Health Effects of a 12-Week Web-Based Lifestyle Intervention for Physically Inactive and Overweight or Obese Adults: Study Protocol of Two Randomized Controlled Clinical Trials
Abstract
:1. Introduction
2. Materials and Methods: Design, Participants, Interventions, and Outcomes
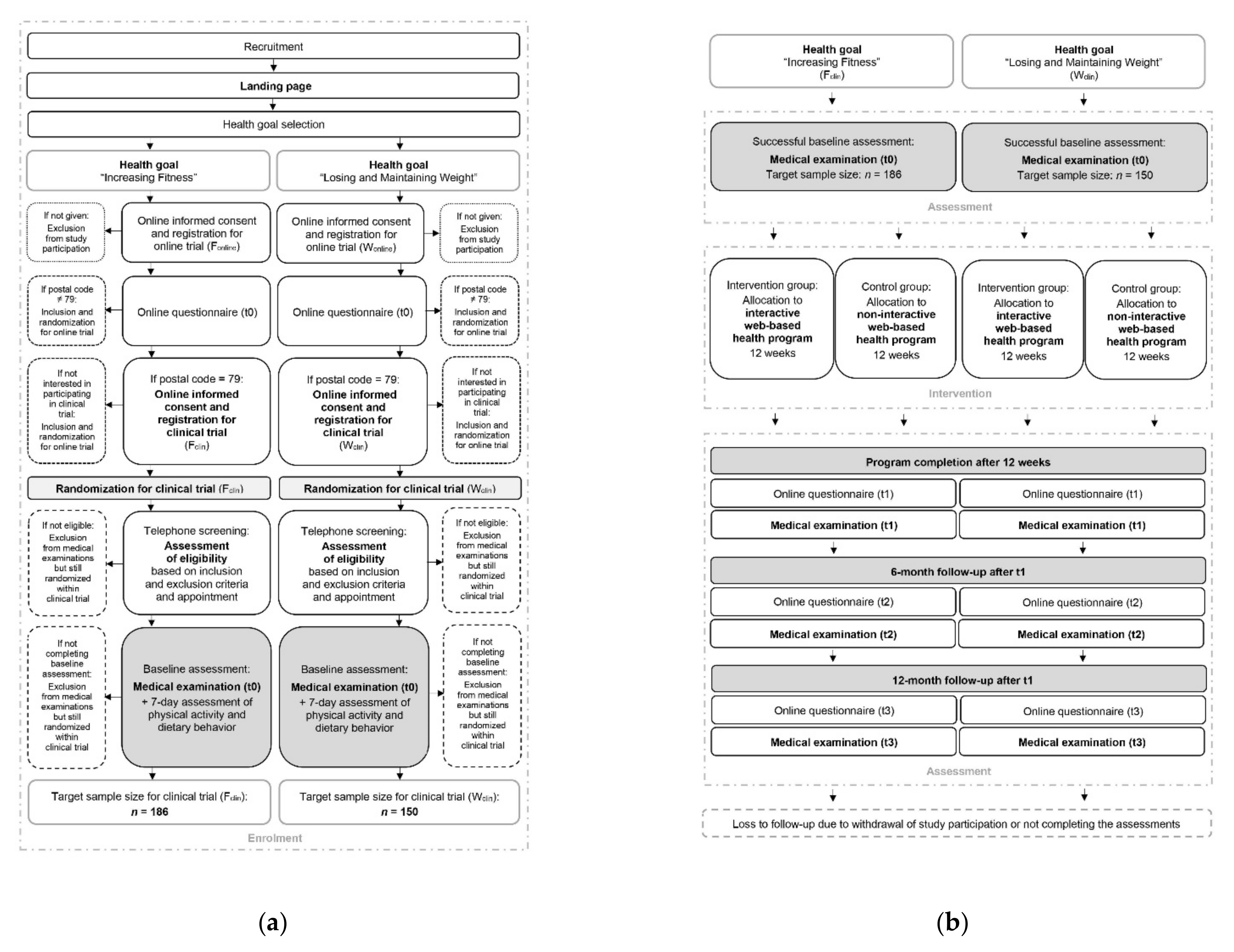
2.1. Study Design, Setting, and Dates
2.2. Eligibility Criteria
2.3. Interventions
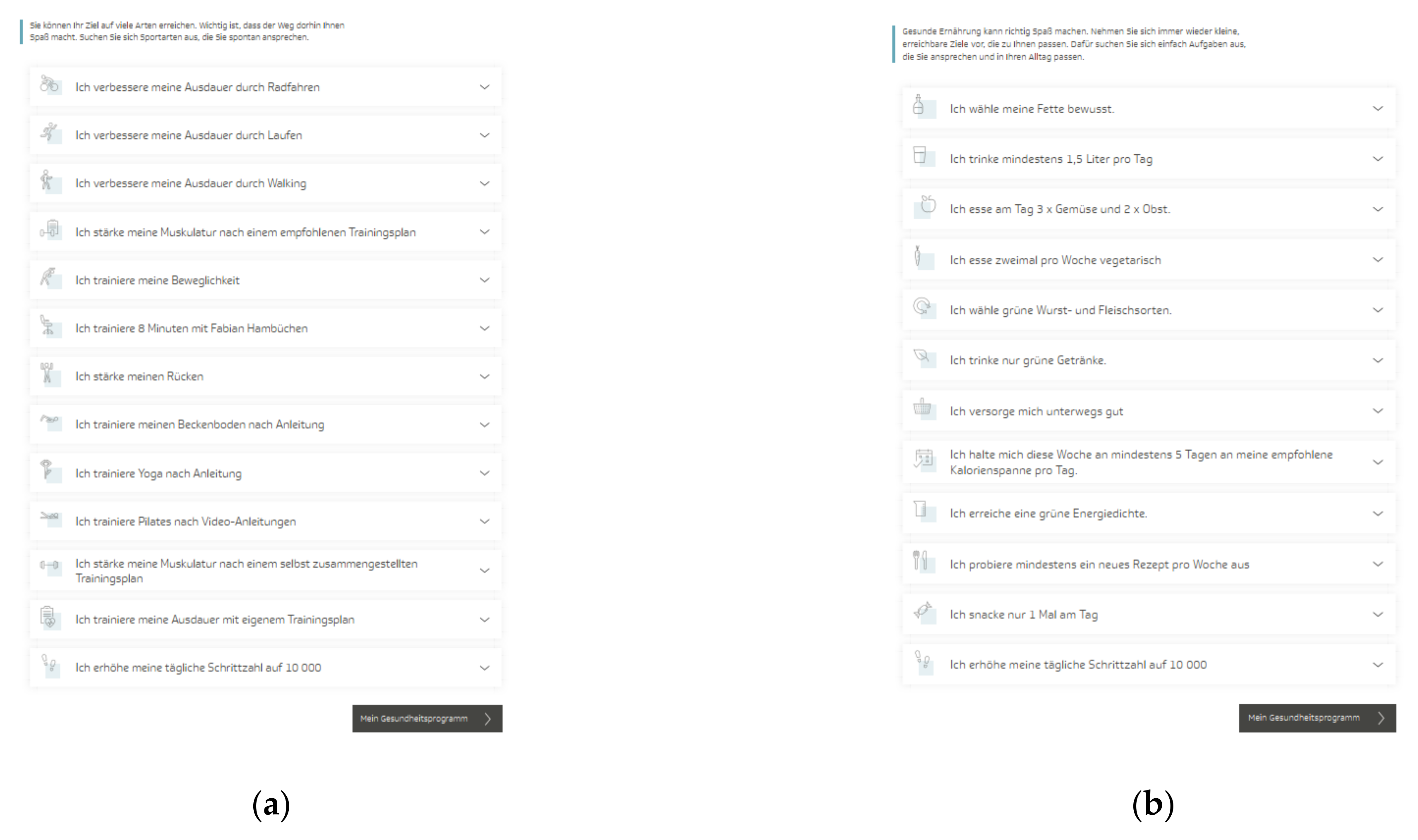
2.3.1. Interactive Web-Based Health Program
2.3.2. Non-Interactive Web-Based Health Program
2.4. Outcomes
2.4.1. Primary Outcomes
2.4.2. Secondary Outcomes
2.4.3. Other Outcomes
2.5. Participant Timeline
2.6. Sample Size
2.7. Recruitment
3. Materials and Methods: Assignment of Interventions
3.1. Allocation
3.2. Blinding
4. Materials and Methods: Data Collection, Management, and Analysis
4.1. Data Collection Methods
4.2. Data Management
4.3. Statistical Methods
- Level 1:
- Level 2:
5. Materials and Methods: Monitoring
5.1. Data Monitoring
5.2. Harms
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Ancillary and Post-Trial Care
Dissemination Policy
Abbreviations
References
- Murray, C.J.L.; Aravkin, A.Y.; Zheng, P.; Abbafati, C.; Abbas, K.M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abdelalim, A.; Abdollahi, M.; Abdollahpour, I.; et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef]
