Current Standards of Early Rehabilitation after Anterior Cruciate Ligament Reconstruction in German Speaking Countries—Differentiation Based on Tendon Graft and Concomitant Injuries
Abstract
:1. Introduction
- (1)
- Does (a) the use of a specific tendon graft, and (b) potentially additional therapy of concomitant pathologies influence surgeons’ choice of a distinct postoperative rehabilitation protocol after ACLR?
- (2)
- To what extent do these rehabilitation recommendations differ?
2. Materials and Methods
3. Results
3.1. Algorithm of Evaluation
3.2. Categories of Early Rehabilitation
3.2.1. Weight Bearing
3.2.2. Range of Motion (ROM)
3.2.3. Utilization of Braces
3.2.4. Continuous Passive/Action Motion Therapy (CPM/CAM)
3.2.5. Start of Rehabilitation and Specific Training
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Colombet, P.; Dejour, D.; Panisset, J.C.; Siebold, R. Current concept of partial anterior cruciate ligament ruptures. Orthop. Traumatol. Surg. Res. 2010, 96 (Suppl. 8), 109–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koch, M.; Zellner, J.; Berner, A.; Grechenig, S.; Krutsch, V.; Nerlich, M.; Angele, P.; Krutsch, W. Influence of preparation and football skill level on injury incidence during an amateur football tournament. Arch. Orthop. Trauma Surg. 2016, 136, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Krutsch, W.; Zellner, J.; Zeman, F.; Nerlich, M.; Koch, M.; Pfeifer, C.; Angele, P. Sports-specific differences in postsurgical infections after arthroscopically assisted anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3878–3883. [Google Scholar] [CrossRef] [PubMed]
- Middleton, K.K.; Hamilton, T.; Irrgang, J.J.; Karlsson, J.; Harner, C.D.; Fu, F.H. Anatomic anterior cruciate ligament (ACL) reconstruction: A global perspective. Part 1. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1467–1482. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.L.; Maradit Kremers, H.; Bryan, A.J.; Larson, D.R.; Dahm, D.L.; Levy, B.A.; Stuart, M.J.; Krych, A.J. Incidence of Anterior Cruciate Ligament Tears and Reconstruction: A 21-Year Population-Based Study. Am. J. Sports Med. 2016, 44, 1502–1507. [Google Scholar] [CrossRef] [PubMed]
- Paschos, N.K.; Howell, S.M. Anterior cruciate ligament reconstruction: Principles of treatment. EFORT Open Rev. 2016, 1, 398–408. [Google Scholar] [CrossRef] [PubMed]
- Shaerf, D.A.; Pastides, P.S.; Sarraf, K.M.; Willis-Owen, C.A. Anterior cruciate ligament reconstruction best practice: A review of graft choice. World J. Orthop. 2014, 5, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Krutsch, W.; Zellner, J.; Baumann, F.; Pfeifer, C.; Nerlich, M.; Angele, P. Timing of anterior cruciate ligament reconstruction within the first year after trauma and its influence on treatment of cartilage and meniscus pathology. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 418–425. [Google Scholar] [CrossRef]
- Vundelinckx, B.; Herman, B.; Getgood, A.; Litchfield, R. Surgical Indications and Technique for Anterior Cruciate Ligament Reconstruction Combined with Lateral Extra-articular Tenodesis or Anterolateral Ligament Reconstruction. Clin. Sports Med. 2017, 36, 135–153. [Google Scholar] [CrossRef] [PubMed]
- Landes, S.; Nyland, J.; Elmlinger, B.; Tillett, E.; Caborn, D. Knee flexor strength after ACL reconstruction: Comparison between hamstring autograft, tibialis anterior allograft, and non-injured controls. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 317–324. [Google Scholar] [CrossRef]
