Abstract
(1) Background: Emotional recognition (ER), the ability to read into others’ minds and recognize others’ emotional states, is important in social environment adaptation. Recently it has been found that ER difficulties affect patients with multiple sclerosis (pMS) and relate to different gray matter atrophy patterns from secondary progressive (SP-pMS) and relapsing–remitting (RR-pMS). The aim of this study was to compare the performances of the two MS phenotypes on the Reading the Mind in the Eyes test (RMEt) and other cognitive, mood and fatigue measures. We also examined associations between performance on the RMEt and cognitive, mood and fatigue variables. (2) Methods: A total of 43 pMS (27RR-pMS/16SP-pMS) underwent a clinical assessment, the RMEt, the cognitive battery, and completed mood and fatigue questionnaires. Both groups’ performances on the RMEt were then correlated with all these measures. (3) Results: the RMEt scores of RR-pMS were significantly correlated with the impairment degree in some cognitive scores. SP-pMS scores correlated mainly with fatigue, anxiety, anger and depression. (4) Conclusions: ER performances relate to cognitive aspects in RR-pMS, whereas mainly to mood outcomes in the SP-pMS group. We can hypothesize that deficits in ER are a further sign of disease progression. Our data support the different roles of cognitive and emotional deficits related to different disease courses and lesional correlates.
1. Introduction
Multiple sclerosis (MS) is a chronic inflammatory degenerative disease of the central nervous system. It is the main cause of non-traumatic disability among young adults and its course is highly variable and unpredictable. MS is characterized by focal and diffuse white matter damage, cortical lesions, cortical atrophy and microstructural abnormalities in deep gray matter (GM) that affect structural and functional connectivity between various brain regions [1,2].
From a clinical point of view, patients with MS (pMS) manifest a rather heterogeneous condition, characterized by cognitive, sensorimotor, visual, vegetative, cerebellar, psychological, social and emotional symptoms, which lead to functional disability and a reduced quality of life [3].
Among the mood disorders, anxiety and depression are commonly reported in pMS [4,5,6]. The first is associated with high levels of disability, progressive disease course [4], comorbid depressive symptoms [5,6] and female sex [5], while depression is associated with neuropathology [7,8], cognitive deficits [9,10] and poor social support [11].
Furthermore, from the emotional point of view, pMS may also have difficulty with anger management [12]. Benito-Leon and colleagues [13] observed higher levels of trait anger in pMS than in a healthy control group. However, other studies have not shown a clear increase in anger levels in MS compared to controls [12,14]; Nocentini et al. [12] reported that pMS had a greater tendency to withhold anger notwithstanding a lower level of control on it than the general population.
Fatigue is one of the most common symptoms experienced by up to 75–90% of pMS [15]. It is considered one of the most disabling symptoms of MS. It can drastically affect patients’ quality of life by also causing severe socioeconomic difficulties due to job loss [15].
Cognitive deficits affect 42–70% of people with MS with significant consequences on quality of life and social participation [16]. The most frequently compromised cognitive functions are memory, attention, information processing speed, abstract/conceptual reasoning and visuospatial skills; on the other hand, primary language skills, immediate and implicit memory and verbal intelligence seem less impaired [16,17]. Although the above-reported cognitive domains have been well studied in MS [18], little attention has been paid to social cognition (SC), defined as a multidimensional construct that encompasses the theory of mind (ToM), emotional recognition (ER) and empathy [19]. These processes allow humans to understand themselves and other individuals, to interact with them and to adaptively orient behaviors toward appropriate goals [20]. Interest in SC has grown over the past twenty years, to such an extent that in 2013 it was included in the latest revision of the Diagnostic and Statistical Manual of Mental Disorders as one of the six major neurocognitive domains, along with learning and memory, complex attention, executive function, perceptual–motor function and language.
In MS, studies conducted on SC have mainly focused on ER, which is the process of identifying human emotions from facial expressions [21], and on ToM, defined as the ability to decode and interpret the mental states of others and to use them to make inferences and predict their behaviors [22]. Two recent meta-analyses [23,24] confirmed the presence of significant deficits in ER and ToM in MS. In particular, in pMS, several researchers have observed difficulties in recognizing negative emotions [25,26,27] and in attributing mental states to others, in verbal and non-verbal ToM tasks [28,29,30]. SC deficits may be of similar magnitude to those observed in other cognitive domains [23] and may contribute to the interpersonal and psychosocial relationship difficulties complained of by pMS [31,32,33]. Aspects of SC (including ToM) and identification of others’ emotional expressions have also been reported to be disturbed in the pediatric onset of MS [34].
More recently, numerous studies have assessed the relationship between SC deficits and general cognitive impairment, revealing inconsistent results. For example, significant correlations have been reported between deficits in SC and processing speed [26,30,35,36,37], working memory [38,39,40,41] and problem-solving [37,41,42]. By contrast, others have found no relationship between social cognitive performance and general cognitive impairment [43,44,45,46]. Pitteri and colleagues [47] sought to overcome these contradictory results by studying performance in SC tasks in a group of relapsing–remitting MS patients (RR-pMS) without cognitive impairment. This study gave results in support of the independence of the SC from classic cognitive deficits: the RR-pMS, despite being cognitively preserved, showed a significantly lower performance than a paired group of healthy controls in ToM, ER and empathy tasks. The absence of association between SC and general cognitive functioning is also supported by a recent meta-analysis [48] conducted on 1708 pwMS and 1518 healthy controls.
