Examining Facilitators and Barriers to Cardiac Rehabilitation Adherence in a Low-Resource Setting in Latin America from Multiple Perspectives
Abstract
:1. Introduction
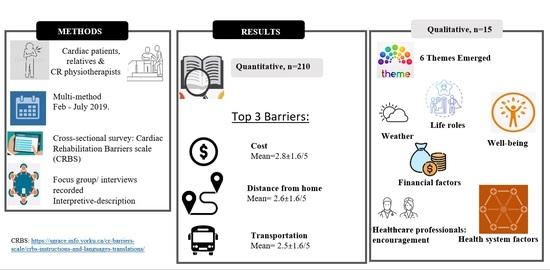
2. Materials and Methods
2.1. Design and Procedure
2.2. Setting
2.3. Participants
2.4. Instruments
2.5. Data Analysis
3. Results
3.1. Respondent Characteristics
3.2. Quantitative Results
3.3. Qualitative Results
3.3.1. Physical and Psychosocial Well-Being
3.3.2. Life Roles
3.3.3. Environmental Factors
3.3.4. Financial Factors
3.3.5. Factors Related to Health Professionals
3.3.6. Health System Factors
3.4. Integration
4. Discussion
Limitations and Directions for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; de Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2017 Update: A Report from the American Heart Association. Circulation 2017, 135, e146–e603. [Google Scholar] [CrossRef]
- Ministerio de Salud y Proteccion Social. Ministerio de Salud y Protección Social Colombia. 2016. Available online: www.minsalud.gov.co/Normatividad_Nuevo/RESOLUCI%C3%93N%204252%20DE%201997.pdf (accessed on 20 December 2020).
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- World Health Organization—Noncommunicable Diseases (NCD) Country Profiles. 2018. Available online: https://www.who.int/nmh/countries/col_en.pdf?ua=1 (accessed on 30 November 2021).
- Camacho, S.; Maldonado, N.; Bustamante, J.; Llorente, B.; Cueto, E.; Cardona, F.; Arango, C. How much for a broken heart? Costs of cardiovascular disease in Colombia using a person-based approach. PLoS ONE 2018, 13, e0208513. [Google Scholar] [CrossRef]
- Grace, S.L.; Turk-Adawi, K.I.; Contractor, A.; Atrey, A.; Campbell, N.; Derman, W.; Melo, G.L.; Oldridge, N.; Sarkar, B.K.; Yeo, T.J.; et al. Cardiac rehabilitation delivery model for low-resource settings. Heart 2016, 102, 1449–1455. [Google Scholar] [CrossRef]
- Kabboul, N.N.; Tomlinson, G.; Francis, T.A.; Grace, S.L.; Chaves, G.; Rac, V.; Daou-Kabboul, T.; Bielecki, J.M.; Alter, D.A.; Krahn, M. Comparative Effectiveness of the Core Components of Cardiac Rehabilitation on Mortality and Morbidity: A Systematic Review and Network Meta-Analysis. J. Clin. Med. 2018, 7, 514. [Google Scholar] [CrossRef] [Green Version]
- Florez, N.; Rodriguez, M.R.A.; Toba, K. Evidencia en la adherencia al programa de rehabilitación cardíaca de la Fundación Cardioinfantil. Bogotá. 2005 a 2009. Ph.D. Thesis, Colombian School of Medicine, Bogota, Colombia, 2010. [Google Scholar]
