Football and Zumba Training in Female Hospital Staff: Effects after 12 and 40 Weeks on Self-Reported Health Status, Emotional Wellbeing, General Self-Efficacy and Sleep Problems
Abstract
1. Introduction
2. Materials and Methods
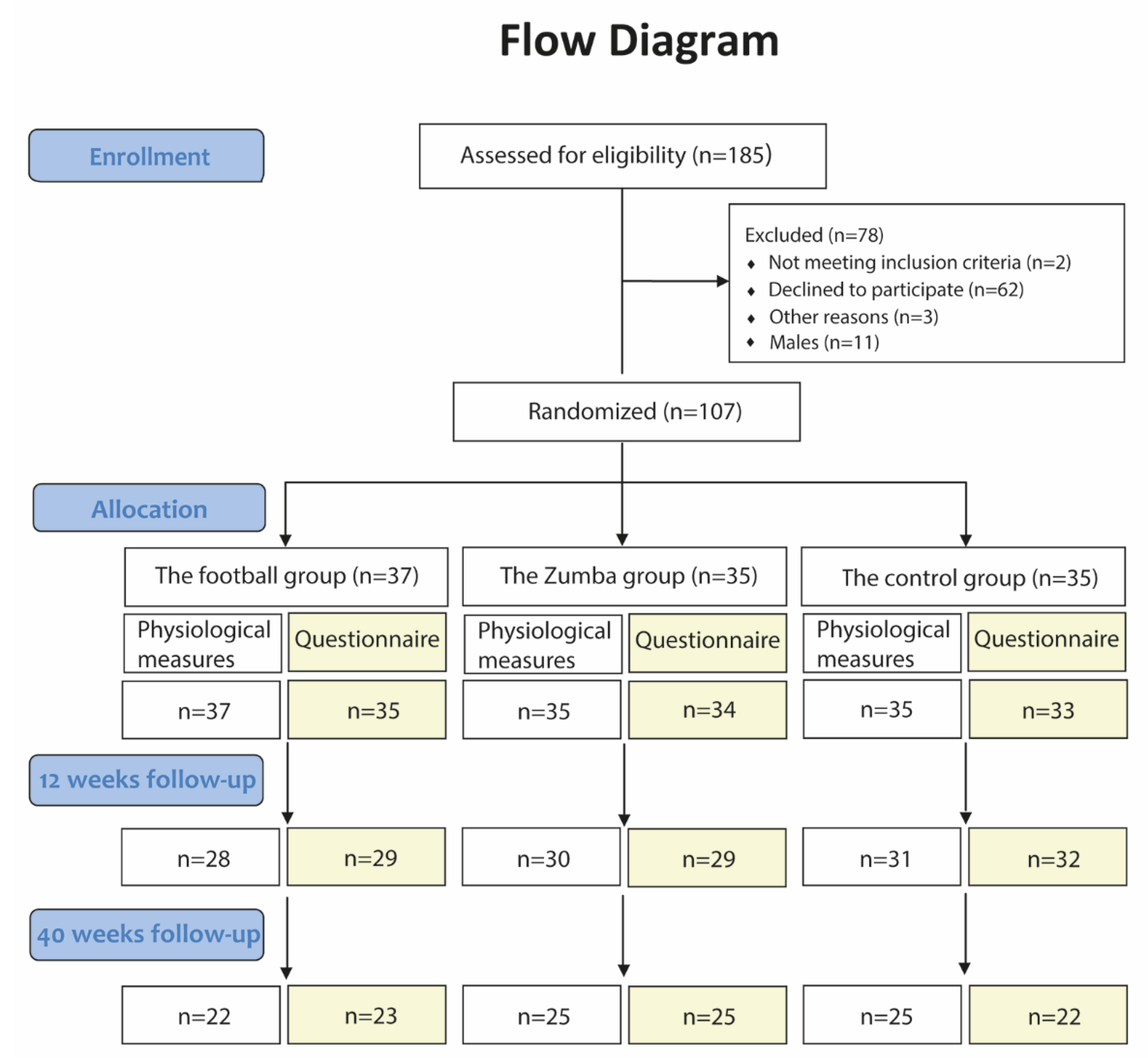
2.1. Study Design
2.2. Recruitment of Participants
2.3. Randomization Procedure
2.4. Intervention Content
2.5. Measurement Procedures Pre, during and Post the Intervention
2.6. Self-Reported Health Status
2.7. Emotional Wellbeing
2.8. General Self-Efficacy
2.9. Sleep
2.10. Statistical Analyses
3. Results
3.1. Baseline Characteristics
3.2. Training Frequency
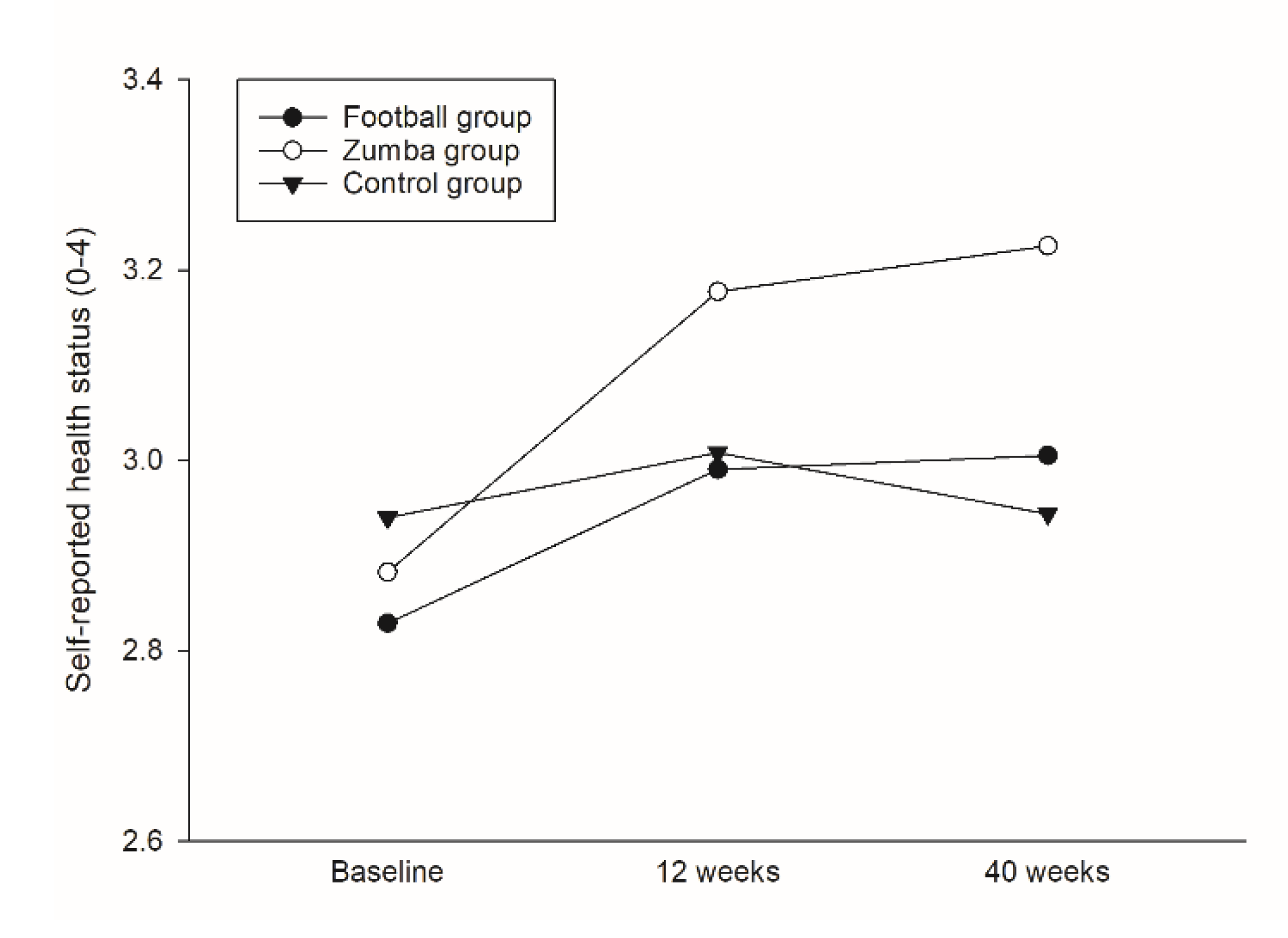
3.3. Self-Reported Health Status
3.4. Emotional Wellbeing
3.5. General Self-Efficacy
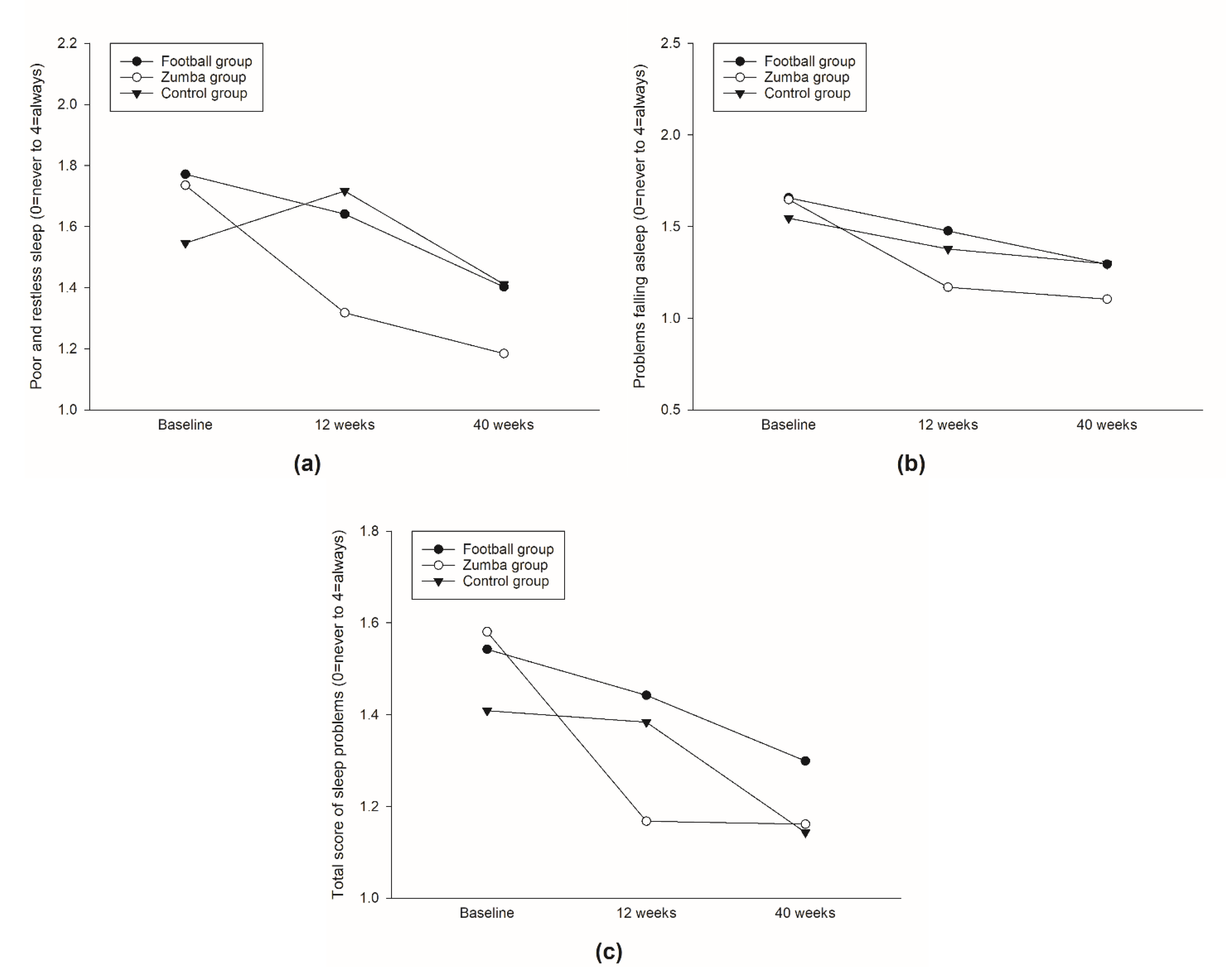
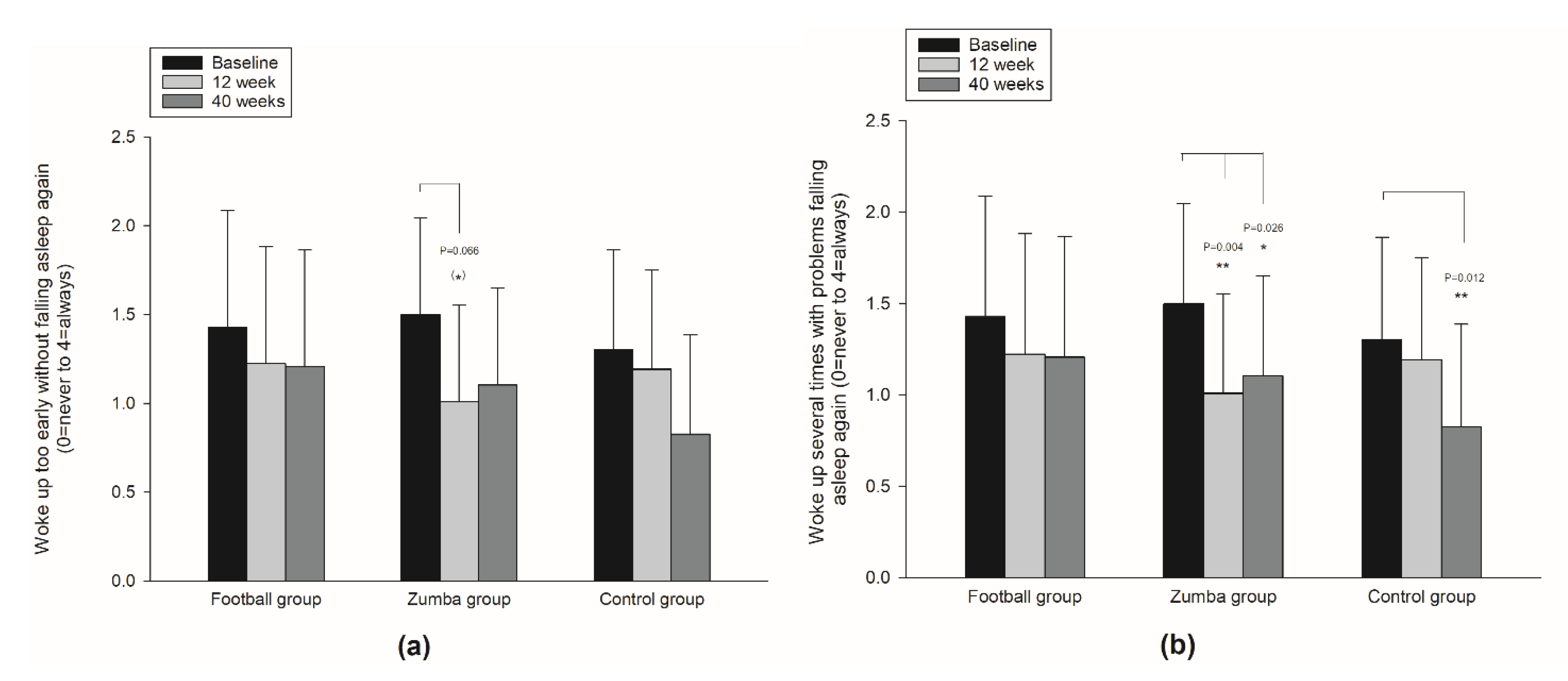
3.6. Sleep
4. Discussion
Strength and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Penque, S. Mindfulness to promote nurses’ well-being. Nurs. Manag. 2019, 50, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Brand, S.L.; Thompson Coon, J.; Fleming, L.E.; Carroll, L.; Bethel, A.; Wyatt, K. Whole-system approaches to improving the health and wellbeing of healthcare workers: A systematic review. PLoS ONE 2017, 12, e0188418. [Google Scholar] [CrossRef] [PubMed]
- Jamali, J.; Roustaei, N.; Ayatollahi, S.M.T.; Sadeghi, E. Factors Affecting Minor Psychiatric Disorder in Southern Iranian Nurses: A Latent Class Regression Analysis. Nurs. Midwifery Stud. 2015, 4, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Pisaniello, S.L.; Winefield, H.R.; Delfabbro, P.H. The influence of emotional labour and emotional work on the occupational health and wellbeing of South Australian hospital nurses. J. Vocat. Behav. 2012, 80, 579–591. [Google Scholar] [CrossRef]
- Mohanty, A.; Kabi, A.; Mohanty, A.P. Health problems in healthcare workers: A review. J Fam. Med. Prim. Care 2019, 8, 2568–2572. [Google Scholar] [CrossRef]
- Lin, P.-Y.; MacLennan, S.; Hunt, N.; Cox, T. The influences of nursing transformational leadership style on the quality of nurses’ working lives in Taiwan: A cross-sectional quantitative study. BMC Nurs. 2015, 14, 1–9. [Google Scholar] [CrossRef][Green Version]
