Characteristics of Clinics without National Health Insurance Contracts: A Nationwide Survey in Taiwan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Background
2.2. Data Sources
2.2.1. The Open Government Data Platform
2.2.2. The NHI Administration Ministry of Health and Welfare Website
2.2.3. Ministry of the Interior Website
2.2.4. Incorporating Development Stratification of Taiwan Townships into Sampling Design of Large-Scale Health Interview Survey
2.3. Data Processing
2.4. Statistical Analysis
2.5. Ethical Approval
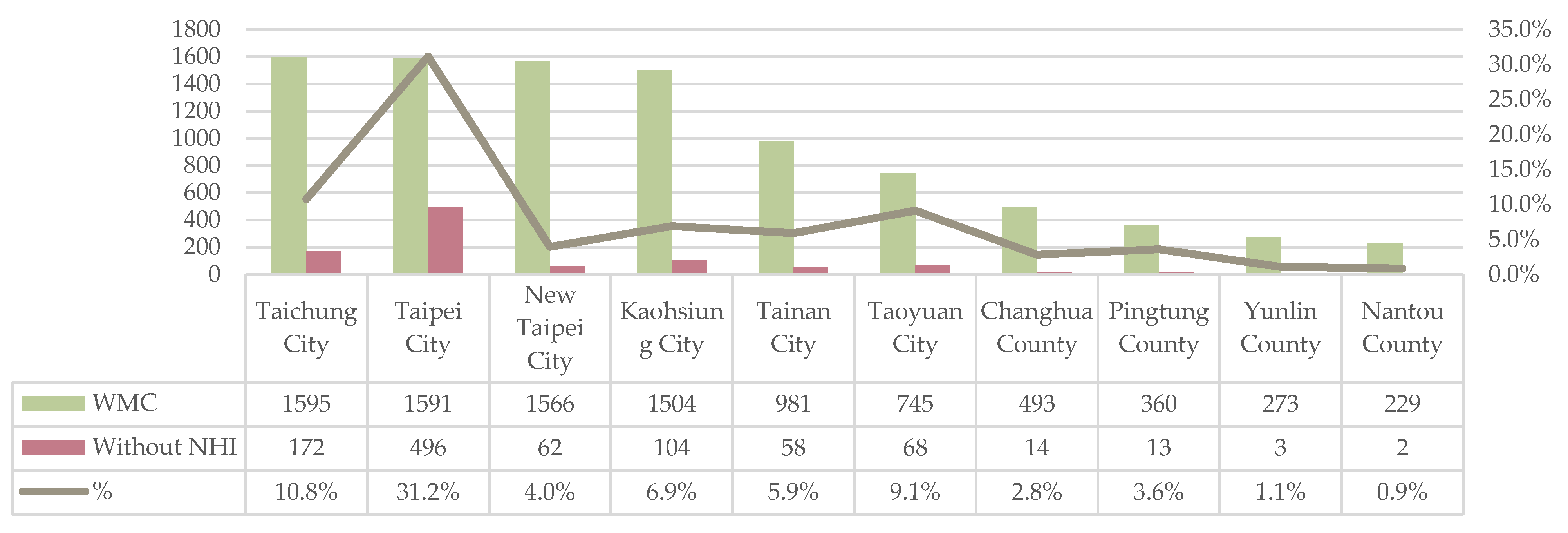
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Declaration of Alma-Ata. Available online: https://cdn.who.int/media/docs/default-source/documents/almaata-declaration-en.pdf?sfvrsn=7b3c2167_2 (accessed on 6 October 2021).
- Wallace, L.S. A view of health care around the world. Ann. Fam. Med. 2013, 11, 84. [Google Scholar] [CrossRef] [PubMed]
- Country Health Profiles. 2021. Available online: https://www.oecd.org/health/country-health-profiles-eu.htm (accessed on 12 June 2021).
- Health-Care Systems: Lessons from the Reform Experience. Available online: https://www.oecd.org/els/health-systems/22364122.pdf (accessed on 12 June 2021).