- Santiago de Araújo Pio, C.; Beckie, T.M.; Varnfield, M.; Sarrafzadegan, N.; Babu, A.S.; Baidya, S.; Buckley, J.; Chen, S.Y.; Gagliardi, A.; Heine, M.; et al. Promoting patient utilization of outpatient cardiac rehabilitation: A joint International Council and Canadian Association of Cardiovascular Prevention and Rehabilitation position statement. Int. J. Cardiol. 2020, 298, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, A.M.; King-Shier, K.M.; Spaling, M.; Duncan, A.; Stone, J.; Jaglal, S.B.; Thompson, D.; Angus, J.E. Factors influencing participation in cardiac rehabilitation programmes after referral and initial attendance: Qualitative systematic review and meta-synthesis. Clin. Rehabil. 2013, 27, 948–959. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, J.; Angarita, A.; Jacome, A.; Malaver, J.; Schmalbach, E.; Diaz, C. Barreras para la participación en programas de rehabilitación cardiaca en pacientes sometidos a revascularización. Rev. Colomb. Cardiol. 2015, 23, 141–147. [Google Scholar]
- Ragupathi, L.; Stribling, J.; Yakunina, Y.; Fuster, V.; McLaughlin, M.A.; Vedanthan, R. Availability, Use, and Barriers to Cardiac Rehabilitation in LMIC. Glob. Heart 2017, 12, 323–334.e10. [Google Scholar] [CrossRef] [Green Version]
- Anchique, C.; Pérez, C.; López, F.; Cortés, M. Estado actual de la rehabilitación cardiovascular en Colombia. Rev. Colomb. Cardiol. 2010, 18, 305–315. [Google Scholar]
- Mair, V.; Breda, A.P.; Nunes, M.E.; Matos, L.D. Evaluating compliance to a cardiac rehabilitation program in a private general hospital. Einstein 2013, 11, 278–284. [Google Scholar] [CrossRef] [Green Version]
- Critchley, K.; Nawal, A.; Benjamin, K. Cardiac rehabilitation programs: An investigation into the reason for non-attendance in Qatar. Innov. Glob. Health Prof. Educ. 2017, 2, 1–11. [Google Scholar] [CrossRef]
- Chai, L.S.; Siop, S.; Putit, Z.; Lim, L.; Gunggu, A.; Tie, S.F. Translation, Adaptation, and Validation of the Malay Version of the Cardiac Rehabilitation Barriers Scale. J. Nurs. Res. 2020, 28, e64. [Google Scholar] [CrossRef]
- Sérvio, T.C.; Britto, R.R.; Ghisi, G.M.L.; da Silva, L.P.; Silva, L.; Lima, M.; Pereira, D.; Grace, S.L. Barriers to cardiac rehabilitation delivery in a low-resource setting from the perspective of healthcare administrators, rehabilitation providers, and cardiac patients. BMC Health Serv. Res. 2019, 19, 615. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanchez, J.A.; Jacome, A.; Pinzon, S. Validez de contenido de la escala de barreras para la rehabilitación cardíaca. Rev. Univ. Y Salud 2015, 17, 170–176. [Google Scholar] [CrossRef] [Green Version]
- Sánchez, J.; Jácome, A.; Larios, B.; Pinzón, S.; Angarita, A. Confiabilidad de la escala de bareras para la rehabilitación cardíaca. Rev. Colomb. Cardiol. 2018, 25, 84–91. [Google Scholar]
- Shanmugasegaram, S.; Gagliese, L.; Oh, P.; Stewart, D.E.; Brister, S.J.; Chan, V.; Grace, S.L. Psychometric validation of the cardiac rehabilitation barriers scale. Clin. Rehabil. 2012, 26, 152–164. [Google Scholar] [CrossRef] [Green Version]
- Dowding, D. Best Practices for Mixed Methods Research in the Health Sciences. John W. Creswell, Ann Carroll Klassen, Vicki L. Plano Clark, Katherine Clegg Smith for the Office of Behavioral and Social Sciences Research; Qualitative Methods Overview Jo Moriarty. Qual. Soc. Work 2013, 12, 541–545. [Google Scholar] [CrossRef]
