Performing Arts in Suicide Prevention Strategies: A Scoping Review
Abstract
1. Introduction
1.1. Suicide and Its Prevention
1.2. Performing Arts and Mental Health
1.3. Performing Arts in Suicide Prevention
1.4. Aims of This Review
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
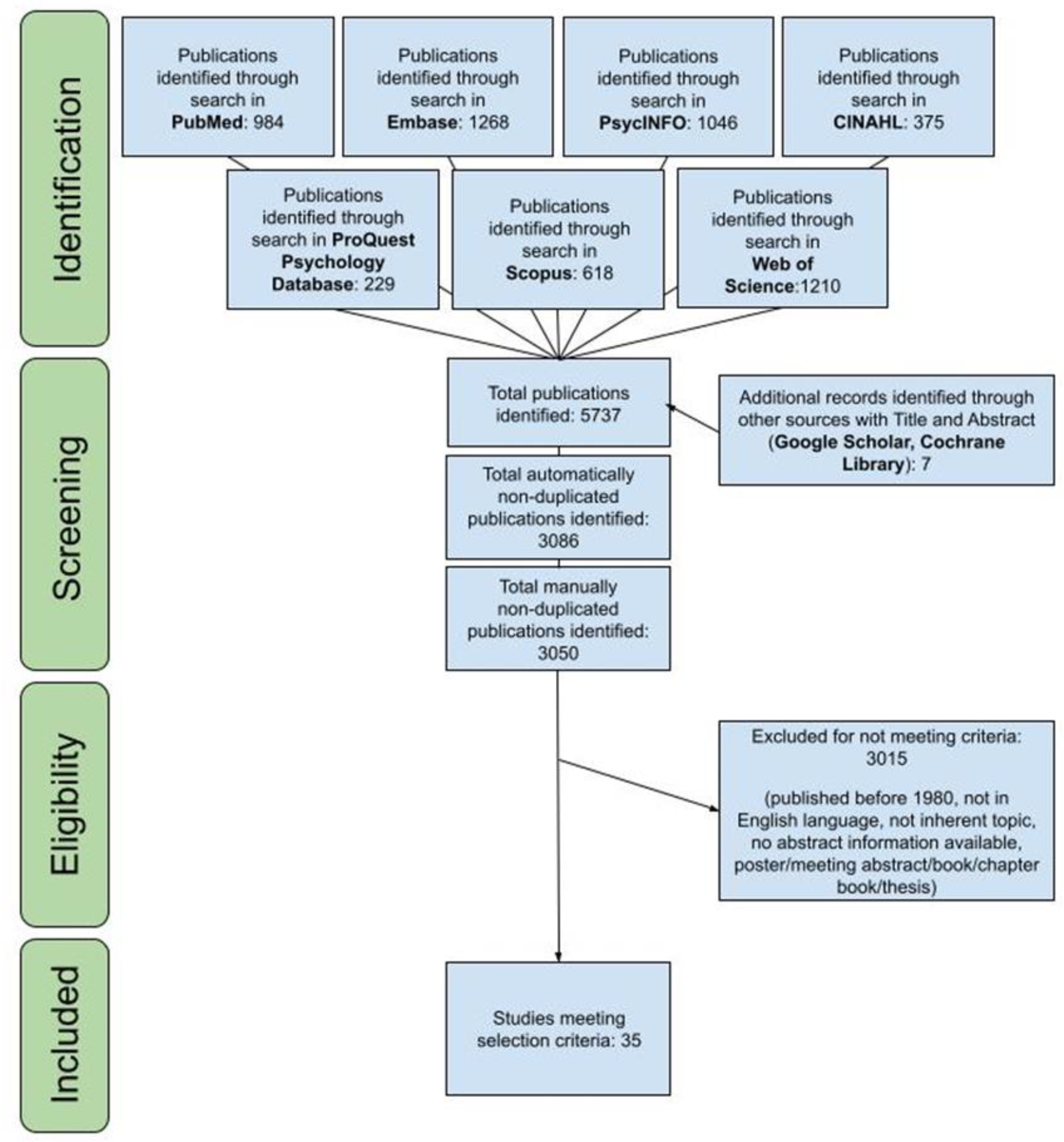
2.2. Screening and Selection of Articles
2.3. Extraction and Presentation of Results
3. Results
3.1. Selected Publications
3.2. Study Design—Which Study Designs Have Been Used to Assess Feasibility, Benefit, and Possible Adverse Effects? on Which Populations and Settings? What Is the Evidence for Feasibility and Effectiveness?
3.3. Purpose and Outcomes—Was There Any Attempt to Estimate Effectiveness? Which Outcomes Have Been Examined? What Is the Evidence for Feasibility and Effectiveness?
3.4. Art Forms—Which Type of Performing Arts Have Been Used on Suicide Prevention?
3.4.1. Theater
3.4.2. Role Playing
3.5. Multiple Art Forms
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization (WHO). Suicide Worldwide in 2019: Global Health Estimates; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Centers for Disease Control and Prevention. Web-Based Injury Statistics Query and Reporting System (WISQARS). 2021. Available online: www.cdc.gov/injury/wisqars (accessed on 30 August 2022).
- Kõlves, K.; de Leo, D. Suicide methods in children and adolescents. Eur. Child Adolesc. Psychiatry 2016, 26, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Mann, J.J. A current perspective of suicide and attempted suicide. Ann. Intern. Med. 2002, 136, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Barraclough, B.M.; Bunch, J.; Nelson, B.; Sainsbury, P. A Hundred Cases of Suicide: Clinical Aspects. Br. J. Psychiatry 1974, 125, 355–373. [Google Scholar] [CrossRef] [PubMed]
- Bertolote, J.M.; Fleischmann, A.; De Leo, D.; Wasserman, D. Suicide and mental disorders: Do we know enough? Br. J. Psychiatry 2003, 183, 382–383. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Risk and Protective Factors. 2022. Available online: https://www.cdc.gov/suicide/factors/index.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fviolenceprevention%2Fsuicide%2Friskprotectivefactors.html (accessed on 30 August 2022).
