Relationship between Socio-Demographic Factors and Posttraumatic Stress Disorder: A Cross Sectional Study among Civilian Participants’ Hostilities in Ukraine
Abstract
:1. Introduction
1.1. Hostilities and PTSD
1.2. Rates of PTSD
1.3. Risk Factors for PTSD
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measure
2.3. Statistical Methods
3. Results
Predictors of PTSD
4. Discussion
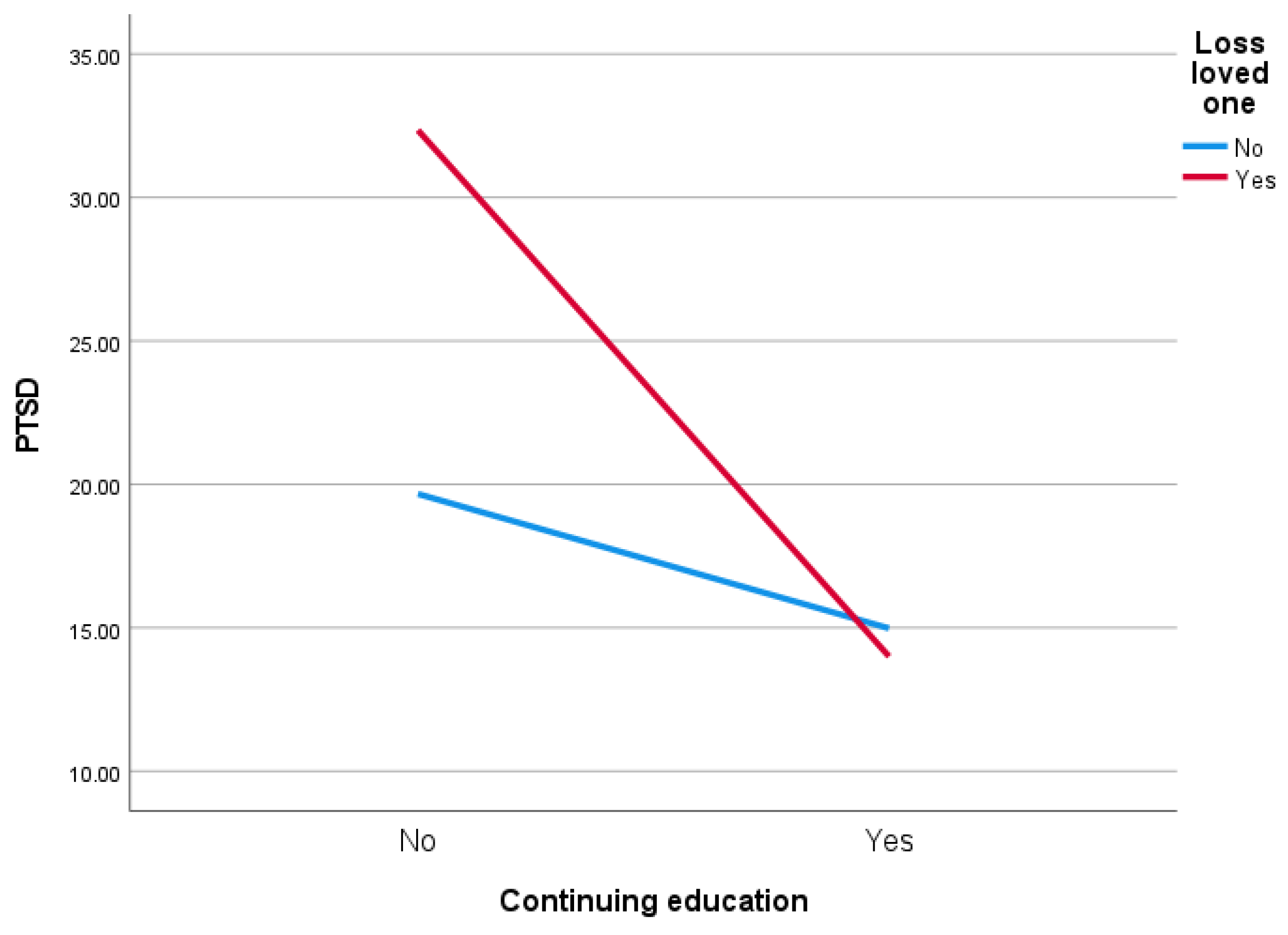
4.1. Loss of a Loved One as a Predictor of PTSD
4.2. Place of Residence as a Predictor of PTSD
4.3. Continuing Education as a Predictor of PTSD
4.4. Gender as a Predictor of PTSD
4.5. Lack of Health Insurance as a Predictor of PTSD
4.6. Implications
4.7. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hoppen, T.H.; Morina, N. The prevalence of PTSD and major depression in the global population of adult war survivors: A meta-analytically informed estimate in absolute numbers. Eur. J. Psychotraumatol. 2019, 10, 1578637. [Google Scholar] [CrossRef] [Green Version]
- Jonsson, O.; Seely, R. Russian Full-Spectrum Conflict: An Appraisal after Ukraine. J. Slav. Mil. Stud. 2015, 28, 1–22. [Google Scholar] [CrossRef]
- Kessler, R.C.; Sonnega, A.; Bromet, E.; Hughes, M.; Nelson, C.B. Posttraumatic stress disorder in the National Comorbidity Survey. Arch. Gen. Psychiatry 1995, 52, 1048–1060. [Google Scholar] [CrossRef] [PubMed]
- Ogińska-Bulik, N.; Juczyński, Z. Consequences of experienced negative life events—Posttraumatic stress disorder symptoms and posttraumatic growth. Psychiatry 2012, 9, 1–10. [Google Scholar]
- McFarlane, A.C. The Long-Term Costs of Traumatic Stress: Intertwined Physical and Psychological Consequences. World Psychiatry 2010, 9, 3–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oquendo, M.; Brent, D.A.; Birmaher, B.; Greenhill, L.; Kolko, D.; Stanley, B.; Zelazny, J.; Burke, A.K.; Firinciogullari, S.; Ellis, S.P.; et al. Posttraumatic Stress Disorder Comorbid with Major Depression: Factors Mediating the Association with Suicidal Behavior. Am. J. Psychiatry 2005, 162, 560–566. [Google Scholar] [CrossRef]
- McEwen, B.S. Central Effects of Stress Hormones in Health and Disease: Understanding the Protective and Damaging Effects of Stress and Stress Mediators. Eur. J. Pharmacol. 2008, 583, 174–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoge, W.C.; Castro, C.A.; Messer, S.C.; McGurk, D.; Cotting, D.I.; Koffman, R.L. Combat Duty in Iraq and Afghanistan, Mental Health Problems, and Barriers to Care. N. Engl. J. Med. 2004, 351, 13–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hall, B.J.; Hobfoll, S.E.; Palmieri, P.A.; Canetti-Nisim, D.; Shapira, O.; Johnson, R.J.; Galea, S. The psychological impact of impending forced settler disengagement in Gaza: Trauma and posttraumatic growth. J. Trauma. Stress 2008, 21, 22–29. [Google Scholar] [CrossRef] [Green Version]
