Association between Perceived Health-Related Quality of Life and Depression with Frailty in the FRASNET Study
Abstract
:1. Introduction
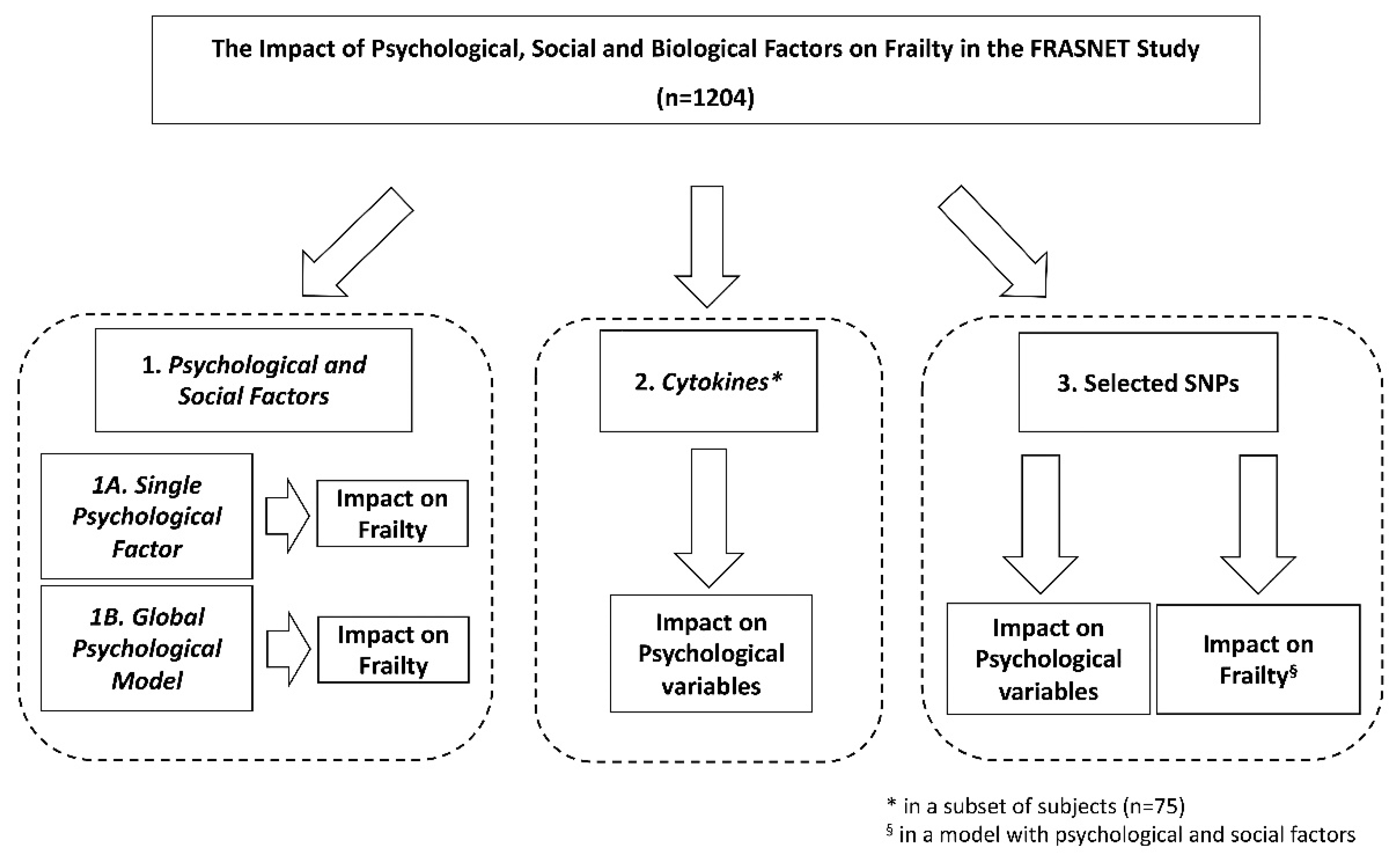
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.2.1. Data Collection
2.2.2. Psychometric Measurements
Mini-Mental State Examination (MMSE)
Geriatric Depression Scale (GDS-15)
SF-36 Medical Outcomes Study Questionnaire Short Form 36 (SF-36) Health Survey
2.2.3. Physical Activity Scale for Elderly (PASE) and Fatigue Severity Scale (FSS)
2.2.4. Frailty Definition and Assessment
2.3. Laboratory Investigations
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Participants
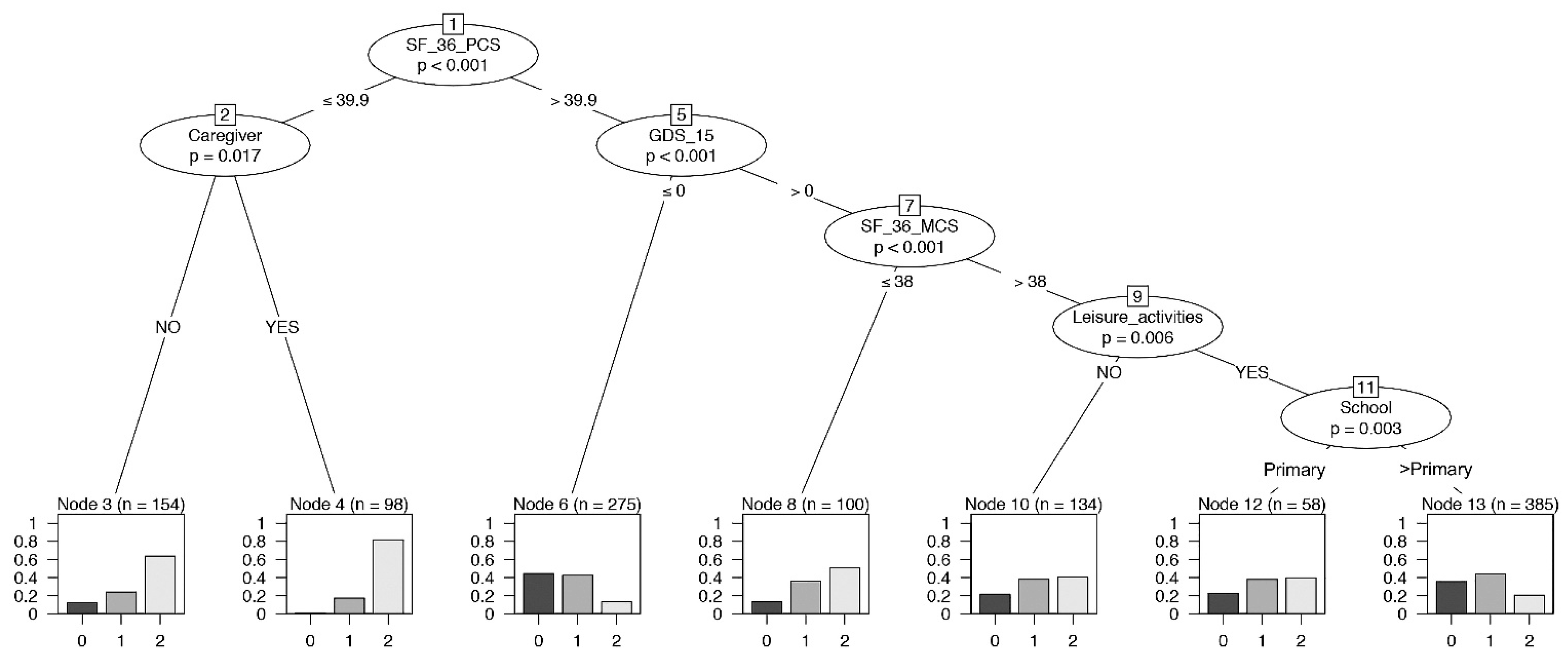
3.2. Impact of the Physical Health Measure of Quality-of-Life Model (SF-36-PCS) on Frailty
3.3. Impact of the Mental Health Measure of Quality-of-Life Model (SF-36-MCS) on Frailty
3.4. Impact of Depression Model (GDS-15) on Frailty
3.5. Impact of the Cognitive Model (MMSE) on Frailty
3.6. Global Psychological Model on Frailty
3.7. Immunological Determinations
3.8. SNPs and Psychological Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- O’Caoimh, R.; Galluzzo, L.; Rodríguez-Laso, Á.; Van der Heyden, J.; Ranhoff, A.H.; Lamprini-Koula, M.; Ciutan, M.; López-Samaniego, L.; Carcaillon-Bentata, L.; Kennelly, S.; et al. Prevalence of frailty at population level in European ADVANTAGE Joint Action Member States: A systematic review and meta-analysis. Ann. Ist. Super. Sanita 2018, 54, 226–238. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older Adults: Evidence for a Phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef] [PubMed]
- Langlois, F.; Vu, T.T.M.; Kergoat, M.-J.; Chassé, K.; Dupuis, G.; Bherer, L. The multiple dimensions of frailty: Physical capacity, cognition, and quality of life. Int. Psychogeriatr. 2012, 24, 1429–1436. [Google Scholar] [CrossRef] [PubMed]
- Lohman, M.; Dumenci, L.; Mezuk, B. Depression and Frailty in Late Life: Evidence for a Common Vulnerability. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2016, 71, 630–640. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bunce, D.; Batterham, P.J.; Mackinnon, A.J. Long-term Associations Between Physical Frailty and Performance in Specific Cognitive Domains. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2019, 74, 919–926. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van der Linden, B.W.A.; Cheval, B.; Sieber, S.; Orsholits, D.; Guessous, I.; Stringhini, S.; Gabriel, R.; Aartsen, M.; Blane, D.; Courvoisier, D.; et al. Life Course Socioeconomic Conditions and Frailty at Older Ages. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2020, 75, 1348–1357. [Google Scholar] [CrossRef] [PubMed]