Interestingly, in a previous study, we found that ER difficulties often affect MS patients with consequences on quality of life, psychosocial adaptation due to problems in understanding pragmatic language statements (such as irony), employment and interpersonal domains (such as personal relationships). ER difficulties were found to relate to a different GM atrophy pattern in secondary progressive (SP-pMS) and RR-pMS [49]. Furthermore, SP-pMS performed significantly worse than matched healthy controls in the emotional recognition task, while RR-pMS did not. We supposed that the different impairment in ER performance between RR-pMS and SP-pMS could depend on the demyelination and neurodegeneration of the cognitive component supporting the ability to process others’ mental states from facial expressions, in the initial stages of MS, and on the affective component in the secondary phase, following the work of Isernia and colleagues [50].
Considering these premises, we could speculate that a widespread pattern supporting SC functioning could have areas or circuits overlapping with those supporting other cognitive and mood functions. These overlapping areas or circuits, when interested in MS-related neurodegeneration, may deal with different patterns of impairment in each aspect of SC. If so, a clearer knowledge of the relationship between SC and other cognitive domains and mood aspects could be acquired, taking into consideration the above-reported different GM atrophy patterns in SP-pMS and RR-pMS. Therefore, the present study intends to explore how the already reported differences between the two main MS phenotypes relate to other important MS-related clinical aspects, such as cognition, mood and fatigue.
2. Materials and Methods
2.1. Participants
To consecutively be enrolled in this study, patients who attended the “Santa Lucia” Foundation MS Clinic had to satisfy the following inclusion criteria: (1) have a diagnosis of MS (McDonald’s criteria revised in 2011 by Polman [51]); (2) have an RR phenotype (MS in which patients have relapses of MS and periods of recovery and stability in between relapses) or SP phenotype (a progressive form of MS that involves fewer attacks, in which the disability gets steadily worse); (3) be 18–65 years old; (4) be native Italian speakers.
The exclusion criteria were: (1) a previous diagnosis of psychiatric or neurological disorders with the exception of MS or a severe systemic disease; (2) use of psychotropic drugs; (3) cognitive impairment severity interfering with the comprehension of tasks; (4) significant impairments in visual, auditory or linguistic functions interfering with the execution of tasks; (5) an MS relapse in the three months prior to their enrolment; (6) use of steroids over the previous month.
Due to the abovementioned criteria, the final sample of participants was 43 patients (27 RR-pMS and 16 SP-pMS). The principal demographic and clinical characteristics of all participants are summarized in Table 1. This study was approved by the Local Ethics Committee (CE/PROG.444-09), and all participants gave their written informed consent before taking part in the study.

Table 1.
Clinical and demographic data of the MS sample.
2.2. Procedures
After having signed the informed consent, patients underwent a clinical assessment with the Expanded Disability Status Scale (EDSS; [52]) by a certified physician and a cognitive assessment with the Italian version of the Minimal Assessment of Cognitive Functioning in Multiple Sclerosis battery (MACFIMS; [53,54]). This battery is composed of seven tests: the California Verbal Learning Test-2 (measurement of verbal learning and memory; CVLT-2); the Brief Visuospatial Memory Test-Revised (visuospatial memory test; BVMTR); the Symbol Digit Modalities Test (information processing speed; SDMT; oral version); the Benton Judgment of Line Orientation test (measures the accuracy of spatial orientation judgments; BJLO); the Controlled Oral Word Association Test (a measure of phonemic fluency; COWAT); the Delis–Kaplan Executive Function System Sorting Test (D-KEFS; a measure of executive functions efficiency); and the Paced Auditory Serial Addition Test 3-s version (a measure of working memory; PASAT). A global cognitive impairment index was also computed for the variables included in the MACFIMS and the calculation was derived from Argento and colleagues [54].
The EDSS is a scale helpful for quantifying disability in MS and monitoring changes in the level of disability over time. The score is based on measures of impairment in eight functional systems: visual functions (problems with sight and visual field); brainstem functions (problems with speech, swallowing and nystagmus); pyramidal functions (muscle weakness or difficulty moving limbs); cerebellar functions (ataxia, loss of balance, coordination or tremor); sensory functions (numbness or loss of sensations); bowel and bladder functions; cerebral functions (problems with thinking and memory); ambulation. The EDSS scale ranges from 0 to 10, in 0.5-unit increments that represent higher levels of disability [52].
After that, pMS were asked to complete a mood assessment performed with the following questionnaires:
The State-Trait Anxiety Inventory (STAI-Y; [55]). This questionnaire is composed of two scales of 20 items each, referring to, respectively, state anxiety and trait anxiety. Total scores are calculated separately for two scales, with higher scores indicating higher anxiety severity.
The Beck Depression Inventory-fast screen (BDIfs; [56,57]). This is a seven-item questionnaire that assesses dysphoria, anhedonia, suicidal ideation and cognition-related symptoms on a three-point scale. The total score is calculated by summing the response given for each item, with higher scores indicating higher depression severity.