- Ahern, J.; Galea, S.; Fernandez, W.G.; Koci, B.; Waldman, R.; Vlahov, D. Gender, social support, and posttraumatic stress in postwar Kosovo. J. Nerv. Ment. Dis. 2004, 192, 762–770. [Google Scholar] [CrossRef] [PubMed]
- Groth, J.; Waszyńska, K.; Zyszczyk, B. Czynniki ryzyka rozwoju zespołu stresu pourazowego u żołnierzy uczestniczących w misjach pokojowych. Studia Eduk. 2013, 26, 297–316. [Google Scholar]
- Bogic, M.; Njoku, A.; Priebe, S. Long-Term Mental Health of War-Refugees: A Systematic Literature Review. BMC Int. Health Hum. Right 2015, 15, 29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morina, N.; Akhtar, A.; Barth, J.; Schnyder, U. Psychiatric Disorders in Refugees and Internally Displaced Persons after Forced Displacement: A Systematic Review. Front. Psychiatry 2018, 9, 433. [Google Scholar] [CrossRef]
- Marshall, G.N.; Schell, T.L.; Elliott, M.N.; Berthold, S.M.; Chun, C.-A. Mental Health of Cambodian Refugees 2 Decades After Resettlement in the United States. JAMA 2005, 294, 571–579. [Google Scholar] [CrossRef] [Green Version]
- Jordan, B.K.; Marmar, C.R.; Fairbank, J.A.; Schlenger, W.E.; Kulka, R.A.; Hough, R.L.; Weiss, D.S. Problems in Families of Male Vietnam Veterans With Posttraumatic Stress Disorder. J. Consult. Clin. Psychol. 1992, 60, 916–926. [Google Scholar] [CrossRef]
- Riley, A.; Akther, Y.; Noor, M.; Rahmat, A.; Welton-Mitchell, C. Systematic human rights violations, traumatic events, daily stressors and mental health of Rohingya refugees in Bangladesh. Confl. Health 2020, 14, 60. [Google Scholar] [CrossRef]
- Kang, H.K.; Natelson, B.H.; Mahan, C.M.; Lee, K.Y.; Murphy, F.M. Post-Traumatic Stress Disorder and Chronic Fatigue Syndrome-like Illness among Gulf War Veterans: A Population-Based Survey of 30,000 Veterans. Am. J. Epidemiol. 2003, 157, 141–148. [Google Scholar] [CrossRef] [Green Version]
- Koren, D.; Norman, D.; Cohen, A.; Berman, J.; Klein, E.M. Increased PTSD Risk with Combat-Related Injury: A Matched Comparison Study of Injured and Uninjured Soldiers Experiencing the Same Combat Events. Am. J. Psychiatry 2005, 162, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Ford, J.D. Disorders of Extreme Stress Following War-Zone Military Trauma: Associated Features of Posttraumatic Stress Disorder or Comorbid but Distinct Syndromes? J. Consult. Clin. Psychol. 1999, 67, 3–12. [Google Scholar] [CrossRef]
- Van Ommeren, M.; de Jong, J.T.V.M.; Sharma, B.; Komproe, I.; Thapa, S.B.; Cardeña, E. Psychiatric Disorders Among Tortured Bhutanese Refugees in Nepal. Arch. Gen. Psychiatry 2011, 58, 475–482. [Google Scholar] [CrossRef] [Green Version]