- Duppen, D.; Lambotte, D.; Dury, S.; Smetcoren, A.-S.; Pan, H.; De Donder, L.; Smetcoren, A.-S.; Dury, S.; De Donder, L.; De Witte, N.; et al. Social Participation in the Daily Lives of Frail Older Adults: Types of Participation and Influencing Factors. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2020, 75, 2062–2071. [Google Scholar] [CrossRef]
- Pilotto, A.; Custodero, C.; Maggi, S.; Polidori, M.C.; Veronese, N.; Ferrucci, L. A multidimensional approach to frailty in older people. Ageing Res. Rev. 2020, 60, 101047. [Google Scholar] [CrossRef]
- Hsu, Y.-H.; Liang, C.-K.; Chou, M.-Y.; Liao, M.-C.; Lin, Y.-T.; Chen, L.-K.; Lo, Y.-K. Association of cognitive impairment, depressive symptoms and sarcopenia among healthy older men in the veterans retirement community in southern Taiwan: A cross-sectional study. Geriatr. Gerontol. Int. 2014, 14, 102–108. [Google Scholar] [CrossRef]
- Lugtenburg, A.; Zuidersma, M.; Wardenaar, K.J.; Aprahamian, I.; Rhebergen, D.; Schoevers, R.A.; Oude Voshaar, R.C. Subtypes of late-life depression: A data-driven approach on cognitive domains and physical frailty. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2021, 76, 141–150. [Google Scholar] [CrossRef]
- Brigola, A.G.; Ottaviani, A.C.; Carvalho, D.H.T.; Oliveira, N.A.; Souza, É.N.; Pavarini, S.C.I. Association between cognitive impairment and criteria for frailty syndrome among older adults. Arq. Neuropsiquiatr. 2020, 78, 2–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaughan, L.; Corbin, A.L.; Goveas, J.S. Depression and frailty in later life: A systematic review. Clin. Interv. Aging 2015, 10, 1947–1958. [Google Scholar] [CrossRef] [Green Version]
- Borges, M.K.; Aprahamian, I.; Romanini, C.V.; Oliveira, F.M.; Mingardi, S.V.B.; Lima, N.A.; Cecato, J.F.; Petrella, M.; Oude Voshaar, R.C. Depression as a determinant of frailty in late life. Aging Ment. Health. 2021, 12, 2279–2285. [Google Scholar] [CrossRef]
- Pothier, K.; Gana, W.; Bailly, N.; Fougère, B. Associations between Frailty and Inflammation, Physical, and Psycho-Social Health in Older Adults: A Systematic Review. Front. Psychol. 2022, 13, 805501. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Garagnani, P.; Vitale, G.; Capri, M.; Salvioli, S. Inflammaging and ‘Garb-aging’. Trends Endocrinol. Metab. 2017, 28, 199–212. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bremmer, M.A.; Beekman, A.T.F.; Deeg, D.J.H.; Penninx, B.W.J.H.; Dik, M.G.; Hack, C.E.; Hoogendijk, W.J.G. Inflammatory markers in late-life depression: Results from a population-based study. J. Affect. Disord. 2008, 106, 249–255. [Google Scholar] [CrossRef]