- Luoma, J.; Martin, C.E.; Pearson, J.L. Contact with Mental Health and Primary Care Providers before Suicide: A Review of the Evidence. Am. J. Psychiatry 2002, 159, 909–916. [Google Scholar] [CrossRef]
- Mann, J.J.; Apter, A.; Bertolote, J.; Beautrais, A.; Currier, D.; Haas, A.; Hegerl, U.; Lonnqvist, J.; Malone, K.M.; Marusic, A.; et al. Suicide Prevention Strategies. JAMA 2005, 294, 2064–2074. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Preventing Suicide: A Global Imperative; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Mann, J.J.; Michel, C.A.; Auerbach, R.P. Improving Suicide Prevention through Evidence-Based Strategies: A Systematic Review. Am. J. Psychiatry 2021, 178, 611–624. [Google Scholar] [CrossRef]
- Zalsman, G.; Hawton, K.; Wasserman, D.; van Heeringen, K.; Arensman, E.; Sarchiapone, M.; Carli, V.; Höschl, C.; Barzilay, R.; Balazs, J.; et al. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry 2016, 3, 646–659. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Comprehensive Mental Health Action Plan 2013–2030; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Gould, M.S.; Greenberg, T.; Velting, D.M.; Shaffer, D. Youth Suicide Risk and Preventive Interventions: A Review of the Past 10 Years. J. Am. Acad. Child Adolesc. Psychiatry 2003, 42, 386–405. [Google Scholar] [CrossRef]
- Zalsman, G.; Hawton, K.; Wasserman, D.; van Heeringen, K.; Arensman, E.; Sarchiapone, M.; Carli, V.; Höschl, C.; Winkler, P.; Balazs, J.; et al. Evidence-based national suicide prevention taskforce in Europe: A consensus position paper. Eur. Neuropsychopharmacol. 2017, 27, 418–421. [Google Scholar] [CrossRef]
- King, K.A.; Strunk, C.M.; Sorter, M.T. Preliminary Effectiveness of Surviving the Teens® Suicide Prevention and Depression Awareness Program on Adolescents’ Suicidality and Self-Efficacy in Performing Help-Seeking Behaviors. J. Sch. Health 2011, 81, 581–590. [Google Scholar] [CrossRef] [PubMed]
- Aseltine, R.H.; James, A.; Schilling, E.A.; Glanovsky, J. Evaluating the SOSsuicide prevention program: A replication and extension. BMC Public Health 2007, 7, 161. [Google Scholar] [CrossRef] [PubMed]
- Wasserman, D.; Hoven, C.W.; Wasserman, C.; Wall, M.; Eisenberg, R.; Hadlaczky, G.; Kelleher, I.; Sarchiapone, M.; Apter, A.; Balazs, J.; et al. School-based suicide prevention programmes: The SEYLE cluster-randomised, controlled trial. Lancet 2015, 385, 1536–1544. [Google Scholar] [CrossRef]
- Niederkrotenthaler, T.; Reidenberg, D.J.; Till, B.; Gould, M.S. Increasing Help-Seeking and Referrals for Individuals at Risk for Suicide by Decreasing Stigma. Am. J. Prev. Med. 2014, 47, S235–S243. [Google Scholar] [CrossRef]
- D’Azevedo, W.L. A structural approach to esthetics: Toward a definition of art in anthropology. Am. Anthropol. 1958, 60. [Google Scholar] [CrossRef]
- Goldblatt, P.F. How John Dewey’s theories underpin art and art education. Educ. Cult. 2006, 22, 17–34. [Google Scholar] [CrossRef]
- Bertram, G.W. Kunst als Menschliche Praxis; Eine Aestethik, Suhrkamp Verlag: Berlin, Germany, 2014. [Google Scholar]
- Clift, S.; Camic, P.M. Oxford Textbook of Creative Arts Health and Wellbeing: International Perspectives on Practice Policy and Research, 1st ed.; Oxford University Press: Oxford, UK, 2016; Available online: https://search.ebscohost.com/login.aspx?direct=true&scope=site&db=nlebk&db=nlabk&AN=1069415 (accessed on 30 August 2022).
- Argyle, E.; Bolton, G. Art in the community for potentially vulnerable mental health groups. Health Educ. 2005, 105, 340–354. [Google Scholar] [CrossRef]
- Madden, C.; Bloom, T. Creativity, health and arts advocacy. Int. J. Cult. Policy 2004, 10, 133–156. [Google Scholar] [CrossRef]
- Parr, H. Mental health, the arts and belongings. Trans. Inst. Br. Geogr. 2006, 31, 150–166. [Google Scholar] [CrossRef]
- Fancourt, D.; Finn, S. What Is the Evidence on the Role of the Arts in Improving Health and well-Being? A Scoping Review; IGO: Copenhagen, Denmark, 2019. [Google Scholar]
- Gaiha, S.M.; Salisbury, T.T.; Usmani, S.; Koschorke, M.; Raman, U.; Petticrew, M. Effectiveness of arts interventions to reduce mental-health-related stigma among youth: A systematic review and meta-analysis. BMC Psychiatry 2021, 21, 1–26. [Google Scholar] [CrossRef]
- Rossi Ghiglione, A.; Fabris, R.M.; Pagliarino, A. Caravan Next. A Social Community Theatre Project. Methodology, Evaluation and Analysis. Franco Angeli 2019, 40–41. Available online: http://ojs.francoangeli.it/_omp/index.php/oa/catalog/book/394 (accessed on 30 August 2022).