- Iversen, A.C.; Fear, N.T.; Ehlers, A.; Hacker Hughes, J.; Hull, L.; Earnshaw, M.; Greenberg, N.; Rona, R.; Wessely, S.; Hotopf, M. Risk factors for post-traumatic stress disorder among UK Armed Forces personnel. Psychol. Med. 2008, 38, 511–522. [Google Scholar] [CrossRef] [Green Version]
- Reisman, M. PTSD Treatment for Veterans: What’s Working, What’s New, and What’s Next. Peer-Rev. J. Formul. Manag. 2016, 41, 623–627. [Google Scholar]
- Orth, U.; Wieland, E. Anger, Hostility, and Posttraumatic Stress Disorder in Trauma-Exposed Adults: A Meta-Analysis. J. Consult. Clin. Psychol. 2006, 74, 698–706. [Google Scholar] [CrossRef] [Green Version]
- Weathers, F.W.; Litz, B.T.; Herman, D.S.; Huska, J.; Keane, T.M. The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. In Proceedings of the Annual Meeting of International Society for Traumatic Stress Studies, San Antonio, TX, USA, 25 October 1993. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Priebe, S.; Bogic, M.; Ajdukovic, D.; Franciskovic, T.; Galeazzi, G.M.; Kucukalic, A.; Lecic-Tosevski, D.; Morina, N.; Popovski, M.; Wang, D.; et al. Mental Disorders Following War in the Balkans: A study in 5 countries. Arch. Gen. Psychiatry 2010, 67, 518–528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shahar, G.; Noyman, G.; Schnidel-Allon, I.; Gilboa-Schechtman, E. Do PTSD symptoms and trauma-related cognitions about the self constitute a vicious cycle? Evidence for both cognitive vulnerability and scarring models. Psychiatry Res. 2013, 205, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Niewiadomska, I.; Kaczmarzyńska, S.; Augustynowicz, W. Distribution of resources and the severity of depression symptoms in people displaced as a result of military operations. Psychoprev. Stud. 2017, 1, 16–25. [Google Scholar]
- Radoń, A.; Niewiadomska, I.; Chwaszcz, J. Resource distribution and the severity of post-traumatic stress disorder symptoms in people displaced as a result of military operations. Psychoprev. Stud. 2017, 1, 5–15. [Google Scholar]
- Benjet, C.; Bromet, E.; Karam, E.; Kessler, R.; McLaughlin, K.; Ruscio, A.; Shahly, V.; Stein, D.J.; Petukhova, M.; Hill, E.; et al. The epidemiology of traumatic event exposure worldwide: Results from the World Mental Health Survey Consortium. Psychol. Med. 2016, 46, 327–343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baráth, A. Perception of trauma and symptoms of PTSD in adolescents in wartime and non-war conditions: An exploratory cross-cultural study. J. Psychol. Mental Health Care 2021, 6. [Google Scholar] [CrossRef]
- Heeke, C.; Kampisiou, C.; Niemeyer, H.; Knaevelsrud, C. A systematic review and meta-analysis of correlates of prolonged grief disorder in adults exposed to violent loss. Eur. J. Psychotraumatol. 2019, 10, 1583524. [Google Scholar] [CrossRef] [PubMed]
