Correlation analysis between the total scores of IAT-20 and SAS, SDS, CTQ-28, SSFD, and FAD.
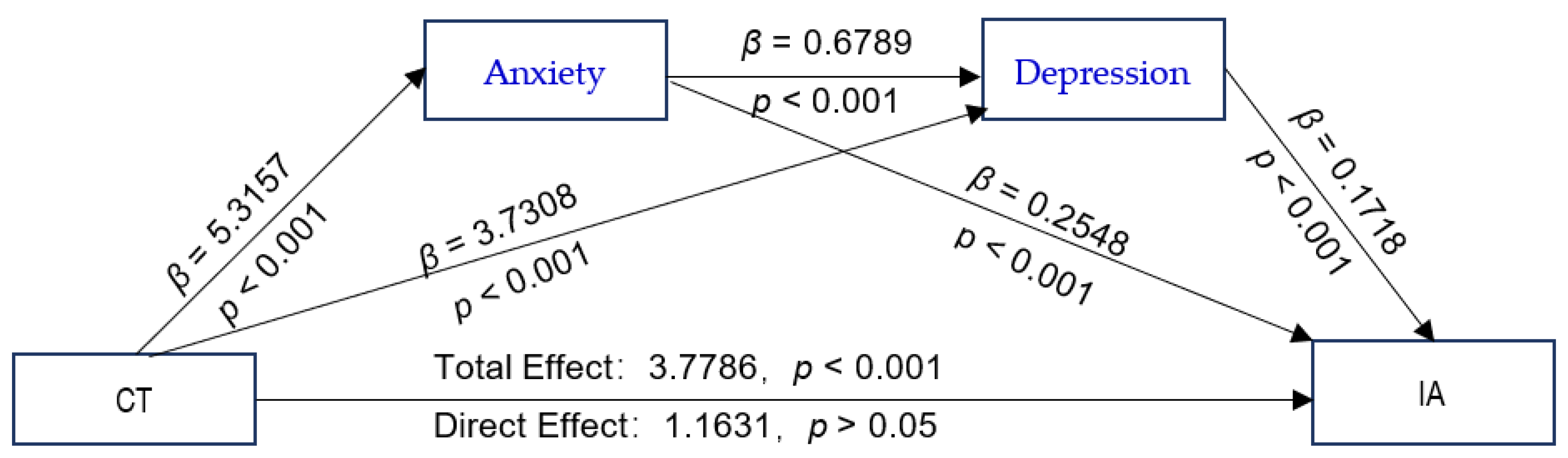
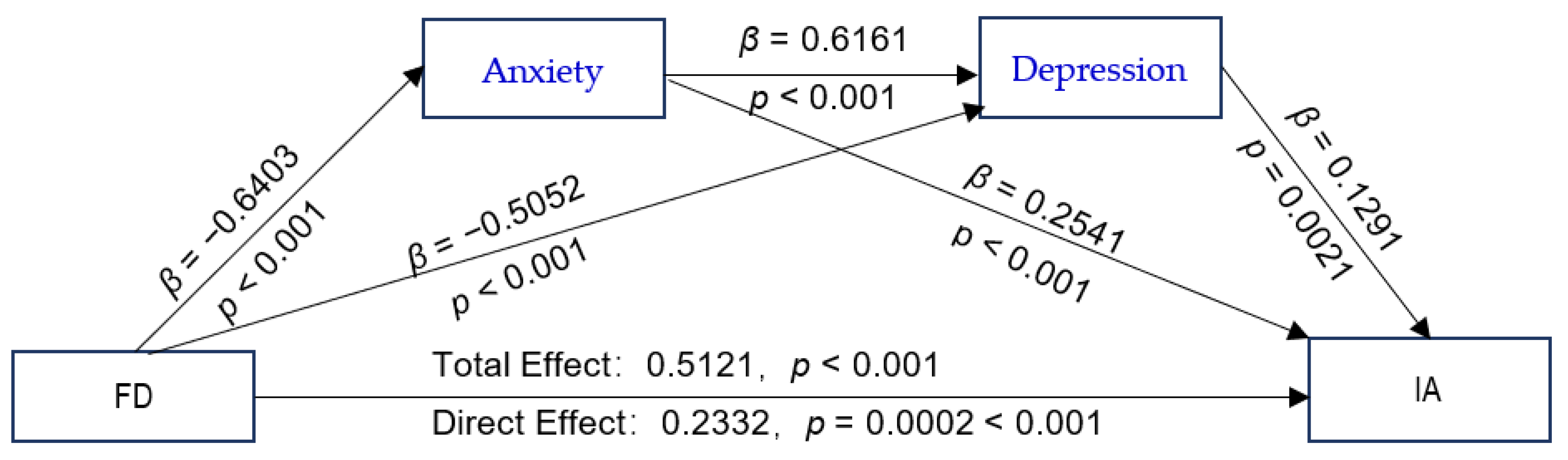
3.4. Childhood Trauma and Poor Family Functioning as Predictors of IA
The proposed chain-mediated model (Model 6) was tested, with CTQ-28 total scores and GF scores as independent variables; IAT-20 scores as the dependent variable; anxiety and depression as mediating variables; and schooling grade, whether or not the adolescent is a single child, parental preference, parental education level, and parental marital quality as control variables. The results of the path coefficients are shown in Figure 2 and Figure 3. The CTQ-28 total scores were positive predictors of the SAS and SDS scores (Figure 2). The values with their bootstrap 95% CI are presented as following: CTQ-28 total scores as predictors of SAS scores: β = 5.3157, bootstrap 95% CI (4.2278, 6.4036); CTQ-28 total scores as predictors of SDS scores: β = 3.7308, bootstrap 95% CI (2.8393, 4.6222); GF as positive predictors of SAS: β = 0.6403, bootstrap 95% CI (0.5558, 0.7248) (Figure 3); and GF scores as positive predictors of SDS scores: β = 0.5052, bootstrap 95% CI (0.4324, 0.5780). All the bootstrap 95% CIs did not contain 0, verifying that Hypothesis 2 is true. The analysis of the direct