An Economic Analysis of Mumps Vaccination in Fiji: Static Model Simulation of Routine Measles–Mumps–Rubella (MMR) Vaccination Instead of Current Measles–Rubella (MR) Vaccination
Abstract
:1. Introduction
2. Materials and Methods
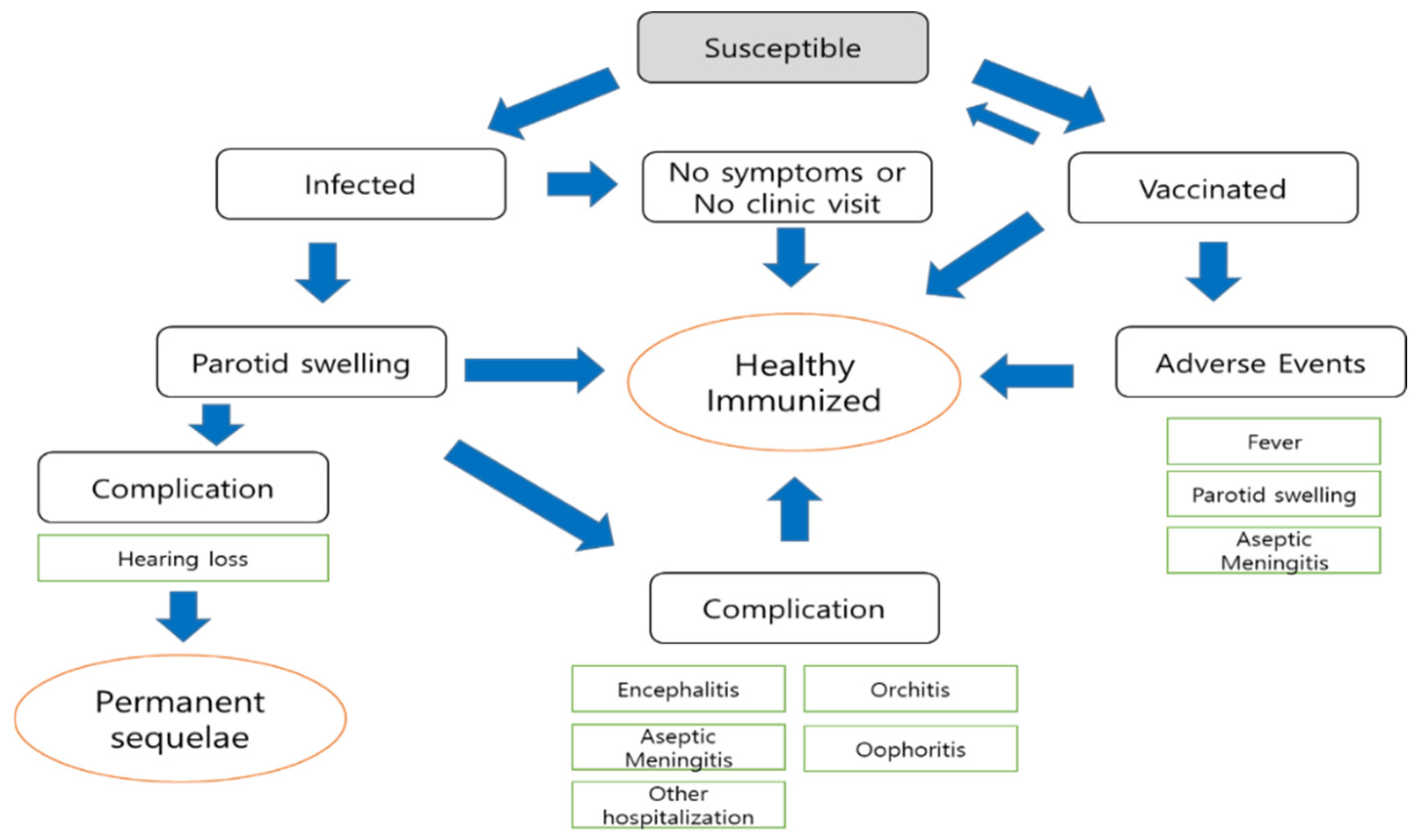
2.1. Estimation of Mumps Incidence and Mumps-Related Complications in Fiji
2.2. Benefits
2.2.1. Benefits from Prevention of Mumps: Opportunity Cost
2.2.2. MMR Vaccine Effectiveness and Vaccination Coverage
2.2.3. Saving Medical Costs
2.2.4. Saving Social Costs
2.3. Cost of MMR Vaccination
2.3.1. Cost of the Mumps Vaccine
2.3.2. Cost of Mumps Vaccination Adverse Events
2.3.3. Discounting
2.4. One-Way and Probabilistic Sensitivity Analysis
3. Results
3.1. Health Effects from the MMR Vaccination
3.2. Benefits
3.3. Costs
3.3.1. Annual Vaccine Costs
3.3.2. Costs from Increased Adverse Events of MMR Vaccination
3.4. Benefit–Cost Ratio of Implementing a Two-Dose MMR Vaccination Program
3.5. Sensitivity Analysis
3.5.1. One-Way Sensitivity Analysis
3.5.2. Probabilistic Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Su, S.-B.; Chang, H.-L.; Chen, K.-T. Current Status of Mumps Virus Infection: Epidemiology, Pathogenesis, and Vaccine. Int. J. Environ. Res. Public Health 2020, 17, 1686. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rubin, S.; Kennedy, R.; Poland, G. Emerging Mumps Infection. Pediatr. Infect. Dis. J. 2016, 35, 799–801. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Immunization Coverage 2018; World Health Organization: Geneva, Switzerland, 2019; Available online: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage (accessed on 17 January 2022).
