Cardio-Pulmonary Dysfunction Evaluation in Patients with Persistent Post-COVID-19 Headache
Abstract
:1. Introduction
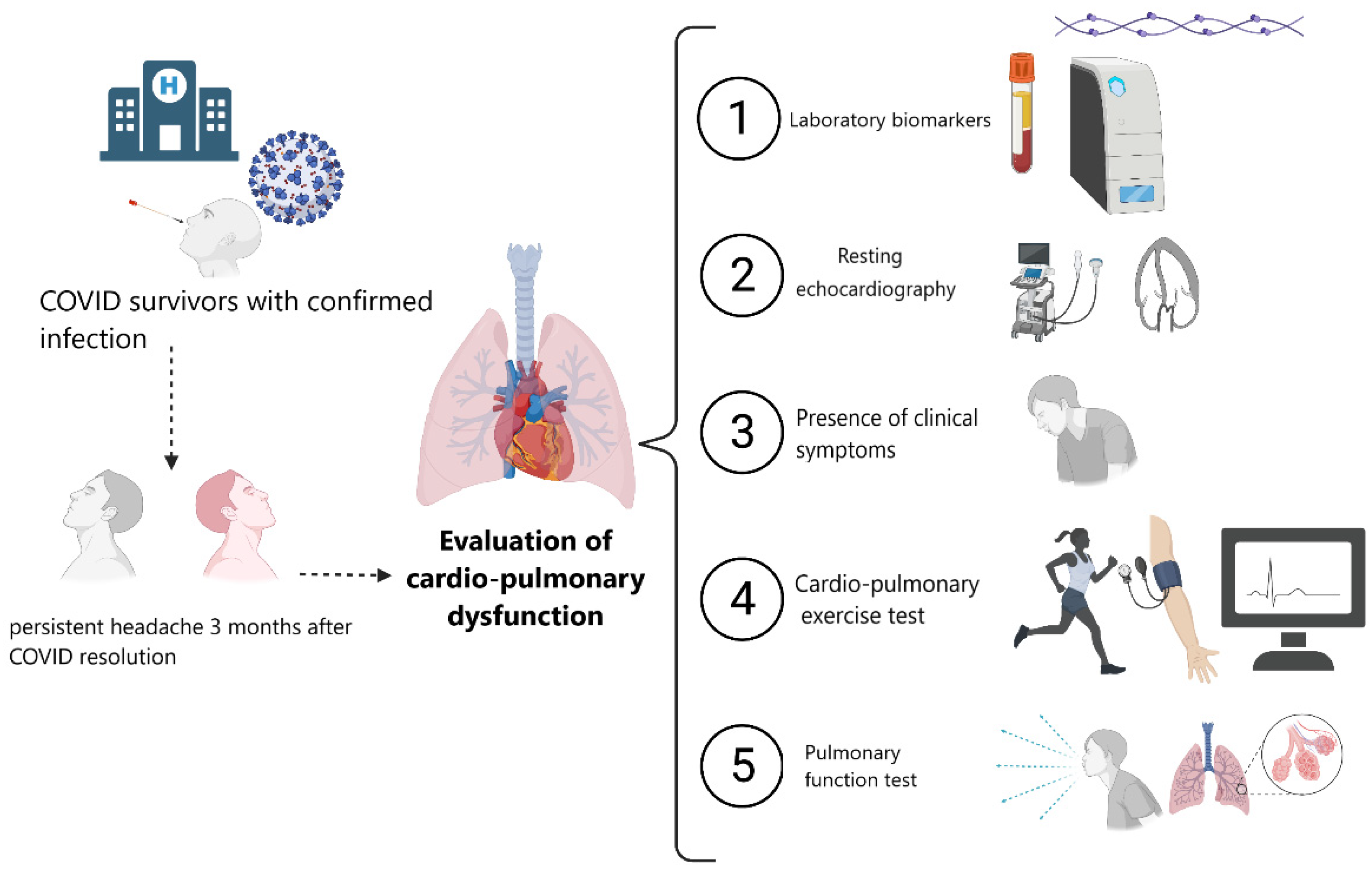
2. Materials and Methods
2.1. Study Design and Patient Selection
2.2. Eligibility Criteria
2.3. Procedure
2.3.1. Demographics and Clinical Data
2.3.2. Quality-of-Life Questionnaire
2.3.3. Pulmonary Function Test
2.3.4. Resting Echocardiography
2.3.5. Cardio-Pulmonary Exercise Test
2.3.6. Laboratory Biomarkers
2.4. Ethics
2.5. Statistical Analysis
3. Results
3.1. Participants
3.2. Laboratory Biomarkers, Echocardiographic Findings, and Quality of Life
3.3. Pulmonary Function Test and Cardio-Pulmonary Exercise Test
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eccles, R. Understanding the symptoms of the common cold and influenza. Lancet Infect. Dis. 2005, 5, 718–725. [Google Scholar] [CrossRef]
- Kuchar, E.; Miśkiewicz, K.; Nitsch-Osuch, A.; Szenborn, L. Pulmonary Infection. Adv. Exp. Med. Biol. 2015, 857, 25–38. [Google Scholar]
- Trigo, J.; García-Azorín, D.; Planchuelo-Gómez, Á.; Martínez-Pías, E.; Talavera, B.; Hernández-Pérez, I.; Valle-Peñacoba, G.; Simón-Campo, P.; De Lera, M.; Chavarría-Miranda, A.; et al. Factors associated with the presence of headache in hospitalized COVID-19 patients and impact on prognosis: A retrospective cohort study. J. Headache Pain 2020, 21, 94. [Google Scholar] [CrossRef]
- Membrilla, J.A.; Lorenzo, Í.; Sastre, M.; de Terán, J.D. Headache as a Cardinal Symptom of Coronavirus Disease 2019: A Cross-Sectional Study. Headache J. Head Face Pain 2020, 60, 2176–2191. [Google Scholar] [CrossRef] [PubMed]
- Caronna, E.; Ballvé, A.; Llauradó, A.; Gallardo, V.J.; Ariton, D.M.; Lallana, S.; Maza, S.L.; Gadea, M.O.; Quibus, L.; Restrepo, J.L.; et al. Headache: A striking prodromal and persistent symptom, predictive of COVID-19 clinical evolution. Cephalalgia 2020, 40, 1410–1421. [Google Scholar] [CrossRef]
