Moral Distress of Intensive Care Nurses: A Phenomenological Qualitative Study Two Years after the First Wave of the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sampling
2.3. Data Collection
2.4. Data Analysis
2.5. Study Rigour
2.6. Ethical Approval
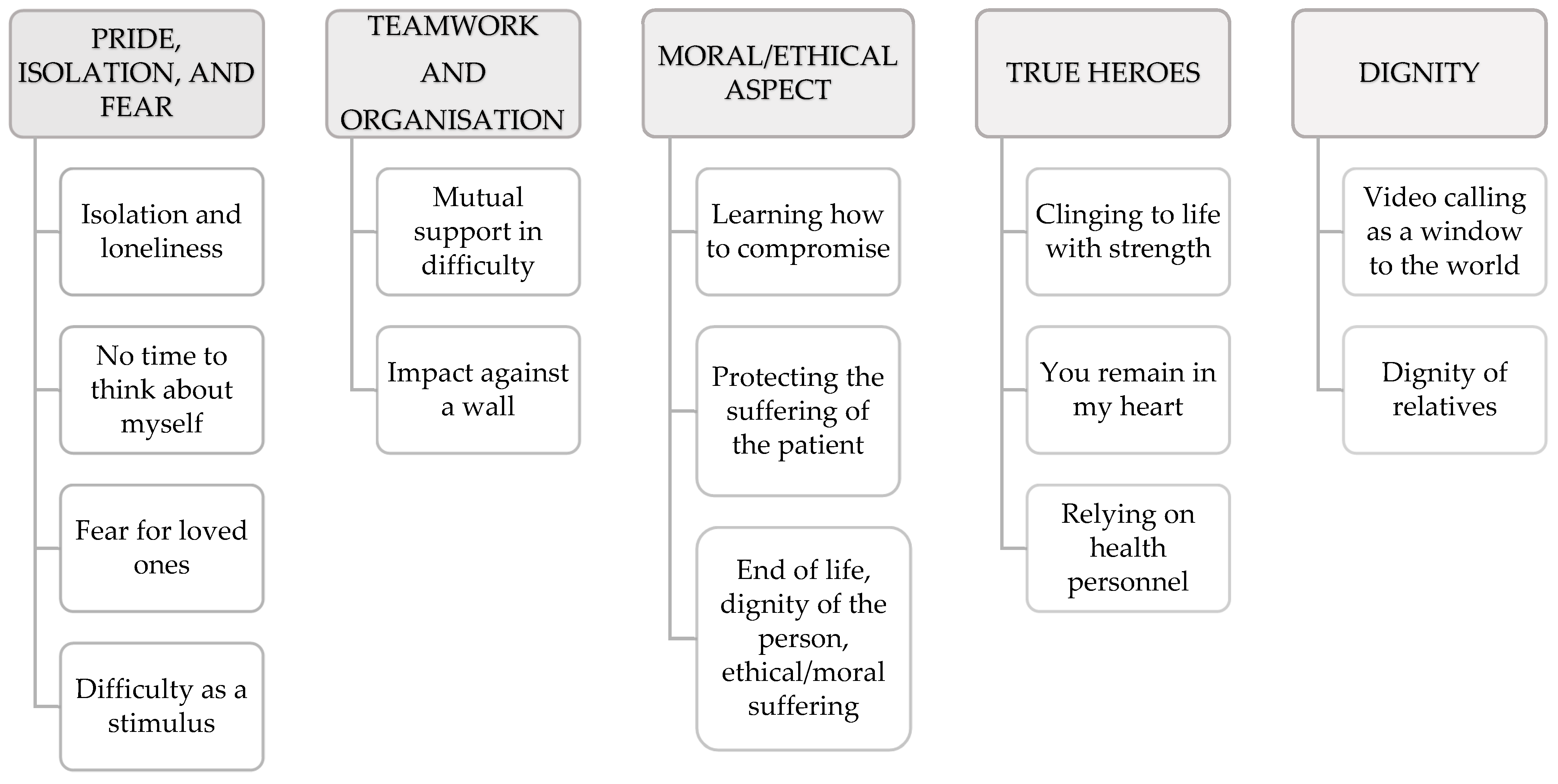
3. Results
3.1. Pride, Isolation, and Fear
3.1.1. Isolation and Loneliness
“Both me and my husband …”–“I tried to keep a certain distance but I do not have a huge house. I was also distancing myself from hugging my little girl, physical contact was not very easy.” (ID.3)
“On the one hand, positive things … one’s own space, one’s own autonomy … on the other hand, however, you have a sense of isolation … in the sense that I am used to arriving home and having a chat with someone … finding myself alone … without being able to go out or anything … it was a mixture of emotions … good and bad ….” (ID.5)
3.1.2. No Time to Think about Myself
“For the first month and a half, the days for us were all the same. This meant that we never stopped and there was no time, for me and for us, to think.” (ID.13)
“I would come home and there would be a moment when I would try to relax, as if all the tension of the day would collapse, and there, however, I would often […] cry […]. I … just needed to let off steam when I came back from there [the hospital].” (ID.12)
3.1.3. Fear for Loved Ones
“At home, I was a bit terrified because it was a bit like the plague, you did not know how to deal with it … Then, obviously, working in a hospital, you had to take some precautions at home as well.” (ID.2)
“It had mixed emotions … I found myself suddenly having to leave home to protect my family, as my father had a heart condition and during the first wave of COVID-19, I had left home and found a rented flat.” (ID.5)
3.1.4. Difficulty as a Stimulus
“The situation taught me a lot, in the sense I think I wouldn’t have arrived today with all the knowledge I have now if it hadn’t been for COVID-19. I quit a lot of safety during COVID-19.” (ID.5)
“It is not trivial to have the courage to face something you do not know.” (ID.11)
3.2. Teamwork and Organisation
3.2.1. Mutual Support in Difficulty
“We were all there fighting the same enemy. Before, we were a little more competitive, in conflict, for example compared to other colleagues from other departments, instead now we were all there, we supported each other.” (ID.1)
“With the doctors and anaesthesiologists there was a good group, a good collaboration, on the other hand we were in the same boat.” (ID.2)
“The problem I found was in managing the constantly changing shifts, the wards were changing and having to keep asking for extreme availability …, at a certain point you realise that availability was taken for granted”–“If I could have … managed more effectively ….”–“The nurses were committed, they accepted the requests and you realise that every time you ask for something you are a bit on eggshells, you have to be more careful because for me there was a lot of insecurity left from this staff point of view … keep changing the colleague.” (ID.4)
“We knew, however, that we could ask her [head nurse]. This I will never stop saying. Even from a psychological point of view … she gave us a great hand.” (ID.12)