- WHO. Mumps Virus Vaccine WHO Position Paper; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Edmunds, W.J.; Gay, N.J.; Kretzschmar, M.; Pebody, R.G.; Wachmann, H. The pre-vaccination epidemiology of measles, mumps and rubella in Europe: Implications for modelling studies. Epidemiol. Infect. 2000, 125, 635–650. [Google Scholar] [CrossRef] [PubMed]
- Marlow, M.A.; Marin, M.; Moore, K.; Patel, M. CDC Guidance for Use of a Third Dose of MMR Vaccine during Mumps Outbreaks. J. Public Health Manag. Pract. 2020, 26, 109–115. [Google Scholar] [CrossRef]
- Peltola, H.; Kulkarni, P.S.; Kapre, S.V.; Paunio, M.; Jadhav, S.S.; Dhere, R.M. Mumps Outbreaks in Canada and the United States: Time for New Thinking on Mumps Vaccines. Clin. Infect. Dis. 2007, 45, 459–466. [Google Scholar] [CrossRef] [Green Version]
- Aasheim, E.T.; Inns, T.; Trindall, A.; Emmett, L.; Brown, K.E.; Williams, C.J.; Reacher, M. Outbreak of mumps in a school setting, United Kingdom, 2013. Hum. Vaccines Immunother. 2014, 10, 2446–2449. [Google Scholar] [CrossRef] [Green Version]
- Betáková, T.; Svetlíková, D.; Gocník, M. Overview of measles and mumps vaccine: Origin, present, and future of vaccine production. Acta Virol. 2013, 57, 91–96. [Google Scholar] [CrossRef] [Green Version]
- WHO. Tenth Pacific Immunization Programme Managers Meeting, Nadi, Fiji, 30 July–3 August 2018: Meeting Report; WHO Regional Office for the Western Pacific: Manila, Philippines, 2018. [Google Scholar]
- Fiji MOHMS. National Notifiable Disease Surveillance Bulletin. Mataika House 2016–2018; Ministry of Health and Medical Services: Suva, Fiji, 2019.
- Oh, C. Sudden Hearing Loss after Mumps Outbreak in CWM Hospital; Case Report; Ministry of Health and Medical Services: Suva, Fiji, 2019; in press.