effects of the CTQ-28 total scores on the IAT-20 scores was not significant (β = 1.1631, p > 0.05). However, the indirect effect of CTQ-28 total scores on IAT-20 scores was significant (β = 2.6155, p < 0.001), indicating a fully mediated effect, which verifies that Hypothesis 3 is true. The total effect of the CTQ-28 total scores on the IAT-20 scores was significant (β = 3.7786, p < 0.001). The direct effect of GF scores on the IAT-20 scores was significant (β = 0.2332, p = 0.0002 < 0.001), and the indirect effect via the SAS and SDS scores were also significant (β = 0.2789, p < 0.001). There was a partial mediating effect via the chain effect of the SAS and SDS scores, verifying that Hypothesis 3 is true. The total effect value of the GF scores on the IAT-20 scores was significant (β = 0.5121, p < 0.001), demonstrating that Hypothesis 1 is true.
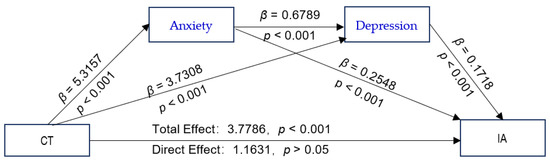
Figure 2.
The chain-mediated model predicting adolescents’ IA based on the experience of childhood trauma mediated by anxiety and depression. Abbreviations: CT, childhood trauma; IA, Internet addiction.
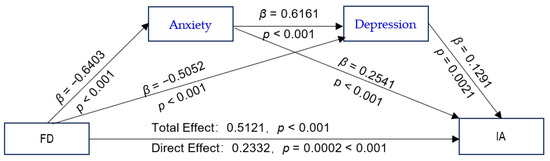
Figure 3.
The chain-mediated model predicting adolescents’ Internet addiction based on family dysfunction mediated by anxiety and depression. Abbreviations: FD, family dysfunction; IA, Internet addiction.