The Modified Impact Fatigue Scale (MFIS; [58]). This is a self-report questionnaire of 21 items rated on a 5-point scale (0 = “Never”; 4 = “Almost always”). The total MFIS score can range from 0 to 84 and is computed by adding the scores from the physical, cognitive and psychosocial subscales. Higher scores indicate greater fatigue.
The State-Trait Anger Expression Inventory-second edition (STAXI-II, [59]). This is a self-report questionnaire used for the assessment of anger levels and expressions. It is made up of 57 items rated on a four-point scale (1 = “Almost never”; 4 = “Almost always”). For each scale higher scores corresponded to higher levels of anger.
STAXI-II includes the seven scales described in Figure 1.
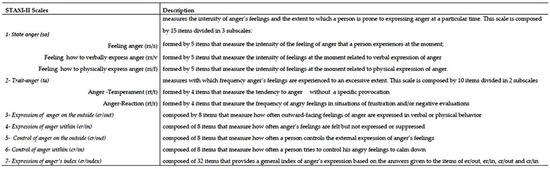
Figure 1.
STAXI-II questionnaire. Description of each scale.
For the aims of the study, we collected data only on three subscales of the STAXI-II: state anger, trait anger and expression of anger index.
To conclude, patients performed a test specifically directed to the assessment of ER: the Reading the Mind in the Eyes test (RMEt; [60,61]). This test consists of 36 black and white stimuli representing the eye region of different individuals (men and women) and four possible adjectives for each stimulus. Participants must examine the images and choose, for each one, which of the four presented adjectives correctly describes the mental state that the person in the photo is expressing (See Figure 2). For each participant, the total number of stimuli correctly recognized was corrected for demographic variables, according to Serafin and Surian’s procedures [62].
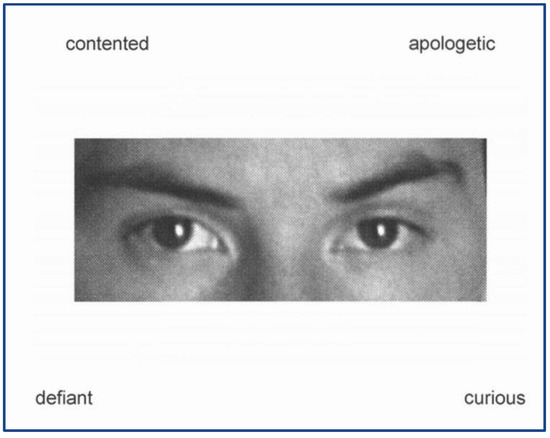
Figure 2.
Example figure of Reading the Mind test item.
2.3. Statistical Analysis
Demographic data were compared between RR-pMS and SP-pMS using independent sample t-tests for age and education, and a chi-squared test for gender (Table 1); t-tests were also used to test for group differences on cognitive and behavioral tests (Table 2). All cognitive and behavioral scores were corrected for the principal demographic variables (age, sex and education). No correction was made for clinical variables as the course diagnosis of MS already accounts for them. Both groups’ performances on the RMEt were then correlated with all these measures using Pearson correlation. For the purposes of this study, different types of statistical analysis were carried out using SPSS 18 (SPSS Inc., Chicago, IL, USA) and a significant threshold throughout this study will be set at p < 0.05.

Table 2.
Cognitive and mood assessment, and comparison between RR-pMS and SP-pMS based on t-test analysis.
3. Results
The results from the comparison of demographics between RR-pMS and SP-pMS revealed that the two samples were comparable in terms of sex and education, but differed significantly with regard to age, disease duration and EDSS score (Table 1), with SP-pMS having higher age, higher disability and higher disease duration.
Similarly, the comparison of cognitive, mood and fatigue scores (Table 2) proved significant differences between SP-pMS and RR-pMS for all cognitive scores except for BJLO (p > 0.05) with SP-pMS being more impaired than RR-pMS. A statistically significant difference was found between groups on fatigue (p = 0.001), though groups did not differ on anxiety, depression and anger (all p-values > 0.05). As expected, based on previous literature, the performances of RR-pMS and SP-pMS were significantly different (p = 0.005).
Analyses revealed that the RMEt scores of RR-pMS were significantly correlated with the impairment degree in some MACFIMS scores: CVLT-IR (r = −0.420; p = 0.029), D-KEFS card sorting 1 (r = −0.410; p = 0.034) and 2 (r = −0.488; p = 0.045), and the global degree of cognitive impairment (r = −0.431; p = 0.025; Table 3). The RMEt scores of SP-pMS correlated with the BVMT-IR score (r = −0.566; p = 0.018), but were also significantly correlated with fatigue (r = −0.692; p = 0.002), anxiety (STAI-Y1: r = −0.689, p = −0.002; STAI-Y2: r = −0.688, p = 0.002), depression (r = −0.687; p = 0.002), anger sa (r = −0.690; p = 0.002), anger ta (r = −0.683; p = 0.003) and anger Er/index (r = −0.691; p = 0.002; Table 3).

Table 3.
