Health-Related Quality of Life (HRQOL) Instruments and Mobility: A Systematic Review
Abstract
:1. Introduction
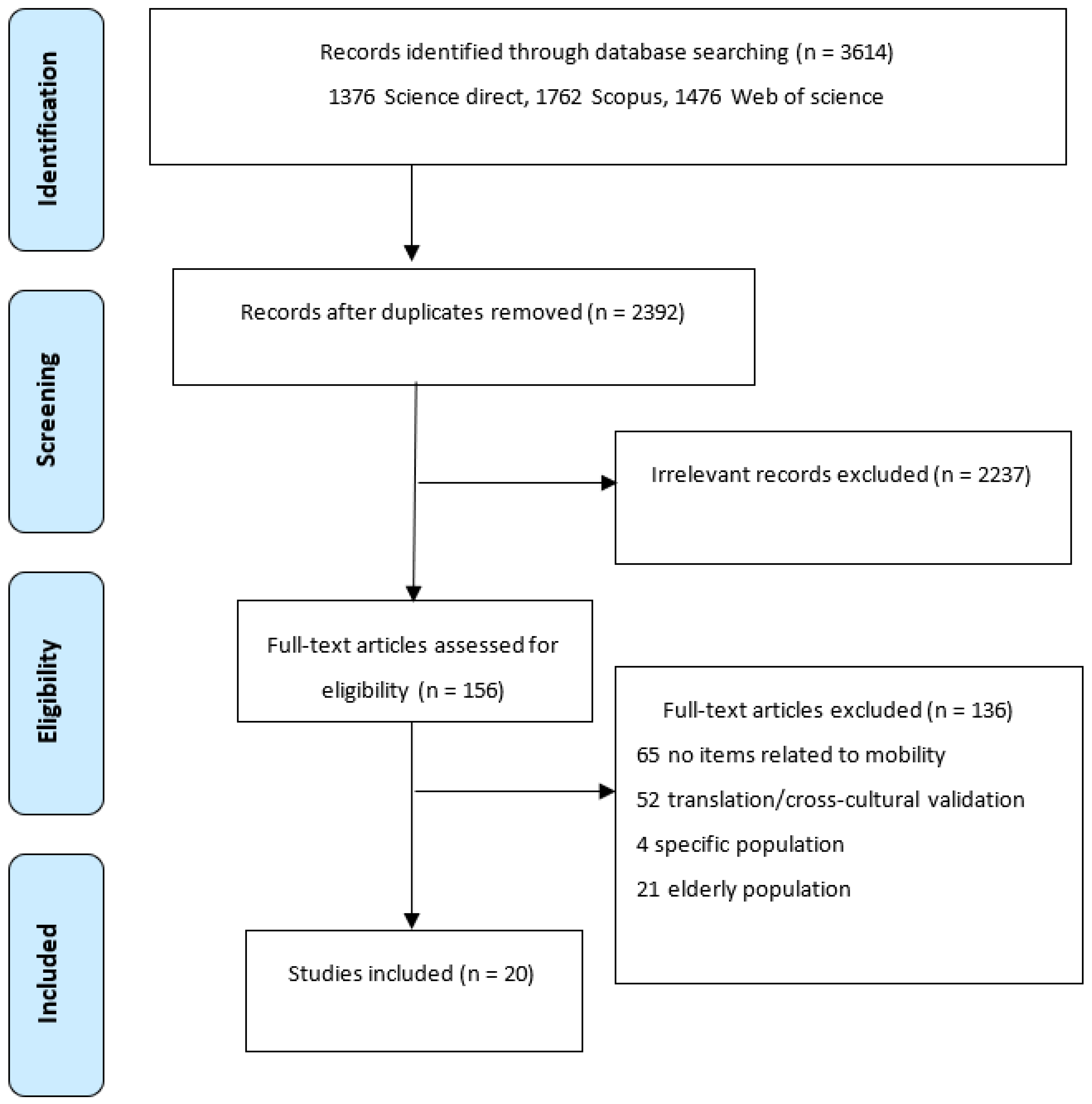
2. Materials and Methods
2.1. Data Sources and Searches
2.2. Study Selection
2.3. Data Extraction
2.4. Linkage of Items to the ICF
2.5. Quality Assessment
3. Results
3.1. Linking to ICF
3.2. Quality Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A
| ICF Category | SF-36 | SF-12 | SF-6D | AQoL | AQoL 8 | AQoL-6D | EQ 5D | EQ 5D (5L) | WHOQOL-Bref | Stark Qol | HUI-2 | HUI-3 | NHP | HINT-20 | QWB-SA | PAT-5D-QoL | HALex | FSQ | SWED-QUAL | MQLI | CAT-Health |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| d Activities and participation | 2 | 1 | 4 | 1 | 2 | 1 | 2 | 1 | |||||||||||||
| d177 Making decisions | 1 | ||||||||||||||||||||
| d230 Carrying out daily routine | 2 | 1 | 1 | ||||||||||||||||||
| d4 Mobility | 1 | 1 | 1 | 1 | |||||||||||||||||
| d410 Changing basic body position | 1 | ||||||||||||||||||||
| d4100 Lying down | 1 | ||||||||||||||||||||
| d4102 Kneeling | 1 | 1 | 1 | 1 | |||||||||||||||||
| d4103 Sitting | 1 | 1 | |||||||||||||||||||
| d4104 Standing | 2 | ||||||||||||||||||||
| d4105 Bending | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||||||
| d415 Maintaining a body position | 1 | 1 | |||||||||||||||||||
| d4150 Maintaining a lying position | 1 | 1 | |||||||||||||||||||
| d4153 Maintaining a sitting position | 1 | ||||||||||||||||||||
| d4154 Maintaining a standing position | 2 | 5 | |||||||||||||||||||
| d430 Lifting and carrying objects | 2 | 1 | 2 | 1 | 1 | 1 | |||||||||||||||
| d4300 Lifting | 1 | 1 | |||||||||||||||||||
| d4301 Carrying in the hands | 1 | ||||||||||||||||||||
| d4302 Carrying in the arms | 1 | ||||||||||||||||||||
| d440 Fine hand use | 1 | 2 | |||||||||||||||||||
| d4400 Picking up | 2 | 1 | |||||||||||||||||||
| d4401 Grasping | 1 | ||||||||||||||||||||
| d445 Hand and arm use | 1 | 3 | |||||||||||||||||||
| d4450 Pulling | 1 | ||||||||||||||||||||
| d4451 Pushing | 1 | 1 | 3 | ||||||||||||||||||
| d4452 Reaching | 1 | ||||||||||||||||||||
| d4453 Turning or twisting the hands or arms | 6 | ||||||||||||||||||||
| d449 Carrying, moving and handling objects, other specified and unspecified | 1 | 1 | 1 | 1 | |||||||||||||||||
| d450 Walking | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 3 | 1 | 1 | |||||||||||
| d4500 Walking short distances | 2 | 1 | 1 | 4 | 1 | 1 | |||||||||||||||
| d4501 Walking long distances | 1 | 2 | 1 | 2 | 1 | ||||||||||||||||
| d455 Moving around | 1 | 1 | 1 | 1 | |||||||||||||||||
| d4551 Climbing | 2 | 1 | 1 | 1 | 1 | 3 | 1 | 1 | 4 | ||||||||||||
| d4552 Running | 1 | 1 | 2 | 1 | |||||||||||||||||
| d4553 Jumping | 1 | ||||||||||||||||||||
| d4600 Moving around within the home | 1 | 1 | 1 | ||||||||||||||||||
| d465 Moving around using equipment | 1 | 1 | 1 | 1 | 1 | ||||||||||||||||
| d469 Walking and moving, other specified and unspecified | 1 | 1 | 1 | ||||||||||||||||||
| d4702Using public motorized transportation | 1 | ||||||||||||||||||||
| d4751 Driving motorized vehicles | 1 | ||||||||||||||||||||
| d498 Mobility, other specified | 1 | ||||||||||||||||||||
| d5 Self-care | 1 | 1 | 1 | ||||||||||||||||||
| d510 Washing oneself | 1 | 2 | 1 | 1 | 1 | 1 | |||||||||||||||
| d520 Caring for body parts | 1 | ||||||||||||||||||||
| d530 Toileting | 1 | ||||||||||||||||||||
| d540 Dressing | 1 | 2 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | ||||||||||||
| d5402 Putting on footwear | 1 | ||||||||||||||||||||
| d550 Eating | 1 | 2 | 1 | ||||||||||||||||||
| d6 Domestic life | 1 | 1 | 1 | ||||||||||||||||||
| d6200 Shopping | 1 | 1 | 3 | 1 | |||||||||||||||||
| d630 Preparing meals | 1 | 1 | 1 | 1 | |||||||||||||||||
| d640 Doing housework | 1 | 1 | 4 | 1 | |||||||||||||||||
| d6401 Cleaning cooking area and utensils | 1 | 2 | |||||||||||||||||||
| d6402 Cleaning living area | 1 | 2 | |||||||||||||||||||
| d649 Household tasks, other specified and unspecified | 1 | 1 | 1 | ||||||||||||||||||
| d6501 Maintaining dwelling and furnishings | 1 | ||||||||||||||||||||
| d6503 Maintaining vehicles | 1 | 1 | |||||||||||||||||||
| d6505 Taking care of plants, indoors and outdoors | 1 | 1 | 1 | 2 | 1 | 1 | |||||||||||||||