The mediating effect of the CTQ-28 total scores on the IAT-20 scores via the SAS and SDS scores was significant (R2 = 0.1992, F [8, 1456] = 45.2615, p < 0.001). The results obtained after bootstrapping showed the indirect effect of anxiety and depression (β = 2.6155; 95% CI = [1.9555, 3.3105]; (Table 3), and there was no significant difference in the effect size between the three pathways.

Table 3.
The chain-mediated effects of childhood trauma on Internet addiction and bias-corrected 95% confidence intervals.
The GF scores were positive predictors of the IAT-20 scores via the SAS and SDS scores, and the regression equation was significant (R2 = 0.2270, F [8, 1446] = 53.0771, p < 0.001). Furthermore, as shown in Table 4, our analysis indicates an indirect effect of anxiety and depression (β = 0.2789; 95% CI = [0.2068, 0.3544]). Among the three pathways, the indirect effect via the SAS scores was larger than that via the SAS–SDS scores (β = 0.1118, bootstrap 95% CI = [0.0231, 0.2089]); the CI value interval did not contain 0, and the effect difference was significant.

Table 4.
The chain-mediated effects of family dysfunction on Internet addiction and bias-corrected 95% confidence intervals.
4. Discussion
4.1. The Variability of Internet Addiction Prevalence with Different Demographic Characteristics among Adolescents
The prevalence of IA among adolescents in the study was 26.2%, which is higher than that (16.5%) reported by Linyuan et al. (2021) [48]. Many current studies have shown that boys are prone to IA and have also said that the prevalence of IA among boys is higher than that among girls [2,35,49]. The differences in IA’s prevalence between genders were insignificant, possibly due to the different ways different genders use the Internet. The 49th China Internet Survey (2022) showed that underage netizens use the Internet for applications such as search engines, social networking sites, news and information, shopping, short videos, animation, and comics [3]. This study showed that the prevalence of adolescent IA was significantly associated with childhood trauma, anxiety and depression, and family dysfunction (poor parental marital quality, low family atmosphere, high family behavioral control, etc.). The poorer the parents’ marriage quality, the higher the prevalence of IA. Frequent and violent conflicts between parents are major factors that lead to family dysfunction, which can cause increased psychological stress or trauma to children in the family. Research has shown that parental marital conflict is a risk factor for adolescent IA [50,51,52]. the prevalence of IA in adolescents with childhood trauma was almost twice as high as the prevalence without childhood trauma. The prevalence of IA in adolescents with anxiety and depression was about 2.5 times higher than that without mood disorders. The worst the family functions, the higher the prevalence of IA in adolescents. Chen et al. (2020) [52] found that terrible family functions can lead children to become involved in the virtual world for temporary emotional support and a sense of belonging.
4.2. Effects of Childhood Trauma on Internet Addiction in Adolescents
According to the present study, boys were more likely to experience childhood trauma than that experienced by girls, and there was no significant difference in the prevalence of IA between the sexes. The prevalence of anxiety and depression was higher in girls than boys, with a substantial difference between the two sexes. Figure 1 shows the association of the prevalence of IA with different emotional disorders and traumatic experiences. The prevalence of IA with emotional abuse and anxiety was the highest. According to the chain-mediated effect results obtained using Process Macro Model 6 (Figure 2), childhood trauma has no direct positive predictive effect on IA but has a significant positive predictive effect on anxiety or depression. Anxiety and depression had significant positive predictive effects on IA. Moreover, childhood trauma and adverse emotions were positively associated with IA. As reported by other researchers, this study showed that anxiety and depression could increase the positive predictive effect of childhood trauma on IA [26,27,53]. Similar to many studies, childhood trauma is a risk factor for emotional dysregulation in adolescents, which further exacerbates the development of IA in adolescents [54,55,56].
