The Difference in Electromyographic Activity While Wearing a Medical Mask in Women with and without Temporomandibular Disorders
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Research Protocol
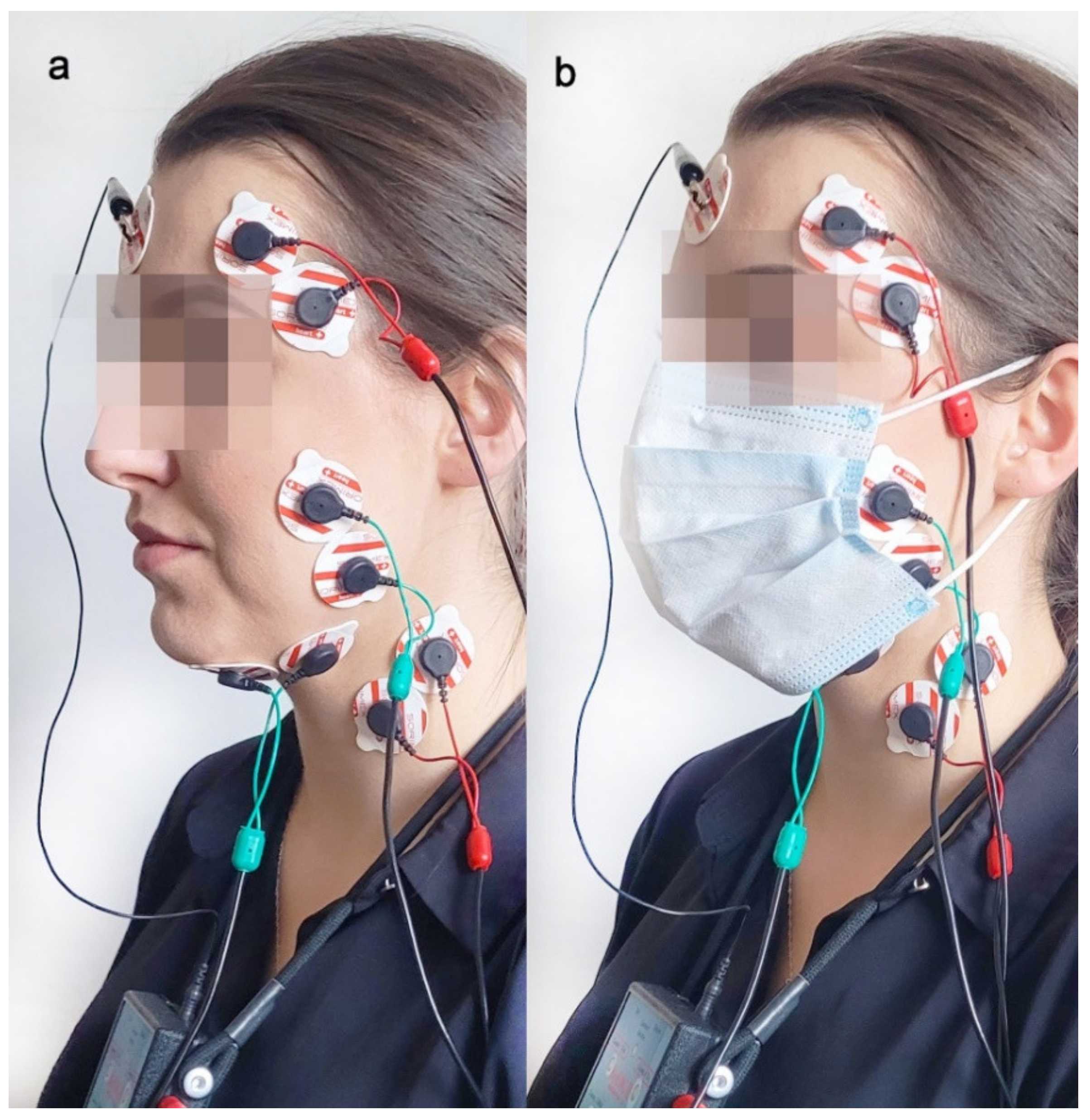
2.3. Electromyographic Examination
2.4. sEMG Signal Processing and Statistical Calculations
3. Results
3.1. Group Overview
3.2. Electromyographic Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rahmani, A.M.; Mirmahaleh, S.Y.H. Coronavirus Disease (COVID-19) Prevention and Treatment Methods and Effective Parameters: A Systematic Literature Review. Sustain. Cities Soc. 2021, 64, 102568. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, M.; Beyrer, C.; Goosby, E. Masks Do More Than Protect Others During COVID-19: Reducing the Inoculum of SARS-CoV-2 to Protect the Wearer. J. Gen. Intern. Med. 2020, 35, 3063–3066. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.-M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.-H.; et al. An Evidence Review of Face Masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118. [Google Scholar] [CrossRef] [PubMed]
- Josef Hemmer, C.; Hufert, F.; Siewert, S.; Reisinger, E. Protection from COVID-19. Dtsch. Arztebl. Int. 2021, 118, 59–65. [Google Scholar] [CrossRef]
- Shenal, B.V.; Radonovich, L.J.; Cheng, J.; Hodgson, M.; Bender, B.S. Discomfort and Exertion Associated with Prolonged Wear of Respiratory Protection in a Health Care Setting. J. Occup. Environ. Hyg. 2011, 9, 59–64. [Google Scholar] [CrossRef]
- Ong, J.J.Y.; Bharatendu, C.; Goh, Y.; Tang, J.Z.Y.; Sooi, K.W.X.; Tan, Y.L.; Tan, B.Y.Q.; Teoh, H.-L.; Ong, S.T.; Allen, D.M.; et al. Headaches Associated with Personal Protective Equipment—A Cross-Sectional Study Among Frontline Healthcare Workers during COVID-19. Headache 2020, 60, 864–877. [Google Scholar] [CrossRef] [Green Version]
- Rosner, E. Adverse Effects of Prolonged Mask Use among Healthcare Professionals during COVID-19. J. Infect. Dis. Epidemiol. 2020, 6, 130. [Google Scholar] [CrossRef]
- Serresse, L.; Simon-Tillaux, N.; Decavèle, M.; Gay, F.; Nion, N.; Lavault, S.; Guerder, A.; Châtelet, A.; Dabi, F.; Demoule, A.; et al. Lifting Dyspnoea Invisibility: COVID-19 Face Masks, the Experience of Breathing Discomfort, and Improved Lung Health Perception—A French Nationwide Survey. Eur. Respir. J. 2022, 59, 2101459. [Google Scholar] [CrossRef]
- Tasic-Kostov, M.; Martinović, M.; Ilic, D.; Cvetkovic, M. Cotton versus Medical Face Mask Influence on Skin Characteristics during COVID-19 Pandemic: A Short-term Study. Skin Res. Technol. 2022, 28, 66–70. [Google Scholar] [CrossRef]
- Ginszt, M.; Zieliński, G.; Szkutnik, J.; Wójcicki, M.; Baszczowski, M.; Litko-Rola, M.; Rózyło-Kalinowska, I.; Majcher, P. The Effects of Wearing a Medical Mask on the Masticatory and Neck Muscle Activity in Healthy Young Women. J. Clin. Med. 2022, 11, 303. [Google Scholar] [CrossRef]
- Durham, J.; Wassell, R. Recent Advancements in Temporomandibular Disorders (TMDs). Rev. Pain 2011, 5, 18–25. [Google Scholar] [CrossRef] [Green Version]