- Suárez-Robles, M.; Iguaran-Bermúdez, M.d.R.; García-Klepizg, J.L.; Lorenzo-Villalba, N.; Méndez-Bailón, M. 90 days post-hospitalization evaluation of residual COVID-19 symptoms through a phone call check list. Pan Afr. Med. J. 2020, 37, 289. [Google Scholar] [CrossRef]
- Logue, J.K.; Franko, N.M.; McCulloch, D.J.; McDonald, D.; Magedson, A.; Wolf, C.R.; Chu, H.Y. Sequelae in Adults at 6 Months After COVID-19 Infection. JAMA Netw. Open 2021, 4, e210830. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Azorin, D.; Layos-Romero, A.; Porta-Etessam, J.; Membrilla, J.A.; Caronna, E.; Gonzalez-Martinez, A.; Mencia, Á.S.; Segura, T.; Gonzalez-García, N.; Díaz-de-Terán, J.; et al. Post-COVID-19 persistent headache: A multicentric 9-months follow-up study of 905 patients. Cephalalgia Int. J. Headache 2022. Advance online publication. [Google Scholar] [CrossRef]
- Rocha-Filho, P.A.S.; Magalhães, J.E. Headache associated with COVID-19: Frequency, characteristics and association with anosmia and ageusia. Cephalalgia 2020, 40, 1443–1451. [Google Scholar] [CrossRef]
- Spuntarelli, V.; Luciani, M.; Bentivegna, E.; Marini, V.; Falangone, F.; Conforti, G.; Rachele, E.S.; Martelletti, P. COVID-19: Is it just a lung disease? A case-based review. SN Compr. Clin. Med. 2020, 2, 1401–1406. [Google Scholar] [CrossRef]
- Martelletti, P.; Bentivegna, E.; Spuntarelli, V.; Luciani, M. Long-COVID Headache. SN Compr. Clin. Med. 2021, 3, 1704–1706. [Google Scholar] [CrossRef]
- Soriano, J.B.; Murthy, S.; Marshall, J.C.; Relan, P.; Diaz, J.V.; WHO Clinical Case Definition Working Group on Post-COVID-19 Condition. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect. Dis. 2022, 22, e102–e107. [Google Scholar] [CrossRef]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef]
- Gonzalez-Martinez, A.; Fanjul, V.; Ramos, C.; Ballesteros, J.S.; Bustamante, M.; Martí, A.V.; Álvarez, C.; del Álamo, Y.G.; Vivancos, J.; Gago-Veiga, A.B. Headache during SARS-CoV-2 infection as an early symptom associated with a more benign course of disease: A case–control study. Eur. J. Neurol. 2021, 28, 3426–3436. [Google Scholar] [CrossRef]