- Global Health Metrics. GBD cause and risk summaries: Low physical activity-Level 2 risk. Lancet 2020, 369, S306–S307. [Google Scholar]
- Global Health Metrics. GBD cause and risk summaries: Dietary risks-Level 2 risk. Lancet 2020, 369, S268–S269. [Google Scholar]
- Global Health Metrics. GBD cause and risk summaries: High body-mass index-Level 2 risk. Lancet 2020, 369, S314–S315. [Google Scholar]
- World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020; World Health Organization: Geneva, Switzerland, 2013; Available online: https://www.who.int/publications/i/item/9789241506236 (accessed on 18 December 2021).
- World Health Organization. Noncommunicable Diseases Country Profiles 2018; World Health Organization: Geneva, Switzerland, 2018; Available online: https://apps.who.int/iris/handle/10665/274512 (accessed on 18 December 2021).
- Finger, J.D.; Mensink, G.B.M.; Lange, C.; Manz, K. Gesundheitsfördernde körperliche Aktivität in der Freizeit bei Erwachsenen in Deutschland. J. Health Monit. 2017, 2, 37–44. [Google Scholar]
- Rütten, A.; Pfeifer, K. Nationale Empfehlungen für Bewegung und Bewegungsförderung. Available online: https://www.sport.fau.de/files/2016/05/Nationale-Empfehlungen-f%C3%BCr-Bewegung-und-Bewegungsf%C3%B6rderung-2016.pdf (accessed on 26 November 2020).