Pearson correlation coefficient and effect size between RMEt performance and cognitive and mood aspects for both RR-pMS and SP-pMS.
4. Discussion
Emotional recognition (ER), in terms of the ability to read into others’ minds and recognize others’ emotional states, plays an important role in social environment adaptation.
Recently, the efficiency of this SC component has gained wide importance as the recent COVID-19 pandemic has imposed the use of face masks. Within even basic conversations, this has required the ability to understand others’ mental states only by observing the eye regions, making the maintenance of appropriate social relationships for pMS even harder. In fact, as previously demonstrated, these patients have difficulties in ER explored by the RMEt to a different degree for the two main courses of the pathology [49].
The aim of this study was to understand how the already reported differences between the two main MS phenotypes relate to other important MS-related clinical aspects, such as cognition, mood and fatigue.
The differences found in the comparison of the two samples for clinical and demographic variables are those expected as the SP course follows the RR one. This implies a longer disease duration and a higher disability level in SP-pMS compared to RR-pMS. In addition, the differences found for cognitive scores and for cognitive impairment index reflect the higher disability of SP-pMS as it has been widely reported in the literature [53,63]. Furthermore, as found in a previous study, patients in the two courses also had significantly different RMEt scores, with RR-pMS performing better than SP-pMS [49].
The results of this study offer a possible explanation of the previously found pattern of differences in emotional recognition between RR-pMS and SP-pMS. In this study, ER performances relate mainly to cognitive aspects in RR-pMS: in particular, immediate recollection of verbal memory and abstract reasoning, two components that require the efficiency of executive functions in terms of attention and categorization [64,65]. The 16 words that compose the CVLT-2 pertain to four categories: this influences the performance according to how subjects can be facilitated in the memorization by the categorization process; this is the same process used in the execution of the D-KEFS card sorting tasks [66]. Furthermore, some studies on alexithymia (defined as the poor efficiency in inferring others’ emotions) have found an association with executive functions’ efficiency (EF) and between EF and memory [67].
Conversely, in SP-MS, ER performances are related mainly to mood aspects, especially with perceived fatigue, anxiety and anger management aspects. The relationship found between fatigue and RMEt scores is not new in the literature. A significant relationship was already found in a previous study on SC in pMS [43], in which the authors hypothesized a similar anatomopathological pattern for the two aspects. Following their explanation, fatigue and SC impairment are associated with reduced function of the right prefrontal and anterior cingulate cortex and structural loss of fiber integrity in the frontal white matter [43]. In our study, we found that this overlapping is specifically related to the SP course of MS.
Interestingly, a significant correlation was found between the performance on the RMEt and the levels of state and trait anger in SP-pMS: patients with higher levels of state anger, trait anger and global anger expression (Er-Index) have a lower ability to decode others’ emotions. Following the description by Spielberger [59], people with high scores in the Er-Index tend to experience strong feelings of anger, which can be either repressed or expressed through aggressive behaviors. These people display anger in many shades of behavior, probably experience extreme difficulty in establishing interpersonal relationships and are at risk of developing medical disorders [59]. This seems to be the case for MS patients and in particular, following actual results, for SP-pMS. Therefore, we can hypothesize that patients in the SP course have some emotional dysregulation, making them impaired in both managing their intense emotions and recognizing others.
The data of this study allow us to say that at least for ER (as a component of the SC) it seems that the impairment found in the two main courses of MS could be caused by the damage of different circuits. In general, given the correlations with some cognitive scales, we can argue that the efficiency of some components of the so-called “executive functions” seems to be necessary to correctly perform the RMEt. In addition to the integrity of the visual system, a categorization process could be needed in order to facilitate the comparison with previous knowledge stored in the memory and subsequently, to allow the correct labeling of that emotion.
This study has some limitations that should be considered. First of all, we have not included a control sample to support the results found within our sample. However, we felt that since we had already found a difference between healthy subjects and MS patients in a previous study, we did not need an additional control group. We also did not perform a regression analysis with all RMEt-associated variables included to find a regression model and did not choose a more conservative approach in interpreting the results. However, we believed that our sample size did not allow for this type of analysis and would have led to underestimating an effect that is present but would only be seen with a less conservative approach. Future research will try to overcome these limitations.
In this study, we primarily aimed to explore the possibility that different MS courses may show different impairments in different aspects of the emotional decoding process. We started with ER but expected to explore these eventual differences in other components of the SC.
We strongly expect that this can help clinicians and researchers resolve the debate on considering SC as a specific cognitive domain or secondary to the efficiency of other cognitive processes.
On the other side, this can help clinicians to better understand when patients could benefit the most from specific training on SC. Otherwise, they should be addressed to other clinical approaches (such as psychotherapy, mindfulness-based programs, etc.) when their social concerns are more linked to mood aspects (such as anxiety, depression and/or anger management dyscontrol).
Future studies are needed to explore the possibility that even other components of SC can follow the pattern of ER and to understand if we can consider this deficit in ER as a further sign of disease progression in MS.