| d750 Informal social relationships | 3 | ||||||||||||||||||||
| d760 Family relationships | 3 | ||||||||||||||||||||
| d820 School education | 1 | 2 | 1 | 1 | |||||||||||||||||
| d850 Remunerative employment | 1 | 3 | 1 | 1 | |||||||||||||||||
| d920 Recreation and leisure | 1 | 2 | 1 | 1 | |||||||||||||||||
| d9201 Sports | 1 | 2 | 1 | 1 | 1 | ||||||||||||||||
| d9204 Hobbies | 1 | ||||||||||||||||||||
| d9205 Socializing | 1 | 1 | |||||||||||||||||||
| d930 Religion and spirituality | 1 |
References
- Cieza, A.; Brockow, T.; Ewert, T.; Amman, E.; Kollerits, B.; Chatterji, S.; Üstün, T.B.; Stucki, G. Linking Health-Status Measurements to the International Classification of Functioning, Disability and Health. J. Rehabil. Med. 2002, 34, 205–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cieza, A.; Geyh, S.; Chatterji, S.; Kostanjsek, N.; Üstün, B.; Stucki, G. ICF Linking Rules: An Update Based on Lessons Learned. J. Rehabil. Med. 2005, 37, 212–218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jette, A.M.; Haley, S. Contemporary Measurement Techniques for Rehabilitation Outcomes Assessment. J. Rehabil. Med. 2005, 37, 339–345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rothstein, J.M.; Campbell, S.K.; Echternach, J.L.; Jette, A.M.; Knecht, H.G.; Rose, S.J. Standards for Tests and Measurements in Physical Therapy Practice. Phys. Ther. 1991, 71, 589–622. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- FDA. Guidance for Industry Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims; FDA: Silver Spring, MD, USA, 2009. [Google Scholar]
- Cieza, A.; Stucki, G. Content Comparison of Health-Related Quality of Life (HRQOL) Instruments Based on the International Classification of Functioning, Disability and Health (ICF). Qual. Life Res. 2005, 14, 1225–1237. [Google Scholar] [CrossRef] [PubMed]
- Schöttker-Königer, T.; Schäfer, A. The Model of Health-Related Quality of Life According to Wilson and Cleary. A Conceptual Framework for the Selection of Physiotherapeutic Intervention Outcomes. Physioscience 2017, 13, 121–128. [Google Scholar] [CrossRef]
- Karimi, M.; Brazier, J. Health, Health-Related Quality of Life, and Quality of Life: What Is the Difference? Pharmacoeconomics 2016, 34, 645–649. [Google Scholar] [CrossRef]
- Moons, P.; Budts, W.; De Geest, S. Critique on the Conceptualisation of Quality of Life: A Review and Evaluation of Different Conceptual Approaches. Int. J. Nurs. Stud. 2006, 43, 891–901. [Google Scholar] [CrossRef]
- Patrick, D.L.; Deyo, R.A. Generic and Disease-Specific Measures in Assessing Health Status and Quality of Life. Med. Care 1989, 27, S217–S232. [Google Scholar] [CrossRef]
- Hays, R.D.; Reeve, B.B. Measurement and Modeling of Health-Related Quality of Life. In Epidemiology and Demography in Public Health; Heggenhougen, H.K., Quah, S.R., Eds.; Elsevier: Berlin/Heidelberg, Germany, 2008; pp. 241–252. [Google Scholar]
- Geyh, S.; Cieza, A.; Kollerits, B.; Grimby, G.; Stucki, G. Content Comparison of Health-Related Quality of Life Measures Used in Stroke Based on the International Classification of Functioning, Disability and Health (ICF): A Systematic Review. Qual. Life Res. 2007, 16, 833–851. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Functioning, Disability and Health (ICF); World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Stucki, G.; Cieza, A.; Ewert, T.; Kostanjsek, N.; Chatterji, S.; Üstün, T.B. Application of the International Classification of Functioning, Disability and Health (ICF) in Clinical Practice. Disabil. Rehabil. 2002, 24, 281–282. [Google Scholar] [CrossRef] [PubMed]
- Fayed, N.; Cieza, A.; Edmond Bickenbach, J. Linking Health and Health-Related Information to the ICF: A Systematic Review of the Literature from 2001 to 2008. Disabil. Rehabil. 2011, 33, 1941–1951. [Google Scholar] [CrossRef] [PubMed]
- Magasi, S.; Post, M.W. A Comparative Review of Contemporary Participation Measures’ Psychometric Properties and Content Coverage. Arch. Phys. Med. Rehabil. 2010, 91, S17–S28. [Google Scholar] [CrossRef]