- Deutsche Gesellschaft für Ernährung, e.V. Referenzwerte für die Nährstoffzufuhr. Available online: https://www.dge.de/wissenschaft/referenzwerte/?L=0 (accessed on 26 November 2020).
- Deutsche Gesellschaft für Ernährung, e.V. Vollwertige Ernährung. Available online: https://www.dge.de/ernaehrungspraxis/vollwertige-ernaehrung/?L=0 (accessed on 26 November 2020).
- Max Rubner-Institut. Nationale Verzehrsstudie II: Ergebnisbericht Teil 2. Die bundesweite Befragung zur Ernährung von Jugendlichen und Erwachsenen. Available online: https://www.mri.bund.de/fileadmin/MRI/Institute/EV/NVSII_Abschlussbericht_Teil_2.pdf (accessed on 18 December 2021).
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation (WHO Technical Report Series 894); World Health Organization: Geneva, Switzerland, 1999; Available online: https://apps.who.int/iris/handle/10665/42330 (accessed on 18 December 2021).
- Schienkiewitz, A.; Mensink, G.B.M.; Kuhnert, R.; Lange, C. Übergewicht und Adipositas bei Erwachsenen in Deutschland. J. Health Monit. 2017, 2, 21–28. [Google Scholar]
- Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of exercise is a major cause of chronic diseases. Compr. Physiol. 2012, 2, 1143–1211. [Google Scholar]
- Lee, I.-M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [Green Version]
- Afshin, A.; Forouzanfar, M.H.; Reitsma, M.B.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; Naghavi, M.; et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar]
- Bouchard, C.; Blair, S.N.; Haskell, W.L. Physical Activity and Health, 2nd ed.; Human Kinetics: Leeds, UK, 2012. [Google Scholar]
- Hardman, A.; Stensel, D.J. Physical Activity and Health: The Evidence Explained, 2nd ed.; Routledge: London, UK, 2009. [Google Scholar]
- Pedersen, B.K.; Saltin, B. Exercise as medicine-evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 2015, 25 (Suppl. S3), 1–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report; U.S. Department of Health and Human Services: Washington, DC, USA, 2018. Available online: https://health.gov/sites/default/files/2019-09/PAG_Advisory_Committee_Report.pdf (accessed on 18 December 2021).
- Schlesinger, S.; Neuenschwander, M.; Schwedhelm, C.; Hoffmann, G.; Bechthold, A.; Boeing, H.; Schwingshackl, L. Food Groups and Risk of Overweight, Obesity, and Weight Gain: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Adv. Nutr. 2019, 10, 205–218. [Google Scholar] [CrossRef] [Green Version]
- Schwingshackl, L.; Hoffmann, G.; Lampousi, A.-M.; Knüppel, S.; Iqbal, K.; Schwedhelm, C.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food groups and risk of type 2 diabetes mellitus: A systematic review and meta-analysis of prospective studies. Eur. J. Epidemiol. 2017, 32, 363–375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fabiani, R.; Naldini, G.; Chiavarini, M. Dietary Patterns and Metabolic Syndrome in Adult Subjects: A Systematic Review and Meta-Analysis. Nutrients 2019, 11, 2056. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buckland, G.; Bach, A.; Serra-Majem, L. Obesity and the Mediterranean diet: A systematic review of observational and intervention studies. Obes. Rev. 2008, 9, 582–593. [Google Scholar] [CrossRef]
- Koloverou, E.; Esposito, K.; Giugliano, D.; Panagiotakos, D. The effect of Mediterranean diet on the development of type 2 diabetes mellitus: A meta-analysis of 10 prospective studies and 136,846 participants. Metabolism 2014, 63, 903–911. [Google Scholar] [CrossRef]
- Esposito, K.; Maiorino, M.I.; Bellastella, G.; Chiodini, P.; Panagiotakos, D.; Giugliano, D. A journey into a Mediterranean diet and type 2 diabetes: A systematic review with meta-analyses. BMJ. Open 2015, 5, e008222. [Google Scholar] [CrossRef] [Green Version]
