Regional Odontodysplasia: A Systematic Review of Case Reports
Abstract
1. Introduction
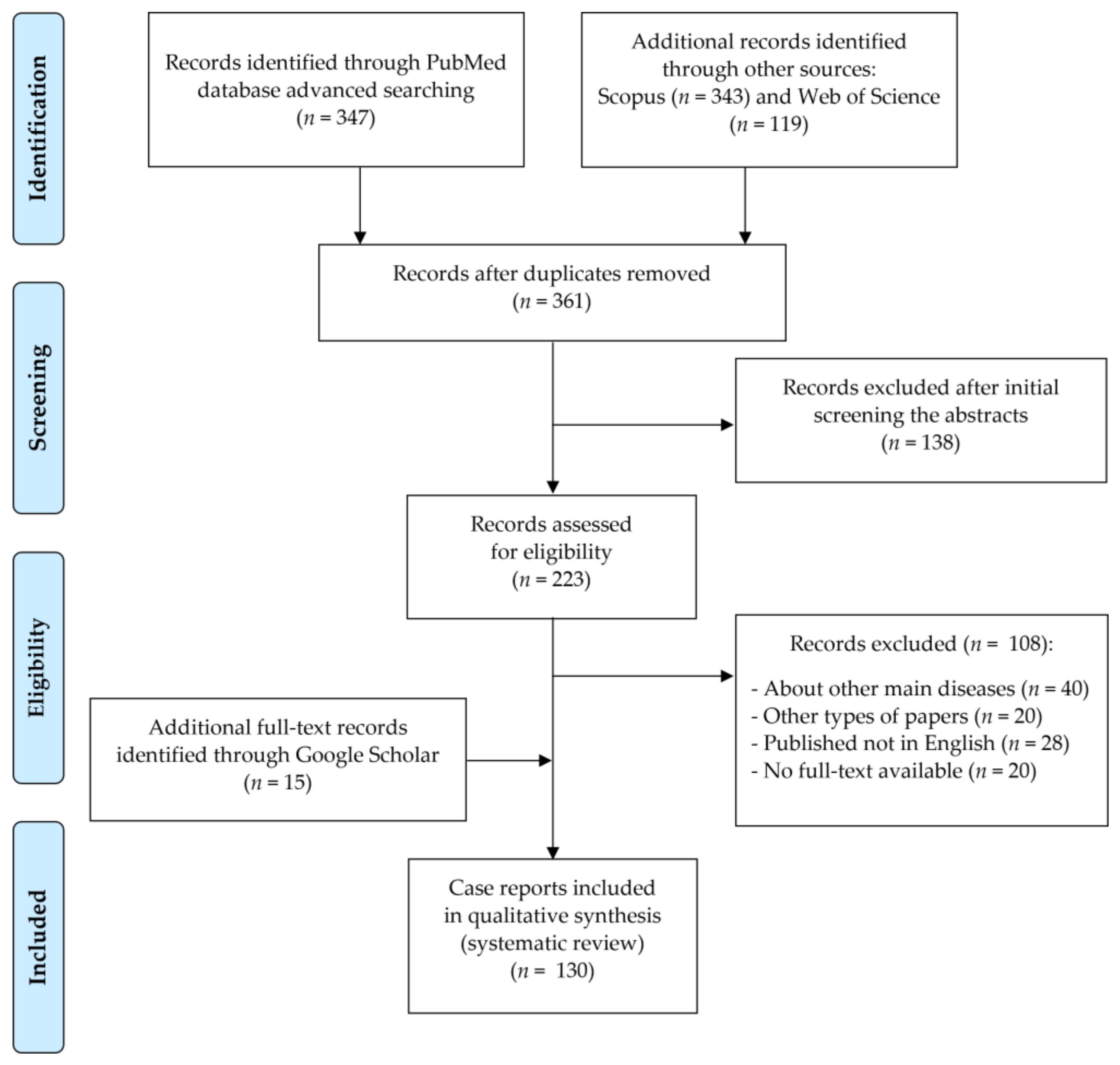
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zegarelli, E.V.; Kutscher, A.H.; Applebaum, E.; Archard, H.O. Odontodysplasia. Oral Surg Oral Med Oral Pathol 1963, 16, 187–193. [Google Scholar] [CrossRef]
- Pandis, N.; Polido, C.; Bell, W.H. Regional Odontodysplasia. A Case Associated with Asymmetric Maxillary and Mandibular Development. Oral Surg. Oral Med. Oral Pathol. 1991, 72, 492–496. [Google Scholar] [CrossRef]
- Cahuana, A.; González, Y.; Palma, C. Clinical Management of Regional Odontodysplasia. Pediatr. Dent. 2005, 27, 34–39. [Google Scholar] [PubMed]
- Gomes, M.P.; Modesto, A.; Cardoso, A.S.; Hespanhol, W. Regional Odontodysplasia: Report of a Case Involving Two Separate Affected Areas. ASDC J. Dent. Child. 1999, 66, 155, 203–207. [Google Scholar] [PubMed]
- Mathew, A.; Dauravu, L.M.; Reddy, S.N.; Kumar, K.R.; Venkataramana, V. Ghost Teeth: Regional Odontodysplasia of Maxillary First Molar Associated with Eruption Disorders in a 10-Year-Old Girl. J. Pharm. Bioallied. Sci. 2015, 7, S800–S803. [Google Scholar] [CrossRef] [PubMed]
- Ponranjini, V.C.; Jayachandran, S.; Bakyalakshmi, K. Regional Odontodysplasia: Report of a Case. J. Dent. Child. 2012, 79, 26–29. [Google Scholar]
- Ozer, L.; Cetiner, S.; Ersoy, E. Regional Odontodysplasia: Report of a Case. J. Clin. Pediatr. Dent. 2004, 29, 45–48. [Google Scholar] [CrossRef]
- Volpato, L.; Botelho, G.; Casela, L.; Borges, A.; Silva, K. Regional Odontodysplasia: Report of a Case in the Mandible Crossing the Midline. J. Contemp. Dent. Pract. 2008, 9, 142–148. [Google Scholar] [CrossRef]
