The Relationship between Dental Fear and Anxiety, General Anxiety/Fear, Sensory Over-Responsivity, and Oral Health Behaviors and Outcomes: A Conceptual Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
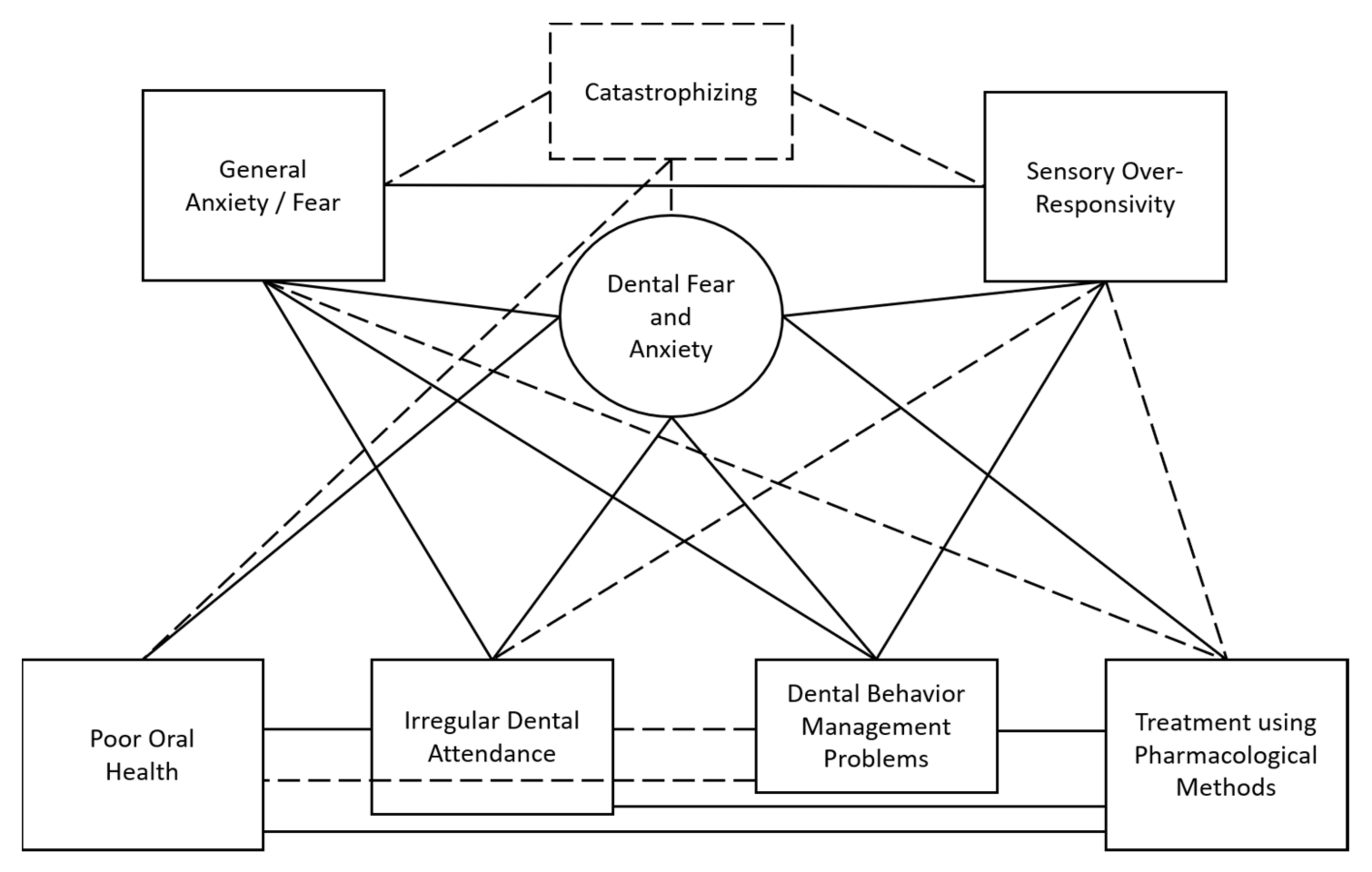
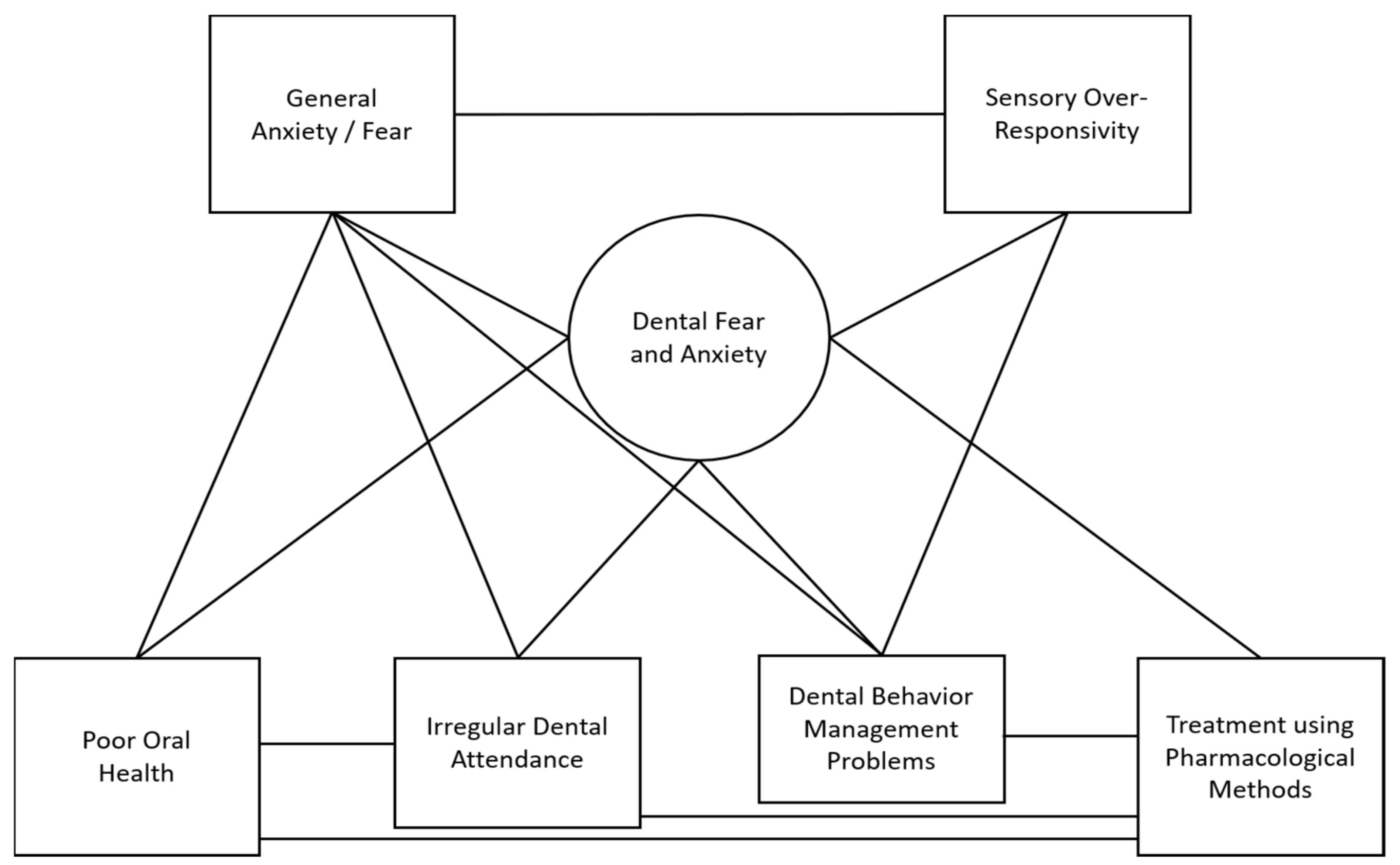
2.3. Model Development
3. Results
3.1. Relationships between Person Factors
3.1.1. DFA: General Anxiety/Fear
3.1.2. DFA: Sensory Over-Responsivity
3.1.3. General Anxiety/Fear: Sensory Over-Responsivity
3.2. Relationships between Oral Health Behaviors and Outcomes and Person Factors
3.2.1. Oral Health: DFA
3.2.2. Oral Health: General Anxiety/Fear
3.2.3. Dental Attendance: DFA
3.2.4. Dental Attendance: General Anxiety/Fear
3.2.5. Dental Behavior Management Problems: DFA
3.2.6. Dental Behavior Management Problems: General Anxiety/Fear
3.2.7. Dental Behavior Management Problems: Sensory Over-Responsivity
3.2.8. Use of Pharmacological Interventions: DFA
3.3. Relationships between Oral Health Behaviors and Outcomes
3.3.1. Oral Health: Dental Attendance
3.3.2. Oral Health: Pharmacological Methods
3.3.3. Dental Behavior Management Problems: Pharmacological Methods
3.3.4. Dental Attendance: Pharmacological Methods
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Armfield, J.M. How do we measure dental fear and what are we measuring anyway? Oral Health Prev. Dent. 2010, 8, 107–115. [Google Scholar]
- Cianetti, S.; Lombardo, G.; Lupatelli, E.; Pagano, S.; Abraha, I.; Montedori, A.; Caruso, S.; Gatto, R.; De Giorgio, S. Dental fear/anxiety among children and adolescents. A systematic review. Eur. J. Paediatr. Dent. 2017, 18, 121–130. [Google Scholar]
- Coxon, J.D.; Hosey, M.T.; Newton, J.T. The oral health of dentally anxious five- and eight-year-olds: A secondary analysis of the 2013 Child Dental Health Survey. Br. Dent. J. 2019, 226, 503–507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guentsch, A.; Stier, C.; Raschke, G.F.; Peisker, A.; Fahmy, M.D.; Kuepper, H.; Schueler, I. Oral health and dental anxiety in a German practice-based sample. Clin. Oral Investig. 2017, 21, 1675–1680. [Google Scholar] [CrossRef] [PubMed]
- Kakkar, M.; Wahi, A.; Thakkar, R.; Vohra, I.; Shukla, A.K. Prevalence of dental anxiety in 10-14 years old children and its implications. J. Dent. Anesth. Pain Med. 2016, 16, 199–202. [Google Scholar] [CrossRef] [Green Version]
- Murthy, A.K.; Pramila, M.; Ranganath, S. Prevalence of clinical consequences of untreated dental caries and its relation to dental fear among 12–15-year-old schoolchildren in Bangalore city, India. Eur. Arch. Paediatr. Dent. 2014, 15, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Rajasekaran, U.; Singh, M.; Goutam, M.; Bhalla, A.; Grover, N.; Galav, A.; Patil, S. A Cross-sectional Study to assess the Perception of Psychosocial Elements among Pediatric Patients visiting Dental Clinics. J. Contemp. Dent. Pract. 2017, 18, 1021–1024. [Google Scholar] [CrossRef] [PubMed]
- Milgrom, P.; Newton, J.T.; Boyle, C.; Heaton, L.J.; Donaldson, N. The effects of dental anxiety and irregular attendance on referral for dental treatment under sedation within the National Health Service in London. Community Dent. Oral Epidemiol. 2010, 38, 453–459. [Google Scholar] [CrossRef] [PubMed]
- Baier, K.; Milgrom, P.; Russell, S.; Mancl, L.; Yoshida, T. Children’s fear and behavior in private pediatric dentistry practices. Pediatr. Dent. 2004, 26, 316–321. [Google Scholar] [PubMed]
- Jain, A.; Suprabha, B.S.; Shenoy, R.; Rao, A. Association of temperament with dental anxiety and behaviour of the preschool child during the initial dental visit. Eur. J. Oral Sci. 2019, 127, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Savanheimo, N.; Sundberg, S.A.; Virtanen, J.I.; Vehkalahti, M.M. Dental care and treatments provided under general anaesthesia in the Helsinki Public Dental Service. BMC Oral Health 2012, 12, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, Y.-L.; Yen, Y.-Y.; Chen, H.-S.; Liu, Y.-C.; Chang, C.-S.; Chen, C.-M.; Chen, F.-L.; Hsu, C.-C.; Lee, C.-H.; Hu, C.-Y.; et al. Child dental fear in low-income and non-low-income families: A school-based survey study. J. Dent. Sci. 2014, 9, 165–171. [Google Scholar] [CrossRef]
- Ogawa, M.; Harano, N.; Ono, K.; Shigeyama-Tada, Y.; Hamasaki, T.; Watanabe, S. Association between sensory processing and dental fear among female undergraduates in Japan. Acta Odontol. Scand. 2019, 77, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.A.; Bendo, C.B.; Ferreira, M.C.; Paiva, S.M.; Vale, M.P.; Serra-Negra, J.M. Association between Childhood Dental Experiences and Dental Fear among Dental, Psychology and Mathematics Undergraduates in Brazil. Int. J. Environ. Res. Public Health 2012, 9, 4676–4687. [Google Scholar] [CrossRef]
- Locker, D.; Liddell, A.; Dempster, L.; Shapiro, D. Age of onset of dental anxiety. J. Dent. Res. 1999, 78, 790–796. [Google Scholar] [CrossRef]
- Seligman, L.D.; Hovey, J.D.; Chacon, K.; Ollendick, T.H. Dental anxiety: An understudied problem in youth. Clin. Psychol. Rev. 2017, 55, 25–40. [Google Scholar] [CrossRef]
- Grisolia, B.M.; dos Santos, A.P.P.; D’Hyppolito, I.M.; Buchanan, H.; Hill, K.; Oliveira, B.H. Prevalence of dental anxiety in children and adolescents globally: A systematic review with meta-analyses. Int. J. Paediatr. Dent. 2021, 31, 168–183. [Google Scholar] [CrossRef]
- Uziel, N.; Meyerson, J.; Winocur, E.; Nabriski, O.; Eli, I. Management of the Dentally Anxious Patient: The Dentist’s Perspective. Oral Health Prev. Dent. 2019, 17, 35–41. [Google Scholar] [CrossRef]
- Åstrøm, A.N.; Skaret, E.; Haugejorden, O. Dental anxiety and dental attendance among 25-year-olds in Norway: Time trends from 1997 to 2007. BMC Oral Health 2011, 11, 10. [Google Scholar] [CrossRef] [Green Version]
- Kirova, D.G.; Atanasov, D.T.; Lalabonova, C.K.; Janevska, S. Dental Anxiety in Adults in Bulgaria. Folia Medica 2010, 52, 49–56. [Google Scholar] [CrossRef] [Green Version]
- Saatchi, M.; Abtahi, M.; Mohammadi, G.; Mirdamadi, M.; Binandeh, E.S. The prevalence of dental anxiety and fear in patients referred to Isfahan Dental School, Iran. Dent. Res. J. 2015, 12, 248–253. [Google Scholar]
- Silveira, E.R.; Cademartori, M.G.; Schuch, H.S.; Armfield, J.A.; Demarco, F.F. Estimated prevalence of dental fear in adults: A systematic review and meta-analysis. J. Dent. 2021, 108, 103632. [Google Scholar] [CrossRef] [PubMed]
- Klingberg, A.P.G. Dental anxiety and behaviour management problems in paediatric dentistry—A review of background factors and diagnostics. Eur. Arch. Paediatr. Dent. 2008, 9, 11–15. [Google Scholar] [CrossRef]
- Klingberg, G.; Broberg, A.G. Dental fear/anxiety and dental behaviour management problems in children and adolescents: A review of prevalence and concomitant psychological factors. Int. J. Paediatr. Dent. 2007, 17, 391–406. [Google Scholar] [CrossRef] [PubMed]
- Porritt, J.; Buchanan, H.; Hall, M.; Gilchrist, F.; Marshman, Z. Assessing children’s dental anxiety: A systematic review of current measures. Community Dent. Oral Epidemiol. 2013, 41, 130–142. [Google Scholar] [CrossRef]
- Yon, M.J.Y.; Che, K.J.; Gao, S.S.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. An introduction to assessing dental fear and anxiety in children. Healthcare 2020, 8, 86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Appukuttan, D.P. Strategies to manage patients with dental anxiety and dental phobia: Literature review. Clin. Cosmet. Investig. Dent. 2016, 8, 35–50. [Google Scholar] [CrossRef] [Green Version]
- Armfield, J.M.; Heaton, L.J. Management of fear and anxiety in the dental clinic: A review. Aust. Dent. J. 2013, 58, 390–407. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, T.T.; Dundar, S.; Bozoglan, A.; Karaman, T.; Dildes, N.; Kaya, F.A.; Altintas, E.; Oztekin, F.; Atas, O.; Alan, H. Is there a relation between dental anxiety, fear and general psychological status? Peer J. 2017, 5, e2978. [Google Scholar] [CrossRef] [Green Version]
- Alasmari, A.A.; Aldossari, G.S.; Aldossary, M.S. Dental Anxiety in Children: A Review of the Contributing Factors. J. Clin. Diagn. Res. 2018, 12, SG01–SG03. [Google Scholar] [CrossRef]
- Folayan, M.O.; Idehen, E.E.; Ojo, O.O. The modulating effect of culture on the expression of dental anxiety in children: A literature review. Int. J. Paediatr. Dent. 2004, 14, 241–245. [Google Scholar] [CrossRef] [PubMed]
- Heaton, L.J.; Smith, T.A.; Raybould, T.P. Factors Influencing Use of Dental Services in Rural and Urban Communities: Considerations for Practitioners in Underserved Areas. J. Dent. Educ. 2004, 68, 1081–1089. [Google Scholar] [CrossRef] [PubMed]