- Mohtadi, N.G.; Chan, D.S.; Dainty, K.N.; Whelan, D.B. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst. Rev. 2011, 9, CD005960. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, N.; Horibe, S.; Sasaki, S.; Kitaguchi, T.; Tagami, M.; Mitsuoka, T.; Toritsuka, Y.; Hamada, M.; Shino, K. Evaluation of active knee flexion and hamstring strength after anterior cruciate ligament reconstruction using hamstring tendons. Arthroscopy 2002, 18, 598–602. [Google Scholar] [CrossRef]
- Kruse, L.M.; Gray, B.; Wright, R.W. Rehabilitation after anterior cruciate ligament reconstruction: A systematic review. J. Bone Jt. Surg. Am. 2012, 94, 1737–1748. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malempati, C.; Jurjans, J.; Noehren, B.; Ireland, M.L.; Johnson, D.L. Current Rehabilitation Concepts for Anterior Cruciate Ligament Surgery in Athletes. Orthopedics 2015, 38, 689–696. [Google Scholar] [CrossRef] [Green Version]
- Wilk, K.E.; Macrina, L.C.; Cain, E.L.; Dugas, J.R.; Andrews, J.R. Recent advances in the rehabilitation of anterior cruciate ligament injuries. J. Orthop. Sports Phys. Ther. 2012, 42, 153–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cavanaugh, J.T.; Powers, M. ACL Rehabilitation Progression: Where Are We Now? Curr. Rev. Musculoskelet. Med. 2017, 10, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Eckenrode, B.J.; Carey, J.L.; Sennett, B.J.; Zgonis, M.H. Prevention and Management of Post-operative Complications Following ACL Reconstruction. Curr Rev. Musculoskelet. Med. 2017, 10, 315–321. [Google Scholar] [CrossRef] [Green Version]
- Andrade, R.; Pereira, R.; van Cingel, R.; Staal, J.B.; Espregueira-Mendes, J. How should clinicians rehabilitate patients after ACL reconstruction? A systematic review of clinical practice guidelines (CPGs) with a focus on quality appraisal (AGREE II). Br. J. Sports Med. 2020, 54, 512–519. [Google Scholar] [CrossRef] [PubMed]
- Deutsche Gesellschaft für Orthopädie und Unfallchirurgie (DGOU) (2021) Nachbehandlungsempfehlungen 2021. 41. Vorderes Kreuzband, Operativ, Arthroskopisch. S83.53. 7th Edition. pp. 98–99. Available online: https://dgou.de/fileadmin/dgou/dgou/Dokumente/Gremien/Sektionen/Rehabilitation/NBE_2021_web.pdf (accessed on 5 March 2022).
- Meuffels, D.E.; Poldervaart, M.T.; Diercks, R.L.; Fievez, A.W.F.M.; Patt, T.W.; van Hart, C.P.; Hammacher, E.R.; van der Meer, F.; Saris, D.B. Guideline on anterior cruciate ligament injury: A multidisciplinary review by the Dutch Orthopaedic Association. Acta Orthop. 2012, 83, 379–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Melick, N.; van Cingel, R.E.; Brooijmans, F.; Neeter, C.; van Tienen, T.; Hullegie, W.; Nijhuis-van der Sanden, M.W.G. Evidence-based clinical practice update: Practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br. J. Sports Med. 2016, 50, 1506–1515. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wright, R.W.; Haas, A.K.; Anderson, J.; Calabrese, G.; Cavanaugh, J.; Hewett, T.E. Anterior Cruciate Ligament Reconstruction Rehabilitation: MOON Guidelines. Sports Health 2015, 7, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Beynnon, B.D.; Johnson, R.J.; Abate, J.A.; Fleming, B.C.; Nichols, C.E. Treatment of anterior cruciate ligament injuries, part 2. Am. J. Sports Med. 2005, 33, 1751–1767. [Google Scholar] [CrossRef] [PubMed]
- Biggs, A.; Jenkins, W.L.; Urch, S.E.; Shelbourne, K.D. Rehabilitation for Patients Following ACL Reconstruction: A Knee Symmetry Model. N. Am. J. Sports Phys. Ther. 2009, 4, 2–12. [Google Scholar] [PubMed]
- Saka, T. Principles of postoperative anterior cruciate ligament rehabilitation. World J. Orthop. 2014, 5, 450–459. [Google Scholar] [CrossRef] [PubMed]
- AWMF. Leitlinie "Vordere Kreuzbandruptur". AWMF Online-Das Portal der Wissenschaftlichen Medizin. 2018. Available online: https://www.awmf.org/leitlinien/detail/ll/012-005.html (accessed on 5 March 2022).