- Kastorini, C.-M.; Milionis, H.J.; Esposito, K.; Giugliano, D.; Goudevenos, J.A.; Panagiotakos, D.B. The effect of Mediterranean diet on metabolic syndrome and its components: A meta-analysis of 50 studies and 534,906 individuals. J. Am. Coll. Cardiol. 2011, 57, 1299–1313. [Google Scholar] [CrossRef] [Green Version]
- Conn, V.S.; Hafdahl, A.; Phillips, L.J.; Ruppar, T.M.; Chase, J.-A.D. Impact of physical activity interventions on anthropometric outcomes: Systematic review and meta-analysis. J. Prim. Prev. 2014, 35, 203–215. [Google Scholar] [CrossRef] [Green Version]
- Schwingshackl, L.; Hoffmann, G.; Kalle-Uhlmann, T.; Arregui, M.; Buijsse, B.; Boeing, H. Fruit and Vegetable Consumption and Changes in Anthropometric Variables in Adult Populations: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. PLoS ONE 2015, 10, e0140846. [Google Scholar] [CrossRef]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef]
- Cornelissen, V.A.; Smart, N.A. Exercise training for blood pressure: A systematic review and meta-analysis. J. Am. Heart. Assoc. 2013, 2, e004473. [Google Scholar] [CrossRef] [Green Version]
- Schwingshackl, L.; Schwedhelm, C.; Hoffmann, G.; Knüppel, S.; Iqbal, K.; Andriolo, V.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food Groups and Risk of Hypertension: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Adv. Nutr. 2017, 8, 793–803. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Chaimani, A.; Schwedhelm, C.; Toledo, E.; Pünsch, M.; Hoffmann, G.; Boeing, H. Comparative effects of different dietary approaches on blood pressure in hypertensive and pre-hypertensive patients: A systematic review and network meta-analysis. Crit. Rev. Food Sci. Nutr. 2019, 59, 2674–2687. [Google Scholar] [CrossRef]
- Boniol, M.; Dragomir, M.; Autier, P.; Boyle, P. Physical activity and change in fasting glucose and HbA1c: A quantitative meta-analysis of randomized trials. Acta Diabetol. 2017, 54, 983–991. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwingshackl, L.; Hoffmann, G.; Iqbal, K.; Schwedhelm, C.; Boeing, H. Food groups and intermediate disease markers: A systematic review and network meta-analysis of randomized trials. Am. J. Clin. Nutr. 2018, 108, 576–586. [Google Scholar] [CrossRef]
- Durstine, J.L.; Grandjean, P.W.; Davis, P.G.; Ferguson, M.A.; Alderson, N.L.; DuBose, K.D. Blood lipid and lipoprotein adaptations to exercise: A quantitative analysis. Sports Med. 2001, 31, 1033–1062. [Google Scholar] [CrossRef] [PubMed]
- Ashor, A.W.; Lara, J.; Siervo, M.; Celis-Morales, C.; Oggioni, C.; Jakovljevic, D.G.; Mathers, J.C. Exercise modalities and endothelial function: A systematic review and dose-response meta-analysis of randomized controlled trials. Sports Med. 2015, 45, 279–296. [Google Scholar] [CrossRef]
- Landberg, R.; Naidoo, N.; van Dam, R.M. Diet and endothelial function: From individual components to dietary patterns. Curr. Opin. Lipidol. 2012, 23, 147–155. [Google Scholar] [CrossRef]
- Shannon, O.M.; Mendes, I.; Köchl, C.; Mazidi, M.; Ashor, A.W.; Rubele, S.; Minihane, A.-M.; Mathers, J.C.; Siervo, M. Mediterranean Diet Increases Endothelial Function in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Nutr. 2020, 150, 1151–1159. [Google Scholar] [CrossRef]
- Deutsche Adipositas-Gesellschaft (DAG) e.V.; Deutsche Diabetes Gesellschaft (DDG); Deutsche Gesellschaft für Ernährung (DGE) e.V.; Deutsche Gesellschaft für Ernährungsmedizin (DGEM) e.V. Interdisziplinäre Leitlinie der Qualität S3 zur „Prävention und Therapie der Adipositas“. Available online: https://www.awmf.org/uploads/tx_szleitlinien/050-001l_S3_Adipositas_Pr%C3%A4vention_Therapie_2014-11-abgelaufen.pdf (accessed on 21 January 2021).
- Bundesärztekammer (BÄK), Kassenärztliche Bundesvereinigung (KBV), Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften. Nationale VersorgungsLeitlinie Therapie des Typ-2-Diabetes–Leitlinien-Report. Available online: http://www.dm-therapie.versorgungsleitlinien.de (accessed on 21 January 2021).