4.3. Poor Family Functioning as a Predictor of Adolescent IA
According to the correlation analysis, the GF and BC scores were significantly correlated in instances where inappropriate control behaviors in the family could damage family functioning. GF scores were negatively correlated with each dimension of the SSFD scores, especially the FA scores. Higher FA scores indicated a more relaxed and pleasant FA, higher GF scores indicated unhealthy family functioning, and poor family functioning was associated with poor FA. The correlations between GF scores and SAS, SDS, and IAT-20 scores were significant, indicating that the less healthy the family functioning, the more likely adolescents are prone to anxiety, depression, and IA, as suggested by Ma (2021) [57] and Chen et al., (2020) [6] that poor family functioning is a risk factor for adolescent mood disorders. Through chain-mediated path analysis, poor family functioning showed a significant positive predictive effect on adolescents’ IA. In addition, poor family functioning is a risk predictor of adolescent emotional disorders. As suggested by Marzilli et al. (2020) [58], symptoms of negative emotions can directly increase the risk of IA, and anxiety and depression are strong risk predictors of IA. In this study, poor family functioning showed an increased risk-predictive effect on adolescents’ IA through the indirect mediated pathway of anxiety and depression. This result was also consistent with previous studies that have shown that a poor family environment is an important risk factor for IA [31,32,33,36,55].
4.4. Limitations and Directions for Future Research
There were some limitations as it is a cross-sectional survey in this study. First, although the questionnaires used in this survey had good reliability and validity, accuracy could not be ensured because the information was collected exclusively through self-reporting, and the researcher did not interview the participants. Second, experiences of childhood trauma, experiences of anxiety and depression, systematic family dynamics, and family functioning are subject to constant change; therefore, it is difficult to establish an accurate correlation between each of these variables and IA, despite accounting for control factors during the analysis. To improve the accuracy of the survey results, the primary guardians of the youth could be surveyed simultaneously in a future study. Finally, since we were not adjusting our analyses, there was also a chance for a residual confounding bias in this study. In the follow-up study, we may consider restricting the selection of study subjects for possible confounding factors to obtain homogeneous study subjects as much as possible. Still, the representativeness of the study subjects may be affected to some extent, in addition to using randomization to select study subjects to reduce confounding bias as much as possible.
5. Conclusions
Anxiety and depression significantly mediate the impact of childhood trauma and poor family functioning on IA in adolescents. Traumatic childhood experiences increase the risk of developing anxiety and depression in adolescents. Furthermore, anxiety and depression were significantly correlated with IA, and childhood trauma was positively associated with adolescent IA. Poor family functioning is a direct risk predictor of IA in adolescents. In addition, poor family functioning enhances the risk prediction of IA in adolescents by significantly increasing the likelihood of suffering from anxiety and depression. This conclusion provides the basis and direction for developing prevention strategies, interventions, and treatment measures for adolescent anxiety, depression, and IA from childhood. These developments should be aimed at improving the family environment in which adolescents grow up, reducing possible childhood traumas, and improving adolescents’ knowledge of the family concept, thereby reducing the prevalence of adolescents’ negative emotions and IA.
Author Contributions
Conceptualization, M.H. and X.Z.; Data curation, M.H., L.X., W.Z. and T.Z.; Formal analysis, Z.A.; Funding acquisition, M.H. and X.Z.; Investigation, M.H. and X.Z.; Methodology, M.H. and Z.A.; Project administration, M.H.; Resources, L.X., W.Z. and Q.W.; Software, Q.W. and Z.A.; Supervision, X.Z.; Writing—original draft, M.H.; Writing—review & editing, M.H. and X.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research was granted from the Foundation of the Shanghai Municipal Commission of Health and Family Planning, grant number (201940161), and Medical Discipline Construction Project of Pudong Health Committee of Shanghai, grant number [PWYgy2021-02].
Institutional Review Board Statement
The study was approved by the Ethical Committee of the Mental Health Center affiliated with Tongji University in Shanghai (No. PDJWLL2019008).
Informed Consent Statement
Informed consent was obtained from all participants, including those younger than 18.