- Hilton, I.V.; Stephen, S.; Barker, J.C.; Weintraub, J.A. Cultural factors and children’s oral health care: A qualitative study of carers of young children. Community Dent. Oral Epidemiol. 2007, 35, 429–438. [Google Scholar] [CrossRef]
- Murad, M.H.; Ingle, N.A.; Assery, M.K. Evaluating factors associated with fear and anxiety to dental treatment—A systematic review. J. Fam. Med. Prim. Care 2020, 9, 4530–4535. [Google Scholar] [CrossRef]
- Siegel, K.; Schrimshaw, E.W.; Kunzel, C.; Wolfson, N.H.; Moon-Howard, J.; Moats, H.L.; Mitchell, D.A. Types of Dental Fear as Barriers to Dental Care among African American Adults with Oral Health Symptoms in Harlem. J. Health Care Poor Underserved 2012, 23, 1294–1309. [Google Scholar] [CrossRef] [Green Version]
- Yakar, B.; Kaygusuz, T.O.; Pirinçci, E. Evaluation of Dental Anxiety and Fear in Patients who admitted to the Faculty of Dentistry: Which Patients are More Risky in terms of Dental Anxiety. Ethiop. J. Health Sci. 2019, 29, 719–726. [Google Scholar] [CrossRef]
- Nissan, S.; Yochman, A.; Blumer, S.; Kharouba, J.; Peretz, B. Children’s Responses to Sensory Stimuli and their Behavior in the Dental Office. J. Clin. Pediatr. Dent. 2017, 41, 10–17. [Google Scholar] [CrossRef]
- Cohen, S.M.; Fiske, J.D.; Newton, J.T. The impact of dental anxiety on daily living. Br. Dent. J. 2000, 189, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Alkan, A.; Cakmak, O.; Yilmaz, S.; Cebi, T.; Gurgan, C. Relationship between Psychological Factors and Oral Health Status and Behaviours. Oral Health Prev. Dent. 2015, 13, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Bernson, J.M.; Elfström, M.L.; Hakeberg, M. Dental coping strategies, general anxiety, and depression among adult patients with dental anxiety but with different dental-attendance patterns. Eur. J. Oral Sci. 2013, 121, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, A.; Broberg, A.; Bodin, L.; Berggren, U.; Arnrup, K. Dental behaviour management problems: The role of child personal characteristics. Int. J. Paediatr. Dent. 2010, 20, 242–253. [Google Scholar] [CrossRef] [PubMed]
- Stein, L.I.; Polido, J.C.; Cermak, S.A. Oral care and sensory over-responsivity in children with autism spectrum disorders. Pediatr. Dent. 2013, 35, 230–235. [Google Scholar] [PubMed]
- Stein, L.I.; Lane, C.J.; Williams, M.E.; Dawson, M.E.; Polido, J.C.; Cermak, S.A. Physiological and Behavioral Stress and Anxiety in Children with Autism Spectrum Disorders during Routine Oral Care. BioMed Res. Int. 2014, 2014, 694876. [Google Scholar] [CrossRef] [PubMed]
- Cermak, S.A.; Stein Duker, L.I.; Williams, M.E.; Dawson, M.E.; Lane, C.J.; Polido, J.C. Sensory Adapted Dental Environments to Enhance Oral Care for Children with Autism Spectrum Disorders: A Randomized Controlled Pilot Study. J. Autism Dev. Disord. 2015, 45, 2876–2888. [Google Scholar] [CrossRef] [PubMed]
- Bedi, R.; Sutcliffe, P.; Donnan, P.T.; Mcconnachie, J. The prevalence of dental anxiety in a group of 13- and 14-year-old Scottish children. Int. J. Paediatr. Dent. 1992, 2, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Chellappah, N.K.; Vignehsa, H.; Milgrom, P.; Lam, L.G. Prevalence of dental anxiety and fear in children in Singapore. Community Dent. Oral Epidemiol. 1990, 18, 269–271. [Google Scholar] [CrossRef]
- D’Alessandro, G.; Alkhamis, N.; Mattarozzi, K.; Mazzetti, M.; Piana, G. Fear of dental pain in Italian children: Child personality traits and parental dental fear. J. Public Health Dent. 2016, 76, 179–183. [Google Scholar] [CrossRef]
- Folayan, M.O.; Idehen, E.E.; Ojo, O.O. Dental anxiety in a subpopulation of African children: Parents ability to predict and its relation to general anxiety and behaviour in the dental chair. Eur. J. Paediatr. Dent. 2004, 5, 19–23. [Google Scholar]
- Klingberg, G.; Berggren, U.; Norén, J.G. Dental fear in an urban Swedish child population: Prevalence and concomitant factors. Community Dent Health 1994, 11, 208–214. [Google Scholar] [PubMed]
- Klingberg, G.; Berggren, U.; Carlsson, S.G.; Noren, J.G. Child dental fear: Cause-related factors and clinical effects. Eur. J. Oral Sci. 1995, 103, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Milgrom, P.; Mancl, L.; King, B.; Weinstein, P. Origins of childhood dental fear. Behav. Res. Ther. 1995, 33, 313–319. [Google Scholar] [CrossRef]
- Salem, K.; Kousha, M.; Anissian, A.; Shahabi, A. Dental Fear and Concomitant Factors in 3-6 Year-old Children. J. Dent. Res. Dent. Clin. Dent. Prospect. 2012, 6, 70–74. [Google Scholar] [CrossRef]
- Xiang, B.; Wong, H.M.; Perfecto, A.P.; McGrath, C.P.J. The association of socio-economic status, dental anxiety, and behavioral and clinical variables with adolescents’ oral health-related quality of life. Qual. Life Res. 2020, 29, 2455–2464. [Google Scholar] [CrossRef]
- Moore, R.; Birn, H.; Kirkegaard, E.; Brodsgaard, I.; Scheutz, F. Prevalence and characteristics of dental anxiety in Danish adults. Community Dent. Oral Epidemiol. 1993, 21, 292–296. [Google Scholar] [CrossRef]
- Abrahamsson, K.H.; Berggren, U.; Carlsson, S.G. Psychosocial aspects of dental and general fears in dental phobic patients. Acta Odontol. Scand. 2000, 58, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Boman, U.W.; Lundgren, J.; Berggren, U.; Carlsson, S.G. Psychosocial and dental factors in the maintenance of severe dental fear. Swed. Dent. J. 2010, 34, 121–127. [Google Scholar] [PubMed]
- Doganer, Y.; Aydogan, U.; Yesil, H.U.; Rohrer, J.; Williams, M.D.; Agerter, D.C. Does the trait anxiety affect the dental fear? Braz. Oral Res. 2017, 31, e36. [Google Scholar] [CrossRef] [Green Version]
- Fiset, L.; Milgrom, P.; Weinstein, P.; Melnick, S. Common fears and their relationship to dental fear and utilization of the dentist. Anesth. Prog. 1989, 36, 258–264. [Google Scholar]
- Fuentes, D.; Gorenstein, C.; Hu, L.W. Dental anxiety and trait anxiety: An investigation of their relationship. Br. Dent. J. 2009, 206, E17. [Google Scholar] [CrossRef]
- Hakeberg, M.; Hägglin, C.; Berggren, U.; Carlsson, S.G. Structural relationships of dental anxiety, mood, and general anxiety. Acta Odontol. Scand. 2001, 59, 99–103. [Google Scholar] [CrossRef]
- Kaakko, T.; Milgrom, P.; Coldwell, S.E.; Getz, T.; Weinstein, P.; Ramsay, D.S. Dental fear among university employees: Implications for dental education. J. Dent. Educ. 1998, 62, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Milgrom, P.; Kleinknecht, R.A.; Elliott, J.; Hsing, L.H.; Choo-Soo, T. A cross-cultural cross validation of the dental fear survey in South East Asia. Behav. Res. Ther. 1990, 28, 227–233. [Google Scholar] [CrossRef]
- Pohjola, V.; Mattila, A.K.; Joukamaa, M.; Lahti, S. Anxiety and depressive disorders and dental fear among adults in Finland. Eur. J. Oral Sci. 2011, 119, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Pohjola, V.; Kunttu, K.; Virtanen, J.I. Psychological Distress, Dental Health, and Dental Fear among Finnish University Students: A National Survey. Int. J. Environ. Res. Public Health 2021, 18, 10245. [Google Scholar] [CrossRef]
- Skaret, E.; Raadal, M.; Berg, E.; Kvale, G. Dental anxiety among 18-yr-olds in Norway, Prevalence and related factors. Eur. J. Oral Sci. 1998, 106, 835–843. [Google Scholar] [CrossRef]
- Strøm, K.; Skaare, A.B.; Willumsen, T. Dental anxiety in 18-year-old Norwegians in 1996 and 2016. Acta Odontol. Scand. 2020, 78, 13–19. [Google Scholar] [CrossRef]
- Witcraft, S.M.; Wickenhauser, M.E.; Maack, D.J.; Dixon, L.J. What sensitivities matter in dental anxiety? Investigating sensitivity to anxiety, pain, and disgust. Psychol. Health Med. 2021, 26, 313–321. [Google Scholar] [CrossRef]
- Zinke, A.; Hannig, C.; Berth, H. Psychological distress and anxiety compared amongst dental patients–results of a cross-sectional study in 1549 adults. BMC Oral Health 2019, 19, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Townend, E.; Dimigen, G.; Fung, D. A clinical study of child dental anxiety. Behav. Res. Ther. 2000, 38, 31–46. [Google Scholar] [CrossRef]
- Locker, D.; Poulton, R.; Thomson, W.M. Psychological disorders and dental anxiety in a young adult population. Community Dent. Oral Epidemiol. 2001, 29, 456–463. [Google Scholar] [CrossRef]
- Vanhee, T.; Mourali, S.; Bottenberg, P.; Jacquet, W.; Abbeele, A.V. Stimuli involved in dental anxiety: What are patients afraid of?: A descriptive study. Int. J. Paediatr. Dent. 2020, 30, 276–285. [Google Scholar] [CrossRef]