- Ramakrishnan, M.; Menon, P. Odontodysplasia Involving Single Tooth: A Rare Entity. SRM J. Res. Dent. Sci. 2014, 5, 140–142. [Google Scholar] [CrossRef]
- Slootweg, P.J.; Meuwissen, P.R. Regional Odontodysplasia in Epidermal Nevus Syndrome. J. Oral Pathol. 1985, 14, 256–262. [Google Scholar] [CrossRef]
- Steiman, H.R.; Cullen, C.L.; Geist, J.R. Bilateral Mandibular Regional Odontodysplasia with Vascular Nevus. Pediatr. Dent. 1991, 13, 303–306. [Google Scholar] [PubMed]
- Koskinen, S.; Keski-Filppula, R.; Alapulli, H.; Nieminen, P.; Anttonen, V. Familial Oligodontia and Regional Odontodysplasia Associated with a PAX9 Initiation Codon Mutation. Clin. Oral Investig. 2019, 23, 4107–4111. [Google Scholar] [CrossRef] [PubMed]
- Fujiwara, T.; Nakano, K.; Sobue, S.; Ooshima, T. Simultaneous Occurrence of Unusual Odontodysplasia and Oligodontia in the Permanent Dentition: Report of a Case. Int. J. Paediatr. Dent. 2000, 10, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Jahanimoghadam, F.; Pishbin, L.; Rad, M. Clinical, Radiographic, and Histologic Evaluation of Regional Odontodysplasia: A Case Report with 5-Year Follow-Up. J. Dent. 2016, 17, 159–163. [Google Scholar]
- Nijakowski, K.; Surdacka, A. Regional Odontodysplasia—A Rare Developmental Dental Anomaly. Pediatr. Pol. 2021, 96, 153–155. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.; Bossuyt, P.; Boutron, I.; Hoffmann, T.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.; Akl, E.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- OCEBM Levels of Evidence. Available online: https://www.cebm.net/2016/05/ocebm-levels-of-evidence/ (accessed on 22 August 2020).
