The Associations between Upper and Lower Body Muscle Strength and Diabetes among Midlife Women
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Handgrip Strength (HGS) and 5-Repetition Chair Stand Test (RCS)
2.3. Muscle Strength Index (MSI)
2.4. Definition of Diabetes Status
2.5. Sociodemographic, Reproductive, and Lifestyle Factors
2.6. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Association between HGS and Diabetes
3.3. Association between RCS and Diabetes
3.4. Association between Combined Muscle Strength Index (MSI) and Diabetes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- NCD Risk Factor Collaboration. Worldwide trends in diabetes since 1980: A pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016, 387, 1513–1530. [Google Scholar] [CrossRef] [Green Version]
- Chan, J.C.; Malik, V.; Jia, W.; Kadowaki, T.; Yajnik, C.S.; Yoon, K.H.; Hu, F.B. Diabetes in Asia: Epidemiology, risk factors, and pathophysiology. JAMA 2009, 301, 2129–2140. [Google Scholar] [CrossRef]
- Wong, L.Y.; Toh, M.P.; Tham, L.W. Projection of prediabetes and diabetes population size in Singapore using a dynamic Markov model. J. Diabetes 2017, 9, 65–75. [Google Scholar] [CrossRef] [Green Version]
- Bellou, V.; Belbasis, L.; Tzoulaki, I.; Evangelou, E. Risk factors for type 2 diabetes mellitus: An exposure-wide umbrella review of meta-analyses. PLoS ONE 2018, 13, e0194127. [Google Scholar] [CrossRef] [Green Version]
- Fletcher, B.; Gulanick, M.; Lamendola, C. Risk factors for type 2 diabetes mellitus. J. Cardiovasc. Nurs. 2002, 16, 17–23. [Google Scholar] [CrossRef]
- Chung, S.M.; Moon, J.S.; Chang, M.C. Prevalence of Sarcopenia and Its Association With Diabetes: A Meta-Analysis of Community-Dwelling Asian Population. Front. Med. 2021, 8, 681232. [Google Scholar] [CrossRef]
- Veronese, N.; Pizzol, D.; Demurtas, J.; Soysal, P.; Smith, L.; Sieber, C.; Strandberg, T.; Bourdel-Marchasson, I.; Sinclair, A.; Petrovic, M.; et al. Association between sarcopenia and diabetes: A systematic review and meta-analysis of observational studies. Eur. Geriatr. Med. 2019, 10, 685–696. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyere, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [Green Version]
- Giovannucci, E.L.; Rezende, L.F.M.; Lee, D.H. Muscle-strengthening activities and risk of cardiovascular disease, type 2 diabetes, cancer and mortality: A review of prospective cohort studies. J. Intern. Med. 2021, 290, 789–805. [Google Scholar] [CrossRef]
- Tarp, J.; Stole, A.P.; Blond, K.; Grontved, A. Cardiorespiratory fitness, muscular strength and risk of type 2 diabetes: A systematic review and meta-analysis. Diabetologia 2019, 62, 1129–1142. [Google Scholar] [CrossRef]
- Samson, M.M.; Meeuwsen, I.B.; Crowe, A.; Dessens, J.A.; Duursma, S.A.; Verhaar, H.J. Relationships between physical performance measures, age, height and body weight in healthy adults. Age Ageing 2000, 29, 235–242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maltais, M.L.; Desroches, J.; Dionne, I.J. Changes in muscle mass and strength after menopause. J. Musculoskelet. Neuronal Interact. 2009, 9, 186–197. [Google Scholar] [PubMed]