- Galani, C.; Schneider, H. Prevention and treatment of obesity with lifestyle interventions: Review and meta-analysis. Int. Public Health J. 2007, 52, 348–359. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Imperatore, G.; Thomas, W.; Cheng, Y.J.; Lobelo, F.; Norris, K.; Devlin, H.M.; Ali, M.K.; Gruss, S.; Bardenheier, B.; et al. Effect of lifestyle interventions on glucose regulation among adults without impaired glucose tolerance or diabetes: A systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2017, 123, 149–164. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Pei, J.-H.; Kuang, J.; Chen, H.-M.; Chen, Z.; Li, Z.-W.; Yang, H.-Z. Effect of lifestyle intervention in patients with type 2 diabetes: A meta-analysis. Metabolism 2015, 64, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Yamaoka, K.; Tango, T. Effects of lifestyle modification on metabolic syndrome: A systematic review and meta-analysis. BMC Med. 2012, 10, 138. [Google Scholar] [CrossRef]
- Yamaoka, K.; Tango, T. Efficacy of lifestyle education to prevent type 2 diabetes: A meta-analysis of randomized controlled trials. Diabetes Care 2005, 28, 2780–2786. [Google Scholar] [CrossRef] [Green Version]
- Ritterband, L.M.; Gonder-Frederick, L.A.; Cox, D.J.; Clifton, A.D.; West, R.W.; Borowitz, S.M. Internet interventions: In review, in use, and into the future. Prof. Psychol. Res. Pr. 2003, 34, 527–534. [Google Scholar] [CrossRef] [Green Version]
- Jahangiry, L.; Farhangi, M.A.; Shab-Bidar, S.; Rezaei, F.; Pashaei, T. Web-based physical activity interventions: A systematic review and meta-analysis of randomized controlled trials. Public Health 2017, 152, 36–46. [Google Scholar] [CrossRef]
- Davies, C.A.; Spence, J.C.; Vandelanotte, C.; Caperchione, C.M.; Mummery, W.K. Meta-analysis of internet-delivered interventions to increase physical activity levels. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 52. [Google Scholar] [CrossRef] [Green Version]
- Norman, G.J.; Zabinski, M.F.; Adams, M.A.; Rosenberg, D.E.; Yaroch, A.L.; Atienza, A.A. A review of eHealth interventions for physical activity and dietary behavior change. Am. J. Prev. Med. 2007, 33, 336–345. [Google Scholar] [CrossRef] [Green Version]
- Broekhuizen, K.; Kroeze, W.; van Poppel, M.N.M.; Oenema, A.; Brug, J. A systematic review of randomized controlled trials on the effectiveness of computer-tailored physical activity and dietary behavior promotion programs: An update. Ann. Behav. Med. 2012, 44, 259–286. [Google Scholar] [CrossRef] [Green Version]
- Hutchesson, M.J.; Rollo, M.E.; Krukowski, R.; Ells, L.; Harvey, J.; Morgan, P.J.; Callister, R.; Plotnikoff, R.; Collins, C.E. eHealth interventions for the prevention and treatment of overweight and obesity in adults: A systematic review with meta-analysis. Obes. Rev. 2015, 16, 376–392. [Google Scholar] [CrossRef] [PubMed]
- Sorgente, A.; Pietrabissa, G.; Manzoni, G.M.; Re, F.; Simpson, S.; Perona, S.; Rossi, A.; Cattivelli, R.; Innamorati, M.; Jackson, J.B.; et al. Web-Based Interventions for Weight Loss or Weight Loss Maintenance in Overweight and Obese People: A Systematic Review of Systematic Reviews. J. Med. Internet Res. 2017, 19, e229. [Google Scholar] [CrossRef]
- Beleigoli, A.M.; Andrade, A.Q.; Cançado, A.G.; Paulo, M.N.; Diniz, M.D.F.H.; Ribeiro, A.L. Web-Based Digital Health Interventions for Weight Loss and Lifestyle Habit Changes in Overweight and Obese Adults: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2019, 21, e298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bian, R.R.; Piatt, G.A.; Sen, A.; Plegue, M.A.; de Michele, M.L.; Hafez, D.; Czuhajewski, C.M.; Buis, L.R.; Kaufman, N.; Richardson, C.R. The Effect of Technology-Mediated Diabetes Prevention Interventions on Weight: A Meta-Analysis. J. Med. Internet Res. 2017, 19, e76. [Google Scholar] [CrossRef] [Green Version]
- Cotter, A.P.; Durant, N.; Agne, A.A.; Cherrington, A.L. Internet interventions to support lifestyle modification for diabetes management: A systematic review of the evidence. J. Diabetes Complicat. 2014, 28, 243–251. [Google Scholar] [CrossRef] [Green Version]
- Kim, G.; Lee, J.-S.; Lee, S.-K. A Technology-Mediated Interventional Approach to the Prevention of Metabolic Syndrome: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 512. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Ye, Z.; Shao, J.; Tang, L.; Zhang, H.; Wang, X.; Qiu, R.; Zhang, Q. Effect of electronic health interventions on metabolic syndrome: A systematic review and meta-analysis. BMJ Open 2020, 10, e036927. [Google Scholar] [CrossRef]
- Vandelanotte, C.; Müller, A.M.; Short, C.E.; Hingle, M.; Nathan, N.; Williams, S.L.; Lopez, M.L.; Parekh, S.; Maher, C.A. Past, Present, and Future of eHealth and mHealth Research to Improve Physical Activity and Dietary Behaviors. J. Nutr. Educ. Behav. 2016, 48, 219–228.e1. [Google Scholar] [CrossRef]
- AOK. Die Online-Programme der AOK. Available online: https://www.aok.de/pk/bw/leistungen-services/online-programme-der-aok/ (accessed on 23 February 2021).
- BARMER. Übersicht Kursangebote. Available online: https://www.barmer.de/kursangebote (accessed on 23 February 2021).
- DAK-Gesundheit. Online-Coachings der DAK-Gesundheit. Available online: https://www.dak.de/dak/leistungen/online-coachings-2071426.html#/ (accessed on 23 February 2021).
- KNAPPSCHAFT. Gesundheitskurse. Available online: https://www.knappschaft.de/DE/LeistungenGesundheit/Gesundheitskurse/gesundheitskurse_node.html (accessed on 23 February 2021).