5. Conclusions
To conclude, the results of this study, in line with what has been demonstrated before, support the hypothesis of a different role of deficits in cognitive and emotional aspects of the ER process depending on MS course and differences in lesion burden. This means that SC, and in particular the emotional recognition process, may be correlated with the damage of different circuits associated with RMEt performance emerging in the two courses of the disease. Therefore, we could state that patients in the two MS courses are differently impaired even in SC performances.
Author Contributions
O.A., conceptualization, project administration, and writing—original draft preparation; C.P., investigation, data curation, and writing—review and editing; M.B., formal analysis, data curation, and writing—review and editing; U.N., conceptualization and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study has been conceptualized according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of I.R.C.C.S. “Santa Lucia” Foundation (protocol code CE/PROG.698; 26 July 2018).
Informed Consent Statement
Informed consent form has been prepared and will be signed by all subjects involved in this study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- DeLuca, G.C.; Yates, R.L.; Beale, H.; Morrow, S.A. Cognitive impairment in multiple sclerosis: Clinical, radiologic and pathologic insights. Brain Pathol. 2015, 25, 79–98. [Google Scholar] [CrossRef] [PubMed]
- Di Filippo, M.; Portaccio, E.; Mancini, A.; Calabresi, P. Multiple sclerosis and cognition: Synaptic failure and network dysfunction. Nat. Rev. Neurosci. 2018, 19, 599–609. [Google Scholar] [CrossRef] [PubMed]
- Lode, K.; Bru, E.; Klevan, G.; Myhr, K.M.; Nyland, H.; Larsen, J.P. Coping with multiple sclerosis: A 5-year follow-up study. Acta Neurol. Scand. 2010, 122, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Askari, F.; Ghajarzadeh, M.; Mohammadifar, M.; Azimi, A.; Sahraian, M.A.; Owji, M. Anxiety in patients with multiple sclerosis: Association with disability, depression, disease type and sex. Acta Med. Iran. 2014, 52, 889–892. [Google Scholar] [PubMed]
- Giordano, A.; Granella, F.; Lugaresi, A.; Martinelli, V.; Trojano, M.; Confalonieri, P.; Radice, D.; Solari, A.; SIMS-Trial group. Anxiety and depression in multiple sclerosis patients around diagnosis. J. Neurol. Sci. 2011, 307, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Hartoonian, N.; Terrill, A.L.; Beier, M.L.; Turner, A.P.; Day, M.A.; Alschuler, K.N. Predictors of anxiety in multiple sclerosis. Rehabil. Psychol. 2015, 60, 91–98. [Google Scholar] [CrossRef]
- Rojas, J.I.; Sanchez, F.; Patrucco, L.; Miguez, J.; Besada, C.; Cristiano, E. Brain structural changes in patients in the early stages of multiple sclerosis with depression. Neurol. Res. 2017, 39, 596–600. [Google Scholar] [CrossRef]
- Van Geest, Q.; Boeschoten, R.E.; Keijzer, M.J.; Steenwijk, M.D.; Pouwels, P.J.; Twisk, J.W.; Smit, J.H.; Uitdehaag, B.M.; Geurts, J.J.; van Oppen, P.; et al. Fronto-limbic disconnection in patients with multiple sclerosis and depression. Mult. Scler. 2019, 25, 715–726. [Google Scholar] [CrossRef]
- Arnett, P.A.; Higginson, C.I.; Voss, W.D.; Wright, B.; Bender, W.I.; Wurst, J.M.; Tippin, J.M. Depressed mood in multiple sclerosis: Relationship to capacity-demanding memory and attentional functioning. Neuropsychology. 1999, 13, 434–446. [Google Scholar] [CrossRef]
- Feinstein, A. Mood disorders in multiple sclerosis and the effects on cognition. J. Neurol. Sci. 2006, 245, 63–66. [Google Scholar] [CrossRef]
- Gay, M.-C.; Vrignaud, P.; Garitte, C.; Meunier, C. Predictors of depression in multiple sclerosis patients. Acta Neurol. Scand. 2010, 121, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Nocentini, U.; Tedeschi, G.; Migliaccio, R.; Dinacci, D.; Lavorgna, L.; Bonavita, S.; Morra, V.B.; Comanducci, G.; Coniglio, G.; Livrea, P.; et al. An exploration of anger phenomenology in multiple sclerosis. Eur. J. Neurol. 2009, 16, 1312–1317. [Google Scholar] [CrossRef]