- Colonial War Memorial Hospital. Time to Introduce Mumps Vaccination in Fiji; Hospital Report; Colonial War Memorial Hospital: Suva, Fiji, 2019; in press. [Google Scholar]
- Morita, S.; Fujiwara, K.; Fukuda, A.; Fukuda, S.; Nishio, S.-Y.; Kitoh, R.; Hato, N.; Ikezono, T.; Ishikawa, K.; Kaga, K.; et al. The clinical features and prognosis of mumps-associated hearing loss: A retrospective, multi-institutional investigation in Japan. Acta Oto-Laryngol. 2017, 137 (Suppl. S565), S44–S47. [Google Scholar] [CrossRef]
- Gupta, R.K.; Best, J.; MacMahon, E. Mumps and the UK epidemic 2005. BMJ 2005, 330, 1132–1135. [Google Scholar] [CrossRef]
- Hashimoto, H.; Fujioka, M.; Kinumaki, H.; Group KAPS. An office-based prospective study of deafness in mumps. Pediatr. Infect. Dis. J. 2009, 28, 173–175. [Google Scholar] [CrossRef] [Green Version]
- Hoshi, S.-l.; Kondo, M.; Okubo, I. Economic evaluation of vaccination programme of mumps vaccine to the birth cohort in Japan. Vaccine 2014, 32, 4189–4197. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Reef, S.; Massoudi, M.; Yusuf, H.R.; Bardenheier, B.; Zimmerman, L. An economic analysis of the current universal 2-dose measles-mumps-rubella vaccination program in the United States. J. Infect. Dis. 2004, 189 (Suppl. 1), S131–S145. [Google Scholar] [PubMed]
- Galazka, A.M.; Robertson, S.E.; Kraigher, A. Mumps and mumps vaccine: A global review. Bull. World Health Organ. 1999, 77, 3. [Google Scholar] [PubMed]
- Devi, R.V.L.; Jenkins, K.; Comrie-Thomson, L.; Stewart, T.; Chan, G. Fiji National Immunisation Coverage Survey—2013. Fiji J. Public Health 2014, 3, 8–13. [Google Scholar]
- WHO/UNICEF. WHO and UNICEF Estimates of Immunization Coverage: 2019 Revision; United Nations’ Children’s Fund: Suva, Fiji, 2019. [Google Scholar]
- Irava, W.; Pellny, M.; Khan, I. Costing Study of Selected Health Facilities in Fiji; Ministry of Health and Medical Services: Suva, Fiji, 2012.
- World Bank. Inflation, Consumer Prices, Fiji; World Bank: Washington, DC, USA, 2021; Available online: https://data.worldbank.org/indicator/FP.CPI.TOTL.ZG?end=2017&locations=FJ&most_recent_year_desc=false&start=2012&view=chart (accessed on 5 September 2021).
- World Bank. Life Expectancy at Birth Total, Fiji; World Bank: Washington, DC, USA, 2021; Available online: https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=FJ (accessed on 6 October 2021).
- Kutty, P.K.; Kyaw, M.H.; Dayan, G.H.; Brady, M.T.; Bocchini, J.J.A.; Reef, S.E.; Bellini, W.J.; Seward, J.F. Guidance for isolation precautions for mumps in the United States: A review of the scientific basis for policy change. Clin. Infect. Dis. 2010, 50, 1619–1628. [Google Scholar] [CrossRef] [PubMed]
- Kitano, T.; Onaka, M.; Ishihara, M.; Nishiyama, A.; Hashimoto, N.; Yoshida, S. Static model simulation for routine mumps vaccination in Japan: With a result of mumps-related complications in a Japanese community hospital. Clin. Exp. Vaccine Res. 2017, 6, 120–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coopers, P.W. Fiji Budget Report 2017–2018; PricewaterhouseCoopers, a Fiji Partnership: London, UK, 2017; p. 1. [Google Scholar]
- UNICEF. Vaccine Price Data; United Nations Children’s Fund: New York, NY, USA, 2021; Available online: https://www.unicef.org/supply/vaccines-pricing-data?page=%2C1#listAnchor (accessed on 6 October 2021).