- García-Prado, A.; González, P. Whom do physicians work for? An analysis of dual practice in the health sector. J. Health Polit. Policy Law 2011, 36, 265–294. [Google Scholar] [CrossRef] [PubMed]
- Tandon, A.; Murray, C.J.; Lauer, J.A.; Evans, D.B.; World Health Organization. Measuring Overall Health System Performance for 191 Countries. Available online: https://www.who.int/healthinfo/paper30.pdf (accessed on 14 October 2021).
- Evans, D.B.; Tandon, A.; Murray, C.J.; Lauer, J.A. Comparative efficiency of national health systems: Cross national econometric analysis. BMJ 2001, 323, 307–310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Camilleri, D.; O’Callaghan, M. Comparing public and private hospital care service quality. Int. J. Health Care Qual. Assur. Inc. Leadersh. Health Serv. 1998, 11, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Kondasani, R.K.; Panda, R.K. Customer perceived service quality, satisfaction and loyalty in Indian private healthcare. Int. J. Health Care Qual. Assur. 2015, 28, 452–467. [Google Scholar] [CrossRef] [PubMed]
- Bhat, R. Characteristics of private medical practice in India: A provider perspective. Health Policy Plan. 1999, 14, 26–37. [Google Scholar] [CrossRef] [PubMed]
- Freed, G.L.; Turbitt, E.; Allen, A. Public or private care: Where do specialists spend their time? Aust. Health Rev. 2017, 41, 541–545. [Google Scholar] [CrossRef]
- Chiang, T.L. Taiwan’s 1995 health care reform. Health Policy 1997, 39, 225–239. [Google Scholar] [CrossRef]
- Cheng, T.M. Taiwan’s new national health insurance program: Genesis and experience so far. Health Aff. 2003, 22, 61–76. [Google Scholar] [CrossRef] [Green Version]
- National Health Insurance Annual Report, 2020–2021. Available online: https://www.nhi.gov.tw/english/Content_List.aspx?n=25A0DB798A6A76B8&topn=BCB2B0D2433F6491 (accessed on 6 October 2021). (In Chinese)
- Wu, T.Y.; Majeed, A.; Kuo, K.N. An overview of the healthcare system in Taiwan. Lond. J. Prim. Care 2010, 3, 115–119. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health and Welfare. Hospital Average Daily Volume. Available online: https://dep.mohw.gov.tw/dos/cp-1735-3243-113.html (accessed on 15 October 2021).
- Diplomate Specialization and Examination Regulations. Available online: https://law.moj.gov.tw/ENG/LawClass/LawAll.aspx?pcode=L0020028 (accessed on 15 October 2021).
- Lu, J.F.R.; Hsiao, W.C. Does universal health insurance make health care unaffordable? Lessons from Taiwan. Health Aff. 2003, 22, 77–88. [Google Scholar] [CrossRef] [PubMed]
- Regulations Governing Contracting and Management of National Health Insurance Medical Care Institutions. Available online: https://law.moj.gov.tw/LawClass/LawAll.aspx?PCode=L0060008 (accessed on 14 October 2021).
- Taiwan Medical Association. Number of Medical Institutions by County and City. Available online: https://www.tma.tw/stats/files/2020/%E8%A1%A84.pdf (accessed on 19 October 2021).
- Bayliss, R.I.S. The National Health Service versus private and complementary medicine. Br. Med. J. 1988, 296, 1457–1459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Humphrey, C.; Russell, J. Motivation and values of hospital consultants in south-east England who work in the National Health Service and do private practice. Soc. Sci. Med. 2004, 59, 1241–1250. [Google Scholar] [CrossRef] [PubMed]
- Basic Information about Medical Institutions and Personnel. Available online: https://data.gov.tw/dataset/15393 (accessed on 2 September 2016).
- Contracted Medical Institutions. National Health Insurance Administration. Available online: https://www.nhi.gov.tw/Content_List.aspx?n=07FEBAA0B8C34D90&topn=D39E2B72B0BDFA15 (accessed on 6 October 2021).
- Monthly Bulletin of Interior Statistics. Available online: https://ws.moi.gov.tw/001/Upload/400/relfile/0/4413/1ef09c4c-ef0e-4035-afdb-ea8fec457491/month/month.html (accessed on 6 October 2021).