- Guetterman, T.C.; Fetters, M.D.; Creswell, J.W. Integrating Quantitative and Qualitative Results in Health Science Mixed Methods Research through Joint Displays. Ann. Fam. Med. 2015, 13, 554–561. [Google Scholar] [CrossRef]
- Fetters, M.D.; Curry, L.A.; Creswell, J.W. Achieving integration in mixed methods designs-principles and practices. Health Serv. Res. 2013, 48, 2134–2156. [Google Scholar] [CrossRef] [Green Version]
- Supervia, M.; Turk-Adawi, K.; Lopez-Jimenez, F.; Pesah, E.; Ding, R.; Britto, R.R.; Bjarnason-Wehrens, B.; Derman, W.; Abreu, A.; Babu, A.; et al. Nature of cardiac rehabilitation around the globe. Eclinical. Med. 2019, 13, 46–56. [Google Scholar] [CrossRef] [Green Version]
- Sandelowski, M. Focus on research methods whatever happened to qualitative description? Res. Nurs. Health 2000, 23, 334–340. [Google Scholar] [CrossRef]
- Bäck, M.; Cider, A.; Herlitz, J.; Lundberg, M.; Jansson, B. Kinesiophobia mediates the influences on attendance at exercise-based cardiac rehabilitation in patients with coronary artery disease. Physiother. Theory Pract. 2016, 32, 571–580. [Google Scholar] [CrossRef]
- Bäck, M.; Öberg, B.; Krevers, B. Important aspects in relation to patients’ attendance at exercise-based cardiac rehabilitation - facilitators, barriers and physiotherapist’s role: A qualitative study. BMC Cardiovasc. Disord. 2017, 17, 77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kocjan, J.; Knapik, A. Barriers of physical activity (kinesiophobia) in patients subjected to cardiac rehabilitation. Balt. J. Health Phys. Act. 2014, 6, 291–297. [Google Scholar] [CrossRef] [Green Version]
- Grace, S.L.; Gravely-Witte, S.; Kayaniyil, S.; Brual, J.; Suskin, N.; Stewart, D.E. A multisite examination of sex differences in cardiac rehabilitation barriers by participation status. J. Womens Health 2009, 18, 209–216. [Google Scholar] [CrossRef] [Green Version]
- Ghisi, G.L.; Dos Santos, R.Z.; Aranha, E.E.; Nunes, A.D.; Oh, P.; Benetti, M.; Grace, S.L. Perceptions of barriers to cardiac rehabilitation use in Brazil. Vasc. Health Risk Manag. 2013, 9, 485–491. [Google Scholar] [CrossRef] [Green Version]
- Kelly, E.; Ivers, N.; Zawi, R.; Barnieh, L.; Manns, B.; Lorenzetti, D.L.; Nicholas, D.; Tonelli, M.; Hemmelgarn, B.; Lewanczuk, R.; et al. Patient navigators for people with chronic disease: Protocol for a systematic review and meta-analysis. Syst. Rev. 2015, 4, 28. [Google Scholar] [CrossRef] [Green Version]
- Reid, R.D.; McDonnell, L.A.; Riley, D.L.; Mark, A.E.; Mosca, L.; Beaton, L.; Papadakis, S.; Blanchard, C.M.; Mochari-Greenberger, H.; O’Farrell, P.; et al. Effect of an intervention to improve the cardiovascular health of family members of patients with coronary artery disease: A randomized trial. Can. Med. Assoc. J. 2014, 186, 23–30. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.; Li, Y.; Chen, J. Hybrid versus traditional cardiac rehabilitation models: A systematic review and meta-analysis. Kardiol. Pol. 2018, 76, 1717–1724. [Google Scholar]