- Schiariti, V.; Fayed, N.; Cieza, A.; Klassen, A.; O’donnell, M. Content Comparison of Health-Related Quality of Life Measures for Cerebral Palsy Based on the International Classification of Functioning. Disabil. Rehabil. 2011, 33, 1330–1339. [Google Scholar] [CrossRef] [PubMed]
- Stucki, A.; Cieza, A.; Schuurmans, M.M.; Ustun, B.; Stucki, G.; Gradinger, F.; Partinen, M. Content Comparison of Health-Related Quality of Life Instruments for Obstructive Sleep Apnea. Sleep Med. 2008, 9, 199–206. [Google Scholar] [CrossRef]
- Stucki, A.; Stucki, G.; Cieza, A.; Schuurmans, M.M.; Kostanjsek, N.; Ruof, J. Content Comparison of Health-Related Quality of Life Instruments for COPD. Respir. Med. 2007, 101, 1113–1122. [Google Scholar] [CrossRef] [Green Version]
- Tschiesner, U.; Rogers, S.N.; Harréus, U.; Berghaus, A.; Cieza, A. Content Comparison of Quality of Life Questionnaires Used in Head and Neck Cancer Based on the International Classification of Functioning, Disability and Health: A Systematic Review. Eur. Arch. Oto-Rhino-Laryngol. 2008, 265, 627–637. [Google Scholar] [CrossRef]
- Prinsen, C.A.C.; Mokkink, L.B.; Bouter, L.M.; Alonso, J.; Patrick, D.L.; de Vet, H.C.W.; Terwee, C.B. COSMIN Guideline for Systematic Reviews of Patient-Reported Outcome Measures. Qual. Life Res. 2018, 27, 1147–1157. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Cieza, A.; Fayed, N.; Bickenbach, J.; Prodinger, B. Refinements of the ICF Linking Rules to Strengthen Their Potential for Establishing Comparability of Health Information. Disabil. Rehabil. 2019, 41, 574–583. [Google Scholar] [CrossRef]
- Mokkink, L.B.; de Vet, H.C.W.; Prinsen, C.A.C.; Patrick, D.L.; Alonso, J.; Bouter, L.M.; Terwee, C.B. COSMIN Risk of Bias Checklist for Systematic Reviews of Patient-Reported Outcome Measures. Qual. Life Res. 2018, 27, 1171–1179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Terwee, C.B.; Prinsen, C.A.; Chiarotto, A.; De Vet, H.; Bouter, L.M.; Marjan, J.A.; Donald, W.; Patrick, L.; Mokkink, L.B.; Terwee, C.B. COSMIN Methodology for Assessing the Content Validity of PROMs: User Manual. Circulation 2018, 120, 1–72. [Google Scholar]
- Terwee, C.B.; Prinsen, C.A.C.; Chiarotto, A.; Westerman, M.J.; Patrick, D.L.; Alonso, J.; Bouter, L.M.; de Vet, H.C.W.; Mokkink, L.B. COSMIN Methodology for Evaluating the Content Validity of Patient-Reported Outcome Measures: A Delphi Study. Qual. Life Res. 2018, 27, 1159–1170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hawthorne, G. Assessing Utility Where Short Measures Are Required: Development of the Short Assessment of Quality of Life-8 (AQoL-8) Instrument. Value Heal. 2009, 12, 948–957. [Google Scholar] [CrossRef] [PubMed]
- Richardson, J.R.J.; Peacock, S.J.; Hawthorne, G.; Iezzi, A.; Elsworth, G.; Day, N.A. Construction of the Descriptive System for the Assessment of Quality of Life AQoL-6D Utility Instrument. Health Qual. Life Outcomes 2012, 10, 38. [Google Scholar] [CrossRef] [Green Version]
- Hawthorne, G.; Richardson, J.; Osborne, R. The Assessment of Quality of Life (AQoL) Instrument: A Psychometric Measure of Health-Related Quality of Life. Qual. Life Res. 1999, 8, 209–224. [Google Scholar] [CrossRef]
- Hawthorne, G.; Richardson, J.; Day, N.A. A Comparison of the Assessment of Quality of Life (AQoL) with Four Other Generic Utility Instruments. Ann. Med. 2001, 33, 358–370. [Google Scholar] [CrossRef]
- Hawthorne, G.; Herrman, H.; Murphy, B. Interpreting the WHOQOL-Bref: Preliminary Population Norms and Effect Sizes. Soc. Indic. Res. 2006, 77, 37–59. [Google Scholar] [CrossRef]
- Brorsson, B.; Ifver, J.; Hays, R.D. The Swedish Health-Related Quality of Life Survey (SWED-QUAL). Qual. Life Res. 1993, 2, 33–45. [Google Scholar] [CrossRef]
- Ware, J.E., Jr.; Kosinski, M.; S.D., M. A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, K.I.; Zapata-Vega, M.I.; Mezzich, J.E.; Mazzotti, G. Validation Study of the Multicultural Quality of Life Index (MQLI) in a Peruvian Sample. Rev. Bras. Psiquiatr. 2006, 28, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Krantz, E.; Wide, U.; Trimpou, P.; Bryman, I.; Landin-Wilhelmsen, K. Comparison between Different Instruments for Measuring Health-Related Quality of Life in a Population Sample, the WHO MONICA Project, Gothenburg, Sweden: An Observational, Cross-Sectional Study. BMJ Open 2019, 9, e024454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palta, M.; Chen, H.-Y.; Kaplan, R.M.; Feeny, D.; Cherepanov, D.; Fryback, D.G. Standard Error of Measurement of 5 Health Utility Indexes across the Range of Health for Use in Estimating Reliability and Responsiveness. Med. Decis. Mak. 2011, 31, 260–269. [Google Scholar] [CrossRef]
