Social Interaction, Lifestyle, and Depressive Status: Mediators in the Longitudinal Relationship between Cognitive Function and Instrumental Activities of Daily Living Disability among Older Adults
Abstract
:1. Introduction
2. Materials and Methods
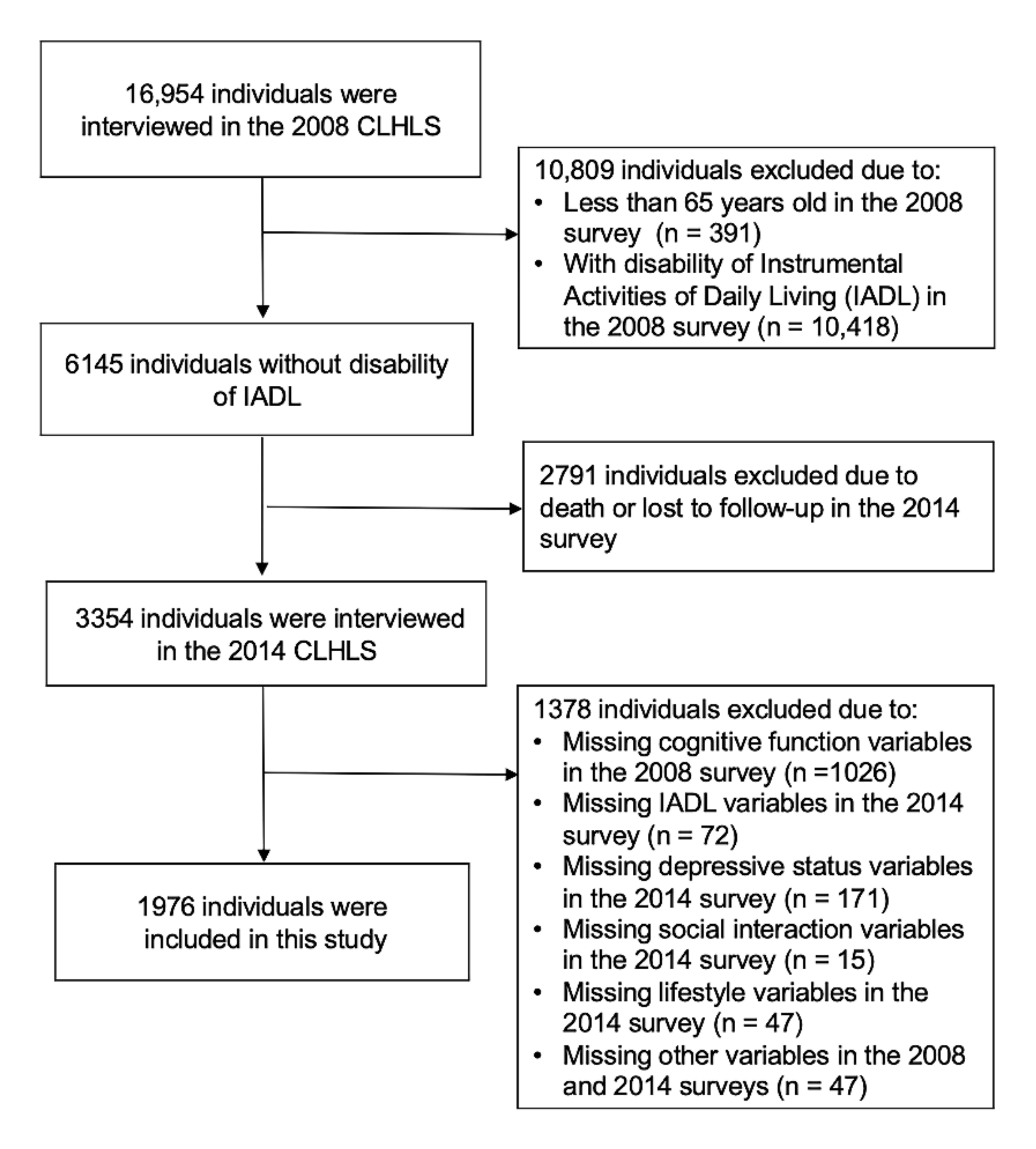
2.1. Study Population
2.2. Measurements
2.2.1. Cognitive Function
2.2.2. Instrumental Activities of Daily Living (IADL) Disability
2.2.3. Social Interaction
2.2.4. Lifestyle
2.2.5. Depressive Status
2.2.6. Covariates
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zeng, Y.; Feng, Q.; Hesketh, T.; Christensen, K.; Vaupel, J.W. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: A cohort study. Lancet 2017, 389, 1619–1629. [Google Scholar] [CrossRef]
- Stineman, M.G.; Xie, D.; Pan, Q.; Kurichi, J.E.; Saliba, D.; Streim, J. Activity of daily living staging, chronic health conditions, and perceived lack of home accessibility features for elderly people living in the community. J. Am. Geriatr. Soc. 2011, 59, 454–462. [Google Scholar] [CrossRef] [Green Version]
- Rosenthal, E.; Brennan, L.; Xie, S.; Hurtig, H.; Milber, J.; Weintraub, D.; Karlawish, J.; Siderowf, A. Association between cognition and function in patients with Parkinson disease with and without dementia. Mov. Disord. 2010, 25, 1170–1176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cahn-Weiner, D.A.; Farias, S.T.; Julian, L.; Harvey, D.J.; Kramer, J.H.; Reed, B.R.; Mungas, D.; Wetzel, M.; Chui, H. Cognitive and neuroimaging predictors of instrumental activities of daily living. J. Int. Neuropsychol. Soc. 2007, 13, 747–757. [Google Scholar] [CrossRef]
- Reppermund, S.; Brodaty, H.; Crawford, J.D.; Kochan, N.A.; Draper, B.; Slavin, M.J.; Trollor, J.N.; Sachdev, P.S. Impairment in instrumental activities of daily living with high cognitive demand is an early marker of mild cognitive impairment: The Sydney memory and ageing study. Psychol. Med. 2013, 43, 2437–2445. [Google Scholar] [CrossRef] [Green Version]
- Bailey, R.; Hillman, C.; Arent, S.; Petitpas, A. Physical activity as an investment in personal and social change: The Human Capital Model. J. Phys. Act. Health 2012, 9, 1053–1055. [Google Scholar] [CrossRef] [PubMed]
- Kotwal, A.A.; Kim, J.; Waite, L.; Dale, W. Social function and cognitive status: Results from a US nationally representative survey of older adults. J. Gen. Intern. Med. 2016, 31, 854–862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohn-Schwartz, E. Pathways from social activities to cognitive functioning: The role of physical activity and mental health. Innov. Aging 2020, 4, igaa015. [Google Scholar] [CrossRef] [PubMed]
- Mendes de Leon, C.F.; Glass, T.A.; Berkman, L.F. Social engagement and disability in a community population of older adults: The New Haven EPESE. Am. J. Epidemiol. 2003, 157, 633–642. [Google Scholar] [CrossRef]