- Ebert, D.D.; Berking, M.; Thiart, H.; Riper, H.; Laferton, J.A.C.; Cuijpers, P.; Sieland, B.; Lehr, D. Restoring depleted resources: Efficacy and mechanisms of change of an internet-based unguided recovery training for better sleep and psychological detachment from work. Health Psychol. 2015, 34S, 1240–1251. [Google Scholar] [CrossRef] [Green Version]
- Heber, E.; Lehr, D.; Ebert, D.D.; Berking, M.; Riper, H. Web-Based and Mobile Stress Management Intervention for Employees: A Randomized Controlled Trial. J. Med. Internet Res. 2016, 18, e21. [Google Scholar] [CrossRef] [Green Version]
- Moritz, S.; Schilling, L.; Hauschildt, M.; Schröder, J.; Treszl, A. A randomized controlled trial of internet-based therapy in depression. Behav. Res. Ther. 2012, 50, 513–521. [Google Scholar] [CrossRef]
- Mehring, M.; Haag, M.; Linde, K.; Wagenpfeil, S.; Schneider, A. Effects of a guided web-based smoking cessation program with telephone counseling: A cluster randomized controlled trial. J. Med. Internet Res. 2014, 16, e218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mehring, M.; Haag, M.; Linde, K.; Wagenpfeil, S.; Schneider, A. Effects of a Web-Based Intervention for Stress Reduction in Primary Care: A Cluster Randomized Controlled Trial. J. Med. Internet Res. 2016, 18, e27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knaack, N.; Gauss, B.; Blieske, P. Mit digitalen Gesundheitszielen in ein gesundes Leben starten. In e-Health 2017: Informations-und Kommunikationstechnologien im Gesundheitswesen; Duesberg, F., Ed.; Medical Future Verlag: Solingen, Germany, 2017; pp. 133–135. [Google Scholar]
- Tinsel, I.; Metzner, G.; Schlett, C.; Sehlbrede, M.; Bischoff, M.; Anger, R.; Brame, J.; König, D.; Wurst, R.; Fuchs, R.; et al. Effectiveness of an interactive web-based health program for adults: A study protocol for three concurrent controlled-randomized trials (EVA-TK-Coach). Trials 2021, 22, 526. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.-W.; Tetzlaff, J.M.; Altman, D.G.; Laupacis, A.; Gøtzsche, P.C.; Krleža-Jerić, K.; Hróbjartsson, A.; Mann, H.; Dickersin, K.; Berlin, J.A.; et al. SPIRIT 2013 statement: Defining standard protocol items for clinical trials. Ann. Intern. Med. 2013, 158, 200–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, A.-W.; Tetzlaff, J.M.; Gøtzsche, P.C.; Altman, D.G.; Mann, H.; Berlin, J.A.; Dickersin, K.; Hróbjartsson, A.; Schulz, K.F.; Parulekar, W.R.; et al. SPIRIT 2013 explanation and elaboration: Guidance for protocols of clinical trials. BMJ 2013, 346, e7586. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fitbit Charge 3, Activity Tracker; Fitbit, Inc.: San Francisco, CA, USA, 2018.
- Cooper, K.H. A Means of Assessing Maximal Oxygen Intake. JAMA 1968, 203, 201–204. [Google Scholar] [CrossRef] [PubMed]
- American College of Sports Medicine. ACSM’s Health-Related Physical Fitness Assessment Manual, 5th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2018. [Google Scholar]
- Farrell, S. 50 Years of the Cooper 12-Minute Run. Available online: https://www.cooperinstitute.org/2018/06/08/50-years-of-the-cooper-12-minute-run (accessed on 31 August 2021).
- Borg, G. Borg’s Perceived Exertion and Pain Scales; Human Kinetics: Champaign, IL, USA, 1998. [Google Scholar]
- Thomas, D.T.; Erdman, K.A.; Burke, L.M. American College of Sports Medicine Joint Position Statement. Nutrition and Athletic Performance. Med. Sci. Sports Exerc. 2016, 48, 543–568. [Google Scholar] [PubMed]
- Seca mBCA 515; Bioelectrical Impedance Analysis Scale; Seca GmbH & Co. KG: Hamburg, Germany, 2019.
- ProFit Cube, Version 2.4.80; ProFit-Software für die Fitnessbranche: Erlangen, Germany, 2019.
- Jamar® Hydraulic, Hand Dynamometer; Performance Health International LTD: Huthwaite, UK, 2017.
- Drake, D.; Kennedy, R.; Wallace, E. The Validity and Responsiveness of Isometric Lower Body Multi-Joint Tests of Muscular Strength: A Systematic Review. Sports Med. Open 2017, 3, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marschall, F.; Gail, S. Standardisierung eines Testprotokolls zur Bestimmung der isometrischen Maximalkraft. Beweg. Gesundh. 2011, 27, 226–230. [Google Scholar] [CrossRef]
- Mathiowetz, V.; Weber, K.; Volland, G.; Kashman, N. Reliability and validity of grip and pinch strength evaluations. J. Hand Surg. Am. 1984, 9, 222–226. [Google Scholar] [CrossRef]
- Roberts, H.C.; Denison, H.J.; Martin, H.J.; Patel, H.P.; Syddall, H.; Cooper, C.; Sayer, A.A. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardised approach. Age Ageing 2011, 40, 423–429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Genius Eco® Funktionsstemme–Liegend/Sitzend–150 kg; Isometric Leg Press; FREI AG: Kirchzarten, Germany, 2014.