- Gao, T.; Ding, X.; Chai, J.; Zhang, Z.; Zhang, H.; Kong, Y.; Mei, S. The influence of resilience on mental health: The role of general well-being. Int. J. Nurs. Pract. 2017, 23, e12535. [Google Scholar] [CrossRef]
- Yu, F.; Cavadino, A.; Mackay, L.; Ward, K.; King, A.; Smith, M. Physical activity and personal factors associated with nurse resilience in intensive care units. J. Clin. Nurs. 2020, 29, 3246–3262. [Google Scholar] [CrossRef]
- De Oliveira, D.R.; Griep, R.H.; Portela, L.F.; Rotenberg, L. Intention to leave profession, psychosocial environment and self-rated health among registered nurses from large hospitals in Brazil: A cross-sectional study. BMC Health Serv. Res. 2017, 17, 1–10. [Google Scholar] [CrossRef]
- Hasselhorn, H.-M.; Tackenberg, P.; Kuemmerling, A.; Wittenberg, J.; Simon, M.; Conway, P.; Bertazzi, P.; Beermann, B.; Büscher, A.; Camerino, D. Nurses’ health, age and the wish to leave the profession--findings from the European NEXT-Study. La Med. Del Lav. 2006, 97, 207–214. [Google Scholar]
- Josephson, M.; Lindberg, P.; Voss, M.; Alfredsson, L.; Vingård, E. The same factors influence job turnover and long spells of sick leave—a 3-year follow-up of Swedish nurses. Eur. J. Public Health 2008, 18, 380–385. [Google Scholar] [CrossRef]
- Cruz, J.P. Quality of life and its influence on clinical competence among nurses: A self-reported study. J. Clin. Nurs. 2017, 26, 388–399. [Google Scholar] [CrossRef]
- Siffleet, J.; Williams, A.M.; Rapley, P.; Slatyer, S. Delivering best care and maintaining emotional wellbeing in the intensive care unit: The perspective of experienced nurses. Appl. Nurs. Res. 2015, 28, 305–310. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy mechanism in human agency. Am. Psychol. 1982, 37, 122. [Google Scholar] [CrossRef]
- Jordan, T.R.; Khubchandani, J.; Wiblishauser, M. The Impact of Perceived Stress and Coping Adequacy on the Health of Nurses: A Pilot Investigation. Nurs. Res. Pract. 2016, 2016, 5843256. [Google Scholar] [CrossRef]
- Han, Y.; Yuan, Y.; Zhang, L.; Fu, Y. Sleep disorder status of nurses in general hospitals and its influencing factors. Psychiatr. Danub. 2016, 28, 176–183. [Google Scholar]