- Keller, S.N.; Austin, C.G.; McNeill, V. A theater intervention to promote communication and disclosure of suicidal ideation. J. Appl. Commun. Res. 2017, 45, 294–312. [Google Scholar] [CrossRef] [PubMed]
- Beidas, R.S.; Cross, W.; Dorsey, S. Show Me, Don’t Tell Me: Behavioral Rehearsal as a Training and Analogue Fidelity Tool. Cogn. Behav. Pract. 2013, 21, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Cramer, H.; Horwood, J.; Payne, S.; Araya, R.; Lester, H.; Salisbury, C. Do depressed and anxious men do groups? What works and what are the barriers to help seeking? Prim. Health Care Res. Dev. 2013, 15, 287–301. [Google Scholar] [CrossRef][Green Version]
- Humair, J.-P.; Cornuz, J. A new curriculum using active learning methods and standardized patients to train residents in smoking cessation. J. Gen. Intern. Med. 2003, 18, 1023–1027. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cargile, A. Beyond the breach: Transforming White identities in the classroom. Race Ethn. Educ. 2004, 7, 351–365. [Google Scholar] [CrossRef]
- IOM. Manual on Community-Based Mental Health and Psychosocial Support in Emergencies and Displacement; IOM: Geneva, Switzerland, 2019. [Google Scholar]
- Innocenti Malini, G.E.; Bernardi, C. (Eds.) Performing the Social Education, Care and Social Inclusion through Theatre; Franco Angeli, Eds.: Milano, Italy, 2021; Volume 196, Available online: http://hdl.handle.net/10807/178370 (accessed on 30 August 2022).
- Rodríguez, J.I.; Rich, M.D.; Hastings, R.; Page, J.L. Assessing the Impact of Augusto Boal’s “Proactive Performance”: An Embodied Approach for Cultivating Prosocial Responses to Sexual Assault. Text Perform. Q. 2006, 26, 229–252. [Google Scholar] [CrossRef]
- Dobson, J. Step by step: The use of creative arts as therapy. Nurs. Stand. 2000, 15, 18–19. [Google Scholar] [CrossRef] [PubMed]
- Mottram, P. Art Therapy with Clients Who have Dementia. Dementia 2003, 2, 272–277. [Google Scholar] [CrossRef]
- Graham-Pole, J. The creative arts: What role do they play? In Handbook of Complementary and Alternative Therapies in Mental Health; Scott, A., Ed.; Academic Press: San Diego, CA, USA, 2002; Volume xxviii, p. 574. [Google Scholar] [CrossRef]
- Hokkanen, L.; Rantala, L.; Remes, A.M.; Härkönen, B.; Viramo, P.; Winblad, I. Dance/Movement Therapeutic Methods in Management of Dementia. J. Am. Geriatr. Soc. 2003, 51, 576–577. [Google Scholar] [CrossRef]
- Daykin, N.; Orme, J.; Evans, D.; Salmon, W.D.; McEachran, M.; Brain, S. The Impact of Participation in Performing Arts on Adolescent Health and Behaviour. J. Health Psychol. 2008, 13, 251–264. [Google Scholar] [CrossRef]
- Clawson, H.J.; Coolbaugh, K. The YouthARTS Development Project; U.S. Department of Justice: Washington, DC, USA, 2001. [Google Scholar]
- Catterall, J.; Chapleau, R.; Iwanga, J. Involvement in the Arts and Human Development: General Involvement and Intensive Involvement in Music and Theatre Arts; Fiske, E., Ed.; Arts Education Partnership and President’s Committee on the Arts and Humanities: Washington, DC, USA, 1999; pp. 1–18. [Google Scholar]
- Heath, S.; Roach, A. Imaginative Actuality: Learning in the Arts during Non-School Hours; Fiske, E., Ed.; Arts Education Partnership and President’s Committee on the Arts and Humanities: Washington, DC, USA, 1999; pp. 19–34. [Google Scholar]
- Seibold, D.R.; Thomas, R.W. Rethinking the role of interpersonal influence processes in alcohol intervention situations. J. Appl. Commun. Res. 1994, 22, 177–197. [Google Scholar] [CrossRef]
- Broome, E.; Dening, T.; Schneider, J.; Brooker, D. Care staff and the creative arts: Exploring the context of involving care personnel in arts interventions. Int. Psychogeriatr. 2017, 29, 1979–1991. [Google Scholar] [CrossRef] [PubMed]
- Staricoff, R. Arts in Health: Review of the Medical Literature; Arts Council England: London, UK, 2004. [Google Scholar]
- Falletti, C.; Sofia, G. Theatre and Cognitive Neuroscience; Bloomensbury Publishing: London, UK, 2017. [Google Scholar]
- Gryglewicz, K.; Monahan, M.F.; Chen, J.I.; Bozzay, M.; Bender, A.; Gleason, L.L.; Witmeier, M.; Karver, M.S. Examining the effects of role play practice in enhancing clinical skills to assess and manage suicide risk. J. Ment. Health 2019, 29, 549–557. [Google Scholar] [CrossRef]
- El-Tannir, A.A. The corporate university model for continuous learning, training and development. Educ. Train. 2002, 44, 76–81. [Google Scholar] [CrossRef]
- Yorks, L.; Marsick, V.J.; Kasl, E.; DeChant, K. Contextualizing Team Learning: Implications for Research and Practice. Adv. Dev. Hum. Resour. 2003, 5, 103–117. [Google Scholar] [CrossRef]
- Clapper, T. Beyond Knowles: What Those Conducting Simulation Need to Know About Adult Learning Theory. Clin. Simul. Nurs. 2010, 6, e7–e14. [Google Scholar] [CrossRef]
- Stepakoff, S. From destruction to creation, from silence to speech: Poetry therapy principles and practices for working with suicide grief. Arts Psychother. 2009, 36, 105–113. [Google Scholar] [CrossRef]
- Gallant, K.; Hamilton-Hinch, B.; White, C.; Litwiller, F.; Lauckner, H. “Removing the thorns”: The role of the arts in recovery for people with mental health challenges. Arts Health 2017, 11, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Leckey, J. The therapeutic effectiveness of creative activities on mental well-being: A systematic review of the literature. J. Psychiatr. Ment. Health Nurs. 2011, 18, 501–509. [Google Scholar] [CrossRef]
- Perkins, R.; Ascenso, S.; Atkins, L.; Fancourt, D.; Williamon, A. Making music for mental health: How group drumming mediates recovery. Psychol. Well-Being Theory Res. Pract. 2016, 6, 1–17. [Google Scholar] [CrossRef]