A nurse interviewed highlighted the care taken by the head nurse, who tried hard to alleviate stress and also took care of the psychological and meditative components.
“The head nurse was very attentive, especially in the beginning. She would help us, she would push us, she would even send us online yoga classes (sneers) … she would make up anything and everything.” (ID.10)
3.2.2. Impact against a Wall
“I remember that we were given the instruction booklet on how to operate the fans. We felt inadequate … let’s just say we improvised a bit from that point of view.” (ID.1)
“Worry, at first worry. First because you didn’t know what it was or how to deal with it and you saw so much confusion around. And the fact of seeing so much, so much confusion around automatically spilled over onto us … At a certain point there were protocols to follow and you found yourself having to be helpless, not being able to do anything at all and seeing a life passing away there, in front of you, without being able to do anything, because nothing worked … so that really leaves a mark on you.” (ID.3)
“It was quite an impact against a wall … in the sense that we found ourselves doing the jobs that we were not ready to do….” (ID.7)
“I absolutely did not share this position, then, show yourself; at a certain point you put on your gown for once, dress up, but come and show yourself … this made us feel abandoned….” (ID.1)
“I understand that there were no resources … but it could have been better managed, in my opinion….” (ID.7)
“Having never worked in such a context, with such a tough and tough care complexity, I found myself having to learn in very few days everything there was to know in order to be able to manage a patient with high care complexity.” (ID.13)
“In my opinion, the biggest difficulty was that we came from different realities, without knowing each other, by the way, so standardising our skills was complicated and I don’t even know if we succeeded in the end.” (ID.10)
3.3. Moral/Ethical Aspect
3.3.1. Learning How to Compromise
“I had a fit of tears, because decisions had been taken which were completely at odds with what we were experiencing, we were pointing out that we were in difficulty with certain aspects….” (ID.1)
“To compromise … to think about certain things”–“obviously terminal patient, non-invasive ventilation, face all bruised … on morphine to try to keep her calm; when asked: ‘excuse me, but hasn’t anyone tried to ask a doctor following her if something concrete can be done?’ It doesn’t change the destiny, rather we put a less invasive aid, but we try not to let her die with a wounded face’ …” (ID.5)
3.3.2. Protecting the Suffering of the Patient
“How hard it was to see the dead person put in the sack with that soaked sheet, to close the sack; to know that no one would ever see him again, no family or anyone. And can you imagine the short pause if it had happened to you! To me!” (ID.3)
3.3.3. End of Life, Dignity of the Person, and Ethical/Moral Suffering
“Because what has always been valid for me, regardless of the COVID-19, is the respect of dignity … both when one is alive but even more so when one is in a terminal phase”–“to try to ensure the life they had as best as possible …” (ID.5)
3.4. True Heroes
3.4.1. Clinging to Life with Strength