- Benito-León, J.; Labiano-Fontcuberta, A.; Mitchell, A.J.; Sara, M.-G.; Martínez-Martín, P. Multiple sclerosis is associated with high trait anger: A case-control study. J. Neurol. Sci. 2014, 340, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Laing, C.M. Emotional Skills and Quality of Life in Multiple Sclerosis. Ph.D. Thesis, University of Aberdeen, Aberdeen, UK, 2016. [Google Scholar]
- Ayache, S.S.; Chalah, M.A. Fatigue in multiple sclerosis—Insights into evaluation and management. Neurophysiol. Clin. 2017, 47, 139–171. [Google Scholar] [CrossRef]
- Chiaravalloti, N.D.; DeLuca, J. Cognitive impairment in multiple sclerosis. Lancet Neurol. 2008, 7, 1139–1151. [Google Scholar] [CrossRef]
- Rao, S.M.; Leo, G.J.; Bernardin, L.; Unverzagt, F. Cognitive dysfunction in multiple sclerosis. I. Frequency, patterns, and prediction. Neurology 1991, 41, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Mohr, D.C.; Cox, D. Multiple sclerosis: Empirical literature for the clinical health psychologist. J. Clin. Psychol. 2001, 57, 479–499. [Google Scholar] [CrossRef]
- Chalah, M.A.; Ayache, S.S. Deficits in Social Cognition: An Unveiled Signature of Multiple Sclerosis. J. Int. Neuropsychol. Soc. 2017, 23, 266–286. [Google Scholar] [CrossRef]
- Giazkoulidou, A.; Messinis, L.; Nasios, G. Cognitive functions and social cognition in multiple sclerosis: An overview. Hell. J. Nucl. Med. 2019, 22, 102–110. [Google Scholar]
- Niedenthal, P.M.; Brauer, M. Social functionality of human emotion. Annu. Rev. Psychol. 2012, 63, 259–285. [Google Scholar] [CrossRef]
- Doskas, T.; Vavougios, G.D.; Karampetsou, P.; Kormas, C.; Synadinakis, E.; Stavrogianni, K.; Sionidou, P.; Serdari, A.; Vorvolakos, T.; Iliopoulos, I.; et al. Neurocognitive impairment and social cognition in multiple sclerosis. Int. J. Neurosci. 2021, 25, 1229–1244. [Google Scholar] [CrossRef] [PubMed]
- Cotter, J.; Firth, J.; Enzinger, C.; Kontopantelis, E.; Yung, A.R.; Elliott, R.; Drake, R.J. Social cognition in multiple sclerosis: A systematic review and meta-analysis. Neurology 2016, 87, 1727–1736. [Google Scholar] [CrossRef]
- Bora, E.; Özakbaş, S.; Velakoulis, D.; Walterfang, M. Social Cognition in Multiple Sclerosis: A Meta-Analysis. Neuropsychol. Rev. 2016, 26, 160–172. [Google Scholar] [CrossRef]
- Beatty, W.W.; Orbelo, D.M.; Sorocco, K.H.; Ross, E.D. Comprehension of affective prosody in multiple sclerosis. Mult. Scler. J. 2003, 9, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Cecchetto, C.; Aiello, M.; D’Amico, D.; Cutuli, D.; Cargnelutti, D.; Eleopra, R.; Rumiati, R.I. Facial and bodily emotion recognition in multiple sclerosis: The role of alexithymia and other characteristics of the disease. J. Int. Neuropsychol. Soc. 2014, 20, 1004–1014. [Google Scholar] [CrossRef] [PubMed]
- Henry, A.; Tourbah, A.; Chaunu, M.-P.; Bakchine, S.; Montreuil, M. Social Cognition Abilities in Patients With Different Multiple Sclerosis Subtypes. J. Int. Neuropsychol. Soc. 2017, 23, 653–664. [Google Scholar] [CrossRef]
- Banati, M.; Sandor, J.; Mike, A.; Illes, E.; Bors, L.; Feldmann, A.; Herold, R.; Illes, Z. Social cognition and Theory of Mind in patients with relapsing-remitting multiple sclerosis. Eur. J. Neurol. 2010, 17, 426–433. [Google Scholar] [CrossRef]
- Henry, A.; Tourbah, A.; Chaunu, M.-P.; Rumbach, L.; Montreuil, M.; Bakchine, S. Social cognition impairments in relapsing-remitting multiple sclerosis. J. Int. Neuropsychol. Soc. 2011, 17, 1122–1131. [Google Scholar] [CrossRef]
- Pöttgen, J.; Dziobek, I.; Reh, S.; Heesen, C.; Gold, S.M. Impaired social cognition in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 2013, 84, 523–528. [Google Scholar] [CrossRef]
- Buhse, M. Assessment of caregiver burden in families of persons with multiple sclerosis. J. Neurosci. Nurs. 2008, 40, 25–31. [Google Scholar] [CrossRef]
- Krause, I.; Kern, S.; Horntrich, A.; Ziemssen, T. Employment status in multiple sclerosis: Impact of disease-specific and non-disease-specific factors. Mult. Scler. J. 2013, 19, 1792–1799. [Google Scholar] [CrossRef]
- Langdon, D.W. Cognition in multiple sclerosis. Curr. Opin. Neurol. 2011, 24, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Green, R.; Adler, A.; Banwell, B.L.; Fabri, T.L.; Yeh, E.A.; Collins, D.L.; Sled, J.G.; Narayanan, S.; Till, C. Involvement of the amygdala in memory and psychosocial functioning in pediatric-onset multiple sclerosis. Dev. Neuropsychol. 2018, 43, 524–534. [Google Scholar] [CrossRef] [PubMed]