- Johnson, J.A.; Pickard, A.S. Comparison of the EQ-5D and SF-12 Health Surveys in a General Population Survey in Alberta, Canada. Med. Care 2000, 38, 115–121. [Google Scholar] [CrossRef]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.F.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and Preliminary Testing of the New Five-Level Version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [Green Version]
- Boyle, M.H.; Furlong, W.; Feeny, D.; Torrance, G.W.; Hatcher, J. Reliability of the Health Utilities Index-Mark III Used in the 1991 Cycle 6 Canadian General Social Survey Health Questionnaire. Qual. Life Res. 1995, 4, 249–257. [Google Scholar] [CrossRef]
- Rebollo, P.; Cueto, E.G.; Zardaín, P.C.; Cuervo, J.; Martínez, I.; Alonso, J.; Ferrer, M.; Muñiz, J. Desarrollo Del CAT-Health, Primer Test Adaptativo Informatizado Para La Evaluación de La Calidad de Vida Relacionada Con La Salud En España. Med. Clin. 2009, 133, 241–251. [Google Scholar] [CrossRef]
- Rebollo, P.; Castejon, I.; Cuervo, J.; Villa, G.; Garcia-Cueto, E.; Diaz-Cuervo, H.; Zardain, P.C.; Muniz, J.; Alonso, J.; CAT-Health Research Group. Validation of a Computer-Adaptive Test to Evaluate Generic Health-Related Quality of Life. Health Qual. Life Outcomes 2010, 8, 147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cleary, P.D.; Jette, A.M. Reliability and Validity of the Functional Status Questionnaire. Qual. Life Res. 2000, 9, 747–753. [Google Scholar] [CrossRef]
- Erickson, P. Evaluation of a Population-Based Measure of Quality of Life: The Health and Activity Limitation Index (HALex). Qual. Life Res. 1998, 7, 101–114. [Google Scholar] [CrossRef]
- Jo, M.W.; Lee, H.J.; Kim, S.Y.; Kim, S.H.; Chang, H.; Ahn, J.; Ock, M. Development and Validation of a Novel Generic Health-Related Quality of Life Instrument with 20 Items (HINT-20). J. Prev. Med. Public Health 2017, 50, 38–59. [Google Scholar] [CrossRef]
- Kopec, J.A.; Sayre, E.C.; Davis, A.M.; Badley, E.M.; Abrahamowicz, M.; Pouchot, J.; Sherlock, L.; Esdaile, J.M. Development of a Paper-and-Pencil Semi-Adaptive Questionnaire for 5 Domains of Health-Related Quality of Life (PAT-5D-QOL). Qual. Life Res. 2013, 22, 2829–2842. [Google Scholar] [CrossRef]
- Hardt, J. A New Questionnaire for Measuring Quality of Life—The Stark QoL. Health Qual. Life Outcomes 2015, 13, 174. [Google Scholar] [CrossRef] [Green Version]
- Ware, J.E.; Sherbourne, C.D. The MOS 36-Item Short-Form Health Survey (Sf-36): I. Conceptual Framework and Item Selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Brazier, J.; Roberts, J.; Deverill, M. The Estimation of a Preference-Based Measure of Health from the SF-36. J. Health Econ. 2002, 21, 271–292. [Google Scholar] [CrossRef] [Green Version]
- The Euroqol Group EuroQol—A New Facility for the Measurement of Health-Related Quality of Life. Health Policy (N. Y.) 1990, 16, 199–208. [CrossRef]
- The WHOQOL Group. The World Health Organization Quality of Life Assessment (WHOQOL): Development and General Psychometric Properties. Soc. Sci. Med. 1998, 46, 1569–1585. [Google Scholar] [CrossRef]
- Feeny, D.; Furlong, W.; Barr, R.D.; Torrance, G.W.; Rosenbaum, P.; Weitzman, S. A Comprehensive Multiattribute System for Classifying the Health Status of Survivors of Childhood Cancer. J. Clin. Oncol. 1992, 10, 923–928. [Google Scholar] [CrossRef] [PubMed]
- Feeny, D.; Furlong, W.; Boyle, M.; Torrance, G.W. Multi-Attribute Health Status Classification Systems: Health Utilities Index. Pharmacoeconomics 1995, 7, 490–502. [Google Scholar] [CrossRef] [PubMed]
- Hunt, S.M.; McEwen, J. The Development of a Subjective Health Indicator. Sociol. Health Illn. 1980, 2, 231–246. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, R.M.; Sieber, W.J.; Ganiats, T.G. The Quality of Well-Being Scale: Comparison of the Interviewer-Administered Version with a Self-Administered Questionnaire. Psychol. Health 1997, 12, 783–791. [Google Scholar] [CrossRef]