- Crawford, P.J.; Aldred, M.J. Regional Odontodysplasia: A Bibliography. J. Oral Pathol. Med. 1989, 18, 251–263. [Google Scholar] [CrossRef]
- Tervonen, S.A.; Stratmann, U.; Mokrys, K.; Reichart, P.A. Regional Odontodysplasia: A Review of the Literature and Report of Four Cases. Clin. Oral Investig. 2004, 8, 45–51. [Google Scholar] [CrossRef]
- Alotaibi, O.; Alotaibi, G.; Alfawaz, N. Regional Odontodysplasia: An Analysis of 161 Cases from 1953 to 2017. Saudi Dent. J. 2019, 31, 306–310. [Google Scholar] [CrossRef]
- Courson, F.; Bdeoui, F.; Danan, M.; Degrange, M.; Gogly, B. Regional Odontodysplasia: Expression of Matrix Metalloproteinases and Their Natural Inhibitors. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2003, 95, 60–66. [Google Scholar] [CrossRef]
- Carlos, R.; Contreras-Vidaurre, E.; de Almeida, O.P.; Silva, K.R.; Abrahão, P.G.; Miranda, A.M.M.A.; Pires, F.R. Regional Odontodysplasia: Morphological, Ultrastructural, and Immunohistochemical Features of the Affected Teeth, Connective Tissue, and Odontogenic Remnants. J. Dent. Child. 2008, 75, 144–150. [Google Scholar]
- Miloglu, O.; Goregen, M.; Akgul, H.M.; Harorli, A. Generalized Familial Crown Resorptions in Unerupted Teeth. Eur. J. Dent. 2011, 5, 206–209. [Google Scholar] [CrossRef] [PubMed]
- Clark, S.L.; Cairns, A.M.; Hunter, K.D. Comparative Case Report of Segmental Odontomaxillary Dysplasia and Regional Odontodysplasia. Dent. Update 2014, 41, 825–831. [Google Scholar] [CrossRef]
- Shah, N.; Gupta, Y.K. Generalized Odontodysplasia—A Case Report. J. Indian Soc. Pedod. Prev. Dent. 1998, 16, 40–43. [Google Scholar]
- Ibrahim Mostafa, M.; Samir Taha, N.; Ismail Mehrez, M.A. Generalised versus Regional Odontodysplasia: Diagnosis, Transitional Management, and Long-Term Followup—A Report of 2 Cases. Case Rep. Dent. 2013, 2013, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Jensen, J.L.; Ambjornsen, E.; Haanaes, H.R.; Storhaug, K. Case Report: Unclassified Syndrome Involving Dental Enamel, Dentine and Lack of Tooth Eruption. Eur. Arch. Paediatr. Dent. 2009, 10, 244–247. [Google Scholar] [CrossRef]
- Majumdar, S.; Uppala, D.; Priyanka, K.; Kumar, S. Bilateral Regional Odontodysplasia: A Rare Case Report. Oral Maxillofac. Pathol. J. 2021, 7, 755–757. [Google Scholar]
- Koruyucu, M.; Yaman, D.; Seymen, F.; Demirel, K.; Gençay, K. Management of Regional Odontodysplasia: A 10-Year-Follow-up Case Report and Literature Review. Eur. Oral Res. 2018, 52, 111–116. [Google Scholar] [CrossRef]
- Abdel-Kader, M.A.; Abdelazeem, A.F.; Ahmed, N.E.-M.B.; Khalil, Y.M.; Mostafa, M.I. Oral Rehabilitation of a Case with Regional Odontodysplasia Using a Regenerative Approach-A Case Report and a Review of Literature. Spec. Care Dentist. 2019, 39, 330–339. [Google Scholar] [CrossRef]
- Bagherpoor, M.R.; Siadat, H.; Nokar, S.; Alikhasi, M. Step-by-Step Oral Rehabilitation of a Generalized Odontodysplastic Patient with Implant-Supported Prostheses: A Clinical Report. Implant. Dent. 2010, 19, 122–127. [Google Scholar] [CrossRef]
- Iizawa, F.; Kinjoh, N.; Taguchi, Y. Regional Odontodysplasia: Long-Term Observation of a Case on the Mandibular Left Side. Pediatric Dent. J. 2010, 20, 103–109. [Google Scholar] [CrossRef][Green Version]
- van der Wal, J.E.; Rittersma, J.; Baart, J.A.; van der Waal, I. Regional Odontodysplasia: Report of Three Cases. Int. J. Oral Maxillofac. Surg. 1993, 22, 356–358. [Google Scholar] [CrossRef]
- von Arx, T. Autotransplantation for Treatment of Regional Odontodysplasia. Case Report with 6-Year Follow-Up. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1998, 85, 304–307. [Google Scholar] [CrossRef]
- Ziegler, S.; Neukam, F.W. Regional Odontodysplasia: Orthodontic Treatment and Transplantation of Premolars. Am. J. Orthod. Dentofacial. Orthop. 2012, 142, 710–719. [Google Scholar] [CrossRef]

| Parameter | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | patients with regional odontodysplasia—aged from 0 to 99 years, both sexes | patients with other developmental dental anomalies |