- Kunutsor, S.K.; Isiozor, N.M.; Khan, H.; Laukkanen, J.A. Handgrip strength-A risk indicator for type 2 diabetes: Systematic review and meta-analysis of observational cohort studies. Diabetes Metab. Res. Rev. 2021, 37, e3365. [Google Scholar] [CrossRef] [PubMed]
- Leong, D.P.; Teo, K.K.; Rangarajan, S.; Lopez-Jaramillo, P.; Avezum, A., Jr.; Orlandini, A.; Seron, P.; Ahmed, S.H.; Rosengren, A.; Kelishadi, R.; et al. Prognostic value of grip strength: Findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet 2015, 386, 266–273. [Google Scholar] [CrossRef]
- Celis-Morales, C.A.; Welsh, P.; Lyall, D.M.; Steell, L.; Petermann, F.; Anderson, J.; Iliodromiti, S.; Sillars, A.; Graham, N.; Mackay, D.F.; et al. Associations of grip strength with cardiovascular, respiratory, and cancer outcomes and all cause mortality: Prospective cohort study of half a million UK Biobank participants. BMJ 2018, 361, k1651. [Google Scholar] [CrossRef]
- Felicio, D.C.; Pereira, D.S.; Assumpcao, A.M.; de Jesus-Moraleida, F.R.; de Queiroz, B.Z.; da Silva, J.P.; de Brito Rosa, N.M.; Dias, J.M.; Pereira, L.S. Poor correlation between handgrip strength and isokinetic performance of knee flexor and extensor muscles in community-dwelling elderly women. Geriatr. Gerontol. Int. 2014, 14, 185–189. [Google Scholar] [CrossRef]
- Yeung, S.S.; Reijnierse, E.M.; Trappenburg, M.C.; Hogrel, J.-Y.; McPhee, J.S.; Piasecki, M.; Sipila, S.; Salpakoski, A.; Butler-Browne, G.; Pääsuke, M. Handgrip strength cannot be assumed a proxy for overall muscle strength. J. Am. Med. Dir. Assoc. 2018, 19, 703–709. [Google Scholar] [CrossRef]
- Buckinx, F.; Landi, F.; Cesari, M.; Fielding, R.A.; Visser, M.; Engelke, K.; Maggi, S.; Dennison, E.; Al-Daghri, N.M.; Allepaerts, S.; et al. Pitfalls in the measurement of muscle mass: A need for a reference standard. J. Cachexia Sarcopenia Muscle 2018, 9, 269–278. [Google Scholar] [CrossRef]
- Martin, H.J.; Yule, V.; Syddall, H.E.; Dennison, E.M.; Cooper, C.; Aihie Sayer, A. Is hand-held dynamometry useful for the measurement of quadriceps strength in older people? A comparison with the gold standard Bodex dynamometry. Gerontology 2006, 52, 154–159. [Google Scholar] [CrossRef]
- McCarthy, E.K.; Horvat, M.A.; Holtsberg, P.A.; Wisenbaker, J.M. Repeated chair stands as a measure of lower limb strength in sexagenarian women. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2004, 59, 1207–1212. [Google Scholar] [CrossRef]
- Vaz, M.M.; Costa, G.C.; Reis, J.G.; Junior, W.M.; Albuquerque de Paula, F.J.; Abreu, D.C. Postural control and functional strength in patients with type 2 diabetes mellitus with and without peripheral neuropathy. Arch. Phys. Med. Rehabil. 2013, 94, 2465–2470. [Google Scholar] [CrossRef] [PubMed]