- Jette, A.M.; Davies, A.R.; Cleary, P.D.; Calkins, D.R.; Rubenstein, L.V.; Fink, A.; Kosecoff, J.; Young, R.T.; Brook, R.H.; Delbanco, T.L. The Functional Status Questionnaire. J. Gen. Intern. Med. 1986, 1, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Mezzich, J.E.; Ruipérez, M.A.; Pérez, C.; Yoon, G.; Liu, J.; Mahmud, S. The Spanish Version of the Quality of Life Index: Presentation and Validation. J. Nerv. Ment. Dis. 2000, 188, 301–305. [Google Scholar] [CrossRef] [PubMed]
- Chiarotto, A.; Terwee, C.B.; Kamper, S.J.; Boers, M.; Ostelo, R.W. Evidence on the Measurement Properties of Health-Related Quality of Life Instruments Is Largely Missing in Patients with Low Back Pain: A Systematic Review. J. Clin. Epidemiol. 2018, 102, 23–37. [Google Scholar] [CrossRef] [PubMed]
- Craxford, S.; Deacon, C.; Myint, Y.; Ollivere, B. Assessing Outcome Measures Used after Rib Fracture: A COSMIN Systematic Review. Injury 2019, 50, 1816–1825. [Google Scholar] [CrossRef]
- Pinto Carral, A.; Fernández Villa, T.; Molina De La Torre, A.J. Patient-Reported Mobility: A Systematic Review. Arch. Phys. Med. Rehabil. 2016, 97, 1182–1194. [Google Scholar] [CrossRef]
- Veldkamp, B.P.; Sluijter, C. Theoretical and Practical Advances in Computer-Based Educational Measurement; Methodology of Educational Measurement and Assessment; Veldkamp, B.P., Sluijter, C., Eds.; Springer International Publishing: Cham, Switzerland, 2019; ISBN 978-3-030-18479-7. [Google Scholar]
- Lohr, K.N. Assessing Health Status and Quality-of-Life Instruments: Attributes and Review Criteria. Qual. Life Res. 2002, 11, 193–205. [Google Scholar] [CrossRef]
| Database | Search Strategy |
|---|---|
| Science Direct | Terms: mobility OR function OR physical; Title, abstract or author-specified keywords: “health-related quality of life” AND (psychometrics OR validity OR reliability) AND NOT (children OR elderly OR adolescents); Title: scale OR questionnaire OR survey OR test OR index. |
| Scopus | TITLE-ABS-KEY (“health-related quality of life”) AND TITLE (scale OR questionnaire OR survey OR test OR instrument OR index) AND TITLE-ABS-KEY ((psychometrics OR valid * OR reliability) AND NOT (child * OR elderly OR pediatric)) AND ALL (mobility OR function * OR physical) |
| Web of Science (includes Medline, Current Contents Connect, Derwent Innovations Index, KCI-Korean Journal Database, Russian Science Citation Index, SciELO Citation Index, and the main Web of Science collection) | TS = “health-related quality of life” AND TI = (scale OR questionnaire OR survey OR test OR instrument OR index) AND TS = (psychometrics OR valid * OR reliability) NOT TS = (child * OR elderly OR pediatric) AND TS = (mobility OR function * OR physical) |
| PROM | Original Author | Year | Dimensions | Items (Mobility-Related Items) | Answer Choices |
|---|---|---|---|---|---|
| SF-36 [47] | Ware | 1992 | Physical functioning | 36 (10) | 1 limited a lot—3 not limited at all |
| Sherbourne | Role physical | 1 all of the time—5 none of the time | |||
| Social functioning | 1 all of the time/not at all—5 none of the time/extremely | ||||
| Bodily pain | 1 lowest—5/6 highest level of pain | ||||
| General mental health | 1 all of the time—5 none of the time | ||||
| Role emotional | 1 all of the time—5 none of the time | ||||
| Vitality | 1 all of the time—5 none of the time | ||||
| General health | 1 excellent or definitely true—5 poor or definitely false | ||||
| SF-12 [33] | Ware et al. | 1996 | Physical functioning | 12 (2) | 1 limited a lot—3 not limited at all |
| Role-Physical | 1 all of the time—5 none of the time | ||||
| Bodily pain | 1 not at all—5 extremely | ||||
| General health | 1 excellent-5 poor | ||||
| Vitality | 1 all of the time—5 none of the time | ||||
| Social functioning | 1 all of the time—5 none of the time | ||||
| Role-Emotional | 1 all of the time—5 none of the time | ||||
| Mental health | 1 all of the time—5 none of the time | ||||
| SF-6D [48] | Brazier et al. | 2002 | Physical functioning | 6 (1) | 1 not limit—6 a lot of limit |
| Role limitations | 1 no problem—4 limited | ||||