- Zieliński, G.; Byś, A.; Szkutnik, J.; Majcher, P.; Ginszt, M. Electromyographic Patterns of Masticatory Muscles in Relation to Active Myofascial Trigger Points of the Upper Trapezius and Temporomandibular Disorders. Diagnostics 2021, 11, 580. [Google Scholar] [CrossRef]
- Tecco, S.; Tetè, S.; D’Attilio, M.; Perillo, L.; Festa, F. Surface Electromyographic Patterns of Masticatory, Neck, and Trunk Muscles in Temporomandibular Joint Dysfunction Patients Undergoing Anterior Repositioning Splint Therapy. Eur. J. Orthod. 2008, 30, 592–597. [Google Scholar] [CrossRef] [Green Version]
- Osiewicz, M.A.; Lobbezoo, F.; Loster, B.W.; Wilkosz, M.; Naeije, M.; Ohrbach, R. Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD): The Polish Version of a Dual-Axis System for the Diagnosis of TMD.* RDC/TMD Form. Open J. Stomatol. 2013, 66, 576–649. [Google Scholar] [CrossRef]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of Recommendations for SEMG Sensors and Sensor Placement Procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [Green Version]
- Ginszt, M.; Zieliński, G. Novel Functional Indices of Masticatory Muscle Activity. J. Clin. Med. 2021, 10, 1440. [Google Scholar] [CrossRef]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect Size Estimates: Current Use, Calculations, and Interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef] [Green Version]
- Lenhard, W.; Lenhard, A. Calculation of Effect Sizes. Psychometrica 2016. [Google Scholar] [CrossRef]
- Tian, L.; Li, X.; Qi, F.; Tang, Q.-Y.; Tang, V.; Liu, J.; Li, Z.; Cheng, X.; Li, X.; Shi, Y.; et al. Calibrated Intervention and Containment of the COVID-19 Pandemic. arXiv 2020, arXiv:2003.07353. [Google Scholar]
- Epstein, D.; Korytny, A.; Isenberg, Y.; Marcusohn, E.; Zukermann, R.; Bishop, B.; Minha, S.; Raz, A.; Miller, A. Return to Training in the COVID-19 Era: The Physiological Effects of Face Masks during Exercise. Scand. J. Med. Sci. Sports 2021, 31, 70–75. [Google Scholar] [CrossRef]
- Fikenzer, S.; Uhe, T.; Lavall, D.; Rudolph, U.; Falz, R.; Busse, M.; Hepp, P.; Laufs, U. Effects of Surgical and FFP2/N95 Face Masks on Cardiopulmonary Exercise Capacity. Clin. Res. Cardiol. 2020, 109, 1522–1530. [Google Scholar] [CrossRef] [PubMed]
- Goh, D.Y.T.; Mun, M.W.; Lee, W.L.J.; Teoh, O.H.; Rajgor, D.D. A Randomised Clinical Trial to Evaluate the Safety, Fit, Comfort of a Novel N95 Mask in Children. Sci. Rep. 2019, 9, 18952. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kyung, S.Y.; Kim, Y.; Hwang, H.; Park, J.-W.; Jeong, S.H. Risks of N95 Face Mask Use in Subjects with COPD. Respir. Care 2020, 65, 658–664. [Google Scholar] [CrossRef] [PubMed]
- Rebmann, T.; Carrico, R.; Wang, J. Physiologic and Other Effects and Compliance with Long-Term Respirator Use among Medical Intensive Care Unit Nurses. Am. J. Infect. Control. 2013, 41, 1218–1223. [Google Scholar] [CrossRef]
- Ramirez-Moreno, J.M.; Ceberino, D.; Gonzalez Plata, A.; Rebollo, B.; Macias Sedas, P.; Hariramani, R.; Roa, A.M.; Constantino, A.B. Mask-Associated ‘de Novo’ Headache in Healthcare Workers during the COVID-19 Pandemic. Occup. Environ. Med. 2021, 78, 548–554. [Google Scholar] [CrossRef]