| Variable | Quantitative | Qualitative | |||
|---|---|---|---|---|---|
| n = 210 | % | n = 9 | % | ||
| Sex | Male | 140 | 67 | 6 | 67 |
| Age | Median (SD) | 65 | 12 | 63 | 33 |
| Residence | Rural | 19 | 9 | 1 | 11 |
| Urban | 187 | 91 | 8 | 89 | |
| Marital Status | Single | 30 | 14 | 0 | 0 |
| Divorced | 23 | 11 | 2 | 22 | |
| Married | 92 | 44 | 6 | 67 | |
| Widow/er | 39 | 19 | 0 | 0 | |
| Common-law | 22 | 11 | 1 | 11 | |
| NR | 3 | 1 | 0 | 0 | |
| Socioeconomic Status | Low | 145 | 69 | 7 | 78 |
| Medium, High | 61 | 29 | 2 | 22 | |
| NR | 3 | 1 | 0 | 0 | |
| Health Insurance * | Subsidized | 36 | 17 | 3 | 33 |
| Contributive | 154 | 74 | 4 | 45 | |
| Special/Pre-paid | 18 | 9 | 2 | 22 | |
| NR | 1 | <1 | 0 | 0 | |
| Work Status | Employee | 63 | 30 | 2 | 22 |
| Study and work | 34 | 16 | 0 | 0 | |
| Home-maker / unpaid | 62 | 30 | 2 | 22 | |
| Retired | 14 | 7 | 0 | 0 | |
| On disability or retired | 17 | 8 | 5 | 56 | |
| Unemployed | 19 | 9 | 0 | 0 | |
| Education Level | None/Primary school | 87 | 42 | 3 | 33 |
| Middle school | 48 | 22 | 3 | 33 | |
| Technician | 16 | 8 | 2 | 22 | |
| Post-Graduate | 58 | 28 | 1 | 11 | |
| Household Living Arrangement | Alone | 10 | 5 | 0 | 0 |
| Husband/wife | 83 | 40 | 6 | 67 | |
| Sons | 41 | 20 | 2 | 22 | |
| Other Relatives | 70 | 33 | 1 | 11 | |
| Friends | 5 | 2 | 0 | 0 | |
| CR Indication | AMI/ACS | 103 | 49 | 5 | 56 |
| Bypass | 23 | 11 | 2 | 22 | |
| Angioplasty | 44 | 21 | 0 | 0 | |
| Valvopathy | 17 | 8 | 2 | 22 | |
| Syncope | 6 | 3 | 0 | 0 | |
| Other § | 16 | 8 | 0 | 0 | |
| Physical Disability | No | 196 | 94 | 9 | 100 |
| Yes | 13 | 6 | 0 | 0 | |
| Number of CR Sessions Attended | 1–11 | 141 | 67 | 3 | 33 |
| 12–23 | 37 | 18 | 1 | 11 | |
| 24–36 | 19 | 9 | 1 | 11 | |
| More | 7 | 3 | 2 | 22 | |
| NR | 5 | 2 | 2 | 22 | |
| Barrier | Mean | SD | Median | IQR |
|---|---|---|---|---|
| Distance | 2.6 | 1.6 | 2 | 1–4 |
| Costs | 2.8 | 1.6 | 3 | 1–4 |
| Transport | 2.5 | 1.6 | 2 | 1–4 |
| Family responsibilities | 1.9 | 1.2 | 1 | 1–2 |
| I didn’t know what CR was | 2.3 | 1.5 | 2 | 1–4 |
| I don’t need CR | 1.6 | 0.9 | 1 | 1–2 |
| I already exercise at home, or in my community | 2.1 | 1.3 | 2 | 1–3 |
| Climate conditions | 2.1 | 1.4 | 1 | 1–3 |
| I find exercise tiring and/or painful | 1.8 | 1.2 | 1 | 1–2 |
| Lack of time | 1.9 | 1.2 | 1 | 1–2 |
| Of work responsibilities | 1.7 | 1.2 | 1 | 1–2 |
| Lack of energy | 1.9 | 1.2 | 1 | 1–2 |
| Other health problems | 1.9 | 1.3 | 1 | 1–3 |
| I feel old | 1.6 | 1 | 1 | 1–2 |
| My doctor didn’t refer me | 1.6 | 1 | 1 | 1–2 |
| A lot of people have heart problems and don’t attend | 1.4 | 0.7 | 1 | 1–2 |