- Martelletti, P.; Bentivegna, E.; Luciani, M.; Spuntarelli, V. Headache as a Prognostic Factor for COVID-19. Time to Re-evaluate. SN Compr. Clin. Med. 2020, 2, 2509–2510. [Google Scholar] [CrossRef]
- Bolay, H.; Karadas, Ö.; Oztürk, B.; Sonkaya, R.; Tasdelen, B.; Bulut, T.D.S.; Gülbahar, Ö.; Özge, A.; Baykan, B. HMGB1, NLRP3, IL-6 and ACE2 levels are elevated in COVID-19 with headache: A window to the infection-related headache mechanism. J. Headache Pain 2021, 22, 94. [Google Scholar] [CrossRef]
- Trigo, J.; García-Azorín, D.; Sierra-Mencía, Á.; Tamayo-Velasco, Á.; Martínez-Paz, P.; Tamayo, E.; Guerrero, A.L.; Gonzalo-Benito, H. Cytokine and interleukin profile in patients with headache and COVID-19: A pilot, CASE-control, study on 104 patients. J. Headache Pain 2021, 22, 51. [Google Scholar] [CrossRef]
- Belvis, R. Headaches During COVID-19: My Clinical Case and Review of the Literature. Headache J. Head Face Pain 2020, 60, 1422–1426. [Google Scholar] [CrossRef]
- Bolay, H.; Gül, A.; Baykan, B. COVID-19 is a Real Headache! Headache J. Head Face Pain 2020, 60, 1415–1421. [Google Scholar] [CrossRef]
- Tolebeyan, A.S.; Zhang, N.; Cooper, V.; Kuruvilla, D.E. Headache in Patients With Severe Acute Respiratory Syndrome Coronavirus 2 Infection: A Narrative Review. Headache J. Head Face Pain 2020, 60, 2131–2138. [Google Scholar] [CrossRef]
- Peng, K.-P. Association between COVID-19 and headache: What evidence and history tell us. Cephalalgia 2001, 40, 1403–1405. [Google Scholar] [CrossRef]
- World Health Organization. Clinical Management of Severe Acute Respiratory Infection When Novel Coronavirus (COVID-19) Infection is Suspected: Interim Guidance. 28 January 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf (accessed on 19 June 2021).