- Liu, C.Y.; Hung, Y.T.; Chuang, Y.L.; Chen, Y.J.; Weng, W.S.; Liu, J.S. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J. Health Manag. 2006, 4, 1–22. [Google Scholar]
- Williams, B.; Whatmough, P.; McGill, J.; Rushton, L. Patients and procedures in short-stay independent hospitals in England and Wales, 1997–1998. J. Public Health Med. 2000, 22, 68–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosenthal, M.M. Growth of private medicine in Sweden: The new diversity and the new challenge. Health Policy 1992, 21, 155–166. [Google Scholar] [CrossRef] [Green Version]
- Regidor, E.; Martínez, D.; Calle, M.E.; Astasio, P.; Ortega, P.; Domínguez, V. Socioeconomic patterns in the use of public and private health services and equity in health care. BMC Health Serv. Res. 2008, 8, 183. [Google Scholar] [CrossRef] [Green Version]
- SenGupta, A.; Nundy, S. The private health sector in India. BMJ 2005, 331, 1157–1158. [Google Scholar] [CrossRef]
- Oliver, D.D. Oliver: Private practice by NHS doctors—Still controversial? BMJ 2018, 362, k3480. [Google Scholar] [CrossRef] [Green Version]
- Brekke, K.R.; Sørgard, L. Public versus private health care in a National Health Service. Health Econ. 2007, 16, 579–601. [Google Scholar] [CrossRef] [Green Version]
- Socha, K.Z.; Bech, M. Physician dual practice: A review of literature. Health Policy 2011, 102, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Martinussen, P.E.; Magnussen, J. Is having private health insurance associated with less support for public healthcare? Evidence from the Norwegian NHS. Health Policy 2019, 123, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Klein, R. The public private mix in the UK. In The Public Private Mix for Health, 1st ed.; CRC Press: London, UK, 2018; pp. 53–72. [Google Scholar]
- Wen, C.P.; Tsai, S.P.; Chung, W.S.I.A. A 10-year experience with universal health insurance in Taiwan: Measuring changes in health and health disparity. Ann. Intern. Med. 2008, 148, 258–267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Black, N.; Pettigrew, M.; McPherson, K. Comparison of NHS and private patients undergoing elective transurethral resection of the prostate for benign prostatic hypertrophy. Qual. Health Care 1993, 2, 11–16. [Google Scholar] [CrossRef] [Green Version]
- Pager, C.K.; McCluskey, P.J. Public versus private patient priorities and satisfaction in cataract surgery. Clin. Exp. Ophthalmol. 2004, 32, 482–487. [Google Scholar] [CrossRef]
- Ofer, G.; Dsc, B.R.; Greenstein, M.; Benbassat, J.; Halevy, J.; Shapira, S. Public and private patients in Jerusalem hospitals: Who operates on whom? Isr. Med. Assoc. J. 2006, 8, 270–276. [Google Scholar]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, P.-J.; Liu, J.-Y.; Ma, H.; Chen, T.-J.; Chou, L.-F.; Hwang, S.-J. Characteristics of Clinics without National Health Insurance Contracts: A Nationwide Survey in Taiwan. Int. J. Environ. Res. Public Health 2022, 19, 1517. https://doi.org/10.3390/ijerph19031517
Lu P-J, Liu J-Y, Ma H, Chen T-J, Chou L-F, Hwang S-J. Characteristics of Clinics without National Health Insurance Contracts: A Nationwide Survey in Taiwan. International Journal of Environmental Research and Public Health. 2022; 19(3):1517. https://doi.org/10.3390/ijerph19031517
Chicago/Turabian StyleLu, Pei-Jyun, Jui-Yao Liu, Hsin Ma, Tzeng-Ji Chen, Li-Fang Chou, and Shinn-Jang Hwang. 2022. "Characteristics of Clinics without National Health Insurance Contracts: A Nationwide Survey in Taiwan" International Journal of Environmental Research and Public Health 19, no. 3: 1517. https://doi.org/10.3390/ijerph19031517