- Bauman, A.; Merom, D.; Bull, F.C.; Buchner, D.M.; Fiatarone Singh, M.A. Updating the evidence for physical activity: Summative reviews of the epidemiological evidence, prevalence, and interventions to promote “active aging”. Gerontologist 2016, 56 (Suppl. 2), S268–S280. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Giovannucci, E.; Boffetta, P.; Fadnes, L.T.; Keum, N.; Norat, T.; Greenwood, D.C.; Riboli, E.; Vatten, L.J.; Tonstad, S. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality-a systematic review and dose-response meta-analysis of prospective studies. Int. J. Epidemiol. 2017, 46, 1029–1056. [Google Scholar] [CrossRef] [PubMed]
- Ngandu, T.; Lehtisalo, J.; Solomon, A.; Levälahti, E.; Ahtiluoto, S.; Antikainen, R.; Bäckman, L.; Hänninen, T.; Jula, A.; Laatikainen, T.; et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet 2015, 385, 2255–2263. [Google Scholar] [CrossRef]
- Ye, X.; Bhupathiraju, S.N.; Tucker, K.L. Variety in fruit and vegetable intake and cognitive function in middle-aged and older Puerto Rican adults. Br. J. Nutr. 2013, 109, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Gehlich, K.H.; Beller, J.; Lange-Asschenfeldt, B.; Köcher, W.; Meinke, M.C.; Lademann, J. Consumption of fruits and vegetables: Improved physical health, mental health, physical functioning and cognitive health in older adults from 11 European countries. Aging Ment. Health 2020, 24, 634–641. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, V.R.; Gobbo, L.A. Occupational and leisure-time physical activity decreases the odds of disability in older adults: Prospective study. Eur. J. Sport Sci. 2021, 21, 927–934. [Google Scholar] [CrossRef]
- Yu, J.; Lim, H.-Y.; Abdullah, F.N.d.o.M.; Chan, H.-M.; Mahendran, R.; Ho, R.; Kua, E.-H.; Power, M.J.; Feng, L. Directional associations between memory impairment and depressive symptoms: Data from a longitudinal sample and meta-analysis. Psychol. Med. 2018, 48, 1664–1672. [Google Scholar] [CrossRef] [PubMed]
- Wassink-Vossen, S.; Collard, R.M.; Oude Voshaar, R.C.; Comijs, H.C.; de Vocht, H.M.; Naarding, P. Physical (in)activity and depression in older people. J. Affect. Disord. 2014, 161, 65–72. [Google Scholar] [CrossRef]
- Van Gool, C.H.; Kempen, G.I.J.M.; Penninx, B.W.J.H.; Deeg, D.J.H.; Beekman, A.T.F.; van Eijk, J.T.M. Relationship between changes in depressive symptoms and unhealthy lifestyles in late middle aged and older persons: Results from the longitudinal aging study Amsterdam. Age Ageing 2003, 32, 81–87. [Google Scholar] [CrossRef] [Green Version]
- Zivin, K.; Llewellyn, D.J.; Lang, I.A.; Vijan, S.; Kabeto, M.U.; Miller, E.M.; Langa, K.M. Depression among older adults in the United States and England. Am. J. Geriatr. Psychiatry 2010, 18, 1036–1044. [Google Scholar] [CrossRef] [Green Version]
- Wu, C. The mediating and moderating effects of depressive symptoms on the prospective association between cognitive function and activities of daily living disability in older adults. Arch. Gerontol. Geriatr. 2021, 96, 104480. [Google Scholar] [CrossRef]