- Castaneda-Sceppa, C.; Price, L.L.; Noel, S.E.; Bassett Midle, J.; Falcon, L.M.; Tucker, K.L. Physical function and health status in aging Puerto Rican adults: The Boston Puerto Rican Health Study. J. Aging Health 2010, 22, 653–672. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Forrest, K.Y.; Zmuda, J.M.; Cauley, J.A. Correlates of decline in lower extremity performance in older women: A 10-year follow-up study. J. Gerontol. A Biol. Sci. Med. Sci. 2006, 61, 1194–1200. [Google Scholar] [CrossRef] [Green Version]
- Thu, W.P.P.; Logan, S.J.S.; Lim, C.W.; Wang, Y.L.; Cauley, J.A.; Yong, E.L. Cohort Profile: The Integrated Women’s Health Programme (IWHP): A study of key health issues of midlife Singaporean women. Int. J. Epidemiol. 2018, 47, 389–390f. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roberts, H.C.; Denison, H.J.; Martin, H.J.; Patel, H.P.; Syddall, H.; Cooper, C.; Sayer, A.A. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardised approach. Age Ageing 2011, 40, 423–429. [Google Scholar] [CrossRef] [Green Version]
- Bellace, J.V.; Healy, D.; Besser, M.P.; Byron, T.; Hohman, L. Validity of the Dexter Evaluation System’s Jamar dynamometer attachment for assessment of hand grip strength in a normal population. J. Hand Ther. 2000, 13, 46–51. [Google Scholar] [CrossRef]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307. [Google Scholar] [CrossRef]
- Simonsick, E.M.; Newman, A.B.; Nevitt, M.C.; Kritchevsky, S.B.; Ferrucci, L.; Guralnik, J.M.; Harris, T.; The Health ABC Study Group. Measuring higher level physical function in well-functioning older adults: Expanding familiar approaches in the Health ABC study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M644–M649. [Google Scholar] [CrossRef] [Green Version]
- Bohannon, R.W. Test-retest reliability of the five-repetition sit-to-stand test: A systematic review of the literature involving adults. J. Strength Cond. Res. 2011, 25, 3205–3207. [Google Scholar] [CrossRef]
- Goldberg, A.; Chavis, M.; Watkins, J.; Wilson, T. The five-times-sit-to-stand test: Validity, reliability and detectable change in older females. Aging Clin. Exp. Res. 2012, 24, 339–344. [Google Scholar] [CrossRef]
- Ganasarajah, S.; Sundstrom Poromaa, I.; Thu, W.P.; Kramer, M.S.; Logan, S.; Cauley, J.A.; Yong, E.L. Objective measures of physical performance associated with depression and/or anxiety in midlife Singaporean women. Menopause 2019, 26, 1045–1051. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes, A. Diagnosis and classification of diabetes mellitus. Diabetes Care 2014, 37, S81–S90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bull, F.C.; Maslin, T.S.; Armstrong, T. Global physical activity questionnaire (GPAQ): Nine country reliability and validity study. J. Phys. Act. Health 2009, 6, 790–804. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pan, W.H.; Yeh, W.T. How to define obesity? Evidence-based multiple action points for public awareness, screening, and treatment: An extension of Asian-Pacific recommendations. Asia Pac. J. Clin. Nutr. 2008, 17, 370–374. [Google Scholar]