| Social functioning | 1 none of the time—5 all of the time | ||||
| Pain | 1 no pain—6 extremely | ||||
| Mental health | 1 none of the time—5 all of the time | ||||
| Vitality | 1 all of the time—5 none of the time | ||||
| AQoL [29] | Hawthorne, et al. | 1999 | Ilness | 15 (3) | 1 highest level—4 lowest level of QOL |
| Independent living | |||||
| Social relationships | |||||
| Physical senses | |||||
| Pshycological well-being | |||||
| AQoL-8 [27] | Hawthorne | 2009 | Independent living | 8 (2) | 1 highest level—4 lowest level of QOL |
| Social relationships | |||||
| Physical senses | |||||
| Pshycological well-being | |||||
| AQoL-6D [28] | Richardson, et al. | 2012 | Independent living | 20 (4) | 4–6 (depending on the question where it goes from the highest QOL level to the lowest) |
| Relationships | |||||
| Mental health | |||||
| Coping | |||||
| Pain | |||||
| Senses | |||||
| EQ-5D [49] | EuroQol group | 1990 | Mobility | 6 (1) | 3 and VAS (0–100). |
| (EQ-5D-5L [38]) | (2011) | Self-care | (5 and VAS (0–100)) | ||
| Usual Activities | |||||
| Pain/Discomfort | |||||
| Anxiety/Depression | |||||
| WHOQOL- BREF [50] | WHOQOL group | 1998 | Physical health | 26 (1) | 5 |
| Psychological | |||||
| Social relationships | |||||
| Environment | |||||
| HUI-2 [51] | Feeny et al. | 1992 | Sensation | 7 (1) | 3–5 |
| Mobility | |||||
| Emotion | |||||
| Cognition | |||||
| Self-care | |||||
| Pain | |||||
| Fertility * | |||||
| HUI-3 [52] | Feeny et al. | 1995 | Vision | 8 (2) | 5–6 |
| Hearing | |||||
| Speech | |||||
| Ambulation | |||||
| Dexterity | |||||
| Emotion | |||||
| Cognition | |||||
| Pain | |||||
| NHP [53] | Hunt McEwen | 1980 | Physical mobility | 38 (8) | 2 (yes–no) |
| Energy | |||||
| Sleep | |||||
| Pain | |||||
| Social isolation | |||||
| Emotional reactions | |||||
| HINT-20 [44] | Jo et al. | 2017 | Physical health | 20 (3) | 4 |
| Social health | |||||
| Mental health | |||||
| Positive health | |||||
| QWB-SA [54] | Kaplan et al. | 1997 | Mobility | 76 (11) | 2 (yes–no questions) |
| Physical activity | 5 (multiple stage questions) | ||||
| Social activity | 4 (3-day recall questions) | ||||
| 58 symptom/problem complexes | |||||
| Stark QoL [46] | Hardt | 2015 | Mood | 9 (6) | Mood and physical functioning: 5 |
| Energy | 16 pictures | Energy: 2 | |||
| Social Contact | Social contact: 3 | ||||
| Physical functioning | |||||
| PAT-5D-QOL [45] | Kopec et al. | 2013 | Walking | 30 (18) | 4 |
| Handling objects | |||||
| Daily activities | |||||
| Pain or discomfort | |||||
| Feelings | |||||
| HALex [43] | Erickson | 1998 | Health perceived | 11 (1) | General health: 5 |
| Activity limitation | Activity limitation: 2 (yes–no) and one question 4 answer choices. | ||||
| FSQ [55] | Jette et al. | 1986 | Physical function | 34 (9) | 4 no difficulty—1 usually did not do because of health, 0 usually did not do for other reasons |
| Pshycological function | 1 all of the time—6 none of the time | ||||
| Social function | 1 all of the time—6 none of the time | ||||
| Role function | 1 all of the time—6 none of the time | ||||
| SWED-QUAL [32] | Brorsson, et al. | 1993 | Physical functioning | 61 (9) | 4–5 |
| Pain | |||||
| Role functioning | |||||
| Emotional well-being | |||||
| Sleep | |||||
| General health | |||||
| Family functioning | |||||
| MQLI [56] | Mezzich, et al. | 2000 | Physical well-being | 10 (2) | VAS (1–10) |
| Psychological/Emotional well-being | |||||
| Self-care and Independent Functioning | |||||
| Occupational functioning | |||||
| Interpersonal functioning | |||||
| Social emotional support | |||||
| Community and services support | |||||
| Personal fulfillment | |||||
| Spiritual fulfillment | |||||
| Overall quality of life | |||||
| CAT-Health [40] | Rebollo et al. | 2009 | HRQOL (unidimensional) | 96 (25) | 5 |
| PROM | Population | Instrument Administration | |||||
|---|---|---|---|---|---|---|---|
| Author Year | Sample Size | Age | Gender | Setting | Country | Language | |
| Mean (SD, Range) Year | % Female | ||||||
| AQoL | Hawthorne 2001 | 976 | 52.4 (18) | 50 | nr | Australia | English |
| AQoL | Hawthorne 1999 | 255 | nr | 53 | nr | Australia | English |