- Smith, A.J.P.; Humphries, S.E. Cytokine and cytokine receptor gene polymorphisms and their functionality. Cytokine Growth Factor Rev. 2009, 20, 43–59. [Google Scholar] [CrossRef]
- Zhao, X.; Logue, M.W.; Hawn, S.E.; Neale, Z.E.; Zhou, Z.; Huber, B.R.; Miller, M.W.; Wolf, E.J. PTSD, major depression, and advanced transcriptomic age in brain tissue. Depress. Anxiety 2022, 39, 824–834. [Google Scholar] [CrossRef]
- Lee, I.-C.; Chiu, Y.-H.; Lee, C.-Y. Exploration of the importance of geriatric frailty on health-related quality of life. Psychogeriatrics 2016, 16, 368–375. [Google Scholar] [CrossRef]
- Poli, S.; Cella, A.; Puntoni, M.; Musacchio, C.; Pomata, M.; Torriglia, D.; Vello, N.; Molinari, B.; Pandolfini, V.; Torrigiani, C.; et al. Frailty is associated with socioeconomic and lifestyle factors in community-dwelling older subjects. Aging Clin. Exp. Res. 2017, 29, 721–728. [Google Scholar] [CrossRef]
- Hardy, S.E.; Kang, Y.; Studenski, S.A.; Degenholtz, H.B. Ability to Walk 1/4 Mile Predicts Subsequent Disability, Mortality, and Health Care Costs. J. Gen. Intern. Med. 2011, 26, 130–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magni, E.; Binetti, G.; Bianchetti, A.; Rozzini, R.; Trabucchi, M. Mini-mental state examination: A normative study in Italian elderly population. Eur. J. Neurol. 1996, 3, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E. SF-36 Health Survey update. Spine 2000, 25, 3130–3139. [Google Scholar] [CrossRef] [PubMed]
- Burke, W.J.; Roccaforte, W.H.; Wengel, S.P. The Short Form of the Geriatric Depression Scale: A Comparison With the 30-Item Form. J. Geriatr. Psychiatry Neurol. 1991, 4, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Shin, C.; Park, M.H.; Lee, S.-H.; Ko, Y.-H.; Kim, Y.-K.; Han, K.-M.; Jeong, H.-G.; Han, C. Usefulness of the 15-item geriatric depression scale (GDS-15) for classifying minor and major depressive disorders among community-dwelling elders. J. Affect. Disord. 2019, 259, 370–375. [Google Scholar] [CrossRef] [PubMed]
- Washburn, R.A.; McAuley, E.; Katula, J.; Mihalko, S.L.; Boileau, R.A. The Physical Activity Scale for the Elderly (PASE). J. Clin. Epidemiol. 1999, 52, 643–651. [Google Scholar] [CrossRef]