- Gao, X.; Hamzah, S.; Yiu, C.K.Y.; McGrath, C.; King, N.M.; Knösel, M.; Spallek, H.; Archaya, A.; Lyons, E.; Lu, A.S. Dental Fear and Anxiety in Children and Adolescents: Qualitative Study Using YouTube. J. Med. Internet Res. 2013, 15, e29. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.M.; Watson, R. An exploration of children’s dental anxiety: Triggers, coping and needs. In Stress and Anxiety: Appli-cations to Social and Environmental Threats, Psychological Well-Being, Occupational Challenges, and Developmental Psychology; Logos Verlag: Berlin/Heidelberg, Germany, 2014; pp. 261–270. [Google Scholar]
- O’Grady, A.; Gray-Burrows, K.; Tahmassebi, J. Inside the waiting room: Process drama and dramatic distancing for involving children in research on dental anxiety. Arts Health 2021, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Tahmassebi, J.F.; Malik, M.; Berg, N.; Pavitt, S.; Gray-Burrows, K.; O’Grady, A. Using process drama to explore the causes of dental anxiety in primary-school children. Eur. Arch. Paediatr. Dent. 2021, 22, 869–877. [Google Scholar] [CrossRef]
- Rajeev, A.; Patthi, B.; Janakiram, C.; Singla, A.; Malhi, R.; Kumari, M. Influence of the previous dental visit experience in seeking dental care among young adults. J. Fam. Med. Prim. Care 2020, 9, 609–613. [Google Scholar] [CrossRef] [PubMed]
- Brady, P.; Dickinson, C.; Whelton, H. Dental anxiety prevalence and surgery environment factors: A questionnaire-based sur-vey of attenders in Ireland. SAAD Dig. 2012, 28, 13–22. [Google Scholar]
- Goldsmith, H.H.; Van Hulle, C.A.; Arneson, C.L.; Schreiber, J.E.; Gernsbacher, M.A. A Population-Based Twin Study of Parentally Reported Tactile and Auditory Defensiveness in Young Children. J. Abnorm. Child Psychol. 2006, 34, 378–392. [Google Scholar] [CrossRef] [Green Version]
- Lane, S.J.; Reynolds, S.; Dumenci, L. Sensory Overresponsivity and Anxiety in Typically Developing Children and Children with Autism and Attention Deficit Hyperactivity Disorder: Cause or Coexistence? Am. J. Occup. Ther. 2012, 66, 595–603. [Google Scholar] [CrossRef] [Green Version]
- Kinnealey, M.; Koenig, K.P.; Smith, S. Relationships between Sensory Modulation and Social Supports and Health-Related Quality of Life. Am. J. Occup. Ther. 2011, 65, 320–327. [Google Scholar] [CrossRef] [Green Version]
- Kinnealey, M.; Fuiek, M. The relationship between sensory defensiveness, anxiety, depression and perception of pain in adults. Occup. Ther. Int. 1999, 6, 195–206. [Google Scholar] [CrossRef]
- Neal, J.A.; Edelmann, R.J.; Glachan, M. Behavioural inhibition and symptoms of anxiety and depression: Is there a specific relationship with social phobia? Br. J. Clin. Psychol. 2002, 41, 361–374. [Google Scholar] [CrossRef]
- Pfeiffer, B.; Kinnealey, M. Treatment of sensory defensiveness in adults. Occup. Ther. Int. 2003, 10, 175–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carpenter, K.L.H.; Baranek, G.T.; Copeland, W.E.; Compton, S.; Zucker, N.; Dawson, G.; Egger, H.L. Sensory Over-Responsivity: An Early Risk Factor for Anxiety and Behavioral Challenges in Young Children. J. Abnorm. Child Psychol. 2019, 47, 1075–1088. [Google Scholar] [CrossRef] [PubMed]
- Ben-Sasson, A.; Carter, A.S.; Briggs-Gowan, M.J. Sensory over-responsivity in elementary school: Prevalence and social-emotional correlates. J. Abnorm. Child Psych. 2009, 37, 705–716. [Google Scholar] [CrossRef] [PubMed]
- Engel-Yeger, B.; Dunn, W.W. The relationship between sensory processing difficulties and anxiety level of healthy adults. Br. J. Occup. Ther. 2011, 74, 210–216. [Google Scholar] [CrossRef]
- Locker, D.; Allen, F. What do measures of ‘oral health-related quality of life’ measure? Community Dent. Oral Epidemiol. 2007, 35, 401–411. [Google Scholar] [CrossRef]
- Carrillo-Díaz, M.; Crego, A.; Armfield, J.M.; Romero, M. Self-assessed oral health, cognitive vulnerability and dental anxiety in children: Testing a mediational model. Community Dent. Oral Epidemiol. 2012, 40, 8–16. [Google Scholar] [CrossRef]
- Goyal, A.; Sharma, A.; Gaur, T.; Singh, J.; Pachori, Y.; Chhabra, K.G.; Chhabra, C. Impact of dental fear on oral health-related quality of life among school going and non-school going children in Udaipur city: A cross-sectional study. Contemp. Clin. Dent. 2014, 5, 42–48. [Google Scholar] [CrossRef]
- Luoto, A.; Lahti, S.; Nevanperä, T.; Tolvanen, M.; Locker, D. Oral-health-related quality of life among children with and without dental fear. Int. J. Paediatr. Dent. 2009, 19, 115–120. [Google Scholar] [CrossRef]
- Merdad, L.; El-Housseiny, A.A. Do children’s previous dental experience and fear affect their perceived oral health-related quality of life (OHRQoL)? BMC Oral Health 2017, 17, 47. [Google Scholar] [CrossRef] [Green Version]
- Slabšinskienė, E.; Kavaliauskienė, A.; Žemaitienė, M.; Vasiliauskienė, I.; Zaborskis, A. Dental Fear and Associated Factors among Children and Adolescents: A School-Based Study in Lithuania. Int. J. Environ. Res. Public Health 2021, 18, 8883. [Google Scholar] [CrossRef] [PubMed]
- Almoznino, G.; Zini, A.; Aframian, D.J.; Kaufman, E.; Lvovsky, A.; Hadad, A.; Levin, L. Oral Health Related Quality of Life in Young Individuals with Dental Anxiety and Exaggerated Gag Reflex. Oral Health Prev. Dent 2015, 13, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Costa, F.S.; Cademartori, M.G.; Silva, M.F.; Nascimento, G.; Shqair, A.Q.; Pinheiro, R.T.; Demarco, F.F.; Goettems, M.L. Anxiety symptoms have a direct effect on oral health perception in young women. Qual. Life Res. 2018, 27, 1583–1588. [Google Scholar] [CrossRef]
- Khan, S.D.A.A.; Alqannass, N.M.; Alwadei, M.M.; Alnajrani, M.D.; Alshahrani, Z.M.; Al Alhareth, A.Y.; Alqahtani, K.M. Assessment of the relationship between dental anxiety and oral health-related quality of life. J. Pharm. Bioallied Sci. 2021, 13, 359. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Bhargav, P.; Patel, A.; Bhati, M.; Balasubramanyam, G.; Duraiswamy, P.; Kulkarni, S. Does dental anxiety influence oral health-related quality of life? Observations from a cross-sectional study among adults in Udaipur district, India. J. Oral Sci. 2009, 51, 245–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGrath, C.; Bedi, R. The association between dental anxiety and oral health-related quality of life in Britain. Community Dent. Oral Epidemiol. 2004, 32, 67–72. [Google Scholar] [CrossRef]
- Mehrstedt, M.; John, M.T.; Tönnies, S.; Micheelis, W. Oral health-related quality of life in patients with dental anxiety. Community Dent. Oral Epidemiol. 2007, 35, 357–363. [Google Scholar] [CrossRef]
- Ng, S.K.S.; Leung, W.K. A community study on the relationship of dental anxiety with oral health status and oral health-related quality of life. Community Dent. Oral Epidemiol. 2008, 36, 347–356. [Google Scholar] [CrossRef] [Green Version]
- Pohjola, V.; Lahti, S.; Suominen-Taipale, L.; Hausen, H. Dental fear and subjective oral impacts among adults in Finland. Eur. J. Oral Sci. 2009, 117, 268–272. [Google Scholar] [CrossRef]
- Song, Y.; Luzzi, L.; Chrisopoulos, S.; Brennan, D. Dentist-patient relationships and oral health impact in Australian adults. Community Dent. Oral Epidemiol. 2020, 48, 309–316. [Google Scholar] [CrossRef]
- Sukumaran, I.; Taylor, S.; Thomson, W.M. The Prevalence and Impact of Dental Anxiety among Adult New Zealanders. Int. Dent. J. 2021, 71, 122–126. [Google Scholar] [CrossRef] [PubMed]
- Alsadat, F.A.; El-Housseiny, A.A.; Alamoudi, N.M.; Elderwi, D.A.; Ainosa, A.M.; Dardeer, F.M. Dental fear in primary school chil-dren and its relation to dental caries. Niger. J. Clin. Pract. 2018, 21, 1454–1460. [Google Scholar] [CrossRef] [PubMed]
- Alvesalo, I.; Murtomaa, H.; Milgrom, P.; Honkanen, A.; Karjalainen, M.; Tay, K.-M. The Dental Fear Survey Schedule: A study with Finnish children. Int. J. Paediatr. Dent. 1993, 3, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Barreto, K.A.; Dos Prazeres, L.D.K.T.; Lima, D.S.M.; Soares, F.C.; Redivivo, R.M.M.P.; da Franca, C.; Colares, V. Factors associated with dental anxiety in Brazilian children during the first transitional period of the mixed dentition. Eur. Arch. Paediatr. Dent. 2017, 18, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Chakradhar, K.; Dolar, D.; Kulkarni, S.; Reddy, B.S.; Reddy, M.P.; Srilatha, A. Correlation of dental anxiety with oral health status and treatment needs among 12-year old indian school going children. Acta Biomed. 2020, 91, e2020095. [Google Scholar]