Data Availability Statement
Based on informed consent, the data involved in this study are for use in this project only.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kuss, D.J.; Billieux, J. Technological addictions: Conceptualisation, measurement, etiology and treatment. Addict. Behav. 2017, 64, 231–233. [Google Scholar] [CrossRef] [PubMed]
- Lozano-Blasco, R.; Robres, A.Q.; Sánchez, A.S. Internet addiction in young adults: A meta-analysis and systematic review. Comput. Hum. Behav. 2022, 130, 107201. [Google Scholar] [CrossRef]
- State Internet Information Office of the People’s Republic of China. The 49th Statistical Report on the Development of the Internet in China. China Internet Network Information Center. 2022. Available online: http://www.cnnic.net.cn/NMediaFile/old_attach/P020220721404263787858.pdf (accessed on 25 February 2022).
- Martins, M.V.; Formiga, A.; Santos, C.; Sousa, D.; Resende, C.; Campos, R.; Nogueira, N.; Carvalho, P.; Ferreira, S. Adolescent internet addiction—Role of parental control and adolescent behaviours. Int. J. Pediatr. Adolesc. Med. 2020, 7, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Fineberg, N.; Demetrovics, Z.; Stein, D.; Ioannidis, K.; Potenza, M.; Grünblatt, E.; Brand, M.; Billieux, J.; Carmi, L.; King, D.; et al. Manifesto for a European research network into Problematic Usage of the Internet. Eur. Neuropsychopharmacol. 2018, 28, 1232–1246. [Google Scholar] [CrossRef]
- Chen, H.-C.; Wang, J.-Y.; Lin, Y.-L.; Yang, S.-Y. Association of Internet Addiction with Family Functionality, Depression, Self-Efficacy and Self-Esteem among Early Adolescents. Int. J. Environ. Res. Public Health 2020, 17, 8820. [Google Scholar] [CrossRef]
- Chung, S.; Lee, J.; Lee, H.K. Personal Factors, Internet Characteristics, and Environmental Factors Contributing to Adolescent Internet Addiction: A Public Health Perspective. Int. J. Environ. Res. Public Health 2019, 16, 4635. [Google Scholar] [CrossRef]
- Bernstein, D.P.; Stein, J.A.; Newcomb, M.D.; Walker, E.; Pogge, D.; Ahluvalia, T.; Stokes, J.; Handelsman, L.; Medrano, M.; Desmond, D.; et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abus. Negl. 2003, 27, 169–190. [Google Scholar] [CrossRef]
- Hurd, Y.L.; Michaelides, M.; Miller, M.L.; Jutras-Aswad, D. Trajectory of adolescent cannabis use on addiction vulnerability. Neuropharmacology 2014, 76, 416–424. [Google Scholar] [CrossRef]
- Ignat, S.; Galutiu, C. Internet Dependence/Social Networks and the Development of Teenage Social Anxiety. Agora Psycho-Pragmatica 2022, 15. Available online: https://www.uav.ro/jour/index.php/app/article/view/1684/1692 (accessed on 26 January 2022).
- Jimeno, M.V.; Ricarte, J.J.; Toledano, A.; Mangialavori, S.; Cacioppo, M.; Ros, L. Role of Attachment and Family Functioning in Problematic Smartphone Use in Young Adults. J. Fam. Issues 2022, 43, 375–391. [Google Scholar] [CrossRef]
- Kanacri, B.P.L.; Pastorelli, C.; Eisenberg, N.; Zuffianò, A.; Castellani, V.; Caprara, G.V. Trajectories of prosocial behavior from adolescence to early adulthood: Associations with personality change. J. Adolesc. 2014, 37, 701–713. [Google Scholar] [CrossRef] [PubMed]
- Kurniasanti, K.S.; Assandi, P.; Ismail, R.I.; Nasrun, M.W.S.; Wiguna, T. Internet addiction: A new addiction? Med. J. Indones. 2019, 28, 82–91. [Google Scholar] [CrossRef]