- Asch, R.H.; Esterlis, I.; Southwick, S.M.; Pietrzak, R.H. Risk and resilience factors associated with traumatic loss-related PTSD in U.S. military veterans: Results from the National Health and Resilience in Veterans Study. Psychiatry Res. 2021, 298, 113775. [Google Scholar] [CrossRef] [PubMed]
- Nickerson, A.; Bryant, R.A.; Steel, Z.; Silove, D.; Brooks, R. The impact of fear for family on mental health in a resettled Iraqi refugee community. J. Psychiatr. Res. 2009, 44, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Elhai, J.D.; Reeves, A.N.; Frueh, B.C. Predictors of Mental Health and Medical Service Use in Veterans Presenting With Combat-Related Posttraumatic Stress Disorder. Psychol. Serv. 2004, 1, 111–119. [Google Scholar] [CrossRef]
- Duke, M.R.; Moore, R.S.; Ames, G. PTSD Treatment-Seeking among Rural Latino Combat Veterans: A Review of the Literature. J. Rural Soc. Sci. 2011, 26, 157–180. [Google Scholar]
- Cohen, S.; Wills, T.A. Stress, Social Support, and the Buffering Hypothesis. Psychol. Bull. 1985, 98, 310–357. [Google Scholar] [CrossRef]
- King, D.W.; Leskin, G.A.; King, L.A.; Weathers, F.W. Confirmatory factor analysis of the clinician-administered PTSD Scale: Evidence for the dimensionality of posttraumatic stress disorder. Psychol. Assess. 1998, 10, 90–96. [Google Scholar] [CrossRef]
- Engdahl, B.; Dikel, T.D.; Eberly, R.; Blank, A. Posttraumatic Stress Disorder in a Community Group of Former Prisoners of War: A Normative Response to Severe Trauma. Am. J. Psychiatry 1997, 154, 1576–1581. [Google Scholar] [CrossRef] [PubMed]
- Xen, C.; Ge, Y.; Tang, B.; Liu, Y.; Kang, P.; Wang, M.; Zhang, L. A Meta-Analysis of Risk Factors for Combat-Related PTSD among Military Personnel and Veterans. PLoS ONE 2015, 10, e0120270. [Google Scholar] [CrossRef] [Green Version]
- Save the Children. Annual Report 2015. Available online: https://www.savethechildren.org/content/dam/usa/reports/annual-report/annual-report/sc-2015-annualreport.pdf (accessed on 12 August 2021).
- Betancourt, T.S.; Meyers-Ohki, S.E.; Charrow, A.P.; Tol, W.A. Interventions for Children Affected by War: An Ecological Perspective on Psychosocial Support and Mental Health Care. Harv. Rev. Psychiatry 2013, 21, 70–91. [Google Scholar] [CrossRef] [PubMed]
- Ijadi-Maghsoodi, R.; Moore, E.M.; Feller, S.; Cohenmehr, J.; Ryan, G.W.; Kataoka, S.; Gelberg, L. Beyond housing: Understanding community integration among homeless-experienced veteran families in the United States. Health Soc. Care Community 2020, 30, e493–e503. [Google Scholar] [CrossRef]
- Hobfoll, S.E.; Melissa, T.; Sandro, G. The Impact of Resource Loss and Traumatic Growth on Probable PTSD and Depression Following Terrorist Attacks. J. Trauma Stress 2006, 6, 867–878. [Google Scholar] [CrossRef] [Green Version]