- Rocha, M.C.P.D.; Martino, M.M.F.D. Stress and sleep quality of nurses working different hospital shifts. Rev. Esc. Enferm. USP 2010, 44, 280–286. [Google Scholar] [CrossRef]
- Geiger-Brown, J.; Trinkoff, A.; Rogers, V.E. The Impact of Work Schedules, Home, and Work Demands on Self-Reported Sleep in Registered Nurses. J. Occup. Environ. Med. 2011, 53, 303–307. [Google Scholar] [CrossRef]
- Feleke, S.A.; Mulatu, M.A.; Yesmaw, Y.S. Medication administration error: Magnitude and associated factors among nurses in Ethiopia. BMC Nurs. 2015, 14, 1–8. [Google Scholar] [CrossRef]
- Tarhan, M.; Aydın, A.; Ersoy, E.; Dalar, L. The sleep quality of nurses and its influencing factors. Eurasian J. Pulmonol. 2018, 20, 78–84. [Google Scholar] [CrossRef]
- Zeng, L.-N.; Yang, Y.; Wang, C.; Li, X.-H.; Xiang, Y.-F.; Hall, B.J.; Ungvari, G.S.; Li, C.-Y.; Chen, C.; Chen, L.-G.; et al. Prevalence of Poor Sleep Quality in Nursing Staff: A Meta-Analysis of Observational Studies. Behav. Sleep Med. 2020, 18, 746–759. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, B.; Mason, O.J. “What is the score?” A review of football-based public mental health interventions. J. Public Ment. Health 2017, 16, 144–158. [Google Scholar] [CrossRef] [PubMed]
- Vendramin, B.; Bergamin, M.; Gobbo, S.; Cugusi, L.; Duregon, F.; Bullo, V.; Zaccaria, M.; Neunhaeuserer, D.; Ermolao, A. Health Benefits of Zumba Fitness Training: A Systematic Review. PM&R 2016, 8, 1181–1200. [Google Scholar] [CrossRef]
- Barene, S.; Krustrup, P.; Jackman, S.R.; Brekke, O.L.; Holtermann, A. Do soccer and Zumba exercise improve fitness and indicators of health among female hospital employees? A 12-week RCT. Scand. J. Med. Sci. Sports 2013, 24, 990–999. [Google Scholar] [CrossRef]
- Barene, S.; Krustrup, P.; Brekke, O.L.; Holtermann, A. Soccer and Zumba as health-promoting activities among female hospital employees: A 40-weeks cluster randomised intervention study. J. Sports Sci. 2014, 32, 1539–1549. [Google Scholar] [CrossRef]
- Barene, S.; Krustrup, P.; Holtermann, A. Effects of the workplace health promotion activities soccer and Zumba on muscle pain, work ability and perceived physical exertion among female hospital employees. PLoS ONE 2014, 9, e115059. [Google Scholar] [CrossRef]