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38, 1–211. [Google Scholar] [CrossRef]
- Spertus, J.A.; Jones, P.G.; Sandhu, A.T.; Arnold, S.V. Interpreting the Kansas City Cardiomyopathy Questionnaire in Clinical Trials and Clinical Care JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 76, 2379–2390. [Google Scholar] [CrossRef]
- Graham, B.L.; Brusasco, V.; Burgos, F.; Cooper, B.G.; Jensen, R.; Kendrick, A.; MacIntyre, N.R.; Thompson, B.R.; Wanger, R. 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur. Respir. J. 2017, 49, 1600016. [Google Scholar] [CrossRef] [Green Version]
- Graham, B.L.; Steenbruggen, I.; Miller, M.R.; Barjaktarevic, I.Z.; Cooper, B.G.; Hall, G.L.; Hallstrand, T.S.; Kaminsky, D.A.; McCarthy, K.; McCormack, M.C.; et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am. J. Respir. Crit. Care Med. 2019, 200, e70–e88. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–271. [Google Scholar] [CrossRef]
- Balady, G.J.; Arena, R.; Sietsema, K.; Myers, J.; Coke, L.; Fletcher, G.F.; Forman, D.; Franklin, B.; Guazzi, M.; Gulati, M.; et al. Clinician’s Guide to Cardiopulmonary Exercise Testing in Adults. Circulation 2010, 122, 191–225. [Google Scholar] [CrossRef] [Green Version]
- Raffaelli, B.; Mecklenburg, J.; Scholler, S.; Overeem, L.H.; Gonçalves, A.S.O.; Reuter, U.; Neeb, L. Primary headaches during the COVID-19 lockdown in Germany: Analysis of data from 2325 patients using an electronic headache diary. J. Headache Pain 2021, 22, 59. [Google Scholar] [CrossRef]
- Wei, J.; Wang, H. Cardiac cephalalgia: Case reports and review. Cephalalgia 2008, 28, 892–896. [Google Scholar] [CrossRef]
- Blacky, R.A.; Rittelmeyer, J.T.; Wallace, M.R. Headache angina. Am. J. Cardiol. 1987, 60, 730. [Google Scholar] [CrossRef]
- Giustino, G.; Croft, L.B.; Stefanini, G.G.; Bragato, R.; Silbiger, J.J.; Vicenzi, M.; Danilov, T.; Kukar, N.; Shaban, N.; Kini, A.; et al. Characterization of Myocardial Injury in Patients With COVID-19. J. Am. Coll. Cardiol. 2020, 76, 2043–2055. [Google Scholar] [CrossRef]
- Imazio, M.; Klingel, K.; Kindermann, I.; Brucato, A.; De Rosa, F.G.; Adler, Y.; De Ferrari, G.M. COVID-19 pandemic and troponin: Indirect myocardial injury, myocardial inflammation or myocarditis? Heart 2020, 106, 1127–1131. [Google Scholar] [CrossRef]
- García-Azorín, D.; Martínez-Pías, E.; Trigo, J.; Hernández-Pérez, I.; Valle-Peñacoba, G.; Talavera, B.; Simón-Campo, P.; De Lera, M.; Chavarría-Miranda, A.; López-Sanz, C.; et al. Neurological Comorbidity Is a Predictor of Death in Covid-19 Disease: A Cohort Study on 576 Patients. Front. Neurol. 2020, 11, 781. [Google Scholar] [CrossRef]