- Solomon, Z.; Neria, Y.; Ohry, A.; Waysman, M.; Ginzburg, K. PTSD among Israeli former prisoners of war and soldiers with combat stress reaction: A longitudinal study. Am. J. Psychiatry 1994, 151, 554–559. [Google Scholar] [PubMed]
- Thabet, A.A.; Tawahina, A.A.; Sarraj, E.E.; Vostanis, P. Death Anxiety, PTSD, Trauma, Grief, and Mental Health of Palestinians Victims of War on Gaza. Health Care Curr. Rev. 2013, 1, 112. [Google Scholar] [CrossRef] [Green Version]
- Ainamani, H.E.; Elbert, T.; Olema, D.K.; Hecker, T. Gender differences in response to war-related trauma and posttraumatic stress disorder—A study among the Congolese refugees in Uganda. BMC Psychiatry 2020, 20, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Onyut, L.P.; Neuner, F.; Ertl, V.; Schauer, E.; Odenwald, M.; Elbert, T. Trauma, poverty and mental health among Somali and Rwandese refugees living in an African refugeee settlement—An epidemiological study. Confl. Health 2009, 3, 6. [Google Scholar] [CrossRef] [Green Version]
- Tekin, A.; Karadağ, H.; Süleymanoğlu, M.; Tekin, M.; Kayran, Y.; Alpak, G.; Sar, V. Prevalence and gender differences in symptomatology of posttraumatic stress disorder and depression among Iraqi Yazidis displaced into Turkey. Eur. J. Psychotraumatol. 2016, 7, 28556. [Google Scholar] [CrossRef]
- Macera, C.; Aralis, H.J.; Highfill-McRoy, R.; Rauh, M.J. Posttraumatic Stress Disorder After Combat Zone Deployment Among Navy and Marine Corps Men and Women. J. Women’s Health 2014, 23, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Luxton, D.D.; Greenburg, D.; Ryan, J.; Niven, A.; Wheeler, G.; Mysliwiec, V. Prevalence and Impact of Short Sleep Duration in Redeployed OIF Soldiers. Sleep 2011, 34, 1189–1195. [Google Scholar] [CrossRef] [Green Version]
- Tolin, D.F.; Foa, E.B. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychol. Bull. 2006, 132, 959–992. [Google Scholar] [CrossRef]
- Roberts, B.; Makhashvili, N.; Javakhishvili, J. Hidden Burderns of Conflict: Issues of Mental Health and Access to Services among IDPs in Ukraine; International Alert: London, UK; GIP: Tbilisi, Georgia; London School of Hygiene and Tropical Medicine: London, UK, 2017. [Google Scholar]
- Haskell, S.G.; Gordon, K.S.; Mattocks, K.; Duggal, M.; Erdos, J.; Justice, A.; Brandt, C.A. Gender Differences in Rates of Depression, PTSD, Pain, Obesity, and Military Sexual Trauma Among Connecticut War Veterans of Iraq and Afghanistan. J. Women’s Health 2010, 19, 267–271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schlenger, W.E.; Kulka, R.A.; Fairbank, J.A.; Hough, R.L.; Jordan, B.K.; Marmar, C.R.; Weiss, D.S. The prevalence of post-traumatic stress disorder in the Vietnam generation: A multimethod, multisource assessment of psychiatric disorder. J. Trauma Stress 1992, 5, 333–363. [Google Scholar] [CrossRef]