- Krupp, L.B.; LaRocca, N.G.; Muir-Nash, J.; Steinberg, A.D. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch. Neurol. 1989, 46, 1121–1123. [Google Scholar] [CrossRef]
- Lorè, N.I.; De Lorenzo, R.; Rancoita, P.M.V.; Cugnata, F.; Agresti, A.; Benedetti, F.; Bianchi, M.E.; Bonini, C.; Capobianco, A.; Conte, C.; et al. CXCL10 levels at hospital admission predict COVID-19 outcome: Hierarchical assessment of 53 putative inflammatory biomarkers in an observational study. Mol. Med. 2021, 27, 129. [Google Scholar] [CrossRef]
- Ho, Y.-Y.; Matteini, A.M.; Beamer, B.; Fried, L.; Xue, Q.-L.; Arking, D.E.; Chakravarti, A.; Fallin, M.D.; Walston, J. Exploring Biologically Relevant Pathways in Frailty. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2011, 66, 975–979. [Google Scholar] [CrossRef]
- Roth, S.M.; Schrager, M.A.; Ferrell, R.E.; Riechman, S.E.; Metter, E.J.; Lynch, N.A.; Lindle, R.S.; Hurley, B.F. CNTF genotype is associated with muscular strength and quality in humans across the adult age span. J. Appl. Physiol. 2001, 90, 1205–1210. [Google Scholar] [CrossRef]
- Waltson, J.; Arking, D.; Fallin, D.; Li, T.; Beamer, B.; Xue, Q.; Ferrucci, L.; Fried, L.; Chakravarti, A. IL-6 gene variation is not associated with increased serum levels of IL-6, muscle, weakness, or frailty in older women. Exp. Gerontol. 2005, 40, 344–352. [Google Scholar] [CrossRef]
- Krieglstein, K.; Miyazono, K.; ten Dijke, P.; Unsicker, K. TGF-β in aging and disease. Cell Tissue Res. 2012, 347, 5–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benke, K.S.; Carlson, M.C.; Doan, B.Q.; Walston, J.D.; Xue, Q.L.; Reiner, A.P.; Fried, L.P.; Arking, D.E.; Chakravarti, A.; Fallin, M.D. The association of genetic variants in interleukin-1 genes with cognition: Findings from the cardiovascular health study. Exp. Gerontol. 2011, 46, 1010–1019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nettiksimmons, J.; Tranah, G.; Evans, D.S.; Yokoyama, J.S.; Yaffe, K. Gene-based aggregate SNP associations between candidate AD genes and cognitive decline. Age 2016, 38, 41. [Google Scholar] [CrossRef] [Green Version]
- Gonda, X.; Petschner, P.; Eszlari, N.; Baksa, D.; Edes, A.; Antal, P.; Juhasz, G.; Bagdy, G. Genetic variants in major depressive disorder: From pathophysiology to therapy. Pharmacol. Ther. 2019, 194, 22–43. [Google Scholar] [CrossRef] [Green Version]
- Hothorn, T.; Hornik, K.; Zeileis, A. Unbiased Recursive Partitioning: A Conditional Inference Framework. J. Comput. Graph. Stat. 2006, 15, 651–674. [Google Scholar] [CrossRef] [Green Version]