- Sonke, J.; Pesata, V.; Nakazibwe, V.; Ssenyonjo, J.; Lloyd, R.; Espino, D.; Nieves, M.; Khandakji, S.; Hahn, P.D.; Kerrigan, M. The Arts and Health Communication in Uganda: A Light Under the Table. Health Commun. 2017, 33, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Michalak, E.E.; Livingston, J.D.; Maxwell, V.; Hole, R.; Hawke, L.D.; Parikh, S.V. Using theatre to address mental illness stigma: A knowledge translation study in bipolar disorder. Int. J. Bipolar Disord. 2014, 2, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Sonke, J.; Sams, K.; Morgan-Daniel, J.; Schaefer, N.; Pesata, V.; Golden, T.; Stuckey, H. Health Communication and the Arts in the United States: A Scoping Review. Am. J. Health Promot. 2020, 35, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, B.A. The Efficacy of Art Therapy in Pediatric Oncology Patients: An Integrative Literature Review. J. Pediatr. Nurs. 2017, 36, 173–178. [Google Scholar] [CrossRef]
- Kasahara-Kiritani, M.; Hadlaczky, G.; Westerlund, M.; Carli, V.; Wasserman, C.; Apter, A.; Balazs, J.; Bobes, J.; Brunner, R.; McMahon, E.M.; et al. Reading Books and Watching Films as a Protective Factor against Suicidal Ideation. Int. J. Environ. Res. Public Health 2015, 12, 15937–15942. [Google Scholar] [CrossRef]
- Gould, M.; Jamieson, P.; Romer, D. Media Contagion and Suicide Among the Young. Am. Behav. Sci. 2003, 46, 1269–1284. [Google Scholar] [CrossRef]
- Wyman, P.A.; Brown, C.H.; Inman, J.; Cross, W.; Schmeelk-Cone, K.; Guo, J.; Pena, J.B. Randomized trial of a gatekeeper program for suicide prevention: 1-year impact on secondary school staff. J. Consult. Clin. Psychol. 2008, 76, 104–115. [Google Scholar] [CrossRef]
- Wasserman, C.; Hoven, C.W.; Wasserman, D.; Carli, V.; Sarchiapone, M.; Al-Halabí, S.; Apter, A.; Balazs, J.; Bobes, J.; Cosman, D.; et al. Suicide prevention for youth—A mental health awareness program: Lessons learned from the Saving and Empowering Young Lives in Europe (SEYLE) intervention study. BMC Public Health 2012, 12, 776. [Google Scholar] [CrossRef]
- Beidas, R.S.; Kendall, P.C. Training therapists in evidence-based practice: A critical review of studies from a systems-contextual perspective. Clin. Psychol. Sci. Pract 2010, 17, 1–30. [Google Scholar] [CrossRef]
- Jackson, E.D.; Potkay, C.H. Audience reactions to the suicide play Quiet Cries. J. Community Psychol. 1974, 2, 16–17. [Google Scholar] [CrossRef]
- Miller-Day, M.; Hecht, M.L. Narrative Means to Preventative Ends: A Narrative Engagement Framework for Designing Prevention Interventions. Health Commun. 2013, 28, 657–670. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Baldini-Soares, C.; Khalil, H.; Parker, D. Scoping reviews. In Aromataris; Munn, Z.E., Ed.; Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Joanna Briggs Institute. Levels of Evidence and Grades of Recommendation Working Party. October 2013. Available online: https://jbi.global/sites/default/files/2019-05/JBI-Levels-of-evidence_2014_0.pdf (accessed on 25 August 2022).
- Morriss, R.; Gask, L.; Battersby, L.; Francheschini, A.; Robson, M. Teaching front-line health and voluntary workers to assess and manage suicidal patients. J. Affect. Disord. 1999, 52, 77–83. [Google Scholar] [CrossRef]
- Høifødt, T.S.; Talseth, A.-G.; Olstad, R. A qualitative study of the learning processes in young physicians treating suicidal patients: From insecurity to personal pattern knowledge and self-confidence. BMC Med. Educ. 2007, 7, 21. [Google Scholar] [CrossRef] [PubMed]
- Cross, W.; Matthieu, M.M.; Cerel, J.; Knox, K.L. Proximate Outcomes of Gatekeeper Training for Suicide Prevention in the Workplace. Suicide Life-Threat. Behav. 2007, 37, 659–670. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.; Rapp-Paglicci, L.; Rowe, W. Evaluating the Efficacy of the Prodigy Prevention Program across Urban and Rural Locales. Infant Ment. Health J. 2008, 26, 65–75. [Google Scholar] [CrossRef]
- Cross, W.; Matthieu, M.M.; Lezine, D.; Knox, K.L. Does a Brief Suicide Prevention Gatekeeper Training Program Enhance Observed Skills? Crisis 2010, 31, 149–159. [Google Scholar] [CrossRef]
- Silverman, Y.; Smith, F.; Burns, M. Coming together in pain and joy: A multicultural and arts-based suicide awareness project. Arts Psychother. 2013, 40, 216–223. [Google Scholar] [CrossRef]
- Vallance, A.K.; Hemani, A.; Fernandez, V.; Livingstone, D.; McCusker, K.; Toro-Troconis, M. Using virtual worlds for role play simulation in child and adolescent psychiatry: An evaluation study. Psychiatr. Bull. 2014, 38, 204–210. [Google Scholar] [CrossRef]
- Birrane, J.; Swan, D.; Aherne, D.; Davis, R.; Hannigan, A.; McPhillips, D.; Meagher, D.; O’Regan, A.; Ryan, P.; Schaffalitzky, E.; et al. Development and evaluation of an educational intervention in youth mental health for primary care practitioners. Ir. J. Psychol. Med. 2014, 32, 137–146. [Google Scholar] [CrossRef][Green Version]
- Fanian, S.; Young, S.K.; Mantla, M.; Daniels, A.; Chatwood, S. Evaluation of the Kts’iìhtła (“We Light the Fire”) Project: Building resiliency and connections through strengths-based creative arts programming for Indigenous youth. Int. J. Circumpolar Health 2015, 74. [Google Scholar] [CrossRef] [PubMed]
- Robinson, J.; Green, G.; Spittal, M.J.; Templer, K.; Bailey, E. Impact and Acceptability of Delivering Skills-based Training on Risk Management (STORM) in Australian Secondary Schools. Health Behav. Policy Rev. 2016, 3, 259–268. [Google Scholar] [CrossRef]
- Bartgis, J. Online Role-play Simulations with Emotionally Responsive Avatars for the Early Detection of Native Youth Psychological Distress, Including Depression and Suicidal Ideation. Am. Indian Alsk. Nativ. Ment. Health Res. 2016, 23, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Keller, S.N.; Wilkinson, T. Preventing suicide in Montana: A community-based theatre intervention. J. Soc. Mark. 2017, 7, 423–440. [Google Scholar] [CrossRef]