| Intervention | not applicable | |
| Comparison | not applicable | |
| Outcomes | clinical description with radiological features and/or histopathological analyses | only histopathological or another analysis without clinical description |
| Study design | case reports | literature reviews, expert opinion, letters to editor, conference reports, case–control, cohort and cross-sectional studies |
| published up to September 2021 | not published in English |
| All n = 180 | Male n = 88 | Female n = 91 | p-Value | ||
|---|---|---|---|---|---|
| dentition | primary | 5.0 | 3.4 | 6.6 | 0.479 |
| secondary | 28.9 | 29.5 | 27.5 | ||
| both | 66.1 | 67.1 | 65.9 | ||
| jaw | maxilla | 61.1 | 58.0 | 63.7 | 0.680 |
| mandible | 30.0 | 34.0 | 26.4 | ||
| both | 8.9 | 8.0 | 9.9 | ||
| quadrants | 1st | 44.4 | 47.7 | 40.7 | 0.281 |
| 2nd | 45.6 | 37.5 | 53.8 | 0.048 * | |
| 3rd | 25.6 | 27.3 | 24.2 | 0.665 | |
| 4th | 28.9 | 26.1 | 31.9 | 0.497 | |
| affected region | left side of maxilla | 25.0 | 18.2 | 31.9 | 0.362 |
| right side of maxilla | 21.7 | 23.8 | 18.7 | ||
| left side of mandible | 10.0 | 15.9 | 4.4 | ||
| right side of mandible | 11.7 | 12.5 | 11.0 | ||
| bilateral maxilla | 14.4 | 15.9 | 13.2 | ||
| bilateral mandible | 8.3 | 5.7 | 11.0 | ||
| ipsilateral left quadrants | 0.0 | 0.0 | 0.0 | ||
| ipsilateral right quadrants | 1.7 | 2.3 | 1.1 | ||
| contralateral quadrants | 0.0 | 0.0 | 0.0 | ||
| without one quadrant | 1.7 | 2.3 | 1.1 | ||
| generalised | 5.5 | 3.4 | 7.6 |
| Clinical Features | All n = 159 | Male n = 76 | Female n = 83 | p-Value |
| yellowish-brown colour | 90.6 | 89.5 | 91.6 | 0.652 |
| gingival swelling | 67.3 | 55.3 | 78.3 | 0.002 * |
| underdeveloped one side of maxilla/mandible | 17.6 | 21.1 | 14.5 | 0.276 |
| active fistulas | 18.9 | 18.4 | 19.3 | 0.890 |
| tooth mobility | 41.5 | 34.2 | 48.2 | 0.074 |
| early loss of primary teeth | 47.8 | 50.0 | 45.8 | 0.595 |
| delayed tooth eruption | 90.6 | 93.4 | 88.0 | 0.239 |
| local pain | 44.7 | 36.8 | 51.8 | 0.058 |
| Radiological features | All n= 166 | Male n= 79 | Female n= 87 | p-Value |
| ghost teeth | 100 | 100 | 100 | - |
| poorly developed buds | 92.2 | 91.1 | 93.1 | 0.638 |
| periapical lesions | 39.2 | 40.5 | 37.9 | 0.734 |
| Treatment Method | All n = 159 | Male n = 75 | Female n = 83 | p-Value |
|---|---|---|---|---|
| conservative restoration | 14.5 | 18.7 | 10.8 | 0.164 |
| steel crown | 5.7 | 8.0 | 3.6 | 0.235 |
| pulpotomy/RCT | 2.5 | 4.0 | 1.2 | 0.264 |
| tooth extraction | 78.6 | 74.7 | 83.1 | 0.191 |
| acrylic partial denture | 34.6 | 40.0 | 30.1 | 0.193 |
| orthodontic treatment | 16.4 | 21.3 | 12.0 | 0.116 |
| implantoprosthetic treatment | 7.5 | 6.7 | 8.4 | 0.676 |
| autotransplantation | 1.9 | 1.3 | 2.4 | 0.621 |
| Histopathological Features | n = 80 |
|---|---|
| hypoplastic and hypomineralised enamel | 77.5 |
| irregular calcification of dentin | 92.5 |
| irregular dentino–enamel junction | 28.8 |
| pulpal calcifications | 45.0 |
| dislocated cementum | 8.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nijakowski, K.; Woś, P.; Surdacka, A. Regional Odontodysplasia: A Systematic Review of Case Reports. Int. J. Environ. Res. Public Health 2022, 19, 1683. https://doi.org/10.3390/ijerph19031683
Nijakowski K, Woś P, Surdacka A. Regional Odontodysplasia: A Systematic Review of Case Reports. International Journal of Environmental Research and Public Health. 2022; 19(3):1683. https://doi.org/10.3390/ijerph19031683
Chicago/Turabian StyleNijakowski, Kacper, Patryk Woś, and Anna Surdacka. 2022. "Regional Odontodysplasia: A Systematic Review of Case Reports" International Journal of Environmental Research and Public Health 19, no. 3: 1683. https://doi.org/10.3390/ijerph19031683
APA StyleNijakowski, K., Woś, P., & Surdacka, A. (2022). Regional Odontodysplasia: A Systematic Review of Case Reports. International Journal of Environmental Research and Public Health, 19(3), 1683. https://doi.org/10.3390/ijerph19031683