- Dahlander, A.; Soares, F.; Grindefjord, M.; Dahllöf, G. Factors Associated with Dental Fear and Anxiety in Children Aged 7 to 9 Years. Dent. J. 2019, 7, 68. [Google Scholar] [CrossRef] [Green Version]
- Folayan, M.O.; Kolawole, K.A.; Onyejaka, N.K.; Agbaje, H.O.; Chukwumah, N.M.; Oyedele, T.A. General anxiety, dental anxiety, digit sucking, caries and oral hygiene status of children resident in a semi-urban population in Nigeria. BMC Oral Health 2018, 18, 66. [Google Scholar] [CrossRef] [Green Version]
- Goettems, M.L.; Shqair, A.Q.; Bergmann, V.F.; Cadermatori, M.G.; Correa, M.B.; Demarco, F.F. Oral health self-perception, dental caries, and pain: The role of dental fear underlying this association. Int. J. Paediatr. Dent. 2018, 28, 319–325. [Google Scholar] [CrossRef]
- Haworth, S.; Dudding, T.; Waylen, A.; Thomas, S.J.; Timpson, N.J. Ten years on: Is dental general anaesthesia in childhood a risk factor for caries and anxiety? Br. Dent. J. 2017, 222, 299–304. [Google Scholar] [CrossRef] [Green Version]
- Howard, K.E.; Freeman, R. Reliability and validity of a faces version of the Modified Child Dental Anxiety Scale. Int. J. Paediatr. Dent. 2007, 17, 281–288. [Google Scholar] [CrossRef]
- Kim, A.H.; Ahn, E.S.; An, S.Y. Factors affecting dental fear in Korean adolescents. J. Korean Dent. Sci. 2017, 10, 22–28. [Google Scholar] [CrossRef]
- Nermo, H.; Willumsen, T.; Johnsen, J.-A.K. Changes in dental anxiety among 15- to 21-year-olds. A 2-year longitudinal analysis based on the Tromsø study: Fit futures. Community Dent. Oral Epidemiol. 2018, 47, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Nicolas, E.; Bessadet, M.; Collado, V.; Carrasco, P.; Rogerleroi, V.; Hennequin, M. Factors affecting dental fear in French children aged 5–12 years. Int. J. Paediatr. Dent. 2010, 20, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Olak, J.; Saag, M.; Honkala, S.; Nõmmela, R.; Runnel, R.; Honkala, E.; Karjalainen, S. Children’s dental fear in relation to dental health and parental dental fear. Stomatologija 2013, 15, 26–31. [Google Scholar]
- Panda, S.; Quadri, M.; Hadi, I.; Jably, R.; Hamzi, A.; Jafer, M. Does Dental Fear in Children Predict Untreated Dental Caries? An Analytical Cross-Sectional Study. Children 2021, 8, 382. [Google Scholar] [CrossRef] [PubMed]
- Raadal, M.; Strand, G.V.; Amarante, E.C.; Kvale, G. Relationship between caries prevalence at 5 years of age and dental anxiety at 10. Eur. J. Paediatr. Dent. 2002, 3, 22–26. [Google Scholar] [PubMed]
- Da Silveira, E.R.; Goettems, M.L.; Demarco, F.F.; Azevedo, M.S. Clinical and Individual Variables in Children’s Dental Fear: A School-Based Investigation. Braz. Dent. J. 2017, 28, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Soares, F.C.; Lima, R.; de Barros, M.V.G.; Dahllöf, G.; Colares, V. Development of dental anxiety in schoolchildren: A 2-year prospective study. Community Dent. Oral Epidemiol. 2017, 45, 281–288. [Google Scholar] [CrossRef]
- Soares, F.C.; Lima, R.A.; Salvador, D.M.; de Barros, M.V.G.; Dahllöf, G.; Colares, V. Reciprocal longitudinal relationship between dental fear and oral health in schoolchildren. Int. J. Paediatr. Dent. 2019, 30, 286–292. [Google Scholar] [CrossRef]
- Torriani, D.D.; Ferro, R.L.; Bonow, M.L.M.; Santos, I.S.; Matijasevich, A.; Barros, A.J.; Demarco, F.F.; Peres, K.G. Dental Caries Is Associated with Dental Fear in Childhood: Findings from a Birth Cohort Study. Caries Res. 2014, 48, 263–270. [Google Scholar] [CrossRef]
- Wang, X.; Bernabe, E.; Pitts, N.; Zheng, S.; Gallagher, J.E. Dental caries thresholds among adolescents in England, Wales, and Northern Ireland, 2013 at 12, and 15 years: Implications for epidemiology and clinical care. BMC Oral Health 2021, 21, 137. [Google Scholar] [CrossRef] [PubMed]
- DeDonno, M. Dental anxiety, dental visits and oral hygiene practices. Oral Health Prev. Dent. 2012, 10, 129–133. [Google Scholar] [PubMed]
- Locker, D.; Liddell, A. Clinical correlates of dental anxiety among older adults. Community Dent. Oral Epidemiol. 1992, 20, 372–375. [Google Scholar] [CrossRef] [PubMed]
- Armfield, J.M. What goes around comes around: Revisiting the hypothesized vicious cycle of dental fear and avoidance. Community Dent. Oral Epidemiol. 2012, 41, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Armfield, J.M.; Stewart, J.F.; Spencer, A.J. The vicious cycle of dental fear: Exploring the interplay between oral health, service utilization and dental fear. BMC Oral Health 2007, 7, 1. [Google Scholar] [CrossRef] [Green Version]
- Armfield, J.M.; Slade, G.D.; Spencer, A.J. Dental fear and adult oral health in Australia. Community Dent. Oral Epidemiol. 2009, 37, 220–230. [Google Scholar] [CrossRef]
- Eitner, S.; Wichmann, M.; Paulsen, A.; Holst, S. Dental anxiety—An epidemiological study on its clinical correlation and effects on oral health. J. Oral Rehabil. 2006, 33, 588–593. [Google Scholar] [CrossRef]
- Heyman, R.E.; Slep, A.M.S.; White-Ajmani, M.; Bulling, L.; Zickgraf, H.F.; Franklin, M.E.; Wolff, M.S. Dental Fear and Avoidance in Treatment Seekers at a Large, Urban Dental Clinic. Oral Health Prev. Dent. 2016, 14, 315–320. [Google Scholar] [CrossRef]
- Julihn, A.; Agholme, M.B.; Grindefjord, M.; Modéer, T. Risk factors and risk indicators associated with high caries experience in Swedish 19-year-olds. Acta Odontol. Scand. 2006, 64, 267–273. [Google Scholar] [CrossRef]
- Kanaffa-Kilijanska, U.; Kaczmarek, U.; Kilijańska, B.; Frydecka, D. Oral health condition and hygiene habits among adult patients with respect to their level of dental anxiety. Oral. Health Prev. Dent. 2014, 12, 233–239. [Google Scholar] [CrossRef]
- Mehrstedt, M.; Tönnies, S.; Eisentraut, I. Dental fears, health status, and quality of life. Anesth. Prog. 2004, 51, 90–94. [Google Scholar] [PubMed]
- Meng, X.; Heft, M.W.; Bradley, M.M.; Lang, P.J. Effect of fear on dental utilization behaviors and oral health outcome. Community Dent. Oral Epidemiol. 2007, 35, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.; Vale, M.P.; Bendo, C.; Paiva, S.M.; Serra-Negra, J.M. Influence of negative dental experiences in childhood on the development of dental fear in adulthood: A case-control study. J. Oral Rehabil. 2017, 15, 100–441. [Google Scholar] [CrossRef] [PubMed]
- Pohjola, V.; Lahti, S.; Vehkalahti, M.M.; Tolvanen, M.; Hausen, H. Association between dental fear and dental attendance among adults in Finland. Acta Odontol. Scand. 2007, 65, 224–230. [Google Scholar] [CrossRef]
- Schuller, A.A.; Willumsen, T.; Holst, D. Are there differences in oral health and oral health behavior between individuals with high and low dental fear? Community Dent. Oral Epidemiol. 2003, 31, 116–121. [Google Scholar] [CrossRef]
- Samorodnitzky, G.R.; Levin, L. Self-assessed dental status, oral behavior, DMF, and dental anxiety. J. Dent. Educ. 2005, 69, 1385–1389. [Google Scholar] [CrossRef]
- Silveira, E.R.; Cademartori, M.G.; Schuch, H.S.; Corrêa, M.B.; Ardenghi, T.M.; Armfield, J.; Horta, B.L.; Demarco, F.F. The vicious cycle of dental fear at age 31 in a birth cohort in Southern Brazil. Community Dent. Oral Epidemiol. 2021, 49, 354–361. [Google Scholar] [CrossRef]
- Sullivan, M.J.L.; Neish, N.R. Catastrophizing, anxiety and pain during dental hygiene treatment. Community Dent. Oral Epidemiol. 1998, 26, 344–349. [Google Scholar] [CrossRef]
- Stouthard, M.E.A.; Hoogstraten, J. Prevalence of dental anxiety in the Netherlands. Community Dent. Oral Epidemiol. 1990, 18, 139–142. [Google Scholar] [CrossRef]
- Syed, S.; Bilal, S.; Dawani, N.; Rizvi, K. Dental anxiety among adult patients and its correlation with self-assessed dental status and treatment needs. J. Pak. Med Assoc. 2013, 63, 614–618. [Google Scholar]
- Yildirim, T.T. Evaluating the Relationship of Dental Fear with Dental Health Status and Awareness. J. Clin. Diagn. Res. 2016, 10, ZC105–ZC109. [Google Scholar] [CrossRef] [PubMed]
- Abanto, J.; Vidigal, E.A.; Carvalho, T.S.; de Sá, S.N.C.; Bönecker, M. Factors for determining dental anxiety in preschool children with severe dental caries. Braz. Oral Res. 2017, 31, e13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buldur, B.; Güvendi, O.N. Conceptual modelling of the factors affecting oral health-related quality of life in children: A path analysis. Int. J. Paediatr. Dent. 2020, 30, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Amorim Júnior, L.A.; Rodrigues, V.B.M.; Costa, L.R.; Corrêa-Faria, P. Is dental anxiety associated with the behavior of sedated children? Braz. Oral Res. 2021, 35, 1–8. [Google Scholar] [CrossRef]