- Kisielinski, K.; Giboni, P.; Prescher, A.; Klosterhalfen, B.; Graessel, D.; Funken, S.; Kempski, O.; Hirsch, O. Is a Mask That Covers the Mouth and Nose Free from Undesirable Side Effects in Everyday Use and Free of Potential Hazards? Int. J. Environ. Res. Public Health 2021, 18, 4344. [Google Scholar] [CrossRef]
- Guo, S.-X.; Li, B.-Y.; Zhang, Y.; Zhou, L.-J.; Liu, L.; Widmalm, S.-E.; Wang, M.-Q. An Electromyographic Study on the Sequential Recruitment of Bilateral Sternocleidomastoid and Masseter Muscle Activity during Gum Chewing. J. Oral Rehabil. 2017, 44, 594–601. [Google Scholar] [CrossRef]
- Strini, P.J.S.A.; Strini, P.J.S.A.; Barbosa, T.d.S.; Gavião, M.B.D. Assessment of Thickness and Function of Masticatory and Cervical Muscles in Adults with and without Temporomandibular Disorders. Arch. Oral Biol. 2013, 58, 1100–1108. [Google Scholar] [CrossRef]
- Pallegama, R.W.; Ranasinghe, A.W.; Weerasinghe, V.S.; Sitheeque, M.A.M. Influence of Masticatory Muscle Pain on Electromyographic Activities of Cervical Muscles in Patients with Myogenous Temporomandibular Disorders. J. Oral Rehabil. 2004, 31, 423–429. [Google Scholar] [CrossRef]
- Li, G.; Wang, S.; Li, M.; Duan, Y.Y. Towards Real-Life EEG Applications: Novel Superporous Hydrogel-Based Semi-Dry EEG Electrodes Enabling Automatically ‘Charge–Discharge’ Electrolyte. J. Neural Eng. 2021, 18, 046016. [Google Scholar] [CrossRef]

| Healthy Group n = 60 | TMD Group n = 55 | Z | p | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | |||
| Age (years) | 23.73 | 2.61 | 23.52 | 2.32 | −0.17 | 0.86 |
| Weight (kg) | 60.19 | 8.70 | 61.68 | 11.19 | 0.11 | 0.91 |
| Height (cm) | 168.10 | 6.39 | 168.39 | 6.37 | 0.39 | 0.69 |
| BMI (kg/m2) | 21.28 | 2.83 | 21.70 | 3.46 | 0.32 | 0.75 |
| MMO (mm) | 48.73 | 6.08 | 45.76 | 7.98 | −1.92 | 0.06 |
| No Mask Measurement TMD Group (n = 55) | Medical Mask Measurement TMD Group (n = 55) | Z | p/ES | ||||
|---|---|---|---|---|---|---|---|
| M (µV) | SD (µV) | M (µV) | SD (µV) | ||||
| Rest | TA R | 3.15 | 2.35 | 2.62 | 2.27 | 1.38 | 0.17 |
| TA L | 3.41 | 2.74 | 2.57 | 2.06 | 2.28 | 0.02 */0.24 | |
| TA Mean | 3.28 | 2.18 | 2.59 | 1.93 | 2.14 | 0.03 */0.23 | |
| MM R | 2.45 | 1.50 | 1.89 | 0.84 | 2.34 | 0.02 */0.25 | |
| MM L | 2.29 | 1.39 | 1.88 | 0.98 | 1.63 | 0.10 | |
| MM Mean | 2.37 | 1.32 | 1.89 | 0.76 | 1.86 | 0.06 | |
| SCM R | 1.35 | 0.53 | 1.18 | 0.35 | 1.57 | 0.12 | |
| SCM L | 1.45 | 0.62 | 1.32 | 0.49 | 1.22 | 0.22 | |
| SCM Mean | 1.40 | 0.53 | 1.25 | 0.37 | 1.44 | 0.15 | |
| DA R | 2.08 | 0.94 | 2.25 | 1.63 | 0.12 | 0.91 | |
| DA L | 2.01 | 0.83 | 2.12 | 1.43 | 0.76 | 0.45 | |
| DA Mean | 2.05 | 0.83 | 2.19 | 1.42 | 0.56 | 0.57 | |
| TA R | 127.79 | 76.96 | 116.41 | 66.71 | 0.83 | 0.40 | |
| Clenching in the intercuspal position | TA L | 123.71 | 67.36 | 109.34 | 67.94 | 1.26 | 0.21 |
| TA Mean | 125.75 | 67.25 | 112.88 | 64.05 | 1.04 | 0.30 | |
| MM R | 137.97 | 107.10 | 115.60 | 98.81 | 1.46 | 0.15 | |
| MM L | 132.51 | 101.91 | 111.82 | 94.83 | 1.31 | 0.19 | |
| MM Mean | 135.24 | 101.98 | 113.71 | 94.59 | 1.44 | 0.15 | |
| SCM R | 8.89 | 7.55 | 7.87 | 7.26 | 1.29 | 0.20 | |
| SCM L | 8.57 | 8.05 | 10.95 | 26.47 | 0.41 | 0.68 | |
| SCM Mean | 8.73 | 7.57 | 9.41 | 15.03 | 0.89 | 0.37 | |
| DA R | 19.30 | 12.05 | 16.95 | 11.48 | 1.47 | 0.14 | |