“I was amazed by the patients. The first day I set foot in that tent I thought “not a single person here gets out, nobody makes it” and instead they really showed strength in sticking to life. I feel so much admiration for them, for how they dealt with this dramatic moment in their lives.” (ID.8)
“Patients have taught us so much.” (ID.10)
3.4.2. You Remain in My Heart
“To the patient [who] tells you ‘I don’t know what happened, I mean, I don’t understand, but I see that I’m slowly getting better’, we tried to give him hope, saying ‘you were really sick before, now you’re slowly getting over it from the critical phase and I’m happy for you, because my efforts have finally paid off’.” (ID.11)
3.4.3. Relying on Health Personnel
“Relatives trusted us, nurses and doctors, without hesitation.” (ID.10)
3.5. Dignity
3.5.1. Video Calling as a Window to the World
“The relatives were far away [but] we managed to use video calls, either to communicate with relatives or to have patients communicate directly with relatives. I must say that with every video call I attended, I almost cried (sneers). It was emotional. [Attending the video calls].” (ID.10)
“Strange, emotional to communicate [with relatives] instead of patients because they were intubated. They couldn’t speak, they had maybe a voice wire and on the phone, they couldn’t be heard, it was you who actually had to then communicate with the relatives. You were immersing yourself in the family, in the intimate [and] in the difficulties that [every] family [had] to face.” (ID.10)
3.5.2. Dignity of Relatives
“The relatives have taught me a tremendous lesson. Seeing the enthusiasm of the first video call was pure joy. I used to say to myself ‘how can they be satisfied with that?’ The relatives had dignity, the ability to give up seeing their loved one, to accept depersonalised telephone information.” (ID.9)
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. COVID-19 Weekly Epidemiological Update; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Legido-Quigley, H.; Asgari, N.; Teo, Y.Y.; Leung, G.M.; Oshitani, H.; Fukuda, K.; Cook, A.R.; Hsu, L.Y.; Shibuya, K.; Heymann, D. Are High-Performing Health Systems Resilient against the COVID-19 Epidemic? Lancet 2020, 395, 848–850. [Google Scholar] [CrossRef] [Green Version]
- Turale, S.; Meechamnan, C.; Kunaviktikul, W. Challenging Times: Ethics, Nursing and the COVID-19 Pandemic. Int. Nurs. Rev. 2020, 67, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Allado, E.; Poussel, M.; Valentin, S.; Kimmoun, A.; Levy, B.; Nguyen, D.T.; Rumeau, C.; Chenuel, B. The Fundamentals of Respiratory Physiology to Manage the COVID-19 Pandemic: An Overview. Front. Physiol. 2021, 11, 615690. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Falcó-Pegueroles, A.; Rosa, D.; Tolotti, A.; Graffigna, G.; Bonetti, L. The Psychosocial Impact of Flu Influenza Pandemics on Healthcare Workers and Lessons Learnt for the COVID-19 Emergency: A Rapid Review. Int. J. Public Health 2020, 65, 1205–1216. [Google Scholar] [CrossRef] [PubMed]
- Villa, G.; Pennestrì, F.; Rosa, D.; Giannetta, N.; Sala, R.; Mordacci, R.; Manara, D.F. Moral Distress in Community and Hospital Settings for the Care of Elderly People. A Grounded Theory Qualitative Study. Healthcare 2021, 9, 1307. [Google Scholar] [CrossRef]