- Owen, J.R.; Pheister, M.; Simons, J.G. Suicide Symposium: A Multidisciplinary Approach to Risk Assessment and the Emotional Aftermath of Patient Suicide. MedEdPORTAL 2018, 14, 10776. [Google Scholar] [CrossRef]
- Nakagami, Y.; Kubo, H.; Katsuki, R.; Sakai, T.; Sugihara, G.; Naito, C.; Oda, H.; Hayakawa, K.; Suzuki, Y.; Fujisawa, D.; et al. Development of a 2-h suicide prevention program for medical staff including nurses and medical residents: A two-center pilot trial. J. Affect. Disord. 2018, 225, 569–576. [Google Scholar] [CrossRef]
- Timmons-Mitchell, J.; Albright, G.; McMillan, J.; Shockley, K.; Cho, S. Virtual Role-play: Middle School Educators Addressing Student Mental Health. Health Behav. Policy Rev. 2019, 6, 546–557. [Google Scholar] [CrossRef]
- Kratz, J.; Bragg, J.E.; Nay, E.D.E.; Miller-Cribbs, J.; Munoz, R.T.; Howell, D. Educational assessment of a social simulation for MSW students using the CAMS framework. Soc. Work Educ. 2020, 41, 248–260. [Google Scholar] [CrossRef]
- Carpenter, D.M.; Roberts, C.A.; Lavigne, J.E.; Cross, W.F. Gatekeeper training needs of community pharmacy staff. Suicide Life-Threat. Behav. 2021, 51, 220–228. [Google Scholar] [CrossRef]
- Hutson, E.; Zeno, R. Clinical Competence for Youth Suicide: Use of Simulation in Pediatric and Psychiatric–Mental Health Nurse Practitioner Programs. J. Psychosoc. Nurs. Ment. Health Serv. 2021, 59, 7–13. [Google Scholar] [CrossRef]
- Ross, S.G.; Dehay, T.; Deiling, M. The Suicide Prevention for College Student Gatekeepers Program. Crisis 2021, 42, 48–55. [Google Scholar] [CrossRef]
- Nash, L.; Scott, K.; Pit, S.; Barnes, E.; Ivory, K.; Hooker, C. Evaluation of a workshop using verbatim theatre stimuli to address challenging workplace situations: A pilot study. Clin. Teach. 2020, 18, 43–50. [Google Scholar] [CrossRef]
- Fenwick, C.D.; Vassilas, C.A.; Carter, H.; Haque, M.S. Training health professionals in the recognition, assessement and management of suicide risk. Int. J. Psychiatry Clin. Pract 2004, 8, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Pasco, S.; Wallack, C.; Sartin, R.M.; Dayton, R. The Impact of Experiential Exercises on Communication and Relational Skills in a Suicide Prevention Gatekeeper-Training Program for College Resident Advisors. J. Am. Coll. Health 2012, 60, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Coleman, D.; Del Quest, A. Science from Evaluation: Testing Hypotheses about Differential Effects of Three Youth-Focused Suicide Prevention Trainings. Soc. Work. Public Health 2014, 30, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Kaur, J. Effect of Life Skills Training on Suicidal Behaviour of Adolescents. MIER J. Educ. Stud. Trends Pract 2021, 269–280. [Google Scholar] [CrossRef]
- Thomas, E.; Morgan, G. Tackling stigma in schools. Mental Health Today 2006, 30–32. [Google Scholar]
- Goldberg, D.P.; Gask, L.; Zakroyeva, A.; Proselkova, E.; Ryzhkova, N.; Williams, P. Training teachers to teach mental health skills to staff in primary care settings in a vast, under-populated area. Ment. Health Fam. Med. 2012, 9, 219–224. [Google Scholar]
- Wasserman, C.; Postuvan, V.; Herta, D.-C.; Iosue, M.; Värnik, P.; Carli, V. Interactions between youth and mental health professionals: The Youth Aware of Mental health (YAM) program experience. PLoS ONE 2018, 13, e0191843. [Google Scholar] [CrossRef]
- Keller, S.; McNeill, V.; Honea, J.; Miller, L.P. A Look at Culture and Stigma of Suicide: Textual Analysis of Community Theatre Performances. Int. J. Environ. Res. Public Health 2019, 16, 352. [Google Scholar] [CrossRef]
- Cross, W.F.; Seaburn, D.; Gibbs, D.; Schmeelk-Cone, K.; White, A.M.; Caine, E.D. Does Practice Make Perfect? A Randomized Control Trial of Behavioral Rehearsal on Suicide Prevention Gatekeeper Skills. J. Prim. Prev. 2011, 32, 195–211. [Google Scholar] [CrossRef] [PubMed]
- Long, M.W.; Albright, G.; McMillan, J.; Shockley, K.M.; Price, O.A. Enhancing Educator Engagement in School Mental Health Care Through Digital Simulation Professional Development. J. Sch. Health 2018, 88, 651–659. [Google Scholar] [CrossRef] [PubMed]
- O’Reilly, C.L.; Moles, R.J.; Boukouvalas, E.; El-Den, S. Assessing students’ mental health crisis skills via consumers with lived experience: A qualitative evaluation. J. Ment. Health Train. Educ. Pract 2019, 14, 361–371. [Google Scholar] [CrossRef]
- Garraza, L.G.; Kuiper, N.; Cross, W.F.; Hicks, B.; Walrath, C. The Effectiveness of Active Learning Strategies in Gatekeeper Training on Behavioral Outcomes. Crisis 2021, 42, 360–368. [Google Scholar] [CrossRef]
- Quinnett, P. QPR: Ask a Question, Save a Life; The QPR Institute and Suicide Awareness/Voices of Education: Spokane, WA, Australia, 1995. [Google Scholar]
| Database | Search String |
|---|---|
| PubMed | (“Suicide”[Mesh] OR suicid*[tiab]) AND (“Drama”[Mesh] OR theat*[tiab] OR drama*[tiab] OR recit*[tiab] OR “performing-art*”[tiab] OR “participatory-art*”[tiab] OR “Psychodrama”[Mesh] OR psychodram*[tiab] OR “role-play”[tiab] OR “role-plays”[tiab] OR “role-playing”[tiab] OR “role-player*”[tiab] OR roleplay*[tiab] OR impersonat*[tiab] OR storytell*[tiab] OR “story-tell*”[tiab]) |
| Embase | ((‘suicidal behavior’/exp OR suicid*:ti,ab,kw) AND (‘drama therapy’/exp OR theat*:ti,ab,kw OR drama*:ti,ab,kw OR recit*:ti,ab,kw OR ‘performing arts’/exp OR ‘performing-art*’:ti,ab,kw OR ‘participatory-art*’:ti,ab,kw OR ‘psychodrama’/exp OR ‘role playing’/exp OR psychodram*:ti,ab,kw OR ‘role-play’:ti,ab,kw OR ‘role-plays’:ti,ab,kw OR ‘role-playing’:ti,ab,kw OR ‘role-player*’:ti,ab,kw OR roleplay*:ti,ab,kw OR impersonat*:ti,ab,kw OR ‘storytelling’/exp OR storytell*:ti,ab,kw OR ‘story-tell*’:ti,ab,kw)) NOT ‘conference abstract’/it |