- Truong, A.; Moukaddam, N.; Toledo, A.; Onigu-Otite, E. Addictive Disorders in Adolescents. Psychiatr. Clin. North Am. 2017, 40, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Dieris-Hirche, J.; Bottel, L.; Bielefeld, M.; Steinbüchel, T.; Kehyayan, A.; Dieris, B.; Wildt, B.T. Media use and Internet addiction in adult depression: A case-control study. Comput. Hum. Behav. 2017, 68, 96–103. [Google Scholar] [CrossRef]
- Khubchandani, J.; Sharma, S.; Price, J.H. COVID-19 Pandemic and the Burden of Internet Addiction in the United States. Psychiatry Int. 2021, 2, 402–409. [Google Scholar] [CrossRef]
- Kuss, D.; Griffiths, M.; Karila, L.; Billieux, J. Internet Addiction: A Systematic Review of Epidemiological Research for the Last Decade. Curr. Pharm. Des. 2014, 20, 4026–4052. [Google Scholar] [CrossRef]
- Kuss, D.J.; Kristensen, A.M.; Lopez-Fernandez, O. Internet addictions outside of Europe: A systematic literature review. Comput. Hum. Behav. 2021, 115, 106621. [Google Scholar] [CrossRef]
- Young, K.S.; Rogers, R.C. The Relationship between Depression and Internet Addiction. Cyberpsychol. Behav. 1998, 1, 25–28. [Google Scholar] [CrossRef]
- Xu, L.; Kuang, L.; Huang, Y.; Wang, W.; Cao, J.; Xiao, M.-N. Abnormal brain activity in adolescents with Internet addiction who attempt suicide: An assessment using functional magnetic resonance imaging. Neural Regen. Res. 2020, 15, 1554–1559. [Google Scholar] [CrossRef]
- Ma, S.; Huang, Y.; Ma, Y. Childhood Maltreatment and Mobile Phone Addiction among Chinese Adolescents: Loneliness as a Mediator and Self-Control as a Moderator. Front. Psychol. 2020, 11, 813. [Google Scholar] [CrossRef]
- Wei, L.; Han, X.; Yu, X.; Sun, Y.; Ding, M.; Du, Y.; Jiang, W.; Zhou, Y.; Wang, H. Brain controllability and morphometry similarity of internet gaming addiction. Methods 2021, 192, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Petry, N.M.; O’Brien, C.P. Internet gaming disorder and the DSM-5. Addiction 2013, 108, 1186–1187. [Google Scholar] [CrossRef] [PubMed]
- Gur, K.; Yurt, S.; Bulduk, S.; Atagöz, S. Internet addiction and physical and psychosocial behavior problems among rural secondary school students. Nurs. Health Sci. 2015, 17, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Lindenberg, K.; Halasy, K.; Schoenmaekers, S. A randomized efficacy trial of a cognitive-behavioral group intervention to prevent Internet Use Disorder onset in adolescents: The PROTECT study protocol. Contemp. Clin. Trials Commun. 2017, 6, 64–71. [Google Scholar] [CrossRef]
- Afifi, T.O.; Taillieu, T.; Salmon, S.; Stewart-Tufescu, A.; Struck, S.; Fortier, J.; MacMillan, H.L.; Sareen, J.; Tonmyr, L.; Katz, L.Y. Protective Factors for Decreasing Nicotine, Alcohol, and Cannabis Use Among Adolescents with a History of Adverse Childhood Experiences (ACEs). Int. J. Ment. Health Addict. 2022, 715. [Google Scholar] [CrossRef]
- Geng, J.; Bao, L.; Wang, H.; Wang, J.; Gao, T.; Lei, L. Does childhood maltreatment increase the subsequent risk of problematic smartphone use among adolescents? A two-wave longitudinal study. Addict. Behav. 2022, 129, 107250. [Google Scholar] [CrossRef]
- Stoltenborgh, M.; Bakermans-Kranenburg, M.J.; Alink, L.R.A.; van Ijzendoorn, M.H. The Prevalence of Child Maltreatment across the Globe: Review of a Series of Meta-Analyses. Child Abus. Rev. 2015, 24, 37–50. [Google Scholar] [CrossRef]
- Hagborg, J.M.; Tidefors, I.; Fahlke, C. Gender differences in the association between emotional maltreatment with mental, emotional, and behavioral problems in Swedish adolescents. Child Abus. Negl. 2017, 67, 249–259. [Google Scholar] [CrossRef]