- Gong, B.; Wu, C. The mediating and moderating effects of depression on the relationship between cognitive function and difficulty in activities of daily living among postmenopausal women. Menopause 2021, 28, 667–677. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Y.; Vaupel, J.; Xiao, Z.; Liu, Y.; Zhang, C. Chinese Longitudinal Healthy Longevity Survey (CLHLS), 1998–2014; Inter-university Consortium for Political and Social Research: Ann Arbor, MI, USA, 2017. [Google Scholar] [CrossRef]
- Zhang, Q.; Wu, Y.; Han, T.; Liu, E. Changes in cognitive function and risk factors for cognitive impairment of the elderly in China: 2005-2014. Int. J. Environ. Res. Public Health 2019, 16, 2847. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; Xiong, Y.; Yu, Q.; Shen, S.; Chen, L.; Lei, X. The activity of daily living (ADL) subgroups and health impairment among Chinese elderly: A latent profile analysis. BMC Geriatr. 2021, 21, 30. [Google Scholar] [CrossRef] [PubMed]
- Deng, Q.; Liu, W. Physical exercise, social interaction, access to care, and community service: Mediators in the relationship between socioeconomic status and health among older patients with diabetes. Front Public Health 2020, 8, 589742. [Google Scholar] [CrossRef]
- Shi, Z.; Zhang, T.; Byles, J.; Martin, S.; Avery, J.C.; Taylor, A.W. Food habits, lifestyle factors and mortality among oldest old Chinese: The Chinese Longitudinal Healthy Longevity Survey (CLHLS). Nutrients 2015, 7, 7562–7579. [Google Scholar] [CrossRef] [Green Version]
- Shen, K.; Zhang, B.; Feng, Q. Association between tea consumption and depressive symptom among Chinese older adults. BMC Geriatr. 2019, 19, 246. [Google Scholar] [CrossRef] [Green Version]
- Zhang, H.; Wang, Z.H.; Wang, L.M.; Qi, S.G.; Li, Z.X. Study on activities of daily living disability in community-dwelling older adults in China. Chin. J. Epidemiol. 2019, 40, 266–271. [Google Scholar] [CrossRef]
- Riou, J.; Guyon, H.; Falissard, B. An introduction to the partial least squares approach to structural equation modelling: A method for exploratory psychiatric research. Int. J. Methods Psychiatr Res. 2016, 25, 220–231. [Google Scholar] [CrossRef]
- Balzi, D.; Lauretani, F.; Barchielli, A.; Ferrucci, L.; Bandinelli, S.; Buiatti, E.; Milaneschi, Y.; Guralnik, J.M. Risk factors for disability in older persons over 3-year follow-up. Age Ageing 2010, 39, 92–98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.; Kim, M.; Han, D. Incidence rates of disability and its associated factors among Korean community-dwelling older adults. Iran. J. Public Health 2020, 49, 1718–1726. [Google Scholar] [CrossRef]
- Connolly, D.; Garvey, J.; McKee, G. Factors associated with ADL/IADL disability in community dwelling older adults in the Irish longitudinal study on ageing (TILDA). Disabil. Rehabil. 2017, 39, 809–816. [Google Scholar] [CrossRef]