- Evenson, K.R.; Goto, M.M.; Furberg, R.D. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 159. [Google Scholar] [CrossRef] [Green Version]
- Feehan, L.M.; Geldman, J.; Sayre, E.C.; Park, C.; Ezzat, A.M.; Yoo, J.Y.; Hamilton, C.B.; Li, L.C. Accuracy of Fitbit Devices: Systematic Review and Narrative Syntheses of Quantitative Data. JMIR Mhealth Uhealth 2018, 6, e10527. [Google Scholar] [CrossRef] [Green Version]
- Ringeval, M.; Wagner, G.; Denford, J.; Paré, G.; Kitsiou, S. Fitbit-Based Interventions for Healthy Lifestyle Outcomes: Systematic Review and Meta-Analysis. J. Med. Internet. Res. 2020, 22, e23954. [Google Scholar] [CrossRef]
- International Physical Activity Questionnaire (Long version) (IPAQ-L). Available online: https://sites.google.com/site/theipaq/questionnaire_links(accessed on 21 December 2021).
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Täger, M.; Peltner, J.; Thiele, S. Evaluation of diet quality by means of the Healthy Eating Index and its modified variants. Ernahrungs Umschau 2016, 63, 110–118. [Google Scholar]
- Wittig, F.; Hoffmann, I. Ernährungsmuster von Bio-Käufern und Nicht-Bio-Käufern. In Auswertung der Daten der Nationalen Verzehrsstudie II (NVS II): Eine integrierte verhaltens- und lebensstilbasierte Analyse des Bio-Konsums; Hoffmann, I., Spiller, A., Eds.; Max Rubner-Institut Karlsruhe, Georg-August-Universität: Göttingen, Germany, 2010; pp. 51–68. Available online: https://orgprints.org/id/eprint/18055/1/18055-08OE056_08OE069-MRI_uni-goettingen-hoffmann_spiller-2010-verzehrsstudie.pdf (accessed on 18 December 2021).
- Bechthold, A. Food energy density and body weight. A scientific statement from the DGE. Ernahrungs Umschau 2014, 61, 2–11. [Google Scholar]
- Stelmach-Mardas, M.; Rodacki, T.; Dobrowolska-Iwanek, J.; Brzozowska, A.; Walkowiak, J.; Wojtanowska-Krosniak, A.; Zagrodzki, P.; Bechthold, A.; Mardas, M.; Boeing, H. Link between Food Energy Density and Body Weight Changes in Obese Adults. Nutrients 2016, 8, 229. [Google Scholar] [CrossRef]
- NutriGuide® Plus, Version 4.8; Nutri-Science GmbH: Freiburg, Germany, 2019.
- Seca 274, Stadiometer; Seca GmbH & Co. KG: Hamburg, Germany, 2019.
- Bosy-Westphal, A.; Schautz, B.; Later, W.; Kehayias, J.J.; Gallagher, D.; Müller, M.J. What makes a BIA equation unique? Validity of eight-electrode multifrequency BIA to estimate body composition in a healthy adult population. Eur. J. Clin. Nutr. 2013, 67 (Suppl. 1), S14–S21. [Google Scholar] [CrossRef] [Green Version]
- Bosy-Westphal, A.; Jensen, B.; Braun, W.; Pourhassan, M.; Gallagher, D.; Müller, M.J. Quantification of whole-body and segmental skeletal muscle mass using phase-sensitive 8-electrode medical bioelectrical impedance devices. Eur. J. Clin. Nutr. 2017, 71, 1061–1067. [Google Scholar] [CrossRef] [PubMed]
- Jensen, B.; Braun, W.; Geisler, C.; Both, M.; Klückmann, K.; Müller, M.J.; Bosy-Westphal, A. Limitations of Fat-Free Mass for the Assessment of Muscle Mass in Obesity. Obes. Facts 2019, 12, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Seca 201, Measuring Tape; Seca GmbH & Co. KG: Hamburg, Germany, 2011.
- World Health Organization. Waist Circumference and Waist-Hip Ratio Report of a WHO Expert Consultation; World Health Organization: Geneva, Switzerland, 2008; Available online: https://www.who.int/publications/i/item/9789241501491 (accessed on 2 September 2021).
- Boso Medicus Exclusive, Electronic Blood Pressure Device; BOSCH + SOHN GmbH & Co. KG: Jungingen, Germany, 2019.
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, 1269–1324. [Google Scholar] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- AngioDefender™, Medical Device; Everist Genomics, Inc.: Ann Arbor, MI, USA, 2019.
- Vascular Age Calculator™ (VAC), Version 4.0.8; Everist Health: Ann Arbor, MI, USA, 2020.