- Barene, S.; Holtermann, A.; Oseland, H.; Brekke, O.-L.; Krustrup, P. Effects on muscle strength, maximal jump height, flexibility and postural sway after soccer and Zumba exercise among female hospital employees: A 9-month randomised controlled trial. J. Sports Sci. 2016, 34, 1849–1858. [Google Scholar] [CrossRef]
- Pohjonen, T.; Ranta, R. Effects of Worksite Physical Exercise Intervention on Physical Fitness, Perceived Health Status, and Work Ability among Home Care Workers: Five-Year Follow-up. Prev. Med. 2001, 32, 465–475. [Google Scholar] [CrossRef]
- Kaleta, D.; Makowiec-Dabrowska, T.; Dziankowska-Zaborszczyk, E.; Jegier, A. Physical activity and self-perceived health status. Int. J. Occup. Med. Environ. Health 2006, 19, 61–69. [Google Scholar] [CrossRef]
- Penedo, F.J.; Dahn, J.R. Exercise and well-being: A review of mental and physical health benefits associated with physical activity. Curr. Opin. Psychiatry 2005, 18, 189–193. [Google Scholar] [CrossRef]
- Aparicio, V.A.; Flor-Alemany, M.; Marín-Jiménez, N.; Coll-Risco, I.; Aranda, P. A 16-week concurrent exercise program improves emotional well-being and emotional distress in middle-aged women: The FLAMENCO project randomized controlled trial. Menopause 2021, 28, 764–771. [Google Scholar] [CrossRef]
- Elavsky, S.; McAuley, E.; Motl, R.W.; Konopack, J.F.; Marquez, D.X.; Hu, L.; Jerome, G.J.; Diener, E. Physical activity enhances long-term quality of life in older adults: Efficacy, esteem, and affective influences. Ann. Behav. Med. 2005, 30, 138–145. [Google Scholar] [CrossRef]
- Lang, C.; Brand, S.; Feldmeth, A.K.; Holsboer-Trachsler, E.; Pühse, U.; Gerber, M. Increased self-reported and objectively assessed physical activity predict sleep quality among adolescents. Physiol. Behav. 2013, 120, 46–53. [Google Scholar] [CrossRef]
- Litleskare, S.; Vaktskjold, A.; Barene, S. A cross-sectional study to examine the association between self-reported sleep and the frequency, duration and intensity of exercise. J. Sports Med. Phys. Fit. 2018, 58, 1635–1641. [Google Scholar] [CrossRef]