- Lau, K.M.; Parikh, M.; Harvey, D.J.; Huang, C.J.; Farias, S.T. Early cognitively based functional limitations predict loss of independence in instrumental activities of daily living in older adults. J. Int. Neuropsychol. Soc. 2015, 21, 688–698. [Google Scholar] [CrossRef] [Green Version]
- Diem, S.J.; Lui, L.-Y.; Langsetmo, L.; Taylor, B.; Cawthon, P.M.; Cauley, J.A.; Ensrud, K.E.; Study of Osteoporotic, F. Effects of mobility and cognition on maintenance of independence and survival among women in late life. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 1251–1257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bennett, H.P.; Corbett, A.J.; Gaden, S.; Grayson, D.A.; Kril, J.J.; Broe, G.A. Subcortical vascular disease and functional decline: A 6-year predictor study. J. Am. Geriatr. Soc. 2002, 50, 1969–1977. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.; Procter-Gray, E.; Churchill, L.; Cheng, J.; Siden, R.; Aguirre, A.; Li, W. Associations among living alone, social support and social activity in older adults. AIMS Public Health 2020, 7, 521–534. [Google Scholar] [CrossRef] [PubMed]
- Uchino, B.N.; Cacioppo, J.T.; Kiecolt-Glaser, J.K. The relationship between social support and physiological processes: A review with emphasis on underlying mechanisms and implications for health. Psychol. Bull. 1996, 119, 488–531. [Google Scholar] [CrossRef] [PubMed]
- Lindsay Smith, G.; Banting, L.; Eime, R.; O’Sullivan, G.; van Uffelen, J.G.Z. The association between social support and physical activity in older adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 56. [Google Scholar] [CrossRef] [PubMed]
- McNeill, L.H.; Wyrwich, K.W.; Brownson, R.C.; Clark, E.M.; Kreuter, M.W. Individual, social environmental, and physical environmental influences on physical activity among black and white adults: A structural equation analysis. Ann. Behav. Med. 2006, 31, 36–44. [Google Scholar] [CrossRef]
- Kanamori, S.; Kai, Y.; Kondo, K.; Hirai, H.; Ichida, Y.; Suzuki, K.; Kawachi, I. Participation in sports organizations and the prevention of functional disability in older Japanese: The AGES Cohort Study. PLoS ONE 2012, 7, e51061. [Google Scholar] [CrossRef]
- Prieto-Flores, M.-E.; Fernandez-Mayoralas, G.; Forjaz, M.J.; Rojo-Perez, F.; Martinez-Martin, P. Residential satisfaction, sense of belonging and loneliness among older adults living in the community and in care facilities. Health Place 2011, 17, 1183–1190. [Google Scholar] [CrossRef]
- Thoits, P.A. Mechanisms linking social ties and support to physical and mental health. J. Health Soc. Behav. 2011, 52, 145–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glass, T.A.; de Leon, C.M.; Marottoli, R.A.; Berkman, L.F. Population based study of social and productive activities as predictors of survival among elderly Americans. BMJ 1999, 319, 478–483. [Google Scholar] [CrossRef] [Green Version]