- Boka, V.; Arapostathis, K.; Karagiannis, V.; Kostanos, N.; van Loveren, C.; Veerkamp, J. Dental fear and caries in 6-12 year old children in Greece. Determination of dental fear cut-off points. Eur. J. Paediatr. Dent. 2017, 18, 45–50. [Google Scholar] [CrossRef]
- Laureano, I.C.C.; Farias, L.; Fernandes, L.H.F.; de Alencar, C.R.B.; Forte, F.D.S.; Honório, D.R.; Cavalcanti, A.L. Dental Fear in Children: Association with Dental Caries and Molar Incisor Hypomineralization. Braz. Dent. J. 2020, 31, 673–679. [Google Scholar] [CrossRef]
- Nermo, H.; Willumsen, T.; Johnsen, J.-A.K. Prevalence of dental anxiety and associations with oral health, psychological distress, avoidance and anticipated pain in adolescence: A cross-sectional study based on the Tromsø study, Fit Futures. Acta Odontol. Scand. 2019, 77, 126–134. [Google Scholar] [CrossRef]
- Taani, D.Q.; El-Qaderi, S.S.; Abu Alhaija, E.S.J. Dental anxiety in children and its relationship to dental caries and gingival condition. Int. J. Dent. Hyg. 2005, 3, 83–87. [Google Scholar] [CrossRef]
- Vignehsa, H.; Chellappah, N.K.; Milgrom, P.; Going, R.; Teo, C.S. A clinical evaluation of high- and low-fear children in Singa-pore. ASDC J. Dent. Child. 1990, 57, 224–228. [Google Scholar]
- Wong, H.M.; Peng, S.; Perfecto, A.; McGrath, C.P.J. Dental anxiety and caries experience from late childhood through adolescence to early adulthood. Community Dent. Oral Epidemiol. 2020, 48, 513–521. [Google Scholar] [CrossRef]
- Folayan, M.O.; El Tantawi, M.; Oginni, A.; Adeniyi, A.; Alade, M.; Finlayson, T.L. Psychosocial, education, economic factors, decision-making ability, and caries status of mothers of children younger than 6 years in suburban Nigeria. BMC Oral Health 2020, 20, 131. [Google Scholar] [CrossRef] [PubMed]
- Pohjola, V.; Nurkkala, M.; Virtanen, J.I. Psychological distress, oral health behaviour and related factors among adolescents: Finnish School Health Promotion Study. BMC Oral Health 2021, 21, 6. [Google Scholar] [CrossRef] [PubMed]
- Veeraboina, N.; Doshi, D.; Kulkarni, S.; Patanapu, S.K.; Dantala, S.N.; Adepu, S. Association of state and trait anxiety with oral health status among adult dental patients. Acta Bio Med. 2020, 91, e2020070. [Google Scholar] [CrossRef]
- Carrillo-Diaz, M.; Crego, A.; Armfield, J.M.; Romero-Maroto, M. Treatment experience, frequency of dental visits, and children’s dental fear: A cognitive approach. Eur. J. Oral Sci. 2012, 120, 75–81. [Google Scholar] [CrossRef]
- Milgrom, P.; Vignehsa, H.; Weinstein, P. Adolescent dental fear and control: Prevalence and theoretical implications. Behav. Res. Ther. 1992, 30, 367–373. [Google Scholar] [CrossRef]
- Paryab, M.; Hosseinbor, M. Dental anxiety and behavioral problems: A study of prevalence and related factors among a group of Iranian children aged 6-12. J. Indian Soc. Pedod. Prev. Dent. 2013, 31, 82–86. [Google Scholar] [CrossRef]
- Tickle, M.; Jones, C.; Buchannan, K.; Milsom, K.M.; Blinkhorn, A.S.; Humphris, G.M. A prospective study of dental anxiety in a cohort of children followed from 5 to 9 years of age. Int. J. Paediatr. Dent. 2009, 19, 225–232. [Google Scholar] [CrossRef]
- Wogelius, P.; Poulsen, S. Associations between dental anxiety, dental treatment due to toothache, and missed dental appointments among six to eight-year-old Danish children: A cross-sectional study. Acta Odontol. Scand. 2005, 63, 179–182. [Google Scholar] [CrossRef]
- Abrahamsson, K.H.; Berggren, U.; Hakeberg, M.; Carlsson, S.G. Phobic dental avoidance and regular dental care in fearful dental patients: A comparative study. Acta Odontol. Scand. 2001, 59, 273–279. [Google Scholar] [CrossRef]
- Chanpong, B.; Haas, D.A.; Locker, D. Need and Demand for Sedation or General Anesthesia in Dentistry: A National Survey of the Canadian Population. Anesth. Prog. 2005, 52, 3–11. [Google Scholar] [CrossRef] [Green Version]
- Domoto, P.; Weinstein, P.; Kamo, Y.; Wohlers, K.; Fiset, L.; Tanaka, A. Dental fear of Japanese residents in the United States. Anesth. Prog. 1991, 38, 90–95. [Google Scholar] [PubMed]
- Erten, H.; Akarslan, Z.Z.; Bodrumlu, E. Dental fear and anxiety levels of patients attending a dental clinic. Quintessence Int. 2006, 37, 304–310. [Google Scholar]
- Goettems, M.L.; Schuch, H.S.; Demarco, F.F.; Ardenghi, T.M.; Torriani, D.D. Impact of dental anxiety and fear on dental care use in Brazilian women. J. Public Health Dent. 2014, 74, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Kurki, P.; Korhonen, M.; Honkalampi, K.; Suominen, A.L. Patients’ multifaceted views of dental fear in a diagnostic interview. Acta Odontol. Scand. 2021, 79, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Liinavuori, A.; Tolvanen, M.; Pohjola, V.; Lahti, S. Longitudinal interrelationships between dental fear and dental attendance among adult Finns in 2000–2011. Community Dent. Oral Epidemiol. 2019, 47, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Milgrom, P.; Coldwell, S.E.; Getz, T.; Weinstein, P.; Ramsay, D.S. Four Dimensions of Fear of Dental Injections. J. Am. Dent. Assoc. 1997, 128, 756–762. [Google Scholar] [CrossRef] [PubMed]
- Moore, R.; Brodsgaard, I.; Mato, T.K.; Kwan, H.W.; Shiau, Y.Y.; Knudsen, R. Fear of injections and report of negative dentist behav-ior among Caucasian American and Taiwanese adults from dental school clinics. Community Dent. Oral. Epidemiol. 1996, 24, 292–295. [Google Scholar] [CrossRef] [PubMed]
- Schneider, A.; Andrade, J.; Tanja-Dijkstra, K.; White, M.; Moles, D.R. The psychological cycle behind dental appointment attendance: A cross-sectional study of experiences, anticipations, and behavioral intentions. Community Dent. Oral Epidemiol. 2016, 44, 364–370. [Google Scholar] [CrossRef] [Green Version]
- Singh, K.A.; Brennan, D.S. Use of dental services among middle-aged adults: Predisposing, enabling and need variables. Aust. Dent. J. 2021, 66, 270–277. [Google Scholar] [CrossRef]
- Sohn, W.; Ismail, A.I. Regular dental visits and dental anxiety in an adult dentate population. J. Am. Dent. Assoc. 2005, 136, 58–66. [Google Scholar] [CrossRef]
- Teo, C.S.; Foong, W.; Lui, H.H.; Vignehsa, H.; Elliott, J.; Milgrom, P. Prevalence of dental fear in young adult Singaporeans. Int. Dent. J. 1990, 40, 37–42. [Google Scholar] [PubMed]
- Yu, J.; Jiang, R.; Nie, E.-M.; Zhang, C.-Y.; Li, X. The Prevalence of Dental Anxiety Associated with Pain among Chinese Adult Patients in Guangzhou. Pain Res. Manag. 2021, 2021, 7992580. [Google Scholar] [CrossRef] [PubMed]
- Levin, L.; Eli, L.; Ashkenazi, M. Dental Anxiety among Young Israeli Male Adults as Related to Treatment Received during Childhood. J. Public Health Dent. 2006, 66, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Nelson, C.I.; Wright, C.D.; Brumbaugh, J.T.; Neiswanger, K.; Crout, R.J.; Lilly, C.L.; Marazita, M.L.; McNeil, D.W. Predictors of use of dental care by children in north-central Appalachia in the USA. PLoS ONE 2021, 16, e0250488. [Google Scholar] [CrossRef] [PubMed]
- Nair, M.A.; Shankarapillai, R.; Chouhan, V. The dental anxiety levels associated with surgical extraction of tooth. Int. J. Dent. Clin. 2009, 1, 20–23. [Google Scholar]
- Arnrup, K.; Broberg, A.G.; Berggren, U.; Bodin, L. Lack of cooperation in pediatric dentistry--the role of child personality characteristics. Pediatr. Dent. 2002, 24, 119–128. [Google Scholar]
- Gustafsson, A.; Arnrup, K.; Broberg, A.G.; Bodin, L.; Berggren, U. Child dental fear as measured with the Dental Subscale of the Children’s Fear Survey Schedule: The impact of referral status and type of informant (child versus parent). Community Dent. Oral Epidemiol. 2010, 38, 256–266. [Google Scholar] [CrossRef]
- Klingberg, G.; Lofqvist, L.V.; Bjarnason, S.; Noren, J.G. Dental behavior management problems in Swedish children. Community Dent. Oral Epidemiol. 1994, 22, 201–205. [Google Scholar] [CrossRef]
- Soares, J.P.; Cardoso, M.; Bolan, M. Demystifying behaviour and dental anxiety in schoolchildren during endodontic treatment for primary teeth—controlled clinical trial. Int. J. Paediatr. Dent. 2019, 29, 249–256. [Google Scholar] [CrossRef]
- Ten Berge, M.; Veerkamp, J.S.J.; Hoogstraten, J.; Prins, P.J.M. The dental subscale of the children’s fear survey schedule: Predictive value and clinical usefulness. J. Psychopath. Behav. Assess. 2002, 24, 115–118. [Google Scholar] [CrossRef]