- Midi, H.; Sarkar, S.K.; Rana, S. Collinearity diagnostics of binary logistic regression model. J. Interdiscip. Math. 2010, 13, 253–267. [Google Scholar] [CrossRef]
- Nick, T.G.; Campbell, K.M. Logistic regression. Top. Biostat. 2007, 273–301. [Google Scholar] [CrossRef]
- LeBlanc, E.S.; Kapphahn, K.; Hedlin, H.; Desai, M.; Parikh, N.I.; Liu, S.; Parker, D.R.; Anderson, M.; Aroda, V.; Sullivan, S.; et al. Reproductive history and risk of type 2 diabetes mellitus in postmenopausal women: Findings from the Women’s Health Initiative. Menopause 2017, 24, 64–72. [Google Scholar] [CrossRef] [Green Version]
- Baliunas, D.O.; Taylor, B.J.; Irving, H.; Roerecke, M.; Patra, J.; Mohapatra, S.; Rehm, J. Alcohol as a risk factor for type 2 diabetes: A systematic review and meta-analysis. Diabetes Care 2009, 32, 2123–2132. [Google Scholar] [CrossRef] [Green Version]
- Shai, I.; Jiang, R.; Manson, J.E.; Stampfer, M.J.; Willett, W.C.; Colditz, G.A.; Hu, F.B. Ethnicity, obesity, and risk of type 2 diabetes in women: A 20-year follow-up study. Diabetes Care 2006, 29, 1585–1590. [Google Scholar] [CrossRef] [Green Version]
- Sundstrom-Poromaa, I.; Thu, W.P.P.; Kramer, M.S.; Logan, S.; Cauley, J.A.; Yong, E.L. Risk factors for insulin resistance in midlife Singaporean women. Maturitas 2020, 137, 50–56. [Google Scholar] [CrossRef]
- Brown, E.C.; Buchan, D.S.; Madi, S.A.; Gordon, B.N.; Drignei, D. Grip Strength Cut Points for Diabetes Risk Among Apparently Healthy U.S. Adults. Am. J. Prev. Med. 2020, 58, 757–765. [Google Scholar] [CrossRef] [PubMed]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Shen, S.; Wang, W.; Zhou, C.; Xu, L.; Qiu, J.; Wang, J.; Meng, X.; Liang, Y.; Niu, K.; et al. Poor lower extremity function was associated with pre-diabetes and diabetes in older chinese people. PLoS ONE 2014, 9, e115883. [Google Scholar] [CrossRef] [Green Version]
- Liang, X.; Jiang, C.Q.; Zhang, W.S.; Zhu, F.; Jin, Y.L.; Cheng, K.K.; Lam, T.H.; Xu, L. Association of a composite score of relative grip strength and timed up and go test with incident type 2 diabetes mellitus: Guangzhou Biobank Cohort Study. Aging 2021, 13, 18376–18391. [Google Scholar] [CrossRef] [PubMed]
- Abdul-Hameed, U.; Rangra, P.; Shareef, M.Y.; Hussain, M.E. Reliability of 1-repetition maximum estimation for upper and lower body muscular strength measurement in untrained middle aged type 2 diabetic patients. Asian J. Sport. Med. 2012, 3, 267–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grøntved, A.; Pan, A.; Mekary, R.A.; Stampfer, M.; Willett, W.C.; Manson, J.E.; Hu, F.B. Muscle-strengthening and conditioning activities and risk of type 2 diabetes: A prospective study in two cohorts of US women. PLoS Med. 2014, 11, e1001587. [Google Scholar] [CrossRef] [PubMed]
- Holten, M.K.; Zacho, M.; Gaster, M.; Juel, C.; Wojtaszewski, J.F.; Dela, F. Strength training increases insulin-mediated glucose uptake, GLUT4 content, and insulin signaling in skeletal muscle in patients with type 2 diabetes. Diabetes 2004, 53, 294–305. [Google Scholar] [CrossRef] [Green Version]