| CINAHL | (MH “Suicide+” OR TI suicid* OR AB suicid*) AND (MH “Drama” OR TI theat* OR AB theat* OR TI drama* OR AB drama* OR TI recit* OR AB recit* OR MH “Performing Arts” OR TI “performing-art*” OR AB “performing-art*” OR TI “participatory-art*” OR AB “participatory-art*” OR MH “Psychodrama+” OR TI psychodram* OR AB psychodram* OR TI “role-play” OR AB “role-play” OR TI “role-plays” OR AB “role-plays” OR TI “role-playing” OR AB “role-playing” OR TI “role-player*” OR AB “role-player*” OR TI roleplay* OR AB roleplay* OR TI impersonat* OR AB impersonat* OR MH “Storytelling+” OR TI storytell* OR AB storytell* OR TI “story-tell*” OR AB “story-tell*”) |
| PsycINFO | (DE “Suicidal Behavior” OR DE “Attempted Suicide” OR DE “Suicidal Ideation” OR DE “Suicide” OR DE “Suicidality” OR DE “Suicide Prevention” OR TI suicid* OR AB suicid*) AND (DE “Theatre” OR DE “Drama” OR TI theat* OR AB theat* OR TI drama* OR AB drama* OR TI recit* OR AB recit* OR MH “Performing Arts” OR TI “performing-art*” OR AB “performing-art*” OR TI “participatory-art*” OR AB “participatory-art*” OR DE “Psychodrama” OR DE “Role Playing” OR TI psychodram* OR AB psychodram* OR TI “role-play” OR AB “role-play” OR TI “role-plays” OR AB “role-plays” OR TI “role-playing” OR AB “role-playing” OR TI “role-player*” OR AB “role-player*” OR TI roleplay* OR AB roleplay* OR TI impersonat* OR AB impersonat* OR DE “Storytelling” OR TI storytell* OR AB storytell* OR TI “story-tell*” OR AB “story-tell*”) |
| ProQuest Psychology Database | (MAINSUBJECT.EXACT(“Suicides & suicide attempts”) OR ti(suicid*) OR ab(suicid*)) MAINSUBJECT.EXACT(“Drama”) OR MAINSUBJECT.EXACT(“Acting”) OR MAINSUBJECT.EXACT(“Performing arts”) OR MAINSUBJECT. EXACT(“Role playing”) OR MAINSUBJECT.EXACT(“Storytelling”) ti(theat* OR drama* OR recit* OR “performing-art*” OR “participatory-art*” OR psychodram* OR “role-play” OR “role-plays” OR “role-playing” OR “role-player*” OR roleplay* OR impersonat* OR storytell* OR “story-tell*”) ab(theat* OR drama* OR recit* OR “performing-art*” OR “participatory-art*” OR psychodram* OR “role-play” OR “role-plays” OR “role-playing” OR “role-player*” OR roleplay* OR impersonat* OR storytell* OR “story-tell*”) 2 OR 3 OR 4 1 AND 5 |
| Scopus | ((TITLE-ABS-KEY (suicid*)) AND (TITLE-ABS-KEY (theat* OR drama* OR recit* OR “performing-art*” OR “participatory-art*” OR psychodram* OR “role-play” OR “role-plays” OR “role-playing” OR “roleplayer*” OR roleplay* OR impersonat* OR storytell* OR “story-tell*”))) AND NOT ((INDEX (medline OR embase)) OR (PMID (1* OR 2* OR 3* OR 4* OR 5* OR 6* OR 7* OR 8* OR 9* OR 0*))) |
| Web of Science | TS = (suicid*) AND TS = (theat* OR drama* OR recit* OR “performing-art*” OR “participatory-art*” OR psychodram* OR “role-play” OR “role-plays” OR “role-playing” OR “role-player*” OR roleplay* OR impersonat* OR storytell* OR “story-tell*”) |
| Reference | Country | Study Design | Main Art Form Used | Purpose | Sample Size and Population | Period of Intervention |
|---|---|---|---|---|---|---|
| Bartgis et al., 2016 [82] | USA | Observational study without a control group | Role-play online | To examine the outcomes for American Indian and Alaska Native students, teachers, and faculty completing online role-play gatekeeper training simulations. | Gatekeepers-9000: university professors, college students, high school, and middle school educators | From April 2011 to December 2013 |
| Birrane et al., 2015 [79] | Ireland | Observational study without a control group | Role play | To describe the development and evaluation of an educational intervention on youth mental health and substance misuse for primary care professionals. | Gatekeepers-30 general practitioners and other primary care professionals | Session: 2 h |
| Carpenter et al., 2021 [88] | USA | Observational study without a control group | Role play | To identify how to adapt the online Veteran Administration’s suicide prevention gatekeeper training program (SAVE) for community pharmacy staff. | Gatekeepers-17 community pharmacy staff members | Session: 20 min and 1 h semi-structured interview. |
| Coleman et al., 2015 [94] | USA | Quasi-experimental prospectively controlled study | Role play | To test hypotheses about two brief suicide prevention gatekeeper trainings (question, persuade, refer [QPR] and RESPONSE) and one longer suicide intervention skills training (Applied Suicide Intervention Skills Training [ASIST]). | Gatekeepers-126 (clinician, teachers, church leaders, coaches, corrections staff) | Session: 1 h 25 min. Period of intervention: 6 months. |
| Cross et al., 2007 [74] | USA | Observational study without a control group | Role play | To evaluate outcomes of a gatekeeper training for suicide prevention in a sample of non-clinicians. | Gatekeepers-76 nonclinical employees in a university hospital | Session: 1 h. Period of intervention: 6 weeks. |
| Cross et al., 2010 [76] | USA | Observational study without a control group | Role play | To assess and predict the impact of brief, gatekeeper training on community members’ observed skills. | Gatekeeper-50 employees at US universities | Session: 6 h. Period of intervention: 4 months. |
| Cross et al., 2011 [100] | USA | RCT | Role play | To compare gatekeeper training as usual with training plus brief behavioral rehearsal for school staff and parents in a school community. | Gatekeepers-114 | Session: 1 h 25 min. Period of intervention: 17 months. |