- Yang, P.-Y.; Ho, K.-H.; Chen, H.-C.; Chien, M.-Y. Exercise training improves sleep quality in middle-aged and older adults with sleep problems: A systematic review. J. Physiother. 2012, 58, 157–163. [Google Scholar] [CrossRef]
- Hays, R.D.; Sherbourne, C.D.; Mazel, R.M. The rand 36-item health survey 1.0. Health Econ. 1993, 2, 217–227. [Google Scholar] [CrossRef]
- Schwarzer, R. Measurement of perceived self-efficacy: Psychometric scales for cross-cultural research; Freie University: Berlin, Germany, 1993. [Google Scholar]
- Akerstedt, T.; Hume, K.; Minors, D.; Waterhouse, J. The meaning of good sleep: A longitudinal study of polysomnography and subjective sleep quality. J. Sleep Res. 1994, 3, 152–158. [Google Scholar] [CrossRef]
- Hansen, A.M.; Gullander, M.; Hogh, A.; Persson, R.; Kolstad, H.A.; Willert, M.V.; Bonde, J.P.; Kaerlev, L.; Rugulies, R.; Grynderup, M.B. Workplace bullying, sleep problems and leisure-time physical activity: A prospective cohort study. Scand. J. Work. Environ. Health 2016, 42, 26–33. [Google Scholar] [CrossRef]
- Dishman, R.K.; Oldenburg, B.; O’Neal, H.; Shephard, R.J. Worksite physical activity interventions. Am. J. Prev. Med. 1998, 15, 344–361. [Google Scholar] [CrossRef]
- Conn, V.; Hafdahl, A.; Cooper, P.; Brown, L.; Lusk, S. Meta-analysis of workplace physical activity interventions. Am. J. Prev. Med. 2009, 37, 330–339. [Google Scholar] [CrossRef]
- Diggle, P.J.; Heagerty, P.; Liang, K.-Y.; Zeger, S. Analysis of Longitudinal Data; Oxford University Press: Oxford, UK, 2002; pp. 33–113. [Google Scholar]
- Faraway, J.J. Extending the linear model with R: Generalized linear, mixed effects and nonparametric regression models. In Chapman and Hall; CRC: Boca Raton, FL, USA, 2016; pp. 195–248. [Google Scholar]
- Okano, G.; Miyake, H.; Mori, M. Leisure Time Physical Activity as a Determinant of Self-Perceived Health and Fitness in Middle-Aged Male Employees. J. Occup. Health 2003, 45, 286–292. [Google Scholar] [CrossRef]
- Kull, M. The relationships between physical activity, health status and psychological well-being of fertility-aged women. Scand. J. Med. Sci. Sports 2002, 12, 241–247. [Google Scholar] [CrossRef]