- Mendes de Leon, C.F.; Seeman, T.E.; Baker, D.I.; Richardson, E.D.; Tinetti, M.E. Self-efficacy, physical decline, and change in functioning in community-living elders: A prospective study. J. Gerontol. B Psychol. Sci. Soc. Sci. 1996, 51, S183–S190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, B.; Wu, Y.; Zhang, T.; Han, J.; Yu, L.; Sun, W. Effect of physical activity on independent living ability among community-dwelling elderly in urban areas of Liaoning Province in China: A population-based study. BMJ Open 2019, 9, e023543. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosenström, T.; Jokela, M. Reconsidering the definition of major depression based on collaborative psychiatric epidemiology surveys. J. Affect Disord. 2017, 207, 38–46. [Google Scholar] [CrossRef] [Green Version]
- Steger, M.F.; Kashdan, T.B. Depression and everyday social activity, belonging, and well-being. J. Couns. Psychol. 2009, 56, 289–300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hagerty, B.M.; Williams, R.A.; Coyne, J.C.; Early, M.R. Sense of belonging and indicators of social and psychological functioning. Arch. Psychiatr. Nurs. 1996, 10, 235–244. [Google Scholar] [CrossRef]
- Lenze, E.J.; Rogers, J.C.; Martire, L.M.; Mulsant, B.H.; Rollman, B.L.; Dew, M.A.; Schulz, R.; Reynolds, C.F., 3rd. The association of late-life depression and anxiety with physical disability: A review of the literature and prospectus for future research. Am. J. Geriatr. Psychiatry 2001, 9, 113–135. [Google Scholar] [CrossRef]
- Boisgontier, M.P.; Orsholits, D.; von Arx, M.; Sieber, S.; Miller, M.W.; Courvoisier, D.; Iversen, M.D.; Cullati, S.; Cheval, B. Adverse childhood experiences, depressive symptoms, functional dependence, and physical activity: A moderated mediation model. J. Phys. Act. Health 2020, 17, 790–799. [Google Scholar] [CrossRef]
- McEwen, B.S.; Sapolsky, R.M. Stress and cognitive function. Curr. Opin. Neurobiol. 1995, 5, 205–216. [Google Scholar] [CrossRef]
- Price, R.B.; Duman, R. Neuroplasticity in cognitive and psychological mechanisms of depression: An integrative model. Mol. Psychiatry 2020, 25, 530–543. [Google Scholar] [CrossRef] [PubMed]
- Schillerstrom, J.E.; Royall, D.R.; Palmer, R.F. Depression, disability and intermediate pathways: A review of longitudinal studies in elders. J. Geriatr. Psychiatry Neurol. 2008, 21, 183–197. [Google Scholar] [CrossRef] [PubMed]