- AlGharebi, S.; Al Halabi, M.; Kowash, M.; Khamis, A.H.; Hussein, I. Children’s dental anxiety (self and proxy reported) and its association with dental behaviour in a postgraduate dental hospital. Eur. Arch. Paediatr. Dent. 2021, 22, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Alshoraim, M.A.; El-Housseiny, A.A.; Farsi, N.M.; Felemban, O.M.; AlAmoudi, N.M.; Alandejani, A.A. Effects of child characteristics and dental history on dental fear: Cross-sectional study. BMC Oral Health 2018, 18, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aminabadi, N.A.; Adhami, Z.E.; Oskouei, S.G.; Najafpour, E.; Jamali, Z. Emotional Intelligence Subscales: Are They Correlated with Child Anxiety and Behavior in the Dental Setting? J. Clin. Pediatr. Dent. 2013, 38, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Buldur, B. Pathways between parental and individual determinants of dental caries and dental visit behaviours among children: Validation of a new conceptual model. Community Dent. Oral Epidemiol. 2020, 48, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.; Lu, J.; Li, P.; Yu, D.; Zhao, W. Prevalence and risk factors of children’s dental anxiety in China: A longitudinal study. BMJ Open 2021, 11, e043647. [Google Scholar] [CrossRef] [PubMed]
- Klaassen, M.; Veerkamp, J.; Hoogstraten, J. Predicting dental anxiety. The clinical value of anxiety questionnaires: An explora-tory study. Eur. J. Paediatr. Dent. 2003, 4, 171–176. [Google Scholar]
- Milgrom, P.; Jie, Z.; Yang, Z.; Tay, K.M. Cross-cultural validity of a parent’s version of the Dental Fear Survey Schedule for chil-dren in Chinese. Behav. Res. Ther. 1993, 32, 131–135. [Google Scholar] [CrossRef]
- Nakai, Y.; Hirakawa, T.; Milgrom, P.; Coolidge, T.; Heima, M.; Mori, Y.; Ishihara, C.; Yakushiji, N.; Yoshida, T.; Shimono, T. The Children’s Fear Survey Schedule-Dental Subscale in Japan. Community Dent. Oral Epidemiol. 2005, 33, 196–204. [Google Scholar] [CrossRef]
- Ramos-Jorge, M.L.; Marques, L.S.; Pavia, S.M.; Serra-Negra, J.M.; Pordeus, I. Predictive factors for child behaviour in the dental environment. Eur. Arch. Paediatr. Dent. 2006, 7, 253–257. [Google Scholar] [CrossRef]
- Versloot, J.; Veerkamp, J.S.J.; Hoogstraten, J. Dental anxiety and psychological functioning in children: Its relationship with behaviour during treatment. Eur. Arch. Paediatr. Dent. 2008, 9, 36–40. [Google Scholar] [CrossRef]
- Wogelius, P.; Poulsen, S.; Sørensen, H.T. Prevalence of dental anxiety and behavior management problems among six to eight years old Danish children. Acta Odontol. Scand. 2003, 61, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Cademartori, M.G.; Costa, V.P.P.; Corrêa, M.B.; Goettems, M.L. The influence of clinical and psychosocial characteristics on children behaviour during sequential dental visits: A longitudinal prospective assessment. Eur. Arch. Paediatr. Dent. 2020, 21, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Ihara, Y.; Fukuda, K.-I.; Saita, N.; Ichinohe, T. Male Gender and High Trait Anxiety Are 2 Major Factors Associated With Severe Dental Fear and Avoidance. Anesth. Prog. 2018, 65, 177–180. [Google Scholar] [CrossRef] [PubMed]
- Stein Duker, L.I.; Pham, P.K.; Polido, J.C.; Cermak, S.A. Oral care and sensory over-responsivity in typically developing children. Pediatr. Dent. 2022. under review. [Google Scholar]
- MacCormac, C.; Kinirons, M. Reasons for referral of children to a general anaesthetic service in Northern Ireland. Int. J. Paediatr. Dent. 1998, 8, 191–196. [Google Scholar] [CrossRef]
- Rajavaara, P.; Rankinen, S.; Laitala, M.-L.; Vähänikkilä, H.; Yli-Urpo, H.; Koskinen, S.; Anttonen, V. The influence of general health on the need for dental general anaesthesia in children. Eur. Arch. Paediatr. Dent. 2017, 18, 179–185. [Google Scholar] [CrossRef]
- Savanheimo, N.; Vehkalahti, M.M.; Pihakari, A.; Numminen, M. Reasons for and parental satisfaction with children’s dental care under general anaesthesia. Int. J. Paediatr. Dent. 2005, 15, 448–454. [Google Scholar] [CrossRef]
- Taskinen, H.; Kankaala, T.; Rajavaara, P.; Pesonen, P.; Laitala, M.-L.; Anttonen, V. Self-reported causes for referral to dental treatment under general anaesthesia (DGA): A cross-sectional survey. Eur. Arch. Paediatr. Dent. 2014, 15, 105–112. [Google Scholar] [CrossRef]
- Kopczynski, K.; Meyer, B.D. Examining Parental Treatment Decisions within a Contemporary Pediatric Dentistry Private Practice. Patient Prefer. Adherence 2021, 15, 645–652. [Google Scholar] [CrossRef]
- MacPherson, L.M.D.; Pine, C.; Tochel, C.; Burnside, G.; Hosey, M.T.; Adair, P. Factors influencing referral of children for dental extractions under general and local anaesthesia. Community Dent Health 2005, 22, 282–288. [Google Scholar]
- Ramdaw, A.; Hosey, M.T.; Bernabe, E. Factors associated with use of general anaesthesia for dental procedures among British children. Br. Dent. J. 2017, 223, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Boyle, C.A.; Newton, J.T.; Milgrom, P. Who is referred for sedation for dentistry and why? Br. Dent. J. 2009, 206, E12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coolidge, T.; Irwin, S.P.; Leyster, K.A.; Milgrom, P. Determinants of receiving intravenous sedation in a sample of dentally-fearful patients in the USA. SAAD Dig. 2012, 28, 52–60. [Google Scholar] [PubMed]
- Sirin, Y.; Yildirimturk, S.; Ay, N. Do state-trait anxiety and previous unpleasant dental experiences predict the need for sedation in women having third molar surgery? Br. J. Oral Maxillofac. Surg. 2020, 58, 530–534. [Google Scholar] [CrossRef] [PubMed]
- Tickle, M.; Williams, M.; Jenner, T.; Blinkhorn, A. The effects of socioeconomic status and dental attendance on dental caries’ experience, and treatment patterns in 5-year-old children. Br. Dent. J. 1999, 186, 135–137. [Google Scholar] [CrossRef]
- Menegazzo, G.R.; Knorst, J.K.; Emmanuelli, B.; Mendes, F.M.; Ardenghi, D.M.; Ardenghi, T.M. Effect of routine dental attendance on child oral health-related quality of life: A cohort study. Int. J. Paediatr. Dent. 2019, 30, 459–467. [Google Scholar] [CrossRef]
- Aldossary, A.; Harrison, V.E.; Bernabé, E. Long-term patterns of dental attendance and caries experience among British adults: A retrospective analysis. Eur. J. Oral Sci. 2015, 123, 39–45. [Google Scholar] [CrossRef]
- Hagman, J.; Wide, U.; Werner, H.; Hakeberg, M. Oral health and oral health behavior in young adults with caries disease. BDJ Open 2021, 7, 1–6. [Google Scholar] [CrossRef]
- Crocombe, L.A.; Brennan, D.S.; Slade, G.D. The influence of dental attendance on change in oral health-related quality of life. Community Dent. Oral Epidemiol. 2012, 40, 53–61. [Google Scholar] [CrossRef]
- Kvist, T.; Zedrén-Sunemo, J.; Graca, E.; Dahllöf, G. Is treatment under general anaesthesia associated with dental neglect and dental disability among caries active preschool children? Eur. Arch. Paediatr. Dent. 2014, 15, 327–332. [Google Scholar] [CrossRef]
- Lee, H.; Faundez, L.; Yarbrough, C.; Lewis, C.; LoSasso, A. Patterns in Pediatric Dental Surgery under General Anesthesia across 7 State Medicaid Programs. JDR Clin. Transl. Res. 2020, 5, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Vinckier, F.; Gizani, S.; Declerck, D. Comprehensive dental care for children with rampant caries under general anaesthesia. Int. J. Paediatr. Dent. 2001, 11, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Arnrup, K.; Broberg, A.G.; Berggren, U.; Bodin, L. Treatment outcome in subgroups of uncooperative child dental patients: An exploratory study. Int. J. Paediatr. Dent. 2003, 13, 304–319. [Google Scholar] [CrossRef] [PubMed]
- Williamson, R.; Oueis, H.; Casamassimo, P.S.; Thikkurissy, S. Association between early childhood caries and behavior as meas-ured by the child behavior checklist. Pediatr. Dent. 2008, 30, 505–509. [Google Scholar]
- Sullivan, M.J.; Neish, N.R. Psychological predictors of pain during dental hygiene treatment. Probe 1997, 31, 123–126. [Google Scholar]
- Engel-Yeger, B.; Dunn, W. Relationship between Pain Catastrophizing Level and Sensory Processing Patterns in Typical Adults. Am. J. Occup. Ther. 2011, 65, e1–e10. [Google Scholar] [CrossRef] [Green Version]
- Meredith, P.J.; Rappel, G.; Strong, J.; Bailey, K.J. Sensory Sensitivity and Strategies for Coping with Pain. Am. J. Occup. Ther. 2015, 69, 6904240010. [Google Scholar] [CrossRef] [Green Version]
- Granot, M.; Ferber, S.G. The Roles of Pain Catastrophizing and Anxiety in the Prediction of Postoperative Pain Intensity: A prospective study. Clin. J. Pain 2005, 21, 439–445. [Google Scholar] [CrossRef]