- McAuley, E.; Doerksen, S.E.; Morris, K.S.; Motl, R.W.; Hu, L.; Wójcicki, T.R.; White, S.M.; Rosengren, K.R. Pathways from physical activity to quality of life in older women. Ann. Behav. Med. 2008, 36, 13–20. [Google Scholar] [CrossRef]
- Paxton, R.J.; Motl, R.W.; Aylward, A.; Nigg, C.R. Physical activity and quality of life—the complementary influence of self-efficacy for physical activity and mental health difficulties. Int. J. Behav. Med. 2010, 17, 255–263. [Google Scholar] [CrossRef]
- Bandura, A. Foreword. In Self-efficacy in Changing Societies; Cambridge University Press: New York, NY, USA, 1995. [Google Scholar] [CrossRef]
- Qiu, D.; Yu, Y.; Li, R.-Q.; Li, Y.-L.; Xiao, S.-Y. Prevalence of sleep disturbances in Chinese healthcare professionals: A systematic review and meta-analysis. Sleep Med. 2020, 67, 258–266. [Google Scholar] [CrossRef]
- Owens, J.A. Sleep Loss and Fatigue in Healthcare Professionals. J Perinat Neonatal Nurs. 2007, 21, 92–100. [Google Scholar] [CrossRef]
- Kredlow, M.A.; Capozzoli, M.C.; Hearon, B.A.; Calkins, A.W.; Otto, M.W. The effects of physical activity on sleep: A meta-analytic review. J. Behav. Med. 2015, 38, 427–449. [Google Scholar] [CrossRef]

| Characteristics | Football Group | Zumba Group | Control Group | Total | p-Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Age (years) | 44.8 | 8.9 | 46.3 | 9.5 | 47.2 | 9.4 | 46.1 | 9.2 | 0.56 |
| Body mass index (kg/m2) | 24.9 | 3.1 | 25.3 | 2.7 | 26.0 | 3.6 | 25.4 | 3.1 | 0.36 |
| Physical activity level (1–4 scale) | 2.5 | 0.6 | 2.5 | 0.7 | 2.6 | 0.6 | 2.5 | 0.6 | 0.68 |
| Self-reported health status (0–4 scale) | 2.83 | 0.79 | 2.88 | 0.73 | 2.97 | 0.76 | 2.89 | 0.75 | 0.74 |
| Emotional wellbeing (0–100%) | 80.7 | 8.5 | 78.9 | 12.4 | 83.8 | 6.4 | 81.1 | 9.5 | 0.10 |
| General self-efficacy (1–5 scale) | 4.01 | 0.46 | 4.04 | 0.37 | 4.09 | 0.36 | 4.05 | 0.40 | 0.71 |
| Sleep problems past 3 months (0–4 scale) | |||||||||
| Poor and restless sleep | 1.31 | 0.96 | 1.44 | 1.16 | 1.24 | 0.92 | 1.33 | 1.01 | 0.70 |
| Problems falling asleep | 1.66 | 1.00 | 1.65 | 0.88 | 1.53 | 1.11 | 1.61 | 0.99 | 0.84 |
| Woke up too early without falling asleep again | 1.43 | 1.04 | 1.50 | 0.86 | 1.29 | 0.87 | 1.41 | 0.92 | 0.65 |