- Falcó-Pegueroles, A.; Zuriguel-Pérez, E.; Via-Clavero, G.; Bosch-Alcaraz, A.; Bonetti, L. Ethical Conflict during COVID-19 Pandemic: The Case of Spanish and Italian Intensive Care Units. Int. Nurs. Rev. 2021, 68, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Manara, D.F.; Villa, G.; Korelic, L.; Arrigoni, C.; Dellafiore, F.; Milani, V.; Ghizzardi, G.; Magon, A.; Giannetta, N.; Caruso, R. One-Week Longitudinal Daily Description of Moral Distress, Coping, and General Health in Healthcare Workers during the First Wave of the COVID-19 Outbreak in Italy: A Quantitative Diary Study. Acta Bio-Med. Atenei Parm. 2021, 92, e2021461. [Google Scholar] [CrossRef]
- Vergano, M.; Bertolini, G.; Giannini, A.; Gristina, G.R.; Livigni, S.; Mistraletti, G.; Riccioni, L.; Petrini, F. Siaarti Recommendations for the Allocation of Intensive Care Treatments in Exceptional, Resource-Limited Circumstances. Minerva Anestesiol. 2020, 86, 469–472. [Google Scholar] [CrossRef]
- Raus, K.; Mortier, E.; Eeckloo, K. Ethical Issues in Managing the COVID-19 Pandemic. Bioethics 2021, 35, 581–588. [Google Scholar] [CrossRef]
- McKenna, H. Covid-19: Ethical Issues for Nurses. Int. J. Nurs. Stud. 2020, 110, 103673. [Google Scholar] [CrossRef]
- Morley, G.; Grady, C.; McCarthy, J.; Ulrich, C.M. Covid-19: Ethical Challenges for Nurses. Hastings Cent. Rep. 2020, 50, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Lusignani, M.; Giannì, M.L.; Re, L.G.; Buffon, M.L. Moral Distress among Nurses in Medical, Surgical and Intensive-Care Units. J. Nurs. Manag. 2017, 25, 477–485. [Google Scholar] [CrossRef] [PubMed]
- McAndrew, N.S.; Leske, J.; Schroeter, K. Moral Distress in Critical Care Nursing: The State of the Science. Nurs. Ethics 2018, 25, 552–570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delfrate, F.; Ferrara, P.; Spotti, D.; Terzoni, S.; Lamiani, G.; Canciani, E.; Bonetti, L. Moral Distress (MD) and Burnout in Mental Health Nurses: A Multicenter Survey. Med. Lav. 2018, 109, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Fumis, R.R.L.; Junqueira Amarante, G.A.; de Fátima Nascimento, A.; Vieira Junior, J.M. Moral Distress and Its Contribution to the Development of Burnout Syndrome among Critical Care Providers. Ann. Intensive Care 2017, 7, 71. [Google Scholar] [CrossRef] [Green Version]
- McCarthy, J.; Gastmans, C. Moral Distress: A Review of the Argument-Based Nursing Ethics Literature. Nurs. Ethics 2015, 22, 131–152. [Google Scholar] [CrossRef] [PubMed]
- Simonovich, S.D.; Webber-Ritchey, K.J.; Spurlark, R.S.; Florczak, K.; Mueller Wiesemann, L.; Ponder, T.N.; Reid, M.; Shino, D.; Stevens, B.R.; Aquino, E.; et al. Moral Distress Experienced by US Nurses on the Frontlines During the COVID-19 Pandemic: Implications for Nursing Policy and Practice. SAGE Open Nurs. 2022, 8, 237796082210910. [Google Scholar] [CrossRef]
- Bayerle, H.; Ike, J.; Logan, R.; Parker, R. Sophocles’ Philoctetes and Moral Injury in the COVID-19 Pandemic. J. Health Commun. 2022, 27, 134–139. [Google Scholar] [CrossRef]
- Silverman, H.J.; Kheirbek, R.E.; Moscou-Jackson, G.; Day, J. Moral Distress in Nurses Caring for Patients with Covid-19. Nurs. Ethics 2021, 28, 1137–1164. [Google Scholar] [CrossRef]