| AQoL-6D | Richardson 2012 | 620 | nr | 53.50 | nr | Australia | English |
| AQoL-8 | Hawthorne 2009 | 3015 | 45 (19) | 51 | nr | Australia | English |
| CAT-Health | Rebollo 2009 | Pilot study = 185 1373 | Pilot study = 50.97 (22.74) 50.03 (18.22) | SA (online) | Spain | Spanish | |
| CAT-Health | Rebollo 2010 | 396 | 48.6 (17.7) | 67 | SA (online) | Spain | Spanish |
| EQ-5D | Johnson 2000 | 1518 | 53.51 (16.61) | 33.5 | SA (online) | Canada | English |
| EQ-5D | Van Agt 1994 | 208 | 49.3 (18.1) | 43.3 | SA | Netherlands | Dutch |
| EQ-5D/HUI-2/HUI-3/SF-6D/QWB-SA | Palta 2011 | 3844 general population/265 cataract patients | 35–89 | 57.3 | Telephone interviewer (general population)/SA (cataract patients) | USA | English |
| EQ-5D-5L | Herdman 2011 | 144 | nr | nr | nr | UK y España | English and Spanish |
| FSQ | Cleary 2000 | 9267 (from several samples) | nr | nr | nr | USA | English |
| HALex | Erickson 1998 | 41,104 | 43.86 (0.15) | 52.59 | Telephone administered | USA | English |
| HINT-20 | Jo 2017 | 1191 | 47 (14.8) 44.6 (13.2) 45.1 (13.3) | 53.4 50.3 52 | SA | Korea | Korean and English |
| HUI-III | Boyle 1995 | 506 | nr | nr | nr | Canada | English/French |
| MQLI | Schwartz 2006 | 260 | nr | nr | Interviewer administered | Peru | Spanish |
| NHP/SF-36 | Krantz 2019 | 412 | 62.8 (range 39–78) | 77 | SA | Sweden | English |
| PAT-5D-QOL | Kopec 2013 | 1349 (version 1) | 67 | 60 | SA | Canada | English |
| SF-12 | Ware 1996 | 3363 | nr | nr | SA | USA | English |
| StarkQoL | Hardt 2015 | 500 | 44.82 (16.11) | 50 | SA (online) | Germany | German/English |
| SWED-QUAL | Brorsson 1993 | 1143/1396 | nr | nr | SA (postal) | Sweden | Swedish/English |
| WHOQOL-Bref | Hawthorne 2006 | 931 | 48.2 (17.3) | 54 | SA | Australia | English |
| ICF Category | HUI-2 | QWB-SA | PAT-5D-QoL | SWED-QUAL | CAT-Health |
|---|---|---|---|---|---|
| b152 Emotional functions | 1 | ||||
| b455 Exercise tolerance functions | 1 | ||||
| b760 Control of voluntary movement functions | 1 | 1 | |||
| b7603 Supportive functions of arm or leg | 1 | ||||
| b770 Gait pattern functions | 1 |
| ICF Category | AQoL | AQoL 8 | HUI-3 | NHP |
|---|---|---|---|---|
| e1151 Assistive products and technology for personal use in daily living | 1 | |||
| e1250 General products and technology for communication | 3 | 2 | ||
| e3 Support and relationships | 2 | 1 |
| ICF Category | SF-36 | SF-12 | SF-6D | AQoL | AQoL 8 | AQoL-6D | EQ 5D | EQ 5D (5L) | WHOQOL-Bref | Stark Qol | HUI-2 | HUI-3 | NHP | HINT-20 | QWB-SA | PAT-5D-QoL | HALex | FSQ | SWED-QUAL | MQLI | CAT-Health |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| d Activities and participation | 2 | 1 | 4 | 1 | 2 | 1 | 2 | 1 | |||||||||||||
| d177 Making decisions | 1 | ||||||||||||||||||||
| d230 Carrying out daily routine | 2 | 1 | 1 | ||||||||||||||||||
| d4 Mobility | 1 | 1 | 1 | 1 | |||||||||||||||||
| d410 Changing basic body position | 2 | 1 | 1 | 1 | 2 | 1 | 2 | 1 | 5 | ||||||||||||
| d415 Maintaining a body position | 2 | 3 | 5 | 2 | |||||||||||||||||
| d430 Lifting and carrying objects | 2 | 3 | 1 | 1 | 2 | 1 | 1 | 1 | |||||||||||||
| d440 Fine hand use | 1 | 4 | 1 | 1 | |||||||||||||||||
| d445 Hand and arm use | 1 | 1 | 1 | 1 | 13 | ||||||||||||||||
| d449 Carrying, moving and handling objects, other specified and unspecified | 1 | 1 | 1 | 1 | |||||||||||||||||
| d450 Walking | 3 | 1 | 1 | 2 | 4 | 3 | 1 | 1 | 9 | 3 | 1 | 1 | |||||||||
| d455 Moving around | 3 | 1 | 1 | 1 | 3 | 1 | 1 | 1 | 1 | 5 | 2 | 1 | 4 | ||||||||
| d460 Moving around in different locations | 1 | 1 | 1 | ||||||||||||||||||
| d465 Moving around using equipment | 1 | 1 | 1 | 1 | 1 | ||||||||||||||||
| d469 Walking and moving, other specified and unspecified | 1 | 1 | 1 | ||||||||||||||||||
| d470 Using transportation | 1 | ||||||||||||||||||||
| d475 Driving | 1 | ||||||||||||||||||||
| d498 Mobility, other specified | 1 | ||||||||||||||||||||
| d5 Self-care | 1 | 1 | |||||||||||||||||||
| d510 Washing oneself | 1 | 2 | 1 | 1 | 1 | 1 | |||||||||||||||
| d520 Caring for body parts | 1 | ||||||||||||||||||||
| d530 Toileting | 1 | ||||||||||||||||||||
| d540 Dressing | 1 | 2 | 1 | 1 | 1 | 2 | 1 | 1 | 2 | ||||||||||||
| d550 Eating | 1 | 2 | 1 | ||||||||||||||||||