- Livingston, N.A.; Lee, D.J.; Mahoney, C.T.; Farmer, S.L.; Cole, T.; Marx, B.P.; Keane, T.M. Longitudinal assessment of PTSD and illicit drug use among male and female OEF-OIF veterans. Addict. Behav. 2021, 118, 106870. [Google Scholar] [CrossRef] [PubMed]
- Hester, D.R. Lack of access to mental health services contributing to the high suicide rates among veterans. Int. J. Ment. Health Syst. 2017, 11, 47. [Google Scholar] [CrossRef]
- Hikmet, J.; Nassar-McMillan, S.C.; Salman, W.A.; Tahar, M.; Jamil, L.H. Iraqi Gulf War Veteran Refugees in the U.S. Soc. Work Health Care 2006, 43, 85–98. [Google Scholar] [CrossRef]
- Al-Krenawi, A.; Graham, J.R. The impact of political violence on psychosocial functioning of individuals and families: The case of Palestinian adolescents. Child Adolesc. Ment. Health 2012, 17, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Collins, P.; Patel, V.; Joestl, S.; March, D.; Insel, T.R.; Daar, A.S.; Bordin, I.A.; Costello, E.J.; Durkin, M.; Fairburn, C.; et al. Grand challenges in global mental health. Nature 2011, 475, 27–30. [Google Scholar] [CrossRef] [PubMed]
- Wooten, N.R. Military Social Work: Opportunities and Challenges for Social Work Education. J. Soc. Work Educ. 2015, 51, 6–26. [Google Scholar] [CrossRef] [Green Version]
- Kranke, D.; Floersc, J.; Dobalian, A. Identifying Aspects of Sameness to Promote Veteran Reintegration with Civilians: Evidence and Implications for Military Social Work. Health Soc. Work 2019, 44, 61–64. [Google Scholar] [CrossRef]
- Forgey, M.A.; Young, S.L. Increasing Military Social Work Knowledge: An Evaluation of Learning Outcomes. Health Soc. Work 2014, 39, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Cox, D.; Pawar, M. The Field of Displacement and Forced Migration: Programs and Strategies. In International Social Work: Issues, Strategies, and Programs; Cox, D., Pawar, M., Eds.; SAGE: London, UK, 2006; pp. 393–422. [Google Scholar] [CrossRef]
- Seifert, R. Social Work and Armed Conflict: How the Everyday Practice of Social Work is Affected by International Politics. Soc. Dialogue. 2015, 10, 44–47. [Google Scholar]
- Semigina, T.; Gusak, N. Armed Conflict in Ukraine and Social Work Response to it: What strategies should be used for internally displaced persons? Soc. Health Commun. Stud. J. 2015, 2, 1–24. [Google Scholar]
- Denov, M.; Shevell, M.C. Social work practice with war affected children and families: The importance of family, culture, arts, and participatory approaches. J. Fam. Soc. Work 2019, 22, 1–16. [Google Scholar] [CrossRef]