- Donkers, M.A.; Gilissen, V.J.H.S.; Candel, M.J.J.M.; van Dijk, N.M.; Kling, H.; Heijnen-Panis, R.; Pragt, E.; van der Horst, I.; Pronk, S.A.; van Mook, W.N.K.A. Moral Distress and Ethical Climate in Intensive Care Medicine during COVID-19: A Nationwide Study. BMC Med. Ethics 2021, 22, 73. [Google Scholar] [CrossRef]
- Bianchi, M.; Prandi, C.; Bonetti, L. Experience of Middle Management Nurses during the COVID-19 Pandemic in Switzerland: A Qualitative Study. J. Nurs. Manag. 2021, 29, 1956–1964. [Google Scholar] [CrossRef] [PubMed]
- Rosa, D.; Villa, G.; Giannetta, N.; Dionisi, S.; Togni, S.; Bonetti, L.; Terzoni, S.; Di Muzio, M.; Di Simone, E. Tackling the Italian Emergency 2019-NCoV: Nurses’ Knowledge, Attitudes and Behaviors: What We Know about the COVID-19? Acta Biomed. Atenei Parm. 2022, 93, e2022010. [Google Scholar] [CrossRef]
- Balice-Bourgois, C.; Bonetti, L.; Tolotti, A.; Liptrott, S.J.; Villa, M.; Luca, C.E.; Steiner, L.M.; Biegger, A.; Goncalves, S.; Moser, L.; et al. Experiences and Needs of Patients, Caregivers and Nurses during the COVID-19 Pandemic: Study Protocol for a Mixed-Methods Multicentre Study. Int. J. Environ. Res. Public. Health 2022, 19, 12838. [Google Scholar] [CrossRef] [PubMed]
- Sheather, J.; Fidler, H. Covid-19 Has Amplified Moral Distress in Medicine. BMJ 2021, 372, n28. [Google Scholar] [CrossRef]
- Corley, M. Moral Distress of Critical Care Nurses. Am. J. Crit. Care 1995, 4, 280–285. [Google Scholar] [CrossRef]
- Jameton, A. Nursing Practice, the Ethical Issues. Int. J. Nurs. Stud. 1984, 22, 343. [Google Scholar] [CrossRef]
- Epstein, E.G.; Delgado, S. Understanding and Addressing Moral Distress. Online J. Issue Nurs. 2010, 15. [Google Scholar] [CrossRef]
- Epstein, E.G.; Hamric, A.B. Moral Distress, Moral Residue, and the Crescendo Effect. J. Clin. Ethics 2009, 20, 330–342. [Google Scholar]
- Smith, J.; Flowers, P.; Larkin, M. Interpretative Phenomenological Analysis: Theory, Method and Research; SAGE Publications: Thousand Oaks, CA, USA, 2009; Volume 6. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [Green Version]
- Wray, N.; Markovic, M.; Manderson, L. “Researcher Saturation”: The Impact of Data Triangulation and Intensive-Research Practices on the Researcher and Qualitative Research Process. Qual. Health Res. 2007, 17, 1392–1402. [Google Scholar] [CrossRef]
- Morse, J.M.; Barrett, M.; Mayan, M.; Olson, K.; Spiers, J. Verification Strategies for Establishing Reliability and Validity in Qualitative Research. Int. J. Qual. Methods 2002, 1, 13–22. [Google Scholar] [CrossRef]
- Rubin, H.; Rubin, I. Qualitative Interviewing: The Art of Hearing Data, 2nd ed.; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2005; ISBN 978-0-7619-2075-5. [Google Scholar]
- Long, T.; Johnson, M. Rigour, Reliability and Validity in Qualitative Research. Clin. Eff. Nurs. 2000, 4, 30–37. [Google Scholar] [CrossRef]
- Spiers, J.; Smith, J.A.; Simpson, P.; Nicholls, A.R. The Treatment Experiences of People Living with Ileostomies: An Interpretative Phenomenological Analysis. J. Adv. Nurs. 2016, 72, 2662–2671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bruce, S.; Allen, D. Moral Distress: One Unit’s Recognition and Mitigation of This Problem. Clin. J. Oncol. Nurs. 2020, 24, 16–18. [Google Scholar] [CrossRef] [PubMed]