| DA L | 17.40 | 13.73 | 15.53 | 12.51 | 0.95 | 0.34 | |
| DA Mean | 18.35 | 12.24 | 16.24 | 11.40 | 1.43 | 0.15 | |
| Clenching on dental cotton rollers | TA R | 137.44 | 160.23 | 110.52 | 51.47 | 0.57 | 0.57 |
| TA L | 113.10 | 54.86 | 104.95 | 56.65 | 0.96 | 0.34 | |
| TA Mean | 125.27 | 91.17 | 107.73 | 51.45 | 0.74 | 0.46 | |
| MM R | 173.14 | 161.56 | 144.30 | 92.06 | 0.89 | 0.37 | |
| MM L | 148.03 | 88.07 | 133.65 | 81.21 | 0.90 | 0.37 | |
| MM Mean | 160.58 | 110.38 | 138.97 | 84.20 | 1.03 | 0.30 | |
| SCM R | 10.79 | 7.54 | 9.45 | 6.70 | 1.31 | 0.19 | |
| SCM L | 10.21 | 7.23 | 9.19 | 6.80 | 0.85 | 0.40 | |
| SCM Mean | 10.50 | 7.08 | 9.32 | 6.39 | 1.03 | 0.30 | |
| DA R | 21.31 | 11.37 | 19.29 | 10.09 | 1.00 | 0.32 | |
| DA L | 18.84 | 11.05 | 15.88 | 8.79 | 1.50 | 0.13 | |
| DA Mean | 20.07 | 10.55 | 17.59 | 8.63 | 1.35 | 0.18 | |
| Maximum mouth opening | TA R | 6.89 | 3.83 | 6.85 | 3.75 | 0.07 | 0.94 |
| TA L | 6.87 | 3.91 | 6.72 | 3.77 | 0.09 | 0.93 | |
| TA Mean | 6.88 | 3.50 | 6.78 | 3.28 | 0.07 | 0.94 | |
| MM R | 7.65 | 5.67 | 7.67 | 6.36 | 0.29 | 0.77 | |
| MM L | 7.98 | 7.82 | 7.73 | 7.58 | 0.44 | 0.66 | |
| MM Mean | 7.81 | 6.60 | 7.70 | 6.87 | 0.36 | 0.72 | |
| SCM R | 8.90 | 7.46 | 8.63 | 6.65 | −0.01 | 0.99 | |
| SCM L | 8.00 | 5.60 | 8.10 | 5.22 | −0.27 | 0.79 | |
| SCM Mean | 8.45 | 6.34 | 8.36 | 5.67 | −0.12 | 0.90 | |
| DA R | 72.65 | 44.04 | 77.29 | 41.11 | −0.84 | 0.40 | |
| DA L | 77.40 | 48.17 | 77.88 | 42.32 | −0.54 | 0.59 | |
| DA Mean | 75.03 | 44.16 | 77.59 | 39.00 | −0.75 | 0.45 | |
| No Mask Measurement Healthy Group (n = 60) | Medical Mask Measurement Healthy Group (n = 60) | Z | p/ES | ||||
|---|---|---|---|---|---|---|---|
| M (µV) | SD (µV) | M (µV) | SD (µV) | ||||
| Rest | TA R | 2.60 | 1.93 | 2.10 | 1.29 | 1.50 | 0.13 |
| TA L | 2.57 | 1.50 | 2.17 | 1.46 | 1.90 | 0.06 | |
| TA Mean | 2.58 | 1.48 | 2.14 | 1.17 | 1.78 | 0.08 | |
| MM R | 2.00 | 1.09 | 1.74 | 1.09 | 2.08 | 0.04 */0.25 | |
| MM L | 2.20 | 1.27 | 1.86 | 1.49 | 2.45 | 0.01 */0.24 | |
| MM Mean | 2.10 | 1.05 | 1.80 | 1.19 | 2.43 | 0.02 */0.26 | |
| SCM R | 1.17 | 0.32 | 1.12 | 0.32 | 1.10 | 0.27 | |
| SCM L | 1.32 | 0.42 | 1.23 | 0.40 | 1.29 | 0.20 | |
| SCM Mean | 1.24 | 0.33 | 1.17 | 0.30 | 0.99 | 0.32 | |
| DA R | 1.91 | 1.05 | 1.92 | 1.12 | 0.33 | 0.74 | |
| DA L | 1.87 | 1.07 | 1.83 | 1.05 | 0.25 | 0.81 | |
| DA Mean | 1.89 | 1.04 | 1.87 | 1.06 | 0.23 | 0.82 | |
| TA R | 147.70 | 89.48 | 130.58 | 81.23 | 1.08 | 0.28 | |
| Clenching in the intercuspal position | TA L | 140.25 | 74.83 | 124.06 | 70.26 | 1.06 | 0.29 |
| TA Mean | 143.97 | 79.13 | 127.32 | 73.97 | 1.06 | 0.29 | |
| MM R | 150.77 | 99.07 | 125.60 | 91.15 | 1.67 | 0.10 | |
| MM L | 146.23 | 102.84 | 124.72 | 92.69 | 1.33 | 0.19 | |
| MM Mean | 148.50 | 97.97 | 125.16 | 89.43 | 1.48 | 0.14 | |
| SCM R | 10.81 | 8.14 | 8.52 | 5.83 | 1.66 | 0.10 | |
| SCM L | 10.68 | 8.17 | 8.80 | 6.24 | 1.27 | 0.20 | |
| SCM Mean | 10.75 | 7.78 | 8.66 | 5.54 | 1.41 | 0.16 | |
| DA R | 22.06 | 14.68 | 19.62 | 13.46 | 0.98 | 0.33 | |
| DA L | 24.38 | 19.84 | 19.53 | 15.04 | 1.50 | 0.13 | |
| DA Mean | 23.22 | 15.48 | 19.58 | 13.28 | 1.33 | 0.19 | |