| Fanian et al., 2015 [80] | Canada | Observational study without a control group | Multiple art forms—spoken word, sound production and design, film, photography, multimedia arts, jewellery making and visual arts. | To evaluate a creative arts workshop for Tłı ̨cho ̨ youth to explore critical community issues and find solutions together using the arts. | 9 youth per day-ages ranged from 13 to 22 | Session: 5 days |
| Fenwick et al., 2004 [92] | UK | Quasi-experimental prospectively controlled study | Role play | To evaluate the impact of two types of training courses: full day workshops with actors role-playing patients; and a half-day lecture. | Gatekeepers-107 from different disciplines | Session: 1 h 45 min. Period of intervention: 2 months. |
| Godoy Garraza et al., 2021 [103] | USA | RCT | Role play | To examine the impact of two training enhancements (role-play and booster) on intermediate gatekeepers training outcomes. | Gatekeepers-661 (287 QPR + Role-play; 374 QPR Alone) | Session: 1–2 h. Period of intervention: 6 months. |
| Goldberg et al., 2012 [97] | Russia | Observational study without a control group | Role play | To improve the education of existing primary care staff on the management of mental health disorders. | Gatekeepers-37 general practitioners, feldshers, practice nurses, psychologists, and teacher | Session: 5 days. Period of intervention: 3 months. |
| Gryglewicz et al., 2020 [50] | USA | Observational study without a control group | Role play | To examine the effect of role-play training on mental health practitioners’ attitudes, subjective norms, and perceived behavioral control surrounding suicide risk assessment behaviors. | Gatekeepers-137 mental health workers | Session: 4.5 h. Period of intervention: 3 years. |
| Høifødt et al., 2007 [73] | Norway | Observational study without a control group | Role play | To describe the experience of newly educated physicians lived experience learning processes related to treating suicidal patients. | Gatekeepers-13 medical candidates | Session: 2 days |
| Hutson et al., 2021 [89] | USA | Observational study without a control group | Role play-simulation | To describe objective structured clinical examinations (OSCEs) for nurse practitioner students aimed at building skills for managing a pediatric patient with acute suicidal ideation. | Gatekeepers-18 nurse practitioners, pediatric nurse practitioner and psychiatric-mental health nurse practitioners | Session: 20 min and 24 h to complete evaluation. |
| Kaur, 2021 [95] | India | Quasi-experimental prospectively controlled study | Role play | To investigate the effect of life skills training on the suicidal behavior of adolescents. | 970 adolescents (485 experimental group; 485 control group) | Session: 40 min |
| Keller et al. J Soc Mark. 2017 [83] | USA | Observational study without a control group | Theater | To examine whether a community-based suicide prevention project could increase willingness to seek professional help for suicidal ideation among eastern Montana youth. | 224 high school students | Session: the performance lasted 20 min, followed by a moderated 40 min Q and A session. Period of intervention: 6 months. |
| Keller et al., 2017 [30] | USA | Observational study without a control group | Theater | To evaluate a community-based, narrative theater project designed to increase awareness and use of suicide prevention resources among eastern Montana youth. | 27 high school students and college students | Session: 12 weeks. Period of intervention: 3 years. |
| Keller et al., 2019 [99] | USA | Cross-sectional study | Theater | To analyze differences in Eastern Montana Caucasian and Native American youths’ experiences with stigma about mental illness that affect help-seeking for suicidal experiences. | 33 high school students and college students | 10 weeks |
| Kratz et al., 2020 [87] | USA | Observational study without a control group | Role play | To evaluate the outcomes of an educational pilot study integrating didactic instruction, readings, role-plays, and simulation for teaching suicide intervention skills. | Gatekeepers-58 Master of Social Work’s students | Session: 50 min. Period of intervention: 16 weeks. |
| Long et al., 2018 [101] | USA | RCT | Role-play online | To evaluate the impact of the At-Risk for Elementary School Educators online mental health role-play simulation for elementary school teachers on changes in teachers’ helping attitudes and behaviors in students experiencing psychological distress. | Gatekeepers-18,896 schoolteachers, mental health professionals | Session: 45–90 min. Period of intervention: 3 months. |
| Morriss et al., 1999 [72] | UK | Observational study without a control group | Role play | To devise and evaluate the retention of a new brief training package for non-psychiatrically trained multidisciplinary staff to assess suicide risk and manage suicidal patients. | Gatekeepers-33 health and voluntary workers | 8 h of interview skills training (2 h sessions). |
| Nakagami et al., 2018 [85] | Japan | Observational study without a control group | Role play | To evaluate a suicide intervention program among medical staff. | Gatekeepers-74 medical staff members | Session: 2 h. Period of intervention: 1 month. |
| Nash et al., 2021 [91] | Australia | Observational study without a control group | Theater | To evaluate a workshop for health care students that used filmed vignettes from a verbatim theater play. | Gatekeepers-65 nursing, medical and allied health students and medical students only. | Session: 90 min |
| O’Reilly et al., 2019 [102] | Australia | RCT | Role play | To use a novel mental health first aid assessment approach involving simulated role-plays enacted by people with a lived experience of mental illness and explore participants’ and simulated patients’ views of participating in simulated role-plays of mental health crises. | Gatekeepers-22 pharmacy students | Mean duration of 28.8 min |