- Rosshandler, Y.; Hall, B.J.; Canetti, D. An Application of an Ecological Framework to Understand Risk Factors of PTSD Due to Prolonged Conflict Exposure: Israeli and Palestinian Adolescents in the Line of Fire. Psychol. Trauma Theory Res. Pract. Policy 2016, 8, 641–648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frančišković, T.; Stevanović, A.; Klarić, M. Combat-Related Posttraumatic Stress Disorder and Families. In Military Deployment and its Consequences for Families. Risk and Resilience in Military and Veteran Families; MacDermid Wadsworth, S., Riggs, D., Eds.; Springer: New York, NY, USA, 2014; pp. 281–292. [Google Scholar] [CrossRef]
- O’Callaghan, P.; Branham, L.; Shannon, C.; Betancourt, T.S.; Dempster, M.; McMullen, J. A Pilot Study of a Family Focused, Psychosocial Intervention with War-Exposed Youth at Risk of Attack and Abduction in North-Eastern Democratic Republic of Congo. Child Abus. Neglect. 2014, 38, 1197–1207. [Google Scholar] [CrossRef]
- Pardeck, J.T. An Ecological Approach for Social Work Practice. J. Sociol. Soc. Welfare 1988, 15, 133–142. [Google Scholar]
- Sullivan, K.; Barr, N.; Kintzle, S.; Gilreath, T.; Castro, C.A. PTSD and Physical Health Symptoms Among Veterans: Association with Child and Relationship Functioning. Marriage Fam. Rev. 2016, 52, 689–705. [Google Scholar] [CrossRef]
- Elbogen, E.B.; Sullivan, C.P.; Wolfe, J.; Wagner, H.R.; Beckham, J.C. Homelessness and money mismanagement in Iraq and Afghanistan veterans. Am. J. Public Health 2013, 2, 248–254. [Google Scholar] [CrossRef]
- Young, Y.M.; Korinek, K.; Zimmer, Z.; Toan, T.K. Assessing Exposure to War-related Traumatic Events in Older Vietnamese War Survivors. Confl. Health 2021, 15, 14. [Google Scholar] [CrossRef]
| n | M | SD | Value | p | Effect Size | ||
|---|---|---|---|---|---|---|---|
| Age | ≤25 | 62 | 14.45 | 12.53 | 2.922 | 0.009 ** | 0.24 |
| 26–30 | 63 | 20.87 | 14.63 | ||||
| 31–35 | 62 | 22.52 | 12.35 | ||||
| 36–40 | 43 | 22.19 | 11.88 | ||||
| 41–45 | 29 | 24.52 | 16.81 | ||||
| 46–50 | 27 | 21.63 | 13.05 | ||||
| >50 | 17 | 23.24 | 17.46 | ||||
| Gender | Female | 74 | 25.39 | 14.18 | −3.420 | 0.001 ** | 0.45 |
| Male | 232 | 19.13 | 13.57 | ||||
| Civil status | Married/cohabitating | 127 | 21.37 | 14.50 | −0.459 | 0.647 | - |
| Single/separated/divorced/widow(er) | 172 | 20.63 | 13.32 | ||||
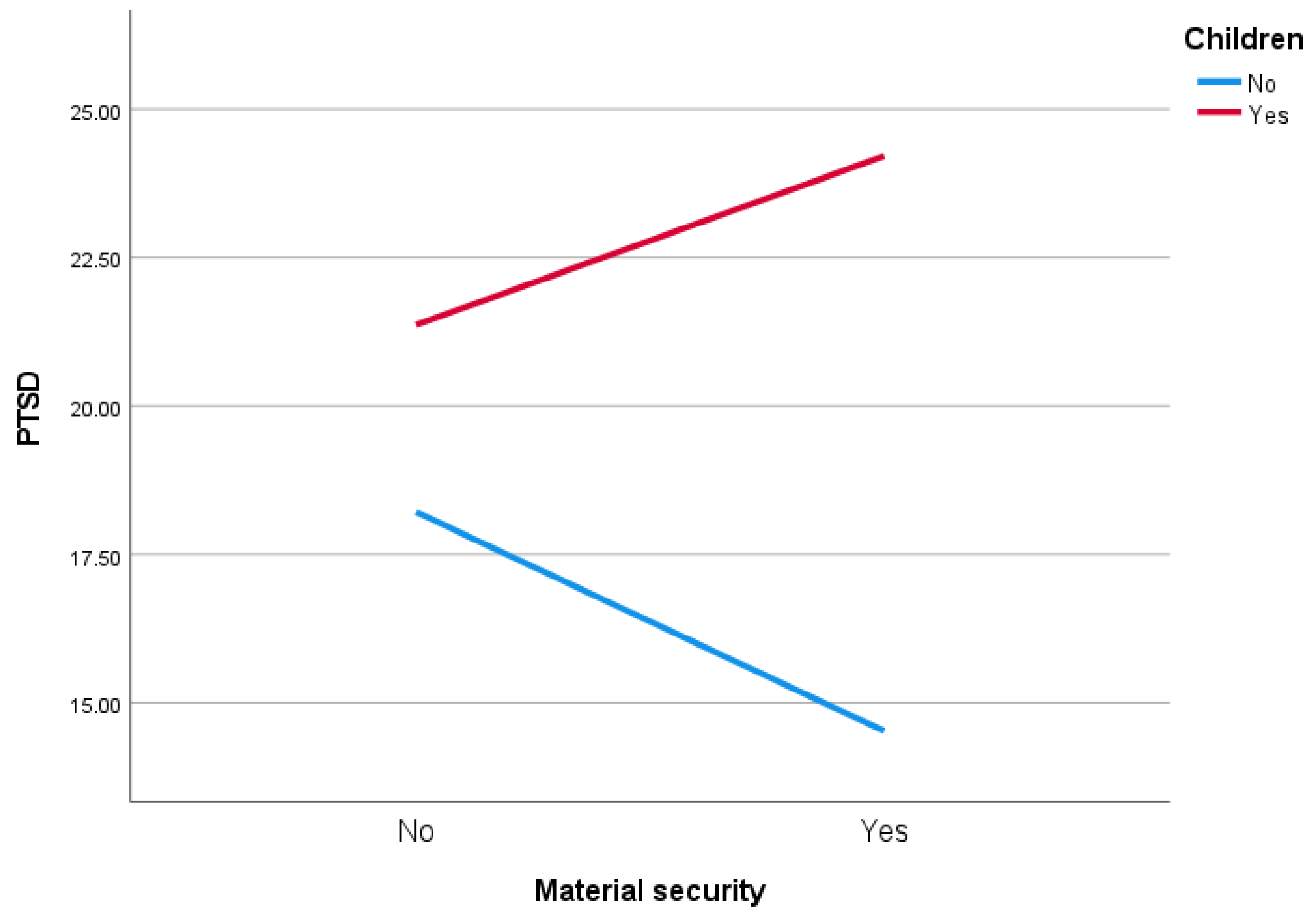
| Children | Yes | 192 | 22.83 | 14.06 | −3.719 | 0.000 *** | 0.44 |
| No | 116 | 16.88 | 12.83 | ||||
| Education | Primary/secondary education | 165 | 21.62 | 15.26 | 1.348 | 0.179 | - |
| Higher education | 132 | 19.40 | 12.55 | ||||
| Continuing education | Yes | 68 | 14.90 | 13.58 | 3.983 | 0.000 *** | 0.55 |
| No | 240 | 22.33 | 13.58 | ||||
| Place of residence | Village | 67 | 25.94 | 13.68 | 3.555 | 0.000 *** | 0.49 |
| City | 236 | 19.23 | 13.63 | ||||
| Material status | Bad | 144 | 22.64 | 14.84 | 2.499 | 0.013 * | 0.28 |