- Zahraei, S.M.; Zamani, G.; Mohammadbeigi, A.; Asgarian, A.; Afrashteh, S.; Gharibnavaz, H.; Haghgou, M.; Kone, S. Estimation of the wastage rate of MMR and pentavalent vaccines in open and closed vials in three western provinces of Iran. Heliyon 2020, 6, e04016. [Google Scholar] [CrossRef]
- Wallace, A.S.; Willis, F.; Nwaze, E.; Dieng, B.; Sipilanyambe, N.; Daniels, D.; Abanida, E.; Gasasira, A.; Mahmud, M.; Ryman, T.K. Vaccine wastage in Nigeria: An assessment of wastage rates and related vaccinator knowledge, attitudes and practices. Vaccine 2017, 35, 6751–6758. [Google Scholar] [CrossRef]
- Fiji Bureau of Statistics. 2017 Population and Housing Census; Bureau of Statistics: Suva, Fiji, 2018.
- WHO. Information Sheet Observed Rate of Vaccine Reactions Measles Mumps and Rubella Vaccines; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/vaccine_safety/initiative/tools/MMR_vaccine_rates_information_sheet.pdf (accessed on 6 October 2021).
- Koplan, J.P.; Preblud, S.R. A benefit-cost analysis of mumps vaccine. Am. J. Dis. Child. 1982, 136, 362–364. [Google Scholar] [CrossRef]
- McDonald, J.C.; Moore, D.L.; Quennec, P. Clinical and epidemiologic features of mumps meningoencephalitis and possible vaccine-related disease. Pediatr. Infect. Dis. J. 1989, 8, 751–755. [Google Scholar] [CrossRef]
- Berger, S.A.; Ginsberg, G.M.; Slater, P.E. Cost-benefit analysis of routine mumps and rubella vaccination for Israeli infants. Isr. J. Med. Sci. 1990, 26, 74–80. [Google Scholar] [PubMed]
- Ministry of HEALTH & Medical Service. Budget 2018–2019 Highlights; MoHMS: Suva, Fiji, 2018. Available online: https://www.health.gov.fj/wp-content/uploads/2018/12/12-July.pdf (accessed on 7 December 2021).
- The Pacific Community. 6th Head of Health Meeting Report; The Pacific Community: Suva, Fiji, 2018; Available online: https://www.spc.int/sites/default/files/eventfiles/2019-03/6th_HOH_Fiji%202018%20Meeting%20Report%20and%20annexes.pdf (accessed on 17 August 2021).
- Berg, A.H.; Blume, S.S. Reasonable Grounds? The Delayed Introduction of MMR Vaccine in Denmark and The Netherlands, 1977–1987. Med. Hist. 2020, 64, 355–373. [Google Scholar] [CrossRef]
- WHO. Immunization Agenda 2030: A Global Strategy to Leave No One Behind; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]



| Mumps Short-Term Complica-Tions | Medical Costs | Social Costs | |||||
|---|---|---|---|---|---|---|---|
| Outpatient Visit (Time) | Admission (Days) | Lab Test (Time) | X-ray (Time) | Unit Costs (FJD) | Productivity Loss (Days) | Unit Costs (FJD) | |
| FJD 46.57 /Time | FJD 121.00 /Day | FJD 22.77 /Time | FJD 18.64 /Time | FJD 21.44 /Day | |||
| Mumps (parotitis) | 2 | 0 | 0 | 0 | 93.14 | 5 | 53.60 |
| Aseptic meningitis | 1 | 10 | 1 | 1 | 1297.95 | 10 | 107.20 |
| Encephalitis | 1 | 21 | 3 | 1 | 2674.46 | 22.7 | 243.34 |
| Orchitis | 2 | 0 | 1 | 1 | 134.55 | 4.9 | 52.53 |
| Oophoritis | 2 | 0 | 1 | 1 | 134.55 | 5.3 | 56.82 |
| Other mumps-related hospitalizations | 1 | 5 | 1 | 1 | 692.96 | 5 | 53.60 |
| Mumps Long-Term Complica-Tions | Medical Cost | Social Cost | ||||||
|---|---|---|---|---|---|---|---|---|