- Wu, C.-H.; Griffin, M.; Parker, S. Developing agency through good work: Longitudinal effects of job autonomy and skill utilization on locus of control. J. Vocat. Behav. 2015, 89, 102–108. [Google Scholar] [CrossRef]
- Shek, D.T.; Yu, L. Adolescent Internet Addiction in Hong Kong: Prevalence, Change, and Correlates. J. Pediatr. Adolesc. Gynecol. 2016, 29, S22–S30. [Google Scholar] [CrossRef]
- Yu, C.; Zhang, W.; Zeng, Y.; Ye, T.; Hu, J.; Li, D. Gratitude, basic psychological needs, and problematic Internet use in adolescence. Psychol. Dev. Educ. 2012, 28, 83–90. [Google Scholar] [CrossRef]
- Dai, L.; Wang, L. Review of Family Functioning. Open J. Soc. Sci. 2015, 3, 134–141. [Google Scholar] [CrossRef]
- Tariq, I.; Majeed, S. Poor Family-Functioning and Lack of Interpersonal Support as Predictors of Online Gaming Addiction in Adolescents. J. Prof. Appl. Psychol. 2022, 3, 53–68. [Google Scholar] [CrossRef]
- Zhang, L.; Ma, X.; Yu, X.; Ye, M.; Li, N.; Lu, S.; Wang, J. Childhood Trauma and Psychological Distress: A Serial Mediation Model among Chinese Adolescents. Int. J. Environ. Res. Public Health 2021, 18, 6808. [Google Scholar] [CrossRef]
- Casaló, L.V.; Escario, J.-J. Predictors of excessive internet use among adolescents in Spain: The relevance of the relationship between parents and their children. Comput. Hum. Behav. 2019, 92, 344–351. [Google Scholar] [CrossRef]
- Dong, B.; Zhao, F.; Wu, X.-S.; Wang, W.-J.; Li, Y.-F.; Zhang, Z.-H.; Sun, Y.-H. Social Anxiety May Modify the Relationship Between Internet Addiction and Its Determining Factors in Chinese Adolescents. Int. J. Ment. Health Addict. 2019, 17, 1508–1520. [Google Scholar] [CrossRef]
- Lukavská, K.; Vacek, J.; Gabhelík, R. The effects of parental control and warmth on problematic internet use in adolescents: A prospective cohort study. J. Behav. Addict. 2020, 9, 664–675. [Google Scholar] [CrossRef]
- Shi, X.; Wang, J.; Zou, H. Family functioning and Internet addiction among Chinese adolescents: The mediating roles of self-esteem and loneliness. Comput. Hum. Behav. 2017, 76, 201–210. [Google Scholar] [CrossRef]
- Zhao, X.F.; Zhang, Y.L.; Li, L.F.; Zhou, Y.F.; Li, H.Z.; Yang, S.C. Reliability and validity of the Chinese version of the Childhood Abuse Questionnaire. J. Chin. J. Clin. Rehabilitation. 2005, 9, 105–107. Available online: http://www.cnki.com.cn/Article/CJFDTOTAL-XDKF200520049.htm (accessed on 28 May 2005).
- Shu, Y.M.; Ivan Jacob, A.P.; Zhang, M.X.; Wu, A.M.S. Psychometric validation of the Internet Gaming Disorder-20 Test among Chinese middle school and university students. J. Behav. Addict. 2019, 8, 295–305. [Google Scholar] [CrossRef]
- Young, K.S. Clinical Assessment of Internet-Addicted Clients. In Internet Addiction: A Handbook and Guide to Evaluation and Treatment; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2007; pp. 19–34. [Google Scholar] [CrossRef]
- Dong, X.L. A Study on Internet Addiction and Its Related Factors among High School Students. Master’s Thesis, Fudan University, Shanghai, China, 2008. Available online: https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD2009&filename=2009018992.nh (accessed on 2 June 2008).
- Yu, L.; Zhao, X.D.; Zeng, W.N.; Tan, J.F.; Yu, Y.L.; Zeng, J.Y.; Wan, C.H. Reliability and validity analysis of the revised version of the Systematic Family Dynamics Self-Assessment Scale in a test of Guangdong students. China Health Stat. 2014, 31, 979–981. Available online: http://www.cqvip.com/qk/94022x/201406/663531902.html (accessed on 25 December 2014).