- Cardoso, A.L.; Fernandes, A.; Aguilar-Pimentel, J.A.; de Angelis, M.H.; Guedes, J.R.; Brito, M.A.; Ortolano, S.; Pani, G.; Athanasopoulou, S.; Gonos, E.S.; et al. Towards frailty biomarkers: Candidates from genes and pathways regulated in aging and age-related diseases. Ageing Res. Rev. 2018, 47, 214–277. [Google Scholar] [CrossRef]
- Soysal, P.; Veronese, N.; Thompson, T.; Kahl, K.G.; Fernandes, B.S.; Prina, A.M.; Solmi, M.; Schofield, P.; Koyanagi, A.; Tseng, P.-T.; et al. Relationship between depression and frailty in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2017, 36, 78–87. [Google Scholar] [CrossRef] [Green Version]
- Crocker, T.F.; Brown, L.; Clegg, A.; Farley, K.; Franklin, M.; Simpkins, S.; Young, J. Quality of life is substantially worse for community-dwelling older people living with frailty: Systematic review and meta-analysis. Qual. Life Res. 2019, 28, 2041–2056. [Google Scholar] [CrossRef] [Green Version]
- Feng, L.; Nyunt, M.S.Z.; Gao, Q.; Feng, L.; Lee, T.S.; Tsoi, T.; Chong, M.S.; Lim, W.S.; Collinson, S.; Yap, P.; et al. Physical Frailty, Cognitive Impairment, and the Risk of Neurocognitive Disorder in the Singapore Longitudinal Ageing Studies. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2016, 72, 369–375. [Google Scholar] [CrossRef]
- Sławuta, A.; Jacek, P.; Mazur, G.; Jankowska-Polańska, B. Quality of Life and Frailty Syndrome in Patients with Atrial Fibrillation. Clin. Interv. Aging 2020, 15, 783–795. [Google Scholar] [CrossRef] [PubMed]
- Ji, L.; Qiao, X.; Jin, Y.; Si, H.; Liu, X.; Wang, C. Age differences in the relationship between frailty and depression among community-dwelling older adults. Geriatr. Nurs. 2020, 41, 485–489. [Google Scholar] [CrossRef] [PubMed]
- Lenti, M.V.; Klersy, C.; Brera, A.S.; Ballesio, A.; Croce, G.; Padovini, L.; Ciccocioppo, R.; Bertolino, G.; Di Sabatino, A.; Corazza, G.R. Aging underlies heterogeneity between comorbidity and multimorbidity frameworks. Intern. Emerg. Med. 2022, 17, 1033–1041. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Zhang, L.; Sun, F.; Li, Y.; Tang, Z. Cognitive function in Prefrail and frail community-dwelling older adults in China. BMC Geriatr. 2019, 19, 53. [Google Scholar] [CrossRef]
- Bradburn, S.; McPhee, J.; Bagley, L.; Carroll, M.; Slevin, M.; Al-Shanti, N.; Barnouin, Y.; Hogrel, J.-Y.; Pääsuke, M.; Gapeyeva, H.; et al. Dysregulation of C-X-C motif ligand 10 during aging and association with cognitive performance. Neurobiol. Aging 2018, 63, 54–64. [Google Scholar] [CrossRef]
- Pankov, R.; Yamada, K.M. Fibronectin at a glance. J. Cell Sci. 2002, 115, 3861–3863. [Google Scholar] [CrossRef] [Green Version]