- Jackson, C.A.; Jones, M.; Tooth, L.; Mishra, G.D.; Byles, J.; Dobson, A. Multimorbidity patterns are differentially associated with functional ability and decline in a longitudinal cohort of older women. Age Ageing 2015, 44, 810–816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Groot, J.C.; de Leeuw, F.E.; Oudkerk, M.; Hofman, A.; Jolles, J.; Breteler, M.M. Cerebral white matter lesions and depressive symptoms in elderly adults. Arch. Gen. Psychiatry 2000, 57, 1071–1076. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hare, D.L.; Toukhsati, S.R.; Johansson, P.; Jaarsma, T. Depression and cardiovascular disease: A clinical review. Eur. Heart J. 2013, 35, 1365–1372. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Characteristic | Total | Without IADL Disability | With IADL Disability | Statistics | |
|---|---|---|---|---|---|
| (n = 1976) | (n = 1400) | (n = 576) | t/χ2 | p-Value | |
| Sociodemographic Variables | |||||
| Age, year (SD) | 74.3 (7.4) | 72.4 (6.2) | 79.0 (7.9) | −17.896 | <0.001 |
| Gender, n (%) | 20.212 | <0.001 | |||
| Male | 1225 (62.0) | 912 (46.2) | 313 (15.8) | ||
| Female | 751 (38.2) | 488 (24.7) | 263 (13.3) | ||
| Education, year (SD) | 4.0 (4.0) | 4.5 (4.1) | 2.9 (3.5) | 8.630 | <0.001 |
| Region of residence, n (%) | 0.039 | 0.844 | |||
| Urban | 255 (12.9) | 182 (9.2) | 73 (3.7) | ||
| Rural | 1721 (87.1) | 1218 (61.6) | 503 (25.5) | ||
| Marital status, n (%) | 49.416 | <0.001 | |||
| Married and living with a spouse | 1295 (65.5) | 985 (49.8) | 310 (15.7) | ||
| Others | 681 (34.5) | 415 (21.0) | 266 (13.5) | ||
| Occupation, n (%) | 9.346 | 0.009 | |||
| Manual worker | 1633 (82.6) | 1136 (57.5) | 497 (25.2) | ||
| Nonmanual worker | 295 (14.9) | 231 (11.7) | 64 (3.2) | ||
| Others | 48 (2.4) | 33 (1.7) | 15 (0.8) | ||
| HI/year, thousand yuan (SD) | 19.5 (22.2) | 19.4 (21.7) | 19.6 (23.5) | −0.169 | 0.866 |
| MC/year, thousand yuan (SD) | 3.4 (13.5) | 3.4 (13.8) | 3.2 (12.7) | 0.341 | 0.733 |
| Social interaction (SD) | 3.3 (1.9) | 3.6 (2.0) | 2.6 (1.3) | 12.141 | <0.001 |
| Play cards and/or mah-jong | 1.8 (1.4) | 2.0 (1.5) | 1.4 (1.0) | 9.999 | <0.001 |
| Organized social activities | 1.5 (1.1) | 1.6 (1.2) | 1.3 (0.8) | 7.595 | <0.001 |
| Health-Related Variables | |||||
| Drinking at present (2008), n (%) | 545 (27.6) | 417 (21.1) | 128 (6.5) | 11.688 | 0.001 |
| Smoking at present (2008), n (%) | 572 (28.9) | 443 (22.4) | 129 (6.5) | 16.966 | <0.001 |
| Exercise at present (2008), n (%) | 891 (45.1) | 628 (31.8) | 263 (13.3) | 0.106 | 0.745 |
| Self-reported Health, n (%) | 0.171 | 0.918 | |||
| Good | 1177 (59.6) | 838 (42.4) | 339 (17.2) | ||
| Fair | 607 (30.7) | 427 (21.6) | 180 (9.1) | ||
| Poor | 192 (9.7) | 135 (6.8) | 57 (2.9) | ||
| Self-reported quality of life, n (%) | 5.545 | 0.063 | |||
| Good | 1200 (60.7) | 831 (42.1) | 369 (18.7) | ||
| Fair | 697 (35.3) | 506 (25.6) | 191 (9.7) | ||
| Poor | 79 (4.0) | 63 (3.2) | 16 (0.8) | ||
| Night sleep duration, hour (SD) | 7.6 (1.9) | 7.5 (1.8) | 7.7 (1.9) | −1.866 | 0.062 |
| Self-reported sleep quality, n (%) | 0.665 | 0.717 | |||
| Good | 1389 (70.3) | 978 (49.5) | 411 (20.8) | ||
| Fair | 393 (19.9) | 285 (14.4) | 108 (5.5) | ||
| Poor | 194 (9.8) | 137 (6.9) | 57 (2.9) | ||
| Body mass index, kg/m2 (SD) | 21.8 (3.6) | 21.9 (3.6) | 21.5 (3.5) | 2.706 | 0.007 |