- Wang, X.D.; Wang, X.L.; Ma, H. Handbook of Mental Health Assessment Scales. China J. Ment. Health Beijing 1999, 12. [Google Scholar]
- Wang, F.F. Testing of anxiety self-rating scales in secondary school students. Chin. Sch. Health 1994, 15, 202–203. Available online: http://www.cqvip.com/qk/96360a/199403/1571945.html (accessed on 20 June 1994).
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis; Methodology in the Social Sciences; The Guilford Press: London, UK, 2013; p. 193. [Google Scholar]
- Deng, L.Y.; Wang, Y.Q.; Yang, Y.M.; Zhou, L.; Li, B.L. Parental Anxiety/Depression and Teenagers’ Phone and Tablet Addiction Under the COVID-19: A Chain Mediation Model. Chin. J. Clin. Psychol. 2021, 29, 1230–1236. [Google Scholar] [CrossRef]
- Zhang, Q.; Wang, C.; Yuan, C.Y.; Zhang, X.H.; Li, Y.J. A gender effect study on the relationship between Internet addiction and adolescent adverse emotional behavior. Chin. J. Clin. Psychol. 2014, 22, 1004–1009. [Google Scholar]
- Gao, T.; Meng, X.; Qin, Z.; Zhang, H.; Gao, J.; Kong, Y.; Hu, Y.; Mei, S. Association between parental marital conflict and Internet addiction: A moderated mediation analysis. J. Affect. Disord. 2018, 240, 27–32. [Google Scholar] [CrossRef]
- Zhang, H.; Spinrad, T.L.; Eisenberg, N.; Luo, Y.; Wang, Z. Young adults’ internet addiction: Prediction by the interaction of parental marital conflict and respiratory sinus arrhythmia. Int. J. Psychophysiol. 2017, 120, 148–156. [Google Scholar] [CrossRef]
- Zheng, X.; Chen, J.; Guo, Y.; Xiong, Q.; Hu, Y.; Shi, S.; Li, C.; Yu, Q. The buffer effect of physical activity: Why does parental marital satisfaction affect adolescents’ problematic Internet use. Addict. Behav. Rep. 2020, 11, 100271. [Google Scholar] [CrossRef]
- Noll, J.G.; Haag, A.-C.; Shenk, C.E.; Wright, M.F.; Barnes, J.E.; Kohram, M.; Malgaroli, M.; Foley, D.J.; Kouril, M.; Bonanno, G.A. An observational study of Internet behaviours for adolescent females following sexual abuse. Nat. Hum. Behav. 2022, 6, 74–87. [Google Scholar] [CrossRef]
- Arslan, G. Psychological maltreatment, forgiveness, mindfulness, and internet addiction among young adults: A study of mediation effect. Comput. Hum. Behav. 2017, 72, 57–66. [Google Scholar] [CrossRef]
- Bland, V.J.; Lambie, I.; Best, C. Does childhood neglect contribute to violent behavior in adulthood? A review of possible links. Clin. Psychol. Rev. 2018, 60, 126–135. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Zhang, R.; Zhornitsky, S.; Le, T.M.; Wang, W.; Li, C.-S.R.; Zhang, S. Depression Mediates the Relationship between Childhood Trauma and Internet Addiction in Female but Not Male Chinese Adolescents and Young Adults. J. Clin. Med. 2021, 10, 5015. [Google Scholar] [CrossRef] [PubMed]
- Ma, X. The Effect of Family Functioning on Depression in Secondary School Students. Master’s Thesis, Tianjin Normal University, Tianjin, China, 2021. [Google Scholar] [CrossRef]
- Marzilli, E.; Cerniglia, L.; Ballarotto, G.; Cimino, S. Internet Addiction among Young Adult University Students: The Complex Interplay between Family Functioning, Impulsivity, Depression, and Anxiety. Int. J. Environ. Res. Public Health 2020, 17, 8231. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).