- Motiejunaite, J.; Balagny, P.; Arnoult, F.; Mangin, L.; Bancal, C.; d’Ortho, M.-P.; Frija-Masson, J. Hyperventilation: A Possible Explanation for Long-Lasting Exercise Intolerance in Mild COVID-19 Survivors? Front. Physiol. 2021, 11, 614590. [Google Scholar] [CrossRef]
- Crisafulli, E.; Gabbiani, D.; Magnani, G.; Dorelli, G.; Busti, F.; Sartori, G.; Senna, G.; Girelli, D. Residual Lung Function Impairment Is Associated with Hyperventilation in Patients Recovered from Hospitalised COVID-19: A Cross-Sectional Study. J. Clin. Med. 2021, 10, 1036. [Google Scholar] [CrossRef]
- Aparisi, Á.; Ybarra-Falcón, C.; García-Gómez, M.; Tobar, J.; Iglesias-Echeverría, C.; Jaurrieta-Largo, S.; Ladrón, R.; Uribarri, A.; Catalá, P.; Hinojosa, W.; et al. Exercise Ventilatory Inefficiency in Post-COVID-19 Syndrome: Insights from a Prospective Evaluation. J. Clin. Med. 2021, 10, 2591. [Google Scholar] [CrossRef]
- Furlan, J.C. Headache attributed to autonomic dysreflexia. Neurology 2011, 77, 792–798. [Google Scholar] [CrossRef]
| Variable | Entire Study Sample N = 70 (100%) | Headache N = 10 (14.3%) | Non-Headache N = 60 (85.7%) | p-Value |
|---|---|---|---|---|
| Demographics | ||||
| Female sex | 45 (64.3) | 10 (100) | 35 (58.3) | 0.011 |
| Age, years | 54.8 ± 11.9 | 46.9 ± 8.45 | 56.13 ± 11.9 | 0.023 |
| BMI, kg/m2 | 27.2 ± 4.6 | 26.43 ± 3.45 | 27.45 ± 4.75 | 0.585 |
| BSA, m2 | 1.82 ± 0.18 | 1.74 ± 0.16 | 1.83 ± 0.18 | 0.118 |
| CKD * | 3 (4.4) | 0 | 3 (5.2) | 0.999 |
| Diabetes | 3 (5.9) | 0 | 3 (5.7) | 0.999 |
| Dyslipidemia | 13 (19.1) | 0 | 13 (22.4) | 0.597 |
| Hypertension | 18 (26.5) | 1 (10) | 17 (29.3) | 0.270 |
| Previous CAD | 1 (1.5) | 0 | 1 (1.7) | 0.999 |
| Prior pulmonary disease | 5 (7.4) | 0 | 5 (8.6) | 0.999 |
| Prior stroke/TIA | 1 (1.5) | 0 | 1 (1.7) | 0.999 |
| Long-COVID symptoms during follow-up | ||||
| Chest pain | 8 (11.4) | 3 (30) | 5 (8.3) | 0.081 |
| Dyspnea | 41 (58.6) | 6 (60) | 35 (58.3) | 0.999 |
| Fatigue | 20 (28.6) | 3 (30) | 17 (28.3) | 0.999 |
| Myalgia | 6 (8.6) | 3 (30) | 3 (5) | 0.034 |
| Neurological symptoms ** | 14 (20) | 7 (70) | 7 (11.7) | <0.001 |
| Paresthesia | 4 (5.7) | 2 (20) | 2 (3.3) | 0.095 |
| Olfactory abnormalities | 6 (8.6) | 3 (30) | 3 (5.0) | 0.034 |
| Taste abnormalities | 4 (5.7) | 1 (10) | 3 (5.0) | 0.468 |
| Palpitations | 10 (14.3) | 3 (30) | 7 (11.7) | 0.147 |
| Entire Study Sample N = 70 (100%) | Headache N = 10 (14.3%) | Non-Headache N = 60 (85.7%) | p-Value | |
|---|---|---|---|---|
| Laboratory markers | ||||
| AST (UI/L) | 19 (16–25) | 16 (11–22) | 21 (18–20) | 0.057 |