| Outpatient Visit (Time) | Hearing Aid (Year) | Lab Test (Time) | Unit Costs (FJD)/Year | Unit Costs (FJD) for Life | Productivity Loss (Days) | Unit Costs (FJD)/Year | Unit Costs (FJD) for Life | |
| FJD 46.57 /Time | FJD 232.84 /Year | FJD 22.77 /Time | 51.1 Year 3% Discount/Year | FJD 21.44 /Day | 51.1 Year 3% Discount/Year | |||
| Permanent hearing impairment | 2 | 1 | 2 | 371.52 | 9938.91 | 4 | 85.76 | 1147.12 |
| Mumps Complications | Incidence (%) | Number of Cases | Reduction in the Number of Cases | Medical Costs per Case (Fj $) | Social Costs per Case (Fj $) | Saved Medical Costs (Fj $) | Saved Social Costs (Fj $) |
|---|---|---|---|---|---|---|---|
| Parotid swelling | 100.00 | 2600.50 | 2324.85 | 93.14 | 53.60 | 216,529.92 | 12,461.80 |
| Aseptic meningitis | 2.23 | 57.99 | 51.84 | 1297.95 | 107.20 | 67,291.01 | 5557.69 |
| Encephalitis | 0.05 | 1.30 | 1.16 | 2674.46 | 243.34 | 3108.86 | 282.87 |
| Orchitis | 0.79 | 20.54 | 18.37 | 134.55 | 52.53 | 2471.16 | 964.74 |
| Oophoritis | 0.10 | 2.60 | 2.32 | 134.55 | 56.82 | 312.80 | 132.09 |
| Hearing loss | 0.10 | 2.60 | 2.32 | 9938.91 | 1147.12 | 23,106.44 | 2666.88 |
| Other hospitalizations | 1.52 | 39.53 | 35.34 | 692.96 | 53.60 | 24,487.76 | 1894.10 |
| Total | 337,307.94 | 136,110.17 |
| Adverse Effect of Mumps Vaccine | Incidence (%) | Number of Cases | Medical Costs per Case (FJD) | Social Costs per Case (FJD) | Total Medical Costs (FJD) | Total Social Costs (FJD) |
|---|---|---|---|---|---|---|
| Parotid swelling | 1.60 | 542.01 | 93.14 | 53.6 | 50,481.48 | 29,051.82 |
| Aseptic meningitis | 0.0457 | 15.48 | 1297.95 | 107.2 | 20,093.82 | 1659.59 |
| Total | 70,575.30 | 30,711.40 |
| Benefits | Costs | Taxpayer’s Perspective | Societal Perspective | |||||
|---|---|---|---|---|---|---|---|---|
| Medical Benefits (1) | Social Benefits (2) | Medical Costs (3) | Social Costs (4) | Vaccine Costs (5) | Net Present Value (1) − (3) − (5) | Benefit–Cost Ratio (1)/((3) + (5)) | Net Present Value (1) + (2) − (3) − (4) − (5) | Benefit–Cost Ratio ((1) + (2))/((3) + (4) + (5)) |
| 337,307.94 | 136,110.17 | 70,575.30 | 30,711.40 | 56,572.92 | 210,159.72 | 2.65 | 315,558.49 | 3.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, C.; Rafai, E.; Cho, Y.; Jun, D.; Cha, S. An Economic Analysis of Mumps Vaccination in Fiji: Static Model Simulation of Routine Measles–Mumps–Rubella (MMR) Vaccination Instead of Current Measles–Rubella (MR) Vaccination. Int. J. Environ. Res. Public Health 2022, 19, 1861. https://doi.org/10.3390/ijerph19031861
Oh C, Rafai E, Cho Y, Jun D, Cha S. An Economic Analysis of Mumps Vaccination in Fiji: Static Model Simulation of Routine Measles–Mumps–Rubella (MMR) Vaccination Instead of Current Measles–Rubella (MR) Vaccination. International Journal of Environmental Research and Public Health. 2022; 19(3):1861. https://doi.org/10.3390/ijerph19031861
Chicago/Turabian StyleOh, Chunghyeon, Eric Rafai, Yinseo Cho, Damin Jun, and Seungman Cha. 2022. "An Economic Analysis of Mumps Vaccination in Fiji: Static Model Simulation of Routine Measles–Mumps–Rubella (MMR) Vaccination Instead of Current Measles–Rubella (MR) Vaccination" International Journal of Environmental Research and Public Health 19, no. 3: 1861. https://doi.org/10.3390/ijerph19031861