| Owen et al., 2018 [84] | USA | Observational study without a control group | Role play | To create a symposium curriculum to provide a structured, safe environment where mental health trainees and practitioners of various specialties cab obtain collegial support and education to reduce the stigma and potential isolation surrounding patient suicide. | 35 mental health practitioners and trainees | Session: 4 h |
| Pasco et al., 2012 [93] | USA | Quasi experimental control study | Role play | To evaluate the efficacy of an experiential-based gatekeeper training, which included an emphasis on enhancing communication skills and relational connections in addition to the didactic foci of standard gatekeeper training. | Gatekeepers-65 college resident advisors | Session: 3 h |
| Robinson et al., 2016 [81] | Australia | Observational study without a control group | Role play | To examine the impact of delivering an evidence-based gatekeeper training package for suicide prevention (STORM®) in an Australian setting. | Gatekeepers-84 staff members from schools | Training package duration (2 days) and FU 8 weeks later. |
| Ross et al., 2021 [90] | USA | Observational study without a control group | Role play | To evaluate the Suicide Prevention for College Student Gatekeepers training program, designed to provide college students with information about the warning signs of suicide, as well as how to intervene when indicated. | Gatekeepers-65 college students | Session: 90 min. Period of intervention: 12 weeks. |
| Silverman et al., 2013 [77] | Canada | Observational study without a control group | Multiple art forms—performing arts (drama, music, artmaking, and writing)—arts-based approach. | To describe a two-day arts-based symposium that brought together members from diverse cultural communities. | 18 members from different cultural communities including the Inuit, Mohawk, Jewish, Christian, Baha’i, South-Asian Canadian, Senior and LGBTQ communities. | Session: 2 days |
| Stewart et al., 2009 [75] | USA | Observational study without a control group | Multiple art forms—classes encompassing the visual, performing, musical, media, and theatre arts. | To examine the effects of the Prodigy Cultural Arts Program on at-risk and adjudicated youth in a rural and an urban locale. | 350 adolescents and their parents | Session: 2 months |
| Thomas et al., 2006 [96] | UK (Scotland) | Cross-sectional study | Theatre | To evaluate STIGMA play and workshops, with the aim of addressing sensitive issues close to young people, such as suicide or self-harm, and to improve seeking help attitudes. | 950 secondary school children | Session: 1 h and 10 min |
| Timmons-Mitchell et al., 2019 [86] | USA | Observational study without a control group | Role-play online | To examine the impact of a virtual training program, Kognito At-Risk role-play simulation, on the mental health and suicide prevention gatekeeping skills of middle school educators. | Gatekeepers-33,703 middle school educators | Session: 45–90 min. Period of intervention: 3 months. |
| Vallance et al., 2014 [78] | UK | Observational study without a control group | Role play | To develop and evaluate a novel teaching session on clinical assessment using role play simulation. | Gatekeepers-10 medical students | Session: 90 min |
| Wasserman et al., 2018 [98] | Estonia, Italy, Romania and Spain | Cross-sectional study | Role play | To discuss mental health in terms relevant to youth (peer support, stress, crisis, depression, suicide, and help-seeking), after their participation in the Youth Aware of Mental Health Program. | 32 adolescents | Session: a five-hour program spanning three weeks. |
| Wasserman et al., 2015 [18] | Europe (Austria, Estonia, France, Germany, Hungary, Ireland, Italy, Romania, Slovenia, and Spain). | RCT | Role play | To report the results of the Saving and Empowering Young Lives in Europe (SEYLE) study, a largescale, multi-country, European randomized controlled trial of the school-based prevention of suicidal behavior in adolescents. | 11,110 adolescents | Session: 5 h in 4 weeks. Period of intervention: 12 months. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Davico, C.; Rossi Ghiglione, A.; Lonardelli, E.; Di Franco, F.; Ricci, F.; Marcotulli, D.; Graziano, F.; Begotti, T.; Amianto, F.; Calandri, E.; et al. Performing Arts in Suicide Prevention Strategies: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 14948. https://doi.org/10.3390/ijerph192214948
Davico C, Rossi Ghiglione A, Lonardelli E, Di Franco F, Ricci F, Marcotulli D, Graziano F, Begotti T, Amianto F, Calandri E, et al. Performing Arts in Suicide Prevention Strategies: A Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(22):14948. https://doi.org/10.3390/ijerph192214948
Chicago/Turabian StyleDavico, Chiara, Alessandra Rossi Ghiglione, Elena Lonardelli, Francesca Di Franco, Federica Ricci, Daniele Marcotulli, Federica Graziano, Tatiana Begotti, Federico Amianto, Emanuela Calandri, and et al. 2022. "Performing Arts in Suicide Prevention Strategies: A Scoping Review" International Journal of Environmental Research and Public Health 19, no. 22: 14948. https://doi.org/10.3390/ijerph192214948
APA StyleDavico, C., Rossi Ghiglione, A., Lonardelli, E., Di Franco, F., Ricci, F., Marcotulli, D., Graziano, F., Begotti, T., Amianto, F., Calandri, E., Tirocchi, S., Carlotti, E. G., Lenzi, M., Vitiello, B., Mazza, M., & Caroppo, E. (2022). Performing Arts in Suicide Prevention Strategies: A Scoping Review. International Journal of Environmental Research and Public Health, 19(22), 14948. https://doi.org/10.3390/ijerph192214948