| Clenching on dental cotton rollers | TA R | 132.67 | 76.61 | 133.72 | 76.23 | −0.25 | 0.80 |
| TA L | 126.42 | 67.38 | 127.60 | 67.55 | −0.15 | 0.88 | |
| TA Mean | 129.54 | 70.06 | 130.66 | 69.39 | −0.21 | 0.83 | |
| MM R | 167.28 | 91.75 | 160.27 | 79.63 | 0.15 | 0.88 | |
| MM L | 163.60 | 95.43 | 155.42 | 85.41 | 0.15 | 0.88 | |
| MM Mean | 165.44 | 90.53 | 157.85 | 78.08 | 0.22 | 0.83 | |
| SCM R | 12.71 | 7.62 | 13.76 | 14.97 | 0.68 | 0.50 | |
| SCM L | 12.17 | 7.12 | 11.81 | 7.94 | 0.45 | 0.66 | |
| SCM Mean | 12.44 | 6.96 | 12.78 | 9.56 | 0.48 | 0.63 | |
| DA R | 22.89 | 11.46 | 22.32 | 10.55 | 0.23 | 0.82 | |
| DA L | 24.73 | 14.44 | 23.14 | 14.58 | 0.88 | 0.38 | |
| DA Mean | 23.81 | 11.98 | 22.73 | 11.71 | 0.55 | 0.58 | |
| Maximum mouth opening | TA R | 7.44 | 4.50 | 10.05 | 19.98 | −0.09 | 0.93 |
| TA L | 7.11 | 4.74 | 7.04 | 4.97 | 0.57 | 0.57 | |
| TA Mean | 7.28 | 4.23 | 8.54 | 10.75 | 0.09 | 0.93 | |
| MM R | 9.65 | 9.05 | 10.80 | 10.73 | −0.31 | 0.76 | |
| MM L | 8.82 | 6.49 | 9.91 | 7.76 | −0.16 | 0.87 | |
| MM Mean | 9.23 | 7.46 | 10.35 | 8.91 | −0.27 | 0.79 | |
| SCM R | 9.49 | 6.74 | 11.63 | 11.27 | −0.77 | 0.44 | |
| SCM L | 9.53 | 8.03 | 10.91 | 10.99 | −0.58 | 0.56 | |
| SCM Mean | 9.51 | 7.07 | 11.27 | 10.69 | −0.55 | 0.58 | |
| DA R | 80.12 | 40.79 | 84.24 | 42.03 | −0.52 | 0.60 | |
| DA L | 78.91 | 40.53 | 86.01 | 42.14 | −0.86 | 0.39 | |
| DA Mean | 79.51 | 38.66 | 85.13 | 39.75 | −0.66 | 0.51 | |
| No Mask Measurement (n = 55) | Medical Mask Measurement (n = 55) | Z | p/ES | ||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Clenching in the intercuspal position | FCI TA R | 63.55 | 57.45 | 10.72 | 7.49 | 7.26 | 0.00 */0.80 |
| FCI TA L | 61.62 | 62.80 | 9.83 | 8.23 | 7.26 | 0.00 */0.80 | |
| FCI TA Total | 59.04 | 55.23 | 10.18 | 7.42 | 7.38 | 0.00 */0.82 | |
| FCI MM R | 78.60 | 99.26 | 66.24 | 57.52 | −0.07 | 0.94 | |
| FCI MM L | 73.09 | 71.39 | 68.81 | 67.72 | 0.56 | 0.57 | |
| FCI MM Total | 73.80 | 81.34 | 63.83 | 58.01 | 0.43 | 0.67 | |
| FCI SCM R | 7.09 | 6.89 | 77.58 | 95.38 | −7.84 | 0.00 */0.87 | |
| FCI SCM L | 6.37 | 6.53 | 74.43 | 81.53 | −7.76 | 0.00 */0.86 | |
| FCI SCM Total | 6.68 | 6.59 | 73.72 | 84.80 | −7.94 | 0.00 */0.88 | |
| FCI DA R | 10.72 | 7.49 | 6.95 | 6.25 | 3.61 | 0.00 */0.40 | |
| FCI DA L | 9.83 | 8.23 | 9.39 | 26.94 | 3.23 | 0.00 */0.36 | |
| FCI DA Total | 10.18 | 7.42 | 8.10 | 15.55 | 3.71 | 0.00 */0.41 | |
| Clenching on dental cotton rollers | FCI TA R | 61.14 | 53.59 | 61.01 | 43.82 | −0.51 | 0.61 |
| FCI TA L | 55.01 | 53.46 | 64.98 | 59.10 | −1.17 | 0.24 | |
| FCI TA Total | 55.30 | 49.76 | 59.27 | 45.17 | −1.04 | 0.30 | |
| FCI MM R | 104.85 | 172.97 | 94.97 | 83.12 | −1.05 | 0.29 | |
| FCI MM L | 80.95 | 59.48 | 87.65 | 70.28 | −0.47 | 0.64 | |
| FCI MM Total | 87.07 | 85.73 | 87.64 | 72.04 | −0.78 | 0.44 | |
| FCI SCM R | 8.42 | 6.01 | 8.47 | 6.12 | 0.05 | 0.96 | |
| FCI SCM L | 7.61 | 5.84 | 7.42 | 5.83 | 0.25 | 0.81 | |
| FCI SCM Total | 7.93 | 5.76 | 7.76 | 5.44 | 0.19 | 0.85 | |
| FCI DA R | 11.67 | 6.87 | 10.59 | 7.47 | 1.11 | 0.27 | |
| FCI DA L | 10.50 | 6.62 | 9.38 | 6.33 | 0.87 | 0.38 | |
| FCI DA Total | 10.98 | 6.36 | 9.83 | 6.42 | 0.97 | 0.33 | |