- De Villers, M.J.; DeVon, H.A. Moral Distress and Avoidance Behavior in Nurses Working in Critical Care and Noncritical Care Units. Nurs. Ethics 2013, 20, 589–603. [Google Scholar] [CrossRef] [Green Version]
- Azoulay, E.; Cariou, A.; Bruneel, F.; Demoule, A.; Kouatchet, A.; Reuter, D.; Souppart, V.; Combes, A.; Klouche, K.; Argaud, L.; et al. Symptoms of Anxiety, Depression, and Peritraumatic Dissociation in Critical Care Clinicians Managing Patients with COVID-19. A Cross-Sectional Study. Am. J. Respir. Crit. Care Med. 2020, 202, 1388–1398. [Google Scholar] [CrossRef] [PubMed]
- Crowe, S.; Howard, A.F.; Vanderspank-Wright, B.; Gillis, P.; McLeod, F.; Penner, C.; Haljan, G. The Effect of COVID-19 Pandemic on the Mental Health of Canadian Critical Care Nurses Providing Patient Care during the Early Phase Pandemic: A Mixed Method Study. Intensive Crit. Care Nurs. 2021, 63, 102999. [Google Scholar] [CrossRef] [PubMed]
- Miljeteig, I.; Forthun, I.; Hufthammer, K.O.; Engelund, I.E.; Schanche, E.; Schaufel, M.; Onarheim, K.H. Priority-Setting Dilemmas, Moral Distress and Support Experienced by Nurses and Physicians in the Early Phase of the COVID-19 Pandemic in Norway. Nurs. Ethics 2021, 28, 66–81. [Google Scholar] [CrossRef]
- Shen, X.; Zou, X.; Zhong, X.; Yan, J.; Li, L. Psychological Stress of ICU Nurses in the Time of COVID-19. Crit. Care 2020, 24, 200. [Google Scholar] [CrossRef]
- Alharbi, J.; Jackson, D.; Usher, K. Compassion Fatigue in Critical Care Nurses: An Integrative Review of the Literature. Saudi Med. J. 2019, 40, 1087–1097. [Google Scholar] [CrossRef]
- Gill, S.; Adenan, A.M.; Ali, A.; Ismail, N.A.S. Living through the COVID-19 Pandemic: Impact and Lessons on Dietary Behavior and Physical Well-Being. Int. J. Environ. Res. Public Health 2022, 19, 642. [Google Scholar] [CrossRef] [PubMed]
- Rolandi, S.; Villa, G.; D’Aloia, P.; Gengo, V.; Negro, A.; Manara, D.F. COVID-19: An Italian Hospital Response From the Nursing Perspective. Nurs. Adm. Q. 2021, 45, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Henrich, N.J.; Dodek, P.M.; Gladstone, E.; Alden, L.; Keenan, S.P.; Reynolds, S.; Rodney, P. Consequences of Moral Distress in the Intensive Care Unit: A Qualitative Study. Am. J. Crit. Care 2017, 26, e48–e57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seyle, H. The Stress of Life; McGraw-Hill: New York, NY, USA, 1956. [Google Scholar]
- Negro, A.; Mucci, M.; Beccaria, P.; Borghi, G.; Capocasa, T.; Cardinali, M.; Pasculli, N.; Ranzani, R.; Villa, G.; Zangrillo, A. Introducing the Video Call to Facilitate the Communication between Health Care Providers and Families of Patients in the Intensive Care Unit during COVID-19 Pandemia. Intensive Crit. Care Nurs. 2020, 60, 102893. [Google Scholar] [CrossRef] [PubMed]
- Giannetta, N.; Villa, G.; Pennestrì, F.; Sala, R.; Mordacci, R.; Manara, D.F. Instruments to Assess Moral Distress among Healthcare Workers: A Systematic Review of Measurement Properties. Int. J. Nurs. Stud. 2020, 111, 103767. [Google Scholar] [CrossRef] [PubMed]
- Lamiani, G.; Ciconali, M.; Argentero, P.; Vegni, E. Clinicians’ Moral Distress and Family Satisfaction in the Intensive Care Unit. J. Health Psychol. 2020, 25, 1894–1904. [Google Scholar] [CrossRef]