- Park, S.W.; Goodpaster, B.H.; Strotmeyer, E.S.; Kuller, L.H.; Broudeau, R.; Kammerer, C.; de Rekeneire, N.; Harris, T.B.; Schwartz, A.V.; Tylavsky, F.A.; et al. Accelerated loss of skeletal muscle strength in older adults with type 2 diabetes: The health, aging, and body composition study. Diabetes Care 2007, 30, 1507–1512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orlando, G.; Balducci, S.; Bazzucchi, I.; Pugliese, G.; Sacchetti, M. Neuromuscular dysfunction in type 2 diabetes: Underlying mechanisms and effect of resistance training. Diabetes/Metab. Res. Rev. 2016, 32, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.J.; Rikli, R.E.; Beam, W.C. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res. Q. Exerc. Sport 1999, 70, 113–119. [Google Scholar] [CrossRef]
| Characteristics | Total N (n = 1170) | No Diabetes (n = 1029, 87.9%) | Diabetes (n = 141, 12.1%) | p-Value |
|---|---|---|---|---|
| Self-reported measures, n (%) | ||||
| Age, years (mean ± SD) | 0.491 | |||
| 45–54 (50.5 ± 2.7) | 511 (43.7) | 453 (44.0) | 58 (41.1) | |
| 55–64 (59.1 ± 2.9) | 512 (43.8) | 451 (43.8) | 61 (43.3) | |
| 65–69 (66.7 ± 1.3) | 147 (12.6) | 125 (12.1) | 22 (15.6) | |
| Ethnicity | <0.001 | |||
| Chinese | 977 (83.5) | 882 (85.7) | 95 (67.4) | |
| Malay | 69 (5.9) | 56 (5.4) | 13 (9.2) | |
| Indian | 124 (10.6) | 91 (8.8) | 33 (23.4) | |
| Education level | 0.232 | |||
| Primary level or below | 172 (14.7) | 151 (14.7) | 21 (14.9) | |
| Pre-university | 761 (65.0) | 662 (64.3) | 99 (70.2) | |
| University | 237 (20.3) | 216 (21.0) | 21 (14.9) | |
| Housing type | 0.496 | |||
| Public (1–3 room) | 140 (12.0) | 120 (11.7) | 20 (14.2) | |
| Public (4–5 room) | 795 (67.9) | 705 (68.5) | 90 (63.8) | |
| Private | 235 (20.1) | 204 (19.8) | 31 (22.0) | |
| Parity | 0.207 | |||
| Nulliparous | 197 (16.8) | 168 (16.3) | 29 (20.6) | |
| Multiparous | 973 (83.2) | 861 (83.7) | 112 (79.4) | |
| Menopausal status | 0.643 | |||
| Premenopausal | 147 (12.6) | 132 (12.8) | 15 (10.6) | |
| Perimenopausal | 184 (15.7) | 159 (15.5) | 25 (17.7) | |
| Postmenopausal | 839 (71.7) | 738 (71.7) | 101 (71.6) | |
| Smoking status | 0.014 | |||
| Non-smokers | 1145 (97.9) | 1011 (98.3) | 134 (95.0) | |
| Smokers | 25 (2.1) | 18 (1.7) | 7 (5.0) | |
| Alcohol consumption | 0.075 | |||
| Non-alcohol consumers | 1133 (96.8) | 993 (96.5) | 140 (99.3) | |
| Alcohol consumers | 37 (3.2) | 36 (3.5) | 1 (0.7) | |
| Physical activity | 0.191 | |||
| Yes | 715 (61.1) | 622 (60.4) | 93 (66.0) | |
| No | 455 (38.9) | 407 (39.6) | 48 (34.0) | |
| Objectively measured parameters, n (%) | ||||
| Height (m) | 0.038 | |||
| <1.55 | 418 (35.7) | 354 (34.4) | 64 (45.4) | |
| 1.55–1.60 | 472 (40.3) | 424 (41.2) | 48 (34.0) | |
| >1.60 | 280 (23.9) | 251 (24.4) | 29 (20.6) | |
| BMI (kg/m2) | <0.001 | |||
| Underweight (<18.5) | 59 (5.0) | 57 (5.5) | 2 (1.4) | |