- Bąk, E.; Młynarska, A.; Marcisz, C.; Bobiński, R.; Sternal, D.; Młynarski, R. The influence of frailty syndrome on quality of life in elderly patients with type 2 diabetes. Qual. Life Res. 2021, 30, 2487–2495. [Google Scholar] [CrossRef]
- Uchmanowicz, I.; Lomper, K.; Gros, M.; Kałużna-Oleksy, M.; Jankowska, E.A.; Rosińczuk, J.; Cyrkot, T.; Szczepanowski, R. Assessment of Frailty and Occurrence of Anxiety and Depression in Elderly Patients with Atrial Fibrillation. Clin. Interv. Aging 2020, 15, 1151–1161. [Google Scholar] [CrossRef]
- Van Nguyen, T.; Le, D.; Tran, K.D.; Bui, K.X.; Nguyen, T.N. Frailty in Older Patients with Acute Coronary Syndrome in Vietnam. Clin. Interv. Aging 2019, 14, 2213–2222. [Google Scholar] [CrossRef] [Green Version]
- Murdaca, G.; Paladin, F.; Casciaro, M.; Vicario, C.M.; Gangemi, S.; Martino, G. Neuro-Inflammaging and Psychopathological Distress. Biomedicines 2022, 10, 2133. [Google Scholar] [CrossRef]
- Shive, C.; Pandiyan, P. Inflammation, Immune Senescence, and Dysregulated Immune Regulation in the Elderly. Front. Aging 2022, 3, 840827. [Google Scholar] [CrossRef]
- Vanleerberghe, P.; De Witte, N.; Claes, C.; Verté, D. The association between frailty and quality of life when aging in place. Arch. Gerontol. Geriatr. 2019, 85, 103915. [Google Scholar] [CrossRef] [PubMed]
- Howrey, B.T.; Al Snih, S.; Middleton, J.A.; Ottenbacher, K.J. Trajectories of Frailty and Cognitive Decline Among Older Mexican Americans. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2020, 75, 1551–1557. [Google Scholar] [CrossRef]
- Sirven, N.; Dumontet, M.; Rapp, T. The dynamics of frailty and change in socio-economic conditions: Evidence for the 65+ in Europe. Eur. J. Public Health 2020, 30, 715–719. [Google Scholar] [CrossRef] [PubMed]
- Picca, A.; Calvani, R.; Cesari, M.; Landi, F.; Bernabei, R.; Coelho-Júnior, H.J.; Marzetti, E. Biomarkers of Physical Frailty and Sarcopenia: Coming up to the Place? Int. J. Mol. Sci. 2020, 21, 5635. [Google Scholar] [CrossRef] [PubMed]
- Hoogendijk, E.O.; Afilalo, J.; Ensrud, K.E.; Kowal, P.; Onder, G.; Fried, L.P. Frailty: Implications for clinical practice and public health. Lancet 2019, 394, 1365–1375. [Google Scholar] [CrossRef] [PubMed]
- Rohrmann, S. Epidemiology of Frailty in Older People. In Advances in Experimental Medicine and Biology; Springer: Cham, Switzerland, 2020; pp. 21–28. [Google Scholar]