- De Jongh, A.; Muris, P.; Ter Horst, G.; Van Zuuren, F.; De Wit, C. Cognitive Correlates of Dental Anxiety. J. Dent. Res. 1994, 73, 561–566. [Google Scholar] [CrossRef]
- Brown, J.; Brown, J.; Woodburn, J. Dental services for children with autism spectrum disorder. Learn Disabil. Pract. 2014, 17, 20–25. [Google Scholar] [CrossRef]
- Dunn, W.; Little, L.; Dean, E.; Robertson, S.; Evans, B. The State of the Science on Sensory Factors and Their Impact on Daily Life for Children: A scoping review. OTJR: Occup. Particip. Health 2016, 36, S3–S26. [Google Scholar] [CrossRef]
- Green, D.; Flanagan, D. Understanding the autistic dental patient. Gen. Dent. 2008, 56, 167–171. [Google Scholar] [PubMed]
- Khrautieo, T.; Srimaneekarn, N.; Rirattanapong, P.; Smutkeeree, A. Association of sensory sensitivities and toothbrushing cooperation in autism spectrum disorder. Int. J. Paediatr. Dent. 2020, 30, 505–513. [Google Scholar] [CrossRef]
- Kuhaneck, H.M.; Chisholm, E.C. Improving dental visits for individuals with autism spectrum disorders through an understanding of sensory processing. Spéc. Care Dent. 2012, 32, 229–233. [Google Scholar] [CrossRef] [PubMed]
- Stein, L.I.; Polido, J.C.; Mailloux, Z.; Coleman, G.G.; Cermak, S.A. Oral care and sensory sensitivities in children with autism spectrum disorders. Spéc. Care Dent. 2011, 31, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Stein Duker, L.I.; Henwood, B.F.; Bluthenthal, R.N.; Juhlin, E.; Polido, J.C.; Cermak, S.A. Parents’ perceptions of dental care challenges in male children with autism spectrum disorder: An initial qualitative exploration. Res. Autism Spectr. Disord. 2017, 39, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Stein Duker, L.I.; Floríndez, L.I.; Como, D.H.; Tran, C.F.; Henwood, B.F.; Polido, J.C.; Cermak, S.A. Strategies for success: A qualitative study of caregiver and dentist approaches to improving oral care for children with autism. Pediatr. Dent. 2019, 41, E4–E12. [Google Scholar]
- Stein Duker, L.I. Adapting oral care protocols to support children with sensory sensitivities: Occupational therapy and dentis-try. In Dental Care for Children with Special Needs: A Clinical Guide; Nelson, T.M., Webb, J.R., Eds.; Springer: Cham, Switzerland, 2019; pp. 77–98. [Google Scholar]
- Thomas, N.; Blake, S.; Morris, C.; Moles, D.R. Autism and primary care dentistry: Parents’ experiences of taking children with autism or working diagnosis of autism for dental examinations. Int. J. Paediatr. Dent. 2017, 28, 226–238. [Google Scholar] [CrossRef]
- Stein Duker, L.I.; Richter, M.; Lane, C.J.; Polido, J.C.; Cermak, S.A. Oral care experiences and challenges for children with Down syndrome: Reports from caregivers. Pediatr. Dent. 2020, 42, 430–435. [Google Scholar]
- Stein Duker, L.I.; Martinez, M.; Lane, C.J.; Polido, J.C.; Cermak, S.A. Association between oral care challenges and sensory over-responsivity in children with Down syndrome. Int. J. Paediatr. Dent. 2021, 1–12. [Google Scholar] [CrossRef]
- Ghanizadeh, A. Parents reported oral sensory sensitivity processing and food preference in ADHD. J. Psychiatr. Ment. Health Nurs. 2013, 20, 426–432. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Dental and Craniofacial Research. Practical Oral Care for People with Autism. NIH Publication No. 09-5190. 2019. Available online: https://www.nidcr.nih.gov/sites/default/files/2017-09/practical-oral-care-autism.pdf (accessed on 1 November 2021).
- Bradt, J.; Teague, A. Music interventions for dental anxiety. Oral Dis. 2018, 24, 300–306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goettems, M.L.; Zborowski, E.J.; Costa, F.D.S.; Costa, V.P.P.; Torriani, D.D. Nonpharmacologic Intervention on the Prevention of Pain and Anxiety During Pediatric Dental Care: A Systematic Review. Acad. Pediatr. 2017, 17, 110–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prado, I.M.; Carcavalli, L.; Abreu, L.G.; Serra-Negra, J.M.; Paiva, S.M.; Martins, C.C. Use of distraction techniques for the management of anxiety and fear in paediatric dental practice: A systematic review of randomized controlled trials. Int. J. Paediatr. Dent. 2019, 29, 650–668. [Google Scholar] [CrossRef] [PubMed]
- Weisfeld, C.C.; Turner, J.A.; Dunleavy, K.; Ko, A.; Bowen, J.I.; Roelk, B.; Eissa, R.; Benfield, E.; Robertson, K. Dealing with Anxious Patients: A Systematic Review of the Literature on Nonpharmaceutical Interventions to Reduce Anxiety in Patients Undergoing Medical or Dental Procedures. J. Altern. Complement. Med. 2021, 27, 717–726. [Google Scholar] [CrossRef]
- Aditya, P.; Prasad, M.G.; Nagaradhakrishna, A.; Raju, N.S.; Babu, D.N. Comparison of effectiveness of three distraction techniques to allay dental anxiety during inferior alveolar nerve block in children: A randomized controlled clinical trial. Heliyon 2021, 7, e08092. [Google Scholar] [CrossRef]
- Asokan, S.; Priya, P.G.; Natchiyar, S.N.; Elamathe, M. Effectiveness of distraction techniques in the management of anxious chil-dren—A randomized controlled pilot trial. J. Indian Soc. Pedod. Prev. Dent. 2020, 38, 407–412. [Google Scholar] [CrossRef]
- Azher, U.; Srinath, S.K.; Nayak, M. Effectiveness of Bubble Breath Play Therapy in the Dental Management of Anxious Children: A Pilot Study. J. Contemp. Dent. Pract. 2020, 21, 17–21. [Google Scholar] [CrossRef]
- Kharouba, J.; Peretz, B.; Blumer, S. The effect of television distraction versus Tell-Show-Do as behavioral management techniques in children undergoing dental treatments. Quintessence Int. 2020, 51, 486–494. [Google Scholar]
- Pande, P.; Rana, V.; Srivastava, N.; Kaushik, N. Effectiveness of different behavior guidance techniques in managing children with negative behavior in a dental setting: A randomized control study. J. Indian Soc. Pedod. Prev. Dent. 2020, 38, 259–265. [Google Scholar] [CrossRef]
- Garrocho-Rangel, A.; Ibarra-Gutiérrez, E.; Rosales-Bérber, M.; Esquivel-Hernández, R.; Esparza-Villalpando, V.; Pozos-Guillén, A. A video eyeglasses/earphones system as distracting method during dental treatment in children: A crossover randomised and controlled clinical trial. Eur. J. Paediatr. Dent. 2018, 19, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Jimeno, F.G.; Bellido, M.M.; Fernández, C.C.; Rodríguez, A.I.L.; Pérez, J.L.; Quesada, J.R.B. Effect of audiovisual distraction on children’s behaviour, anxiety and pain in the dental setting. Eur. J. Paediatr. Dent. 2015, 15, 297–302. [Google Scholar]
- Marwah, N.; Prabhakar, A.R.; Raju, O.S. Music distraction-its efficacy in management of anxious pediatric dental patients. J. Indian Soc. Pedod. Prev. Dent. 2005, 23, 168–170. [Google Scholar] [CrossRef] [PubMed]
- Torres-Gomez, J.; Arnason, S.; Hoopes, W.; Vandewalle, K. Management of dental anxiety via distraction technique. J. Clin. Exp. Dent. 2021, 13, e350–e356. [Google Scholar] [CrossRef]
- Alnamankany, A. Video modelling and dental anxiety in children. A randomised clinical trial. Eur. J. Paediatr. Dent. 2019, 20, 242–246. [Google Scholar] [CrossRef]
- Elangovan, A.; Mungara, J.; Injeti, M.; Joseph, E.; Sakthivel, R.; Selvaraju, G. Child’s dental fear: Cause related factors and the influence of audiovisual modeling. J. Indian Soc. Pedod. Prev. Dent. 2013, 31, 215. [Google Scholar] [CrossRef]
- Sakthivel, R.; Poornima, V.; Jayanthi, M.; Nilaya Reddy, V.; Selvaraju, G.; Sakthivel, M.R. Evaluation of anxiety and the effect of modeling in children undergoing orthopantomographic examination. J. Indian Acad. Oral. Med. Radiol. 2013, 25, 274–277. [Google Scholar]
- Karekar, P.; Bijle, M.N.; Walimbe, H. Effect of Three Behavior Guidance Techniques on Anxiety Indicators of Children Undergoing Diagnosis and Preventive Dental Care. J. Clin. Pediatr. Dent. 2019, 43, 167–172. [Google Scholar] [CrossRef]
- Howard, K.E.; Freeman, R. An evaluation of the PALS after treatment modelling intervention to reduce dental anxiety in child dental patients. Int. J. Paediatr. Dent. 2009, 19, 233–242. [Google Scholar] [CrossRef]
- Farhat-McHayleh, N.; Harfouche, A.; Souaid, P. Techniques for managing behaviour in pediatric dentistry: Comparative study of live modelling and tell-show-do based on children’s heart rates during treatment. J. Can. Dent. Assoc. 2009, 75, 283. [Google Scholar]