| I can manage my problem and don’t need help | 1.3 | 0.6 | 1 | 1–2 |
| I think I was referred but they didn’t call me | 1.4 | 0.8 | 1 | 1–2 |
| A lot of time passed before I could get in the program | 1.7 | 1.2 | 1 | 1–2 |
| I prefer to take care of my own health, not in group Subscales | 1.6 | 1 | 1 | 1–2 |
| Perceived need/ healthcare factors | 1.7 | 0.6 | 1.6 | 1.1–2.1 |
| Logistical factors | 2.4 | 1.1 | 2.2 | 1.4–3.2 |
| Work/time conflicts | 1.8 | 1.0 | 1.5 | 1–2 |
| Comorbidities/ functional status | 1.8 | 0.8 | 1.8 | 1–2.3 |
| Total | 1.9 | 0.6 | 1.9 | 1.4–2.3 |
| Barriers | Facilitators |
|---|---|
| Weather # | Physiological factors +,* |
| Transportation cost +,*,# | Cardiologist and internist physicians +,* |
| Other costs +,* | Physiotherapist +,# |
| Health insurance +,*,# | Group exercise +,*,# |
| Clinic location *,+ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rangel-Cubillos, D.M.; Vega-Silva, A.V.; Corzo-Vargas, Y.F.; Molano-Tordecilla, M.C.; Peñuela-Arévalo, Y.P.; Lagos-Peña, K.M.; Jácome-Hortúa, A.M.; Villamizar-Jaimes, C.J.; Grace, S.L.; Dutra de Souza, H.C.; et al. Examining Facilitators and Barriers to Cardiac Rehabilitation Adherence in a Low-Resource Setting in Latin America from Multiple Perspectives. Int. J. Environ. Res. Public Health 2022, 19, 1911. https://doi.org/10.3390/ijerph19041911
Rangel-Cubillos DM, Vega-Silva AV, Corzo-Vargas YF, Molano-Tordecilla MC, Peñuela-Arévalo YP, Lagos-Peña KM, Jácome-Hortúa AM, Villamizar-Jaimes CJ, Grace SL, Dutra de Souza HC, et al. Examining Facilitators and Barriers to Cardiac Rehabilitation Adherence in a Low-Resource Setting in Latin America from Multiple Perspectives. International Journal of Environmental Research and Public Health. 2022; 19(4):1911. https://doi.org/10.3390/ijerph19041911
Chicago/Turabian StyleRangel-Cubillos, Diana Marcela, Andrea Vanessa Vega-Silva, Yully Fernanda Corzo-Vargas, Maria Camila Molano-Tordecilla, Yesica Paola Peñuela-Arévalo, Karen Mayerly Lagos-Peña, Adriana Marcela Jácome-Hortúa, Carmen Juliana Villamizar-Jaimes, Sherry L. Grace, Hugo Celso Dutra de Souza, and et al. 2022. "Examining Facilitators and Barriers to Cardiac Rehabilitation Adherence in a Low-Resource Setting in Latin America from Multiple Perspectives" International Journal of Environmental Research and Public Health 19, no. 4: 1911. https://doi.org/10.3390/ijerph19041911
APA StyleRangel-Cubillos, D. M., Vega-Silva, A. V., Corzo-Vargas, Y. F., Molano-Tordecilla, M. C., Peñuela-Arévalo, Y. P., Lagos-Peña, K. M., Jácome-Hortúa, A. M., Villamizar-Jaimes, C. J., Grace, S. L., Dutra de Souza, H. C., Angarita-Fonseca, A., & Sánchez-Delgado, J. C. (2022). Examining Facilitators and Barriers to Cardiac Rehabilitation Adherence in a Low-Resource Setting in Latin America from Multiple Perspectives. International Journal of Environmental Research and Public Health, 19(4), 1911. https://doi.org/10.3390/ijerph19041911