| Maximum mouth opening | FOI TA R | 3.21 | 2.24 | 3.68 | 2.52 | −1.17 | 0.24 |
| FOI TA L | 2.93 | 2.36 | 4.01 | 3.58 | −1.53 | 0.13 | |
| FOI TA Total | 2.92 | 2.02 | 3.69 | 2.66 | −1.62 | 0.11 | |
| FOI MM R | 4.08 | 3.74 | 5.01 | 4.95 | −1.37 | 0.17 | |
| FOI MM L | 4.66 | 5.14 | 5.14 | 4.84 | −1.18 | 0.24 | |
| FOI MM Total | 4.21 | 4.20 | 4.88 | 4.60 | −1.19 | 0.23 | |
| FOI SCM R | 7.03 | 5.84 | 7.71 | 6.16 | −1.24 | 0.21 | |
| FOI SCM L | 6.05 | 4.45 | 6.65 | 4.62 | −0.94 | 0.35 | |
| FOI SCM Total | 6.43 | 4.78 | 6.99 | 4.74 | −1.14 | 0.25 | |
| FOI DA R | 40.82 | 32.53 | 42.13 | 26.81 | −0.68 | 0.50 | |
| FOI DA L | 44.46 | 40.74 | 45.17 | 29.97 | −0.81 | 0.42 | |
| FOI DA Total | 3.21 | 2.24 | 3.68 | 2.52 | −1.17 | 0.24 | |
| No Mask Measurement (n = 60) | Medical Mask Measurement (n = 60) | Z | p/ES | ||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Clenching in the intercuspal position | FCI TA R | 74.62 | 55.54 | 13.62 | 10.31 | 8.16 | 0.00 */0.86 |
| FCI TA L | 70.54 | 49.09 | 15.08 | 14.57 | 7.66 | 0.00 */0.81 | |
| FCI TA Total | 68.24 | 45.44 | 14.31 | 11.18 | 8.15 | 0.00 */0.86 | |
| FCI MM R | 97.52 | 93.64 | 84.33 | 82.60 | 0.76 | 0.45 | |
| FCI MM L | 88.94 | 82.61 | 83.88 | 75.35 | 0.30 | 0.77 | |
| FCI MM Total | 90.76 | 83.24 | 78.40 | 70.87 | 0.71 | 0.48 | |
| FCI SCM R | 10.03 | 9.17 | 94.88 | 89.62 | −8.35 | 0.00 */0.88 | |
| FCI SCM L | 8.97 | 8.57 | 95.90 | 97.09 | −7.77 | 0.00 */0.82 | |
| FCI SCM Total | 9.40 | 8.26 | 92.75 | 85.48 | −8.13 | 0.00 */0.86 | |
| FCI DA R | 13.62 | 10.31 | 8.06 | 5.68 | 3.34 | 0.00 */0.35 | |
| FCI DA L | 15.08 | 14.57 | 7.73 | 6.05 | 4.21 | 0.00 */0.45 | |
| FCI DA Total | 14.31 | 11.18 | 7.77 | 5.26 | 3.89 | 0.00 */0.41 | |
| Clenching on dental cotton rollers | FCI TA R | 65.02 | 46.62 | 80.23 | 67.41 | −1.38 | 0.17 |
| FCI TA L | 62.86 | 39.76 | 80.67 | 61.44 | −1.14 | 0.26 | |
| FCI TA Total | 60.42 | 37.55 | 74.22 | 52.07 | −1.32 | 0.19 | |
| FCI MM R | 102.15 | 80.10 | 113.17 | 75.37 | −1.19 | 0.23 | |
| FCI MM L | 97.89 | 81.92 | 113.40 | 98.29 | −1.04 | 0.30 | |
| FCI MM Total | 97.68 | 76.96 | 110.06 | 77.66 | −1.20 | 0.23 | |
| FCI SCM R | 11.75 | 8.75 | 13.06 | 13.87 | −0.32 | 0.75 | |
| FCI SCM L | 10.18 | 7.55 | 10.45 | 7.99 | 0.00 | 1.00 | |
| FCI SCM Total | 10.83 | 7.61 | 11.66 | 9.77 | −0.12 | 0.90 | |
| FCI DA R | 14.22 | 8.03 | 14.71 | 9.38 | 0.10 | 0.92 | |
| FCI DA L | 15.24 | 10.24 | 14.77 | 10.79 | 0.62 | 0.53 | |
| FCI DA Total | 14.65 | 8.49 | 14.61 | 9.34 | 0.38 | 0.71 | |
| Maximum mouth opening | FOI TA R | 3.79 | 2.88 | 7.19 | 20.51 | −1.35 | 0.18 |
| FOI TA L | 3.54 | 3.15 | 4.32 | 3.63 | −1.63 | 0.10 | |
| FOI TA Total | 3.45 | 2.41 | 4.79 | 5.03 | −1.65 | 0.10 | |
| FOI MM R | 6.43 | 9.19 | 8.27 | 12.39 | −1.51 | 0.13 | |
| FOI MM L | 5.53 | 6.26 | 7.44 | 8.41 | −1.86 | 0.06 | |
| FOI MM Total | 5.85 | 7.36 | 7.73 | 10.13 | −1.56 | 0.12 | |
| FOI SCM R | 8.46 | 5.90 | 10.99 | 10.51 | −0.93 | 0.35 | |
| FOI SCM L | 7.62 | 6.17 | 9.18 | 8.09 | −1.24 | 0.21 | |
| FOI SCM Total | 7.93 | 5.81 | 9.87 | 8.50 | −1.00 | 0.32 | |
| FOI DA R | 51.19 | 34.77 | 54.12 | 34.31 | −0.72 | 0.47 | |
| FOI DA L | 51.64 | 34.77 | 56.64 | 36.13 | −1.03 | 0.30 | |