| C-reactive protein (mg/L) | 1.3 (1–2.8) | 1.6 (1–2.6) | 1.3 (1–2.8) | 0.992 |
| Creatinine (mg/dL) | 0.84 (0.75–0.98) | 0.82 (0.77–0.85) | 0.85 (0.75–0.99) | 0.411 |
| D-Dimer (ng/mL) | 265 (188–377) | 240.5 (154–413) | 267 (196–377) | 0.618 |
| Ferritin (ng/mL) | 113.1 (50.1–159.1) | 55.65 (30.5–123) | 122 (53.3–171.3) | 0.052 |
| Fibrinogen | 427 (376–491) | 498 (468–504) | 421 (367–466) | 0.028 |
| Interleukin-6 (pg/mL) | 3.42 (2.6–4.4) | 2.62 (2.28–3.48) | 3.49 (2.63–4.45) | 0.174 |
| Haemoglobin (g/dL) | 14 (13.5–15.3) | 13.8 (13.6–14.7) | 14.2 (13.5–15.6) | 0.310 |
| Lymphocytes (cells/mm3) | 2185 (1800–2790) | 1845 (1520–2650) | 2270 (1815–2900) | 0.264 |
| NT-ProBNP (pg/mL) | 41 (23–68) | 50 (25–92) | 39.5 (20–68) | 0.669 |
| Hs TnT (pg/mL) | 5.4 (3.1–7.54) | 3 (3–3.67) | 5.57 (3.93–7.7) | 0.029 |
| Resting echocardiographic findings | ||||
| LAVI (mL/m2) | 22.1 (17.7–27.8) | 23.4 (21.2–25.4) | 217 (17.6–29) | 0.999 |
| LVEF (%) | 64 (59–68) | 66 (61–70) | 63 (58–68) | 0.233 |
| LVEDVi (mL/m2) | 75 (66–100) | 39.6 (33.1–42.4) | 44.4 (38.4–54.2) | 0.067 |
| LVESVi (mL/m2) | 16.2 (12.3–20.1) | 14 (10.2–16.7) | 16.5 (12.7–20.6) | 0.196 |
| Mitral E/A ratio | 0.9 (0.76–1.22) | 1.27 (1.06–1.48) | 0.88 (0.75–1.2) | 0.010 |
| E/e’ | 6.5 (4.9–7.9) | 6.27 (4.7–7.35) | 6.57 (5–8.13) | 0.544 |
| TAPSE (mm) | 23 (20–26) | 22 (21–26) | 23 (20–25) | 0.853 |
| Global longitudinal strain (%) | 20 (22–19) | 20 (22–19) | 20 (22–19) | 0.643 |
| Kansas City Cardiomyopathy Questionnaire | ||||
| Global score | 70 ± 19.42 | 64.53 ± 22.5 | 71 ± 18.8 | 0.335 |
| QoL | 58.4 ± 29.55 | 57.5 ± 33.9 | 58.6 ± 29 | 0.918 |
| Physical function | 66.9 ± 14.6 | 65 ± 14.4 | 67.28 ± 14.8 | 0.654 |
| Social function | 65.46 ± 26.7 | 49.5 ± 25.1 | 68.4 ± 21.2 | 0.014 |
| Symptom score | 80.7 ± 22.6 | 70.2 ± 21.8 | 82.6 ± 20.8 | 0.235 |
| Entire Study Sample N = 70 (100%) | Headache N = 10 (14.3%) | Non-Headache N = 60 (85.7%) | p-Value | |
|---|---|---|---|---|
| Cardio-pulmonary exercise test | ||||
| Breathing reserve (%) | 41 (32–51) | 45 (30–50) | 41 (34–52) | 0.723 |
| RER | 1.11 (1.05–1.21) | 1.05 (1.01–1.08) | 1.12 (1.05–1.21) | 0.059 |
| Peak Vo2 (mL/min/kg) | 19.4 (17.2–24.8) | 19.9 (17.2–22.6) | 19.5 (17.1–24.6) | 0.754 |
| % of predicted pVo2 | 88 (76–100) | 88 (78–94) | 88 (74–100) | 0.820 |
| Vo2 at AT1 (mL/min/kg) | 15.4 (12–19.2) | 18.7 (14.9–19.6) | 15.3 (11.8–19) | 0.219 |
| % of predicted Vo2/HR | 101 (83–110) | 103 (93–108) | 101 (79–110) | 0.756 |
| VE/Vco2 slope | 30.3 (27.5–34.9) | 30 (29.7–34.3) | 30.6 (27–35.5) | 0.942 |
| VE/Vco2 at AT1 | 34.7 (32.3–39.5) | 33.7 (32.5–39.5) | 34.9 (32.2–39.3) | 0.806 |