| d6 Domestic life | 1 | 1 | 1 | ||||||||||||||||||
| d620 Acquisition of goods and services | 1 | 1 | 3 | 1 | |||||||||||||||||
| d630 Preparing meals | 1 | 1 | 1 | 1 | |||||||||||||||||
| d640 Doing housework | 1 | 1 | 1 | 1 | 8 | 1 | |||||||||||||||
| d649 Household tasks, other specified and unspecified | 1 | 1 | 1 | ||||||||||||||||||
| d650 Caring for household objects | 2 | 2 | 1 | 2 | 2 | 1 | |||||||||||||||
| d750 Informal social relationships | 3 | ||||||||||||||||||||
| d760 Family relationships | 3 | ||||||||||||||||||||
| d820 School education | 1 | 2 | 1 | 1 | |||||||||||||||||
| d850 Remunerative employment | 1 | 3 | 1 | 1 | |||||||||||||||||
| d920 Recreation and leisure | 1 | 2 | 1 | 3 | 2 | 1 | 2 | 2 | |||||||||||||
| d930 Religion and spirituality | 1 |
| PROM | PROM Design | Total PROM Development | ||||||
|---|---|---|---|---|---|---|---|---|
| General Design Requirements | Concept Elicitation | Total PROM Design | ||||||
| Clear Construct | Clear Origin of Construct | Clear Target Population for Which the PROM Was Developed | Clear Context of Use | PROM Developed in Sample Representing the Target Population | ||||
| SF-12 [33,57] | V | V | V | V | I | I | I | |
| AQOL [30,58] | V | V | V | V | I | I | I | |
| SF-36 [57] | V | V | V | V | I | I | ||
| NHP [57] | D | D | I | D | I | I | I | |
| EQ-5D [37,57] | I | D | V | V | I | I | I | |
| CAT-Health [40] | V | V | V | D | D | I | I | I |
| EQ-5D-5L [38,58] | V | V | V | V | D | I | I | I |
| HINT-20 [44] | V | V | V | V | V | D | D | I |
| HUI 2 and 3 [58] | V | V | V | V | I | I | I | |
| PROM | Structural Validity | Internal Consistency | Reliability | Measurement Error | Criterion Validity | Hypotheses Testing for Construct Validity | Responsiveness | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Meth Quality | Rating | Meth Quality | Rating | Meth Quality | Rating | Meth Quality | Rating | Meth Quality | Rating | Meth Quality | Rating | Meth Quality | Rating | |
| SF-12 | Very low | ? | Moderate | + | Low | ? | ||||||||
| Aqol | Moderate | - | High | - | High | ? | Moderate | ? | ||||||
| AQoL-8 | Moderate | ? | High | + | Moderate | ? | ||||||||
| AQoL-6D | High | + | ||||||||||||
| SF-36 | High | + | High | + | ||||||||||
| SF-6D | High | + | Very low | - | Low | ? | ||||||||
| NHP | High | - | High | + | ||||||||||
| Stark QoL | Low | + | High | - | High | ? | ||||||||
| EQ-5D | High | + | Very low | - | Low | ? | High | - | ||||||
| CAT-Health | High | ? | High | + | High | + | ||||||||
| HINT-20 | Moderate | - | High | + | Low | - | Moderate | + | ||||||
| HALex | Moderate | |||||||||||||
| FSQ | High | - | Very low | - | Moderate | ? | ||||||||
| HUI-3 | High | + | Very low | + | Low | ? | ||||||||
| HUI-2 | High | + | Very low | - | Low | ? | ||||||||
| QWB | High | - | Very low | - | Low | ? | ||||||||
| SWED-QUAL | High | + | Low | |||||||||||
| MQLI | Very low | ? | Low | ? | Very low | - | Low | |||||||
| WHOQOL-BREF | High | - | Moderate | ? | ||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernández-Segura, N.; Marcos-Delgado, A.; Pinto-Carral, A.; Fernández-Villa, T.; Molina, A.J. Health-Related Quality of Life (HRQOL) Instruments and Mobility: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 16493. https://doi.org/10.3390/ijerph192416493
Hernández-Segura N, Marcos-Delgado A, Pinto-Carral A, Fernández-Villa T, Molina AJ. Health-Related Quality of Life (HRQOL) Instruments and Mobility: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(24):16493. https://doi.org/10.3390/ijerph192416493
Chicago/Turabian StyleHernández-Segura, Natalia, Alba Marcos-Delgado, Arrate Pinto-Carral, Tania Fernández-Villa, and Antonio J. Molina. 2022. "Health-Related Quality of Life (HRQOL) Instruments and Mobility: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 24: 16493. https://doi.org/10.3390/ijerph192416493
APA StyleHernández-Segura, N., Marcos-Delgado, A., Pinto-Carral, A., Fernández-Villa, T., & Molina, A. J. (2022). Health-Related Quality of Life (HRQOL) Instruments and Mobility: A Systematic Review. International Journal of Environmental Research and Public Health, 19(24), 16493. https://doi.org/10.3390/ijerph192416493