| FOI DA Total | 51.17 | 33.80 | 55.03 | 34.43 | −0.81 | 0.42 | |
| Healthy Group (n = 60) | TMD Group (n = 55) | Z | p/ES | ||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Clenching in the intercuspal position | FCI TA R | 74.62 | 55.54 | 63.55 | 57.45 | −1.46 | 0.14 |
| FCI TA L | 70.54 | 49.09 | 61.62 | 62.80 | −1.84 | 0.07 | |
| FCI TA Total | 68.24 | 45.44 | 59.04 | 55.23 | −1.85 | 0.06 | |
| FCI MM R | 97.52 | 93.64 | 78.60 | 99.26 | −1.79 | 0.07 | |
| FCI MM L | 88.94 | 82.61 | 73.09 | 71.39 | −1.30 | 0.19 | |
| FCI MM Total | 90.76 | 83.24 | 73.80 | 81.34 | −1.65 | 0.10 | |
| FCI SCM R | 10.03 | 9.17 | 7.09 | 6.89 | −2.57 | 0.01 */0.28 | |
| FCI SCM L | 8.97 | 8.57 | 6.37 | 6.53 | −2.61 | 0.01 */0.28 | |
| FCI SCM Total | 9.40 | 8.26 | 6.68 | 6.59 | −2.82 | 0.00 */0.31 | |
| FCI DA R | 13.62 | 10.31 | 10.72 | 7.49 | −1.42 | 0.16 | |
| FCI DA L | 15.08 | 14.57 | 9.83 | 8.23 | −2.76 | 0.01 */0.30 | |
| FCI DA Total | 14.31 | 11.18 | 10.18 | 7.42 | −2.24 | 0.02 */0.24 | |
| Clenching on dental cotton rollers | FCI TA R | 65.02 | 46.62 | 61.14 | 53.59 | −1.00 | 0.32 |
| FCI TA L | 62.86 | 39.76 | 55.01 | 53.46 | −2.02 | 0.04 */0.22 | |
| FCI TA Total | 60.42 | 37.55 | 55.30 | 49.76 | −1.63 | 0.10 | |
| FCI MM R | 102.15 | 80.10 | 104.85 | 172.97 | −2.12 | 0.03 */0.23 | |
| FCI MM L | 97.89 | 81.92 | 80.95 | 59.48 | −1.09 | 0.28 | |
| FCI MM Total | 97.68 | 76.96 | 87.07 | 85.73 | −1.59 | 0.11 | |
| FCI SCM R | 11.75 | 8.75 | 8.42 | 6.01 | −3.11 | 0.00 */0.34 | |
| FCI SCM L | 10.18 | 7.55 | 7.61 | 5.84 | −2.83 | 0.00 */0.31 | |
| FCI SCM Total | 10.83 | 7.61 | 7.93 | 5.76 | −3.19 | 0.00 */0.35 | |
| FCI DA R | 14.22 | 8.03 | 11.67 | 6.87 | −1.87 | 0.06 | |
| FCI DA L | 15.24 | 10.24 | 10.50 | 6.62 | −3.24 | 0.00 */0.35 | |
| FCI DA Total | 14.65 | 8.49 | 10.98 | 6.36 | −2.72 | 0.01 */0.29 | |
| Maximum mouth opening | FOI TA R | 3.79 | 2.88 | 3.21 | 2.24 | −1.08 | 0.28 |
| FOI TA L | 3.54 | 3.15 | 2.93 | 2.36 | −0.87 | 0.39 | |
| FOI TA Total | 3.45 | 2.41 | 2.92 | 2.02 | −1.11 | 0.27 | |
| FOI MM R | 6.43 | 9.19 | 4.08 | 3.74 | −1.93 | 0.05 | |
| FOI MM L | 5.53 | 6.26 | 4.66 | 5.14 | −0.83 | 0.40 | |
| FOI MM Total | 5.85 | 7.36 | 4.21 | 4.20 | −1.50 | 0.13 | |
| FOI SCM R | 8.46 | 5.90 | 7.03 | 5.84 | −2.16 | 0.03 */0.23 | |
| FOI SCM L | 7.62 | 6.17 | 6.05 | 4.45 | −1.72 | 0.09 | |
| FOI SCM Total | 7.93 | 5.81 | 6.43 | 4.78 | −1.95 | 0.05 | |
| FOI DA R | 51.19 | 34.77 | 40.82 | 32.53 | −1.71 | 0.09 | |
| FOI DA L | 51.64 | 34.77 | 44.46 | 40.74 | −1.37 | 0.17 | |
| FOI DA Total | 51.17 | 33.80 | 42.23 | 35.71 | −1.58 | 0.11 | |
| Healthy Group (n = 60) | TMD Group (n = 55) | Z | p/ES | ||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Clenching in the intercuspal position | FCI TA R | 13.62 | 10.31 | 10.72 | 7.49 | −1.42 | 0.16 |
| FCI TA L | 15.08 | 14.57 | 9.83 | 8.23 | −2.76 | 0.01 | |
| FCI TA Total | 14.31 | 11.18 | 10.18 | 7.42 | −2.24 | 0.02 */0.24 | |
| FCI MM R | 84.33 | 82.60 | 66.24 | 57.52 | −1.25 | 0.21 | |
| FCI MM L | 83.88 | 75.35 | 68.81 | 67.72 | −1.35 | 0.18 | |
| FCI MM Total | 78.40 | 70.87 | 63.83 | 58.01 | −1.45 | 0.15 | |