- Lee, L.; Patel, T.; Costa, A.; Bryce, E.; Hillier, L.M.; Slonim, K.; Hunter, S.W.; Heckman, G.; Molnar, F. Screening for frailty in primary care: Accuracy of gait speed and hand-grip strength. Can. Fam. Physician 2017, 63, e51–e57. [Google Scholar]
- Labarca, G.; Saavedra, D.; Dreyse, J.; Jorquera, J.; Barbe, F. Efficacy of CPAP for Improvements in Sleepiness, Cognition, Mood, and Quality of Life in Elderly Patients With OSA. Chest 2020, 158, 751–764. [Google Scholar] [CrossRef]
- Wood, B.M.; Nicholas, M.K.; Blyth, F.; Asghari, A.; Gibson, S. The Utility of the Short Version of the Depression Anxiety Stress Scales (DASS-21) in Elderly Patients with Persistent Pain: Does Age Make a Difference? Pain Med. 2010, 11, 1780–1790. [Google Scholar] [CrossRef] [Green Version]
- Marconcin, P.; Barak, S.; Ferrari, G.; Gouveia, É.R.; de Maio Nascimento, M.; Willig, R.; Varela, M.; Marques, A. Prevalence of Frailty and Its Association with Depressive Symptoms among European Older Adults from 17 Countries: A 5-Year Longitudinal Study. Int. J. Environ. Res. Public Health 2022, 19, 14055. [Google Scholar] [CrossRef]
- Sciorati, C.; Gamberale, R.; Monno, A.; Citterio, L.; Lanzani, C.; De Lorenzo, R.; Ramirez, G.A.; Esposito, A.; Manunta, P.; Manfredi, A.A.; et al. Pharmacological blockade of TNFα prevents sarcopenia and prolongs survival in aging mice. Aging 2020, 12, 23497–23508. [Google Scholar] [CrossRef] [PubMed]


| Parameter | Total = 1204 n (%) | Mean ± SD | Median (Interquartile Range: 25th to 75th Percentiles) |
|---|---|---|---|
| Gender | |||
| Male | 481 (40.0) | ||
| Female | 723 (60.0) | ||
| Age | 73.3 ± 5.73 | ||
| Age groups | |||
| 65–75 years | 815 (67.7) | ||
| 76–85 years | 349 (29.0) | ||
| >85 years | 40 (3.3) | ||
| Weight | 70.9 ± 13.02 | ||
| BMI | 27.0 ± 4.22 | ||
| BMI groups | |||
| Underweight (<18.5) | 7 (0.6) | ||
| Normal weight (18.5–24) | 397 (33.0) | ||
| Overweight (25–29) | 541 (44.9) | ||
| Obesity (30–40) | 253 (21.0) | ||
| Morbid obesity (>40) | 6 (0.5) | ||
| Educational level (n = 1201) | |||
| Primary | 201 (16.7) | ||
| Lower secondary | 274 (22.8) | ||
| Upper secondary | 514 (42.8) | ||
| University | 212 (17.7) | ||
| Leisure activities (n = 1186) | 906 (75.4) | ||
| Annual income (n = 1187) | |||
| >10,000 euros | 1075 (90.6) | ||
| Caregiver (n = 1177) | 557 (47.3) | ||
| Living alone (n = 1196) | 289 (24.2) | ||
| Number of daily medications (quartiles) | |||
| 1 medication | 328 (27.3) | ||
| 2–3 medications | 413 (34.3) | ||
| 4–5 medications | 275 (22.8) | ||
| >5 medications | 188 (15.6) | ||
| Frailty | |||
| Robust | 334 (27.7) | ||
| Pre-frail | 449 (37.3) | ||