| Chronic diseases, n (%) | |||||
| Hypertension | 457 (23.1) | 308 (15.6) | 149 (7.5) | 3.434 | 0.064 |
| Diabetes | 66 (3.3) | 50 (2.5) | 16 (0.8) | 0.796 | 0.372 |
| Heart disease | 208 (10.5) | 144 (7.3) | 64 (3.2) | 0.295 | 0.587 |
| Global cognitive function (SD) | 28.4 (2.3) | 28.6 (2.0) | 27.8 (2.7) | 6.553 | <0.001 |
| Orientation | 11.6 (1.0) | 11.7 (0.9) | 11.5 (1.1) | 2.859 | 0.004 |
| Memory | 5.5 (1.0) | 5.6 (0.9) | 5.4 (1.2) | 4.288 | <0.001 |
| Attention and calculation | 5.4 (1.0) | 5.5 (0.9) | 5.1 (1.2) | 7.034 | <0.001 |
| Language | 5.9 (0.4) | 5.9 (0.4) | 5.9 (0.4) | 2.306 | 0.021 |
| Depressive status (SD) | 10.8 (3.4) | 10.3 (3.3) | 11.9 (3.5) | −9.690 | <0.001 |
| Lifestyle, score (SD) | 1.8 (0.8) | 1.9 (0.8) | 1.7 (0.8) | 6.041 | <0.001 |
| Fruit, n (%) | 902 (45.6) | 655 (33.1) | 247 (12.5) | 2.507 | 0.113 |
| Vegetable, n (%) | 1838 (93.0) | 1221 (67.4) | 507 (25.7) | 31.229 | <0.001 |
| Exercise, n (%) | 880 (44.5) | 680 (34.4) | 200 (10.1) | 31.688 | <0.001 |
| Variables | Standardized Estimate | Standard Errors | LLCI | ULCI | p | Ratio |
|---|---|---|---|---|---|---|
| Direct effect on IADL | ||||||
| Cognitive function | −0.007 | 0.072 | −0.124 | 0.147 | 0.885 | - |
| Indirect effect | ||||||
| Social interaction (a1 × b1) | −0.095 | 0.045 | −0.183 | −0.007 | <0.001 | 46.34% |
| Lifestyle (a2 × b2) | −0.086 | 0.042 | −0.168 | −0.004 | <0.001 | 41.95% |
| Depressive status (a3 × b3) | −0.017 | 0.007 | −0.032 | −0.003 | 0.003 | 8.29% |
| Total effect | −0.205 | 0.039 | −0.282 | −0.128 | <0.001 | - |
| Difference of indirect effects | ||||||
| a1 × b1 − 2 × b2 | −0.008 | 0.055 | −0.115 | 0.098 | 0.875 | - |
| a1 × b1 − a3 × b3 | −0.077 | 0.043 | −0.162 | 0.007 | <0.001 | - |
| a2 × b2 − a3 ×b3 | −0.069 | 0.041 | −0.149 | 0.011 | 0.013 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Q.; Wu, C. Social Interaction, Lifestyle, and Depressive Status: Mediators in the Longitudinal Relationship between Cognitive Function and Instrumental Activities of Daily Living Disability among Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 4235. https://doi.org/10.3390/ijerph19074235
Li Q, Wu C. Social Interaction, Lifestyle, and Depressive Status: Mediators in the Longitudinal Relationship between Cognitive Function and Instrumental Activities of Daily Living Disability among Older Adults. International Journal of Environmental Research and Public Health. 2022; 19(7):4235. https://doi.org/10.3390/ijerph19074235
Chicago/Turabian StyleLi, Qiuhong, and Chao Wu. 2022. "Social Interaction, Lifestyle, and Depressive Status: Mediators in the Longitudinal Relationship between Cognitive Function and Instrumental Activities of Daily Living Disability among Older Adults" International Journal of Environmental Research and Public Health 19, no. 7: 4235. https://doi.org/10.3390/ijerph19074235