| Good | 163 | 18.73 | 12.57 | ||||
| Lost loved one | Yes | 57 | 28.65 | 16.27 | −5.090 | 0.000 *** | 0.69 |
| No | 245 | 18.61 | 12.67 | ||||
| Distance from hostilities | ≤500 km | 71 | 21.11 | 13.49 | 0.340 | 0.712 | - |
| 501–999 km | 171 | 19.61 | 13.68 | ||||
| ≥1000 km | 41 | 20.78 | 15.38 | ||||
| Health insurance | Yes | 54 | 16.61 | 12.48 | 2.448 | 0.015 * | 0.38 |
| No | 255 | 21.65 | 13.98 | ||||
| Savings | Yes | 75 | 18.52 | 12.07 | 1.584 | 0.114 | - |
| No | 233 | 21.42 | 14.33 | ||||
| Material security | Yes | 145 | 21.22 | 13.72 | −0.688 | 0.492 | - |
| No | 163 | 20.13 | 14.08 | ||||
| Model | R | R2 | Adjusted R2 | R2 Change | F Change | p |
|---|---|---|---|---|---|---|
| 1 | 0.286 | 0.082 | 0.078 | 0.082 | 24.106 | 0.000 *** |
| 2 | 0.379 | 0.143 | 0.137 | 0.062 | 19.413 | 0.000 *** |
| 3 | 0.429 | 0.184 | 0.175 | 0.041 | 13.412 | 0.000 *** |
| 4 | 0.480 | 0.231 | 0.219 | 0.047 | 16.233 | 0.000 *** |
| 5 | 0.508 | 0.258 | 0.244 | 0.027 | 9.720 | 0.002 ** |
| Unstandardized Coefficients | Beta | t | p | 95% CI | Collinearity | ||||
|---|---|---|---|---|---|---|---|---|---|
| B | S.E | Lower | Upper | Tol. | VIF | ||||
| Constant | 27.121 | 1.742 | 15.572 | 0.000 *** | 23.692 | 30.550 | |||
| Lost loved one | 7.543 | 1.951 | 0.208 | 3.867 | 0.000 *** | 3.703 | 11.384 | 0.957 | 1.045 |
| Place of residence | −1.972 | 0.385 | −0.280 | −5.126 | 0.000 *** | −2.729 | −1.215 | 0.931 | 1.074 |
| Gender | 8.682 | 1.801 | 0.270 | 4.821 | 0.000 *** | 5.136 | 12.228 | 0.889 | 1.124 |
| Continuing education | −6.091 | 1.797 | −0.185 | −3.389 | 0.001 ** | −9.630 | −2.552 | 0.930 | 1.076 |
| Health insurance | −6.333 | 2.031 | −0.172 | −3.118 | 0.002 ** | −10.332 | −2.334 | 0.911 | 1.097 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fel, S.; Jurek, K.; Lenart-Kłoś, K. Relationship between Socio-Demographic Factors and Posttraumatic Stress Disorder: A Cross Sectional Study among Civilian Participants’ Hostilities in Ukraine. Int. J. Environ. Res. Public Health 2022, 19, 2720. https://doi.org/10.3390/ijerph19052720
Fel S, Jurek K, Lenart-Kłoś K. Relationship between Socio-Demographic Factors and Posttraumatic Stress Disorder: A Cross Sectional Study among Civilian Participants’ Hostilities in Ukraine. International Journal of Environmental Research and Public Health. 2022; 19(5):2720. https://doi.org/10.3390/ijerph19052720
Chicago/Turabian StyleFel, Stanisław, Krzysztof Jurek, and Katarzyna Lenart-Kłoś. 2022. "Relationship between Socio-Demographic Factors and Posttraumatic Stress Disorder: A Cross Sectional Study among Civilian Participants’ Hostilities in Ukraine" International Journal of Environmental Research and Public Health 19, no. 5: 2720. https://doi.org/10.3390/ijerph19052720