- Budny, J.; Fox, J.; Rauh, M.; Fineberg, M. Emerging Trends in Anterior Cruciate Ligament Reconstruction. J. Knee Surg. 2017, 30, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Teske, W.; Anastisiadis, A.; Lichtinger, T.; von Schulze Pellengahr, C.; von Engelhardt, L.V.; Theodoridis, T. Rupture of the anterior cruciate ligament. Diagnostics and therapy. Orthopade 2010, 39, 883–898. [Google Scholar] [CrossRef] [PubMed]
- Tyler, T.F.; McHugh, M.P.; Gleim, G.W.; Nicholas, S.J. The effect of immediate weightbearing after anterior cruciate ligament reconstruction. Clin. Orthop. Relat. Res. 1998, 357, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Van Grinsven, S.; van Cingel, R.E.; Holla, C.J.; van Loon, C.J. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 1128–1144. [Google Scholar] [CrossRef] [PubMed]
- Valle, C.; Hirschmüller, A.; Schmitt-Sody, M.; Haller, B.; Keller, M.; Schoch, W.; Hoffmann, H.; Minzlaff, P. Standards in der Nachbehandlung nach vorderem Kreuzbandersatz im deutschsprachigen Raum. Sportverletz. Sportschaden 2018, 32, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Merchan, E.C. Knee Bracing after Anterior Cruciate Ligament Reconstruction. Orthopedics 2016, 39, e602–e609. [Google Scholar] [CrossRef] [PubMed]
- Wright, R.W.; Fetzer, G.B. Bracing after ACL reconstruction: A systematic review. Clin. Orthop. Relat. Res. 2007, 455, 162–168. [Google Scholar] [CrossRef]
- Tashiro, T.; Kurosawa, H.; Kawakami, A.; Hikita, A.; Fukui, N. Influence of medial hamstring tendon harvest on knee flexor strength after anterior cruciate ligament reconstruction. A detailed evaluation with comparison of single- and double-tendon harvest. Am. J. Sports Med. 2003, 31, 522–529. [Google Scholar] [CrossRef]
- Keays, S.L.; Bullock-Saxton, J.; Keays, A.C. Strength and function before and after anterior cruciate ligament reconstruction. Clin. Orthop. Relat. Res. 2000, 373, 174–183. [Google Scholar] [CrossRef]
- O’Donnell, K.; Freedman, K.B.; Tjoumakaris, F.P. Rehabilitation Protocols After Isolated Meniscal Repair: A Systematic Review. Am. J. Sports Med. 2017, 45, 1687–1697. [Google Scholar] [CrossRef]
- VanderHave, K.L.; Perkins, C.; Le, M. Weightbearing Versus Nonweightbearing After Meniscus Repair. Sports Health 2015, 7, 399–402. [Google Scholar] [CrossRef] [Green Version]
- Cavanaugh, J.T.; Killian, S.E. Rehabilitation following meniscal repair. Curr Rev. Musculoskelet. Med. 2012, 5, 46–58. [Google Scholar] [CrossRef] [Green Version]
- Mangine, R.E.; Minning, S.J.; Eifert-Mangine, M.; Colosimo, A.J.; Donlin, M. Management of the Patient with an ACL/MCL Injured Knee. N. Am. J. Sports Phys. Ther. 2008, 3, 204–211. [Google Scholar]
- Rosso, F.; Bonasia, D.E.; Cottino, U.; Cambursano, S.; Dettoni, F.; Rossi, R. Factors Affecting Subjective and Objective Outcomes and Return to Play in Anterior Cruciate Ligament Reconstruction: A Retrospective Cohort Study. Joints 2018, 6, 23–32. [Google Scholar] [CrossRef] [Green Version]