| Woke up several times and unable to fall asleep again | 1.77 | 0.88 | 1.74 | 0.83 | 1.53 | 0.96 | 1.68 | 0.89 | 0.48 |
| Total score of sleep problems | 1.54 | 0.78 | 1.58 | 0.75 | 1.40 | 0.83 | 1.51 | 0.78 | 0.60 |
| Characteristics | Within-Group Changes | Between-Group Differences | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SG | ZG | CG | SG Group vs. CG | ZG vs. CG | ||||||||
| Change | 95% CI | Change | 95% CI | Change | 95% CI | Diff. | 95% CI | Sig. | Diff. | 95% CI | p-Value | |
| Self-reported health (0–4 scale) | ||||||||||||
| 0–12 weeks | 0.16 | −0.07 to 0.39 | 0.30 * | 0.07 to 0.52 | 0.07 | −0.16 to 0.30 | 0.04 | −0.10 to 0.18 | 0.585 | 0.16 | 0.02 to 0.30 | 0.025 |
| 0–40 weeks | 0.18 | −0.07 to 0.42 | 0.34 ** | 0.11 to 0.58 | 0.00 | −0.25 to 0.26 | ||||||
| Emotional wellbeing (0–100%) | ||||||||||||
| 0–12 weeks | 3.27 * | 0.58 to 5.95 | 3.30 * | 0.60 to 6.00 | 0.99 | −1.69 to 3.67 | −0.10 | −1.81 to 1.62 | 0.913 | −0.24 | −1.94 to 1.47 | 0.786 |
| 0–40 weeks | 2.63 (*) | −0.25 to 5.51 | 4.44 ** | 1.62 to 7.26 | 2.36 | −0.62 to 5.35 | ||||||
| General self-efficacy (1–5 scale) | ||||||||||||
| 0–12 weeks | 0.15 * | 0.03 to 0.26 | −0.02 | −0.13 to 0.10 | −0.03 | −0.14 to 0.08 | 0.03 | −0.04 to 0.10 | 0.375 | 0.00 | −0.07 to 0.07 | 0.933 |
| 0–40 weeks | 0.02 | −0.10 to 0.15 | 0.08 | −0.05 to 0.20 | 0.04 | −0.09 to 0.17 | ||||||
| Sleep problems past 3 months (0–4 scale) | ||||||||||||
| Poor and restless sleep | ||||||||||||
| 0–12 weeks | −0.13 | −0.43 to 0.16 | −0.42 ** | −0.71 to −0.12 | 0.17 | −0.12 to 0.47 | −0.10 | −0.29 to 0.09 | 0.296 | −0.27 | −0.45 to −0.09 | 0.004 |
| 0–40 weeks | −0.37 * | −0.69 to −0.05 | −0.55 *** | −0.86 to −0.24 | −0.14 | −0.46 to 0.19 | ||||||
| Problems falling asleep | ||||||||||||
| 0–12 weeks | −0.18 | −0.45 to 0.09 | −0.48 *** | −0.75 to −0.20 | −0.17 | −0.44 to 0.10 | 0.00 | −0.17 to 0.18 | 0.973 | −0.17 | −0.33 to 0.00 | 0.055 |
| 0–40 weeks | −0.36 * | −0.66 to −0.07 | −0.54 *** | −0.83 to −0.26 | −0.25 | −0.55 to 0.06 | ||||||
| Woke up too early without falling asleep again | ||||||||||||