| Frail | 421 (35.0) | ||
| SF-36-MCS | 51.0 (44–55) | ||
| SF-36-PCS | 48.0 (41–52) | ||
| MMSE | |||
| Normal cognitive functioning (30–24) | 1337 (94.4) | ||
| Moderate cognitive functioning (23–18) | 67 (5.6) | ||
| GDS-15 (n = 1192) | |||
| Without depression (0–5) | 1016 (85.2) | ||
| Mild depression (6–9) | 125 (10.5) | ||
| Moderate/Severe depression (10–13) | 51 (4.3) |
| SF-36-PCS SNP | Risk Allele | Genotype | Mean (st dev) | Comparison a | Beta | 95% CI | p Value | |
| CNTF rs1800169 [G>A] | G | AA AG GG | 46.6 (8.3) 47.5 (8.5) 46.1 (8.5) | GG vs. AG/AA | −1.33 | [−2.36;−0.30] | 0.007 | |
| TGFB1 rs1800469 [C>T] | C | CC CT TT | 45.7 (8.5) 47.3 (8.4) 46.6 (8.5) | CC vs. TC/TT | −1.38 | [−2.36;−0.40] | 0.010 | |
| MTR rs1050993 [G>A] | G | AA AG GG | 47.5 (8.9) 46.3 (8.4) 46.1 (8.3) | AG/GG vs. AA | −1.29 | [−2.46;−0.13] | 0.019 | |
| MMSE SNP | Risk Allele | Genotype | % MMSE < 24 | Comparison b | OR | 95% CI | p Value | |
| IL6 rs1800795 [G>C] | G | CC CG GG | 7 3.4 8.9 | CG/GG vs. CC | 2.26 | [1.37;3.79] | 0.0016 | |
| Frailty SNP | Risk Allele | Genotype | % Pre-Frailty | % Frailty | Comparison c | OR | 95% CI | p Value |
| FN1 rs7567647 [G>A] | A | AA AG GG | 23.1 34.6 39.6 | 61.5 33.8 34.4 | AA vs. AG AA vs. GG | 3.85 3.45 | [1.92;8.33] [1.75;7.69] | 0.0003 0.0006 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delli Zotti, G.B.; Citterio, L.; Farinone, S.; Concas, M.P.; Brioni, E.; Zagato, L.; Messaggio, E.; Faienza, S.; Simonini, M.; Napoli, A.; et al. Association between Perceived Health-Related Quality of Life and Depression with Frailty in the FRASNET Study. Int. J. Environ. Res. Public Health 2022, 19, 16776. https://doi.org/10.3390/ijerph192416776
Delli Zotti GB, Citterio L, Farinone S, Concas MP, Brioni E, Zagato L, Messaggio E, Faienza S, Simonini M, Napoli A, et al. Association between Perceived Health-Related Quality of Life and Depression with Frailty in the FRASNET Study. International Journal of Environmental Research and Public Health. 2022; 19(24):16776. https://doi.org/10.3390/ijerph192416776
Chicago/Turabian StyleDelli Zotti, Giulia B., Lorena Citterio, Sara Farinone, Maria Pina Concas, Elena Brioni, Laura Zagato, Elisabetta Messaggio, Sipontina Faienza, Marco Simonini, Alessandra Napoli, and et al. 2022. "Association between Perceived Health-Related Quality of Life and Depression with Frailty in the FRASNET Study" International Journal of Environmental Research and Public Health 19, no. 24: 16776. https://doi.org/10.3390/ijerph192416776