| PETCO2 (mmHg) at AT1 | 38 (33.5–39.5) | 38 (34–38) | 37 (33.5–40) | 0.956 |
| % of predicted HR | 90.3 (83.9–97.4) | 87 (81.7–94.7) | 92 (84–99) | 0.385 |
| Resting systolic BP (mmHg) | 139 (124–146) | 122 (109–140) | 140 (126–147) | 0.020 |
| Peak systolic BP (mmHg) | 143 (160–177) | 139 (134–143) | 163 (151–180) | <0.001 |
| Resting diastolic BP (mmHg) | 86 (77–95) | 86 (75–94) | 86 (75–95) | 0.692 |
| Peak diastolic BP (mmHg) | 90 (81–100) | 80 (77–90) | 91 (85–100) | 0.059 |
| Pulmonary function | ||||
| DLCO % of predicted | 88.8 (80–97) | 94 (85.5–97) | 87 (79–95.3) | 0.297 |
| FEV1 % of predicted | 112 (103.5–121.5) | 114 (104–124) | 112 (103–120) | 0.742 |
| FVC% of predicted | 116 (105–131) | 124 (114–132) | 115 (104–130) | 0.263 |
| FEV1/FVC (%) | 100 (91.6–105) | 99 (94–103) | 100 (90–105) | 0.728 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aparisi, Á.; Ybarra-Falcón, C.; Iglesias-Echeverría, C.; García-Gómez, M.; Marcos-Mangas, M.; Valle-Peñacoba, G.; Carrasco-Moraleja, M.; Fernández-de-las-Peñas, C.; Guerrero, Á.L.; García-Azorín, D. Cardio-Pulmonary Dysfunction Evaluation in Patients with Persistent Post-COVID-19 Headache. Int. J. Environ. Res. Public Health 2022, 19, 3961. https://doi.org/10.3390/ijerph19073961
Aparisi Á, Ybarra-Falcón C, Iglesias-Echeverría C, García-Gómez M, Marcos-Mangas M, Valle-Peñacoba G, Carrasco-Moraleja M, Fernández-de-las-Peñas C, Guerrero ÁL, García-Azorín D. Cardio-Pulmonary Dysfunction Evaluation in Patients with Persistent Post-COVID-19 Headache. International Journal of Environmental Research and Public Health. 2022; 19(7):3961. https://doi.org/10.3390/ijerph19073961
Chicago/Turabian StyleAparisi, Álvaro, Cristina Ybarra-Falcón, Carolina Iglesias-Echeverría, Mario García-Gómez, Marta Marcos-Mangas, Gonzalo Valle-Peñacoba, Manuel Carrasco-Moraleja, César Fernández-de-las-Peñas, Ángel L. Guerrero, and David García-Azorín. 2022. "Cardio-Pulmonary Dysfunction Evaluation in Patients with Persistent Post-COVID-19 Headache" International Journal of Environmental Research and Public Health 19, no. 7: 3961. https://doi.org/10.3390/ijerph19073961
APA StyleAparisi, Á., Ybarra-Falcón, C., Iglesias-Echeverría, C., García-Gómez, M., Marcos-Mangas, M., Valle-Peñacoba, G., Carrasco-Moraleja, M., Fernández-de-las-Peñas, C., Guerrero, Á. L., & García-Azorín, D. (2022). Cardio-Pulmonary Dysfunction Evaluation in Patients with Persistent Post-COVID-19 Headache. International Journal of Environmental Research and Public Health, 19(7), 3961. https://doi.org/10.3390/ijerph19073961