| Normal (18.5–22.9) | 482 (41.2) | 446 (43.3) | 36 (25.5) | |
| Overweight (23.0–27.5) | 403 (34.4) | 352 (34.2) | 51 (36.2) | |
| Obese (>27.5) | 226 (19.3) | 174 (16.9) | 52 (36.9) | |
| Visceral adipose tissue (cm2) | <0.001 | |||
| <88.6 | 393 (33.6) | 379 (36.8) | 14 (9.9) | |
| 88.6–131.0 | 385 (32.9) | 345 (33.5) | 40 (28.4) | |
| >131.0 | 392 (33.5) | 305 (29.6) | 87 (61.7) | |
| ALM/height2 | <0.001 | |||
| <5.4 | 606 (51.8) | 561 (54.5) | 45 (31.9) | |
| ≥5.4 | 564 (48.2) | 468 (45.5) | 96 (68.1) | |
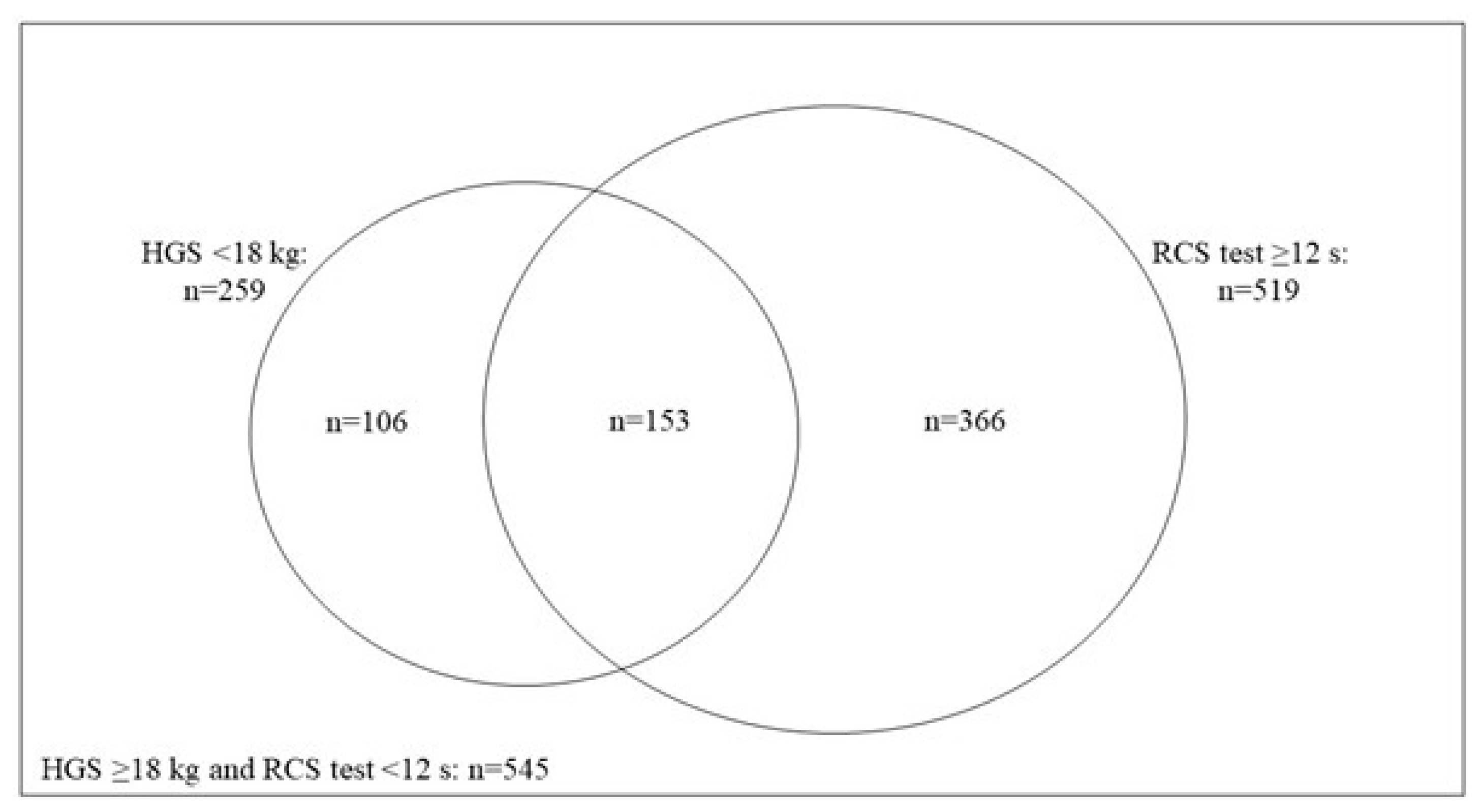
| Handgrip strength (kg) | 0.006 | |||
| <18 | 259 (22.1) | 215 (20.9) | 44 (31.2) | |
| ≥18 | 911 (77.9) | 814 (79.1) | 97 (68.8) | |
| 5-repetition chair stand test (s) 1 | 0.005 | |||
| ≥12 | 519 (44.4) | 441 (42.9) | 78 (55.3) | |
| <12 | 651 (55.6) | 588 (57.1) | 63 (44.7) | |
| Muscle strength index | <0.001 | |||
| Poor 2 | 153 (13.1) | 119 (11.6) | 34 (24.1) | |
| Intermediate 3 | 472 (40.3) | 418 (40.6) | 54 (38.3) | |
| Normal 4 | 545 (46.6) | 492 (47.8) | 53 (37.6) | |
| Muscle Strength Measures | Unadjusted | Model 1 | Model 2 | Model 3 |
|---|---|---|---|---|
| OR (95% CI) | ||||
| HGS (kg) | ||||
| <18 | 1.72 (1.17, 2.53) ** | 1.61 (1.07, 2.42) * | 1.66 (1.09, 2.55) * | 1.59 (1.03, 2.44) * |
| ≥18 | Reference | |||
| RCS test (s) | ||||
| <12 | Reference | |||
| ≥12 | 1.65 (1.16, 2.35) ** | 1.59 (1.09, 2.30) * | 1.43 (0.98, 2.10) | 1.36 (0.92, 2.00) |
| MSI | ||||
| Poor 1 | 2.65 (1.65, 4.27) *** | 2.49 (1.50, 4.14) *** | 2.37 (1.40, 4.03) ** | - |
| Intermediate 2 | 1.20 (0.80, 1.79) | 1.13 (0.75, 1.71) | 1.04 (0.68, 1.60) | - |
| Normal 3 | Reference | - | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wong, B.W.X.; Thu, W.P.P.; Chan, Y.H.; Kramer, M.S.; Logan, S.; Cauley, J.A.; Yong, E.-L. The Associations between Upper and Lower Body Muscle Strength and Diabetes among Midlife Women. Int. J. Environ. Res. Public Health 2022, 19, 13654. https://doi.org/10.3390/ijerph192013654
Wong BWX, Thu WPP, Chan YH, Kramer MS, Logan S, Cauley JA, Yong E-L. The Associations between Upper and Lower Body Muscle Strength and Diabetes among Midlife Women. International Journal of Environmental Research and Public Health. 2022; 19(20):13654. https://doi.org/10.3390/ijerph192013654
Chicago/Turabian StyleWong, Beverly W. X., Win Pa Pa Thu, Yiong Huak Chan, Michael S. Kramer, Susan Logan, Jane A. Cauley, and Eu-Leong Yong. 2022. "The Associations between Upper and Lower Body Muscle Strength and Diabetes among Midlife Women" International Journal of Environmental Research and Public Health 19, no. 20: 13654. https://doi.org/10.3390/ijerph192013654
APA StyleWong, B. W. X., Thu, W. P. P., Chan, Y. H., Kramer, M. S., Logan, S., Cauley, J. A., & Yong, E.-L. (2022). The Associations between Upper and Lower Body Muscle Strength and Diabetes among Midlife Women. International Journal of Environmental Research and Public Health, 19(20), 13654. https://doi.org/10.3390/ijerph192013654