| FCI SCM R | 94.88 | 89.62 | 77.58 | 95.38 | −1.48 | 0.14 | |
| FCI SCM L | 95.90 | 97.09 | 74.43 | 81.53 | −1.48 | 0.14 | |
| FCI SCM Total | 92.75 | 85.48 | 73.72 | 84.80 | −1.42 | 0.15 | |
| FCI DA R | 8.06 | 5.68 | 6.95 | 6.25 | −1.72 | 0.09 | |
| FCI DA L | 7.73 | 6.05 | 9.39 | 26.94 | −1.80 | 0.07 | |
| FCI DA Total | 7.77 | 5.26 | 8.10 | 15.55 | −1.83 | 0.07 | |
| Clenching on dental cotton rollers | FCI TA R | 80.23 | 67.41 | 61.01 | 43.82 | −1.78 | 0.08 |
| FCI TA L | 80.67 | 61.44 | 64.98 | 59.10 | −1.82 | 0.07 | |
| FCI TA Total | 74.22 | 52.07 | 59.27 | 45.17 | −1.93 | 0.05 | |
| FCI MM R | 113.17 | 75.37 | 94.97 | 83.12 | −2.01 | 0.04 */0.22 | |
| FCI MM L | 113.40 | 98.29 | 87.65 | 70.28 | −1.88 | 0.06 | |
| FCI MM Total | 110.06 | 77.66 | 87.64 | 72.04 | −2.06 | 0.04 */0.22 | |
| FCI SCM R | 13.06 | 13.87 | 8.47 | 6.12 | −3.22 | 0.00 */0.35 | |
| FCI SCM L | 10.45 | 7.99 | 7.42 | 5.83 | −3.13 | 0.00 */0.34 | |
| FCI SCM Total | 11.66 | 9.77 | 7.76 | 5.44 | −3.42 | 0.00 */0.37 | |
| FCI DA R | 14.71 | 9.38 | 10.59 | 7.47 | −2.63 | 0.01 */0.28 | |
| FCI DA L | 14.77 | 10.79 | 9.38 | 6.33 | −3.32 | 0.00 */0.36 | |
| FCI DA Total | 14.61 | 9.34 | 9.83 | 6.42 | −3.04 | 0.00 */0.33 | |
| Maximum mouth opening | FOI TA R | 7.19 | 20.51 | 3.68 | 2.52 | −1.06 | 0.29 |
| FOI TA L | 4.32 | 3.63 | 4.01 | 3.58 | −0.77 | 0.44 | |
| FOI TA Total | 4.79 | 5.03 | 3.69 | 2.66 | −0.98 | 0.33 | |
| FOI MM R | 8.27 | 12.39 | 5.01 | 4.95 | −2.21 | 0.03 */0.24 | |
| FOI MM L | 7.44 | 8.41 | 5.14 | 4.84 | −1.88 | 0.06 | |
| FOI MM Total | 7.73 | 10.13 | 4.88 | 4.60 | −2.11 | 0.04 */0.23 | |
| FOI SCM R | 10.99 | 10.51 | 7.71 | 6.16 | −1.85 | 0.06 | |
| FOI SCM L | 9.18 | 8.09 | 6.65 | 4.62 | −1.87 | 0.06 | |
| FOI SCM Total | 9.87 | 8.50 | 6.99 | 4.74 | −2.04 | 0.04 */0.22 | |
| FOI DA R | 54.12 | 34.31 | 42.13 | 26.81 | −1.99 | 0.05 */0.22 | |
| FOI DA L | 56.64 | 36.13 | 45.17 | 29.97 | −1.68 | 0.09 | |
| FOI DA Total | 55.03 | 34.43 | 43.00 | 25.80 | −1.83 | 0.07 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ginszt, M.; Zieliński, G.; Szkutnik, J.; Wójcicki, M.; Baszczowski, M.; Litko-Rola, M.; Zielińska, D.; Różyło-Kalinowska, I. The Difference in Electromyographic Activity While Wearing a Medical Mask in Women with and without Temporomandibular Disorders. Int. J. Environ. Res. Public Health 2022, 19, 15559. https://doi.org/10.3390/ijerph192315559
Ginszt M, Zieliński G, Szkutnik J, Wójcicki M, Baszczowski M, Litko-Rola M, Zielińska D, Różyło-Kalinowska I. The Difference in Electromyographic Activity While Wearing a Medical Mask in Women with and without Temporomandibular Disorders. International Journal of Environmental Research and Public Health. 2022; 19(23):15559. https://doi.org/10.3390/ijerph192315559
Chicago/Turabian StyleGinszt, Michał, Grzegorz Zieliński, Jacek Szkutnik, Marcin Wójcicki, Michał Baszczowski, Monika Litko-Rola, Diana Zielińska, and Ingrid Różyło-Kalinowska. 2022. "The Difference in Electromyographic Activity While Wearing a Medical Mask in Women with and without Temporomandibular Disorders" International Journal of Environmental Research and Public Health 19, no. 23: 15559. https://doi.org/10.3390/ijerph192315559