- Vishwakarma, A.P.; Bondarde, P.A.; Patil, S.B.; Dodamani, A.; Vishwakarma, P.Y.; Mujawar, S.A. Effectiveness of two different behavioral modification techniques among 5–7-year-old children: A randomized controlled trial. J. Indian Soc. Pedod. Prev. Dent. 2017, 35, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Gu, Z.; Wang, Y.; Wu, Q.; Chen, V.; Xu, X.; Zhou, X. Effect of audiovisual distraction on the management of dental anxiety in children: A systematic review. Int. J. Paediatr. Dent. 2018, 29, 14–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robertson, M.; Araujo, M.P.; Innes, N. Anxiety and fear management in paediatric dentistry using distraction techniques. Evid. Based Dent. 2019, 20, 50–51. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Qin, D.; Shen, L.; Ji, P.; Wang, J. Does audiovisual distraction reduce dental anxiety in children under local anesthesia? A systematic review and meta-analysis. Oral Dis. 2017, 25, 416–424. [Google Scholar] [CrossRef] [PubMed]
- Boman, U.W.; Carlsson, V.; Westin, M.; Hakeberg, M. Psychological treatment of dental anxiety among adults: A systematic review. Eur. J. Oral Sci. 2013, 121, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Coldwell, S.E.; Getz, T.; Milgrom, P.; Prall, C.W.; Spadafora, A.; Ramsay, D.S. CARL: A LabVIEW 3 computer program for conducting exposure therapy for the treatment of dental injection fear. Behav. Res. Ther. 1998, 36, 429–441. [Google Scholar] [CrossRef]
- Coldwell, S.E.; Wilhelm, F.H.; Milgrom, P.; Prall, C.W.; Getz, T.; Spadafora, A.; Chiu, I.-Y.; Leroux, B.G.; Ramsay, D.S. Combining alprazolam with systematic desensitization therapy for dental injection phobia. J. Anxiety Disord. 2007, 21, 871–887. [Google Scholar] [CrossRef]
- Hauge, M.S.; Stora, B.; Vassend, O.; Hoffart, A.; Willumsen, T. Dentist-administered cognitive behavioural therapy versus four habits/midazolam: An RCT study of dental anxiety treatment in primary dental care. Eur. J. Oral Sci. 2021, 129, e12794. [Google Scholar] [CrossRef]
- Kebriaee, F.; Shirazi, A.S.; Fani, K.; Moharreri, F.; Soltanifar, A.; Khaksar, Y.; Mazhari, F. Comparison of the effects of cognitive behavioural therapy and inhalation sedation on child dental anxiety. Eur. Arch. Paediatr. Dent. 2014, 16, 173–179. [Google Scholar] [CrossRef]
- Kvale, G.; Berggren, U.; Milgrom, P. Dental fear in adults: A meta-analysis of behavioral interventions. Community Dent. Oral Epidemiol. 2004, 32, 250–264. [Google Scholar] [CrossRef]
- Öst, L.G.; Kvale, G. Effects of cognitive behavioural treatments: A systematic review and meta-analysis. In Cognitive Behaviour Therapy for Dental Phobia and Anxiety; Öst, L.G., Skaret, E., Eds.; Wiley-Blackwell: Hoboken, NJ, USA, 2013; pp. 163–182. [Google Scholar]
- Porritt, J.; Rodd, H.; Morgan, A.; Williams, C.; Gupta, E.; Kirby, J.; Creswell, C.; Newton, T.; Stevens, K.; Baker, S.; et al. Development and Testing of a Cognitive Behavioral Therapy Resource for Children’s Dental Anxiety. JDR Clin. Transl. Res. 2017, 2, 23–37. [Google Scholar] [CrossRef]
- Shahnavaz, S.; Hedman-Lagerlöf, E.; Grindefjord, M.; Reuterskiöld, L.; Dahllöf, G. Cognitive Behavioral Therapy for Children with Dental Anxiety: A randomized controlled trial. JDR Clin. Transl. Res. 2016, 1, 234–243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shahnavaz, S.; Hedman-Lagerlöf, E.; Hasselblad, T.; Reuterskiold, L.; Kaldo, V.; Dahllöf, G. Internet-Based Cognitive Behavioral Therapy for Children and Adolescents With Dental Anxiety: Open Trial. J. Med. Internet Res. 2018, 20, e12. [Google Scholar] [CrossRef] [PubMed]
- Heyman, R.; Wojda, A.; Eddy, J.; Haydt, N.; Geiger, J.; Slep, A.S. Dentist-Perceived Barriers and Attractors to Cognitive-Behavioral Treatment Provided by Mental Health Providers in Dental Practices. Adv. Dent. Res. 2018, 29, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Hmud, R.; Walsh, L.J. Dental anxiety: Causes, complications and management approaches. J. Minim. Interv. Dent. 2009, 2, 67–78. [Google Scholar]
- Walsh, L.J. Anxiety prevention: Implementing the 4 S principle in conservative dentistry. Auxilliary 2007, 17, 24–26. [Google Scholar]
- Cai, H.; Xi, P.; Zhong, L.; Chen, J.; Liang, X. Efficacy of aromatherapy on dental anxiety: A systematic review of randomised and quasi-randomised controlled trials. Oral Dis. 2021, 27, 829–847. [Google Scholar] [CrossRef]
- Arslan, I.; Aydinoglu, S.; Karan, N.B. Can lavender oil inhalation help to overcome dental anxiety and pain in children? A randomized clinical trial. Eur. J. Pediatr. 2020, 179, 985–992. [Google Scholar] [CrossRef]
- Ghaderi, F.; Solhjou, N. The effects of lavender aromatherapy on stress and pain perception in children during dental treatment: A randomized clinical trial. Complement. Ther. Clin. Pract. 2020, 40, 101182. [Google Scholar] [CrossRef]
- Jadhav, G.R.; Mittal, P. Evaluation of aromatherapy on success rate of inferior alveolar nerve block in teeth with irreversible pulpitis: A prospective randomized clinical trial. Quintessence Int. 2020, 51, 864–870. [Google Scholar]
- Purohit, A.; Singh, A.; Purohit, B.; Shakti, P.; Shah, N. Is aromatherapy associated with patient’s dental anxiety levels? A systematic review and meta-analysis. J. Dent. Anesthesia Pain Med. 2021, 21, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.Y.; Yang, H.; Chi, H.J.; Chen, H.M. Physiological effects of deep touch pressure on anxiety alleviation: The weighted blanket approach. J. Med. Biol. Eng. 2012, 33, 463–470. [Google Scholar] [CrossRef]
- Chen, H.-Y.; Yang, H.; Meng, L.-F.; Chan, P.-Y.S.; Yang, C.-Y. Effect of deep pressure input on parasympathetic system in patients with wisdom tooth surgery. J. Formos. Med. Assoc. 2016, 115, 853–859. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, H.-Y.; Yang, H.; Chi, H.-J.; Chen, H.-M. Parasympathetic effect of deep pressure input on third molar extraction in adolescents. J. Formos. Med Assoc. 2019, 118, 1317–1324. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, M.; Melmed, R.N.; Sgan-Cohen, H.D.; Eli, I.; Parush, S. Behavioural and physiological effect of dental environment sensory adaptation on children’s dental anxiety. Eur. J. Oral Sci. 2007, 115, 479–483. [Google Scholar] [CrossRef]
- Shapiro, M.; Sgan-Cohen, H.D.; Parush, S.; Melmed, R.N. Influence of Adapted Environment on the Anxiety of Medically Treated Children with Developmental Disability. J. Pediatr. 2009, 154, 546–550. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, M.; Melmed, R.N.; Sgan-Cohen, H.D.; Parush, S. Effect of sensory adaptation on anxiety of children with developmental disabilities: A new approach. Pediatr. Dent. 2009, 31, 222–228. [Google Scholar]
- Kim, G.; Carrico, C.; Ivey, C.; Wunsch, P.B. Impact of sensory adapted dental environment on children with developmental disabilities. Spéc. Care Dent. 2019, 39, 180–187. [Google Scholar] [CrossRef]
- Potter, C.N.; Wetzel, J.L.; Learman, K.E. Effect of sensory adaptations for routine dental care in individuals with intellectual and developmental disabilities: A preliminary study. J. Intellect. Dev. Disabil. 2019, 44, 305–314. [Google Scholar] [CrossRef]
- American Academy of Pediatric Dentistry. Behavior guidance for the pediatric dental patient. In The Reference Manual of Pediatric Dentistry; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2021; pp. 306–324. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stein Duker, L.I.; Grager, M.; Giffin, W.; Hikita, N.; Polido, J.C. The Relationship between Dental Fear and Anxiety, General Anxiety/Fear, Sensory Over-Responsivity, and Oral Health Behaviors and Outcomes: A Conceptual Model. Int. J. Environ. Res. Public Health 2022, 19, 2380. https://doi.org/10.3390/ijerph19042380
Stein Duker LI, Grager M, Giffin W, Hikita N, Polido JC. The Relationship between Dental Fear and Anxiety, General Anxiety/Fear, Sensory Over-Responsivity, and Oral Health Behaviors and Outcomes: A Conceptual Model. International Journal of Environmental Research and Public Health. 2022; 19(4):2380. https://doi.org/10.3390/ijerph19042380
Chicago/Turabian StyleStein Duker, Leah I., Mollianne Grager, Willa Giffin, Natasha Hikita, and José C. Polido. 2022. "The Relationship between Dental Fear and Anxiety, General Anxiety/Fear, Sensory Over-Responsivity, and Oral Health Behaviors and Outcomes: A Conceptual Model" International Journal of Environmental Research and Public Health 19, no. 4: 2380. https://doi.org/10.3390/ijerph19042380
APA StyleStein Duker, L. I., Grager, M., Giffin, W., Hikita, N., & Polido, J. C. (2022). The Relationship between Dental Fear and Anxiety, General Anxiety/Fear, Sensory Over-Responsivity, and Oral Health Behaviors and Outcomes: A Conceptual Model. International Journal of Environmental Research and Public Health, 19(4), 2380. https://doi.org/10.3390/ijerph19042380