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Sherrington, A.; Newham, J.J.; Bell, R.; Adamson, A.; McColl, E.; Araujo-Soares, V. Systematic review and meta-analysis of internet-delivered interventions providing personalized feedback for weight loss in overweight and obese adults. Obes. Rev. 2016, 17, 541–551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chambliss, H.O.; Huber, R.C.; Finley, C.E.; McDoniel, S.O.; Kitzman-Ulrich, H.; Wilkinson, W.J. Computerized self-monitoring and technology-assisted feedback for weight loss with and without an enhanced behavioral component. Patient Educ. Couns. 2011, 85, 375–382. [Google Scholar] [CrossRef]
- Pahlke, F.; König, I.R.; Zielger, A. Randomization in Treatment Arms (RITA): Ein Randomisierungs-Programm für klinische Studien. Inform. Biom. Epidemiol. Med. Bio. 2004, 35, 1–22. [Google Scholar]
- IBM SPSS Statistics, Version 28.0.0.0; IBM Corporation: Armonk, NY, USA, 2021.
- R Core Team. R: A Language and Environment for Statistical Computing, Version 4.0.5; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- RStudio Team. RStudio: Integrated Development for R, Version 1.4.1106; RStudio, Inc.: Boston, MA, USA, 2021. [Google Scholar]

| Outcome | Measurement Time Point | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| t0 1 | t1 2 | t2 3 | t3 4 | ||||||
| primary | health goal achievement | Fclin | cardiorespiratory fitness | maximum oxygen uptake (VO2max) (ml/min/kg) | x | x | x | x | |
| Wclin | anthropometry | body weight (kg) | x | x | x | x | |||
| secondary | behavioral | Fclin Wclin | physical activity behavior | steps taken (steps/day) | x | x | x | x | |
| sedentary behavior (minutes/day) | |||||||||
| physical activity (light, moderate, vigorous intensity) (minutes/week) | |||||||||
| Fclin Wclin | dietary behavior | energy and nutrient intake (kcal, µg, mg, g, %) | x | x | x | x | |||
| food consumption (HEI-NVS 5) (g, ml, score) | |||||||||
| Wclin | energy density (kcal/g) | ||||||||
| physiological | Fclin | musculoskeletal fitness | maximum isometric strength (N, kg, lbs) | x | x | x | x | ||
| Fclin | anthropometry | body weight (kg) | x | x | x | x | |||
| Fclin Wclin | body height (cm) | ||||||||
| body mass index (BMI) (kg/m2) | |||||||||
| fat mass (kg, %) | |||||||||
| fat-free mass (kg, %) | |||||||||
| waist circumference (cm) | |||||||||
| secondary | physiological | Fclin Wclin | blood pressure | systolic blood pressure (mmHg) | x | x | x | x | |
| diastolic blood pressure (mmHg) | |||||||||
| heart rate (bpm) | |||||||||
| Fclin Wclin | blood levels | blood lipids | total cholesterol (mg/dL) | x | x | x | x | ||
| LDL 6 cholesterol (mg/dL) | |||||||||
| HDL 7 cholesterol (mg/dL) | |||||||||
| triglycerides (mg/dL) | |||||||||
| blood glucose | fasting plasma glucose (mg/dL) | x | x | x | x | ||||
| HbA1c 8 (mol/mol Hb, %) | |||||||||
| Fclin Wclin | vascular health | endothelial function (FMD) 9 (%) | x | x | x | x | |||
| vascular age (days) | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brame, J.; Kohl, J.; Wurst, R.; Fuchs, R.; Tinsel, I.; Maiwald, P.; Fichtner, U.; Armbruster, C.; Bischoff, M.; Farin-Glattacker, E.; et al. Health Effects of a 12-Week Web-Based Lifestyle Intervention for Physically Inactive and Overweight or Obese Adults: Study Protocol of Two Randomized Controlled Clinical Trials. Int. J. Environ. Res. Public Health 2022, 19, 1393. https://doi.org/10.3390/ijerph19031393
Brame J, Kohl J, Wurst R, Fuchs R, Tinsel I, Maiwald P, Fichtner U, Armbruster C, Bischoff M, Farin-Glattacker E, et al. Health Effects of a 12-Week Web-Based Lifestyle Intervention for Physically Inactive and Overweight or Obese Adults: Study Protocol of Two Randomized Controlled Clinical Trials. International Journal of Environmental Research and Public Health. 2022; 19(3):1393. https://doi.org/10.3390/ijerph19031393
Chicago/Turabian StyleBrame, Judith, Jan Kohl, Ramona Wurst, Reinhard Fuchs, Iris Tinsel, Phillip Maiwald, Urs Fichtner, Christoph Armbruster, Martina Bischoff, Erik Farin-Glattacker, and et al. 2022. "Health Effects of a 12-Week Web-Based Lifestyle Intervention for Physically Inactive and Overweight or Obese Adults: Study Protocol of Two Randomized Controlled Clinical Trials" International Journal of Environmental Research and Public Health 19, no. 3: 1393. https://doi.org/10.3390/ijerph19031393
APA StyleBrame, J., Kohl, J., Wurst, R., Fuchs, R., Tinsel, I., Maiwald, P., Fichtner, U., Armbruster, C., Bischoff, M., Farin-Glattacker, E., Lindinger, P., Bredenkamp, R., Gollhofer, A., & König, D. (2022). Health Effects of a 12-Week Web-Based Lifestyle Intervention for Physically Inactive and Overweight or Obese Adults: Study Protocol of Two Randomized Controlled Clinical Trials. International Journal of Environmental Research and Public Health, 19(3), 1393. https://doi.org/10.3390/ijerph19031393