- Bisecco, A.; Altieri, M.; Santangelo, G.; Di Nardo, F.; Docimo, R.; Caiazzo, G.; Capuano, R.; Pappacena, S.; d’Ambrosio, A.; Bonavita, S.; et al. Resting-State Functional Correlates of Social Cognition in Multiple Sclerosis: An Explorative Study. Front. Behav. Neurosci. 2020, 13, 276. [Google Scholar] [CrossRef] [PubMed]
- Czekóová, K.; Shaw, D.J.; Saxunová, K.; Dufek, M.; Mareček, R.; Vaníček, J.; Brázdil, M. Impaired Self-Other Distinction and Subcortical Gray-Matter Alterations Characterize Socio-Cognitive Disturbances in Multiple Sclerosis. Front. Neurol. 2019, 10, 525. [Google Scholar] [CrossRef] [PubMed]
- Henry, J.D.; Phillips, L.H.; Beatty, W.W.; McDonald, S.; Longley, W.A.; Joscelyne, A.; Rendell, P.G. Evidence for deficits in facial affect recognition and theory of mind in multiple sclerosis. J. Int. Neuropsychol. Soc. 2009, 15, 277–285. [Google Scholar] [CrossRef]
- Genova, H.M.; Cagna, C.J.; Chiaravalloti, N.D.; DeLuca, J.; Lengenfelder, J. Dynamic Assessment of Social Cognition in Individuals with Multiple Sclerosis: A Pilot Study. J. Int. Neuropsychol. Soc. 2016, 22, 83–88. [Google Scholar] [CrossRef]
- Lenne, B.; Barthélémy, R.; Nandrino, J.-L.; Sequeira, H.; Pinti, A.; Mecheri, H.; Kwiatkowski, A.; Hautecoeur, P. Impaired recognition of facial emotional expressions in multiple sclerosis. Neuropsychol. Trends 2014, 15, 67–83. [Google Scholar] [CrossRef]
- Raimo, S.; Trojano, L.; Pappacena, S.; Alaia, R.; Spitaleri, D.; Grossi, D.; Santangelo, G. Neuropsychological correlates of theory of mind deficits in patients with multiple sclerosis. Neuropsychology. 2017, 31, 811–821. [Google Scholar] [CrossRef]
- Dulau, C.; Deloire, M.; Diaz, H.; Saubusse, A.; Charre-Morin, J.; Prouteau, A.; Brochet, B. Social cognition according to cognitive impairment in different clinical phenotypes of multiple sclerosis. J. Neurol. 2017, 264, 740–748. [Google Scholar] [CrossRef]
- Pinto, C.; Gomes, F.; Moreira, I.; Rosa, B.; Santos, E.; Silva, A.M.; Cavaco, S. Emotion recognition in multiple sclerosis. J. Eye Track. Vis. Cogn. Emot. 2012, 2, 76–81. [Google Scholar]
- Neuhaus, M.; Bagutti, S.; Yaldizli, Ö.; Zwahlen, D.; Schaub, S.; Frey, B.; Fischer-Barnicol, B.; Burgunder, J.M.; Martory, M.D.; Pöttgen, J.; et al. Characterization of social cognition impairment in multiple sclerosis. Eur. J. Neurol. 2018, 25, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Roca, M.; Manes, F.; Gleichgerrcht, E.; Ibáñez, A.; de Toledo, M.E.G.; Marenco, V.; Bruno, D.; Torralva, T.; Sinay, V. Cognitive but not affective theory of mind deficits in mild relapsing-remitting multiple sclerosis. Cogn. Behav. Neurol. 2014, 27, 25–30. [Google Scholar] [CrossRef]
- Golde, S.; Heine, J.; Pöttgen, J.; Mantwill, M.; Lau, S.; Wingenfeld, K.; Otte, C.; Penner, I.K.; Engel, S.A.K.; Heeen, C.; et al. Distinct Functional Connectivity Signatures of Impaired Social Cognition in Multiple Sclerosis. Front. Neurol. 2020, 11, 507. [Google Scholar] [CrossRef] [PubMed]
- Batista, S.; Freitas, S.; Afonso, A.; Macário, C.; Sousa, L.; Cunha, L.; Santana, I. Theory of Mind and Executive Functions are Dissociated in Multiple Sclerosis. Arch. Clin. Neuropsychol. 2018, 33, 541–551. [Google Scholar] [CrossRef]
- Pitteri, M.; Genova, H.; Lengenfelder, J.; DeLuca, J.; Ziccardi, S.; Rossi, V.; Calabrese, M. Social cognition deficits and the role of amygdala in relapsing remitting multiple sclerosis patients without cognitive impairment. Mult. Scler. Relat. Disord. 2019, 29, 118–123. [Google Scholar] [CrossRef]
- Lin, X.; Zhang, X.; Liu, Q.; Zhao, P.; Zhong, J.; Pan, P.; Wang, G.; Yi, Z. Social cognition in multiple sclerosis and its subtypes: A meta-analysis. Mult. Scler. Relat. Disord. 2021, 52, 102973. [Google Scholar] [CrossRef]
- Argento, O.; Spanò, B.; Serra, L.; Incerti, C.C.; Bozzali, M.; Caltagirone, C.; Francia, A.; Fratino, M.; Nocentini, U.; Piacentini, C.; et al. Relapsing-remitting and secondary-progressive multiple sclerosis patients differ in decoding others’ emotions by their eyes. Eur. J. Neurol. 2022, 29, 505–514. [Google Scholar] [CrossRef]