- Herbst, E.; Hoser, C.; Hildebrandt, C.; Raschner, C.; Hepperger, C.; Pointner, H.; Fink, C. Functional assessments for decision-making regarding return to sports following ACL reconstruction. Part II: Clinical application of a new test battery. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 1283–1291. [Google Scholar] [CrossRef] [Green Version]
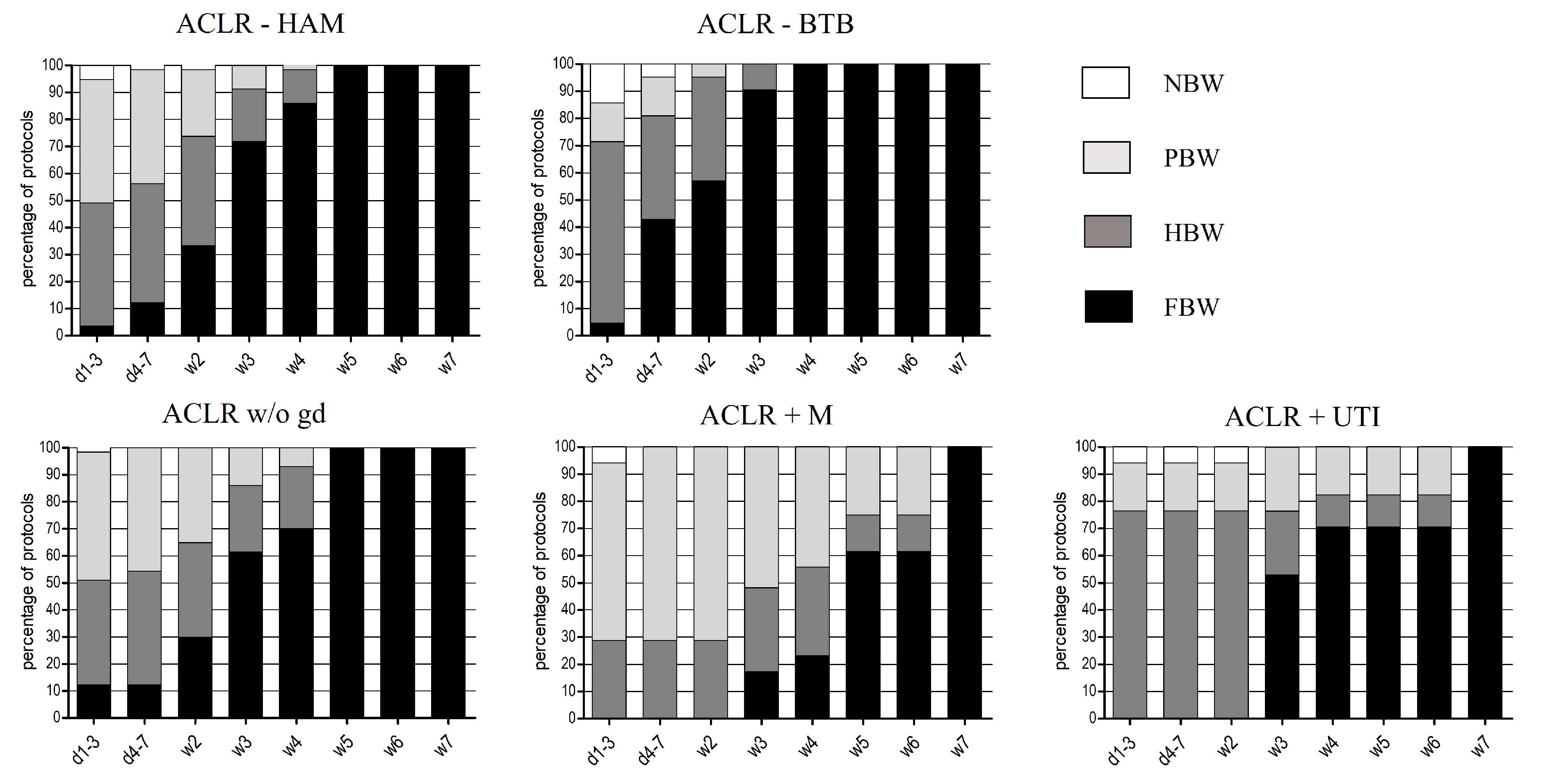




| Categories of Early Rehabilitation | |
|---|---|
| Weight bearing | no body weight (NBW) |
| partial body weight (PBW; loading up to 20 kg) | |
| half body weight (HBW; loading more than 20 kg) | |
| full body weight (FBW; unlimited loading) | |
| Range of motion (extension/flexion) | immobilization 0° |
| 0-0-30° | |
| 0-0-60° | |
| 0-0-90° | |
| free | |
| Utilization of braces | yes/no |
| recommended wearing time (weeks) | |
| Continuous passive/active motion | no CPM/CAM recommended |
| CPM recommended | |
| CAM recommended | |
| Start of rehabilitation training | weeks after surgery |
| Start of specific training | weeks after surgery |
| ACLR—Groups | |
|---|---|
| ACLR—HAM | ACLR using hamstring tendon grafts |
| ACLR—BTB | ACLR using bone–patellar tendon–bone grafts |
| ACLR—w/o gd | ACLR without graft differentiation |
| ACLR+M | ACLR with additional meniscus repair |
| ACLR+UTI | ACLR with additional meniscus and medial collateral ligament therapy |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Memmel, C.; Krutsch, W.; Szymski, D.; Pfeifer, C.; Henssler, L.; Frankewycz, B.; Angele, P.; Alt, V.; Koch, M. Current Standards of Early Rehabilitation after Anterior Cruciate Ligament Reconstruction in German Speaking Countries—Differentiation Based on Tendon Graft and Concomitant Injuries. Int. J. Environ. Res. Public Health 2022, 19, 4060. https://doi.org/10.3390/ijerph19074060
Memmel C, Krutsch W, Szymski D, Pfeifer C, Henssler L, Frankewycz B, Angele P, Alt V, Koch M. Current Standards of Early Rehabilitation after Anterior Cruciate Ligament Reconstruction in German Speaking Countries—Differentiation Based on Tendon Graft and Concomitant Injuries. International Journal of Environmental Research and Public Health. 2022; 19(7):4060. https://doi.org/10.3390/ijerph19074060
Chicago/Turabian StyleMemmel, Clemens, Werner Krutsch, Dominik Szymski, Christian Pfeifer, Leopold Henssler, Borys Frankewycz, Peter Angele, Volker Alt, and Matthias Koch. 2022. "Current Standards of Early Rehabilitation after Anterior Cruciate Ligament Reconstruction in German Speaking Countries—Differentiation Based on Tendon Graft and Concomitant Injuries" International Journal of Environmental Research and Public Health 19, no. 7: 4060. https://doi.org/10.3390/ijerph19074060