| 0–12 weeks | 0.08 | −0.24 to 0.39 | −0.30 (*) | −0.62 to 0.02 | 0.01 | −0.30 to 0.33 | 0.06 | −0.14 to 0.26 | 0.525 | −0.08 | −0.28 to 0.12 | 0.423 |
| 0–40 weeks | −0.07 | −0.41 to 0.27 | −0.22 | −0.55 to 0.11 | −0.14 | −0.50 to 0.21 | ||||||
| Woke up several times with problems falling asleep again | ||||||||||||
| 0–12 weeks | −0.20 | −0.54 to 0.13 | −0.49 ** | −0.83 to −0.16 | −0.11 | −0.44 to 0.22 | 0.10 | −0.11 to 0.31 | 0.357 | −0.03 | −0.24 to 0.18 | 0.771 |
| 0–40 weeks | −0.22 | −0.58 to 0.14 | −0.40 * | −0.74 to −0.05 | −0.48 * | −0.85 to −0.11 | ||||||
| Total score of sleep problems | ||||||||||||
| 0–12 weeks | −0.10 | −0.33 to 0.13 | −0.41 *** | −0.65 to −0.18 | −0.03 | −0.26 to 0.21 | 0.01 | −0.13 to 0.16 | 0.865 | −0.14 | −0.29 to 0.00 | 0.051 |
| 0–40 weeks | −0.24 (*) | −0.49 to 0.00 | −0.42 *** | −0.66 to −0.18 | −0.27 * | −0.52 to −0.01 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barene, S.; Krustrup, P. Football and Zumba Training in Female Hospital Staff: Effects after 12 and 40 Weeks on Self-Reported Health Status, Emotional Wellbeing, General Self-Efficacy and Sleep Problems. Int. J. Environ. Res. Public Health 2022, 19, 1685. https://doi.org/10.3390/ijerph19031685
Barene S, Krustrup P. Football and Zumba Training in Female Hospital Staff: Effects after 12 and 40 Weeks on Self-Reported Health Status, Emotional Wellbeing, General Self-Efficacy and Sleep Problems. International Journal of Environmental Research and Public Health. 2022; 19(3):1685. https://doi.org/10.3390/ijerph19031685
Chicago/Turabian StyleBarene, Svein, and Peter Krustrup. 2022. "Football and Zumba Training in Female Hospital Staff: Effects after 12 and 40 Weeks on Self-Reported Health Status, Emotional Wellbeing, General Self-Efficacy and Sleep Problems" International Journal of Environmental Research and Public Health 19, no. 3: 1685. https://doi.org/10.3390/ijerph19031685
APA StyleBarene, S., & Krustrup, P. (2022). Football and Zumba Training in Female Hospital Staff: Effects after 12 and 40 Weeks on Self-Reported Health Status, Emotional Wellbeing, General Self-Efficacy and Sleep Problems. International Journal of Environmental Research and Public Health, 19(3), 1685. https://doi.org/10.3390/ijerph19031685