- Isernia, S.; Baglio, F.; d’Arma, A.; Groppo, E.; Marchetti, A.; Massaro, D. Social Mind and Long-Lasting Disease: Focus on Affective and Cognitive Theory of Mind in Multiple Sclerosis. Front. Psychol. 2019, 10, 218. [Google Scholar] [CrossRef]
- Polman, C.H.; Reingold, S.C.; Banwell, B.; Clanet, M.; Cohen, J.A.; Filippi, M.; Fujihara, K.; Havrdova, E.; Hutchinson, M.; Kappos, L.; et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann. Neurol. 2011, 69, 292–302. [Google Scholar] [CrossRef]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef] [PubMed]
- Benedict, R.H.; Fischer, J.S.; Archibald, C.J.; Arnett, P.A.; Beatty, W.W.; Bobholz, J.; Chelune, G.J.; Fisk, J.D.; Langdon, D.W.; Caruso, L.; et al. Minimal neuropsychological assessment of MS patients: A consensus approach. Clin. Neuropsychol. 2002, 16, 381–397. [Google Scholar] [CrossRef] [PubMed]
- Argento, O.; Incerti, C.C.; Quartuccio, M.E.; Magistrale, G.; Francia, A.; Caltagirone, C.; Pisani, V.; Nocentini, U. The Italian validation of the minimal assessment of cognitive function in multiple sclerosis (MACFIMS) and the application of the Cognitive Impairment Index scoring procedure in MS patients. Neurol. Sci. 2018, 39, 1237–1244. [Google Scholar] [CrossRef] [PubMed]
- Spielberger, C.D. Manual for the State-Trait Anxiety Inventory (Form Y) (‘Self-Evaluation Questionnaire’); Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Beck, A.T.; Steer, R.A.; Brown, G.K. BDI-Fast Screen for Medical Patients: Manual; Psychological Corporation: San Antonio, TX, USA, 2000. [Google Scholar]
- Benedict, R.H.; Fishman, I.; McClellan, M.M.; Bakshi, R.; Weinstock-Guttman, B. Validity of the Beck Depression Inventory-Fast Screen in multiple sclerosis. Mult. Scler. 2003, 9, 393–396. [Google Scholar] [CrossRef]
- Fisk, J.D.; Ritvo, P.G.; Ross, L.; Haase, D.A.; Marrie, T.J.; Schlech, W.F. Measuring the functional impact of fatigue: Initial validation of the fatigue impact scale. Clin. Infect. Dis. 1994, 18 (Suppl. 1), S79–S83. [Google Scholar] [CrossRef] [PubMed]
- Spielberger, C.D. Staxi-2: State-Trait Anger Expression Inventory-2; Professional Manual; PAR, Psychological Assessment Resources: Odessa, FL, USA, 1999. [Google Scholar]
- Baron-Cohen, S.; Jolliffe, T.; Mortimore, C.; Robertson, M. Another advanced test of theory of mind: Evidence from very high functioning adults with autism or asperger syndrome. J. Child. Psychol. Psychiatry 1997, 38, 813–822. [Google Scholar] [CrossRef]
- Baron-Cohen, S.; Wheelwright, S.; Hill, J.; Raste, Y.; Plumb, I. The “Reading the Mind in the Eyes” Test revised version: A study with normal adults, and adults with Asperger syndrome or high-functioning autism. J. Child. Psychol. Psychiatry 2001, 42, 241–251. [Google Scholar] [CrossRef]
- Serafin, M.; Surian, L. Il test degli occhi: Uno strumento per valutare la “Teoria della Mente”. G. Ital. Psicol. 2004, 31, 839–862. [Google Scholar]
- Brochet, B.; Ruet, A. Cognitive impairment in multiple sclerosis with regards to disease duration and clinical phenotypes. Front. Neurol. 2019, 10, 261. [Google Scholar] [CrossRef]
- Argento, O.; Pisani, V.; Incerti, C.C.; Magistrale, G.; Caltagirone, C.; Nocentini, U. The California Verbal Learning Test-II: Normative data for two Italian alternative forms. Clin. Neuropsychol. 2014, 28 (Suppl. 1), 42–54. [Google Scholar] [CrossRef]
- Kramer, J.H.; Rosen, H.J.; Du, A.-T.; Schuff, N.; Hollnagel, C.; Weiner, M.W.; Miller, B.L.; Delis, D.C. Dissociations in hippocampal and frontal contributions to episodic memory performance. Neuropsychology 2005, 19, 799. [Google Scholar] [CrossRef] [PubMed]
- Mattioli, F.; Stampatori, C.; Bellomi, F.; Scarpazza, C.; Galli, P.; Guarneri, C.; Corso, B.; Montomoli, C.; Niccolai, C.; Goretti, B.; et al. Assessing executive function with the D-KEFS sorting test: Normative data for a sample of the Italian adult population. Neurol. Sci. 2014, 35, 1895–1902. [Google Scholar] [CrossRef] [PubMed]
- Correro, A.N.; Paitel, E.R.; Byers, S.J.; Nielson, K.A. The role of alexithymia in memory and executive functioning across the lifespan. Cogn. Emot. 2021, 35, 524–539. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).