- Villa, M.; Balice-Bourgois, C.; Tolotti, A.; Falcó-Pegueroles, A.; Barello, S.; Luca, E.C.; Clivio, L.; Biegger, A.; Valcarenghi, D.; Bonetti, L. Ethical Conflict and Its Psychological Correlates among Hospital Nurses in the Pandemic: A Cross-Sectional Study within Swiss COVID-19 and Non-COVID-19 Wards. Int. J. Environ. Res. Public. Health 2021, 18, 12012. [Google Scholar] [CrossRef]
- Gobbi, P.; Castoldi, M.G.; Alagna, R.A.; Brunoldi, A.; Pari, C.; Gallo, A.; Magri, M.; Marioni, L.; Muttillo, G.; Passoni, C.; et al. Validity of the Italian Code of Ethics for Everyday Nursing Practice. Nurs. Ethics 2018, 25, 906–917. [Google Scholar] [CrossRef]
- Marcomini, I.; Destrebecq, A.; Rosa, D.; Terzoni, S. Self-Reported Skills for Ensuring Patient Safety and Quality of Care among Italian Nursing Students: A Descriptive Cross-Sectional Study. Int. J. Health Promot. Educ. 2021, 60, 67–78. [Google Scholar] [CrossRef]
- Choe, K.; Kang, Y.; Park, Y. Moral Distress in Critical Care Nurses: A Phenomenological Study. J. Adv. Nurs. 2015, 71, 1684–1693. [Google Scholar] [CrossRef]
- Mealer, M.; Moss, M. Moral Distress in ICU Nurses. Intensive Care Med. 2016, 42, 1615–1617. [Google Scholar] [CrossRef] [PubMed]
| Questions |
|---|
| 1. Could he talk about you? |
| 2. How would you describe yourself as a nurse? |
| 3. What was the period of the COVID-19 pandemic like for you? |
| a. What was your experience in your private life? |
| b. What was your experience in your working life? |
| 4. Could you tell us what kind of experience was the COVID-19 pandemic for you with respect to your moral or ethical perspective? |
| 5. What influenced your decisions from an ethical or moral perspective during the period of the COVID-19 pandemic? |
| 6. Could you tell us about situations in which you disagreed with your team about what was ethically or morally correct during the period of the COVID-19 pandemic? |
| 7. How did this experience influence you? |
| Female | 9 |
| Male | 7 |
| With partner | 7 |
| Single | 9 |
| Age (Mean) | 38.03 (Range 25–54) |
| Years working experiences | 14.52 (Range 1–33) |
| Years working experience ICU (Mean) | 1.77 (Range 3 months to 8 years) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosa, D.; Bonetti, L.; Villa, G.; Allieri, S.; Baldrighi, R.; Elisei, R.F.; Ripa, P.; Giannetta, N.; Amigoni, C.; Manara, D.F. Moral Distress of Intensive Care Nurses: A Phenomenological Qualitative Study Two Years after the First Wave of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 15057. https://doi.org/10.3390/ijerph192215057
Rosa D, Bonetti L, Villa G, Allieri S, Baldrighi R, Elisei RF, Ripa P, Giannetta N, Amigoni C, Manara DF. Moral Distress of Intensive Care Nurses: A Phenomenological Qualitative Study Two Years after the First Wave of the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2022; 19(22):15057. https://doi.org/10.3390/ijerph192215057
Chicago/Turabian StyleRosa, Debora, Loris Bonetti, Giulia Villa, Sara Allieri, Riccardo Baldrighi, Rolando Francesco Elisei, Paola Ripa, Noemi Giannetta, Carla Amigoni, and Duilio Fiorenzo Manara. 2022. "Moral Distress of Intensive Care Nurses: A Phenomenological Qualitative Study Two Years after the First Wave of the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 19, no. 22: 15057. https://doi.org/10.3390/ijerph192215057





