Implementation of a Psychiatric Consultation for Healthcare Workers during First Wave of COVID-19 Outbreak
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Interventions
2.3. Materials
2.4. Data Analysis
2.4.1. Quantitative Analysis
2.4.2. Qualitative Analysis
3. Results
3.1. CovidPsy Consultation Activity
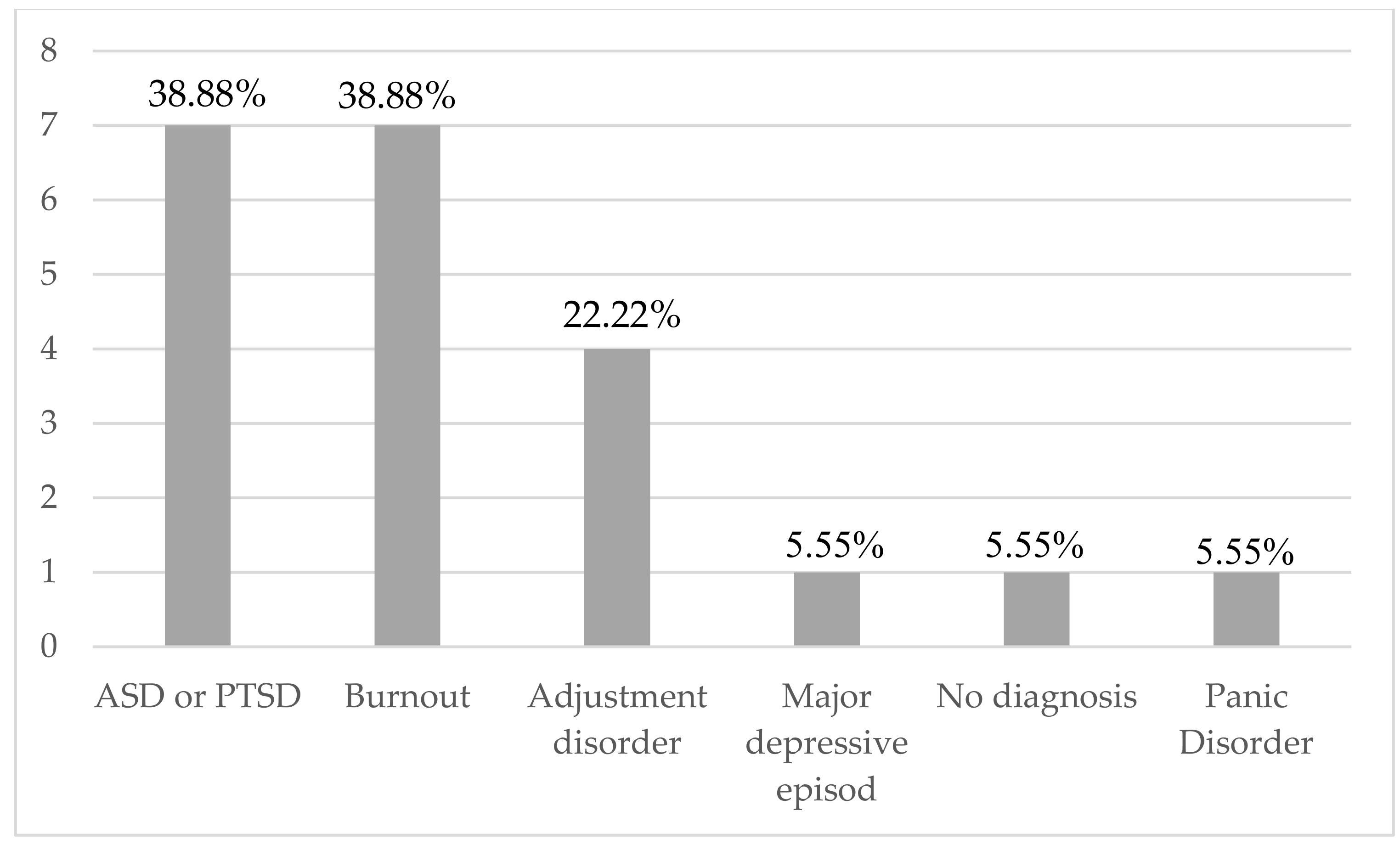
3.1.1. Quantitative Analysis of Clinical Data
3.1.2. Qualitative Analysis of Clinical Data: Difficulties and Stress Factors during the First Wave of the COVID-19 Pandemic
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- John Hopkins University of Medicine. Coronavirus Ressource Center. Available online: https://coronavirus.jhu.edu/map.html (accessed on 17 May 2021).
- Office Fédéral de la Santé Publique. Cas Confirmés en Laboratoire. Available online: https://www.covid19.admin.ch/fr/epidemiologic/case (accessed on 17 May 2021).
- World Health Organization. Interim Briefing Note—Taking into Account the Psychosocial and Mental Health Aspects of the COVID-19 Epidemic. 2020. Available online: https://interagencystandingcommittee.org/iasc-referencegroup-mental-health-and-psychosocial-support-emergency-settings/interim-briefing (accessed on 17 March 2020).
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Batra, K.; Singh, T.P.; Sharma, M.; Batra, R.; Schvaneveldt, N. Investigating the Psychological Impact of COVID-19 among Healthcare Workers: A Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 9096. [Google Scholar] [CrossRef] [PubMed]
- Carmassi, C.; Foghi, C.; Dell’Oste, V.; Cordone, A.; Bertelloni, C.A.; Bui, E.; Dell’Osso, L. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: What can we expect after the COVID-19 pandemic. Psychiatry Res. 2020, 292, 113312. [Google Scholar] [CrossRef] [PubMed]
- Maves, R.C.; Downar, J.; Dichter, J.R.; Hick, J.L.; Devereaux, A.; Geiling, J.A.; Kissoon, N.; Hupert, N.; Niven, A.S.; King, M.A.; et al. Triage of Scarce Critical Care Resources in COVID-19 An Implementation Guide for Regional Allocation: An Expert Panel Report of the Task Force for Mass Critical Care and the American College of Chest Physicians. Chest 2020, 158, 212–225. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef] [Green Version]
- Rotenstein, L.S.; Torre, M.; Ramos, M.A.; Rosales, R.C.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA 2018, 320, 1131–1150. [Google Scholar] [CrossRef] [Green Version]
- West, C.P.; Dyrbye, L.N.; Shanafelt, T.D. Physician burnout: Contributors, consequences and solutions. J. Intern. Med. 2018, 283, 516–529. [Google Scholar] [CrossRef] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Brewin, C.R.; Andrews, B.; Valentine, J.D. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J. Consult. Clin. Psychol. 2000, 68, 748–766. [Google Scholar] [CrossRef]
- Bai, Y.; Lin, C.C.; Lin, C.Y.; Chen, J.Y.; Chue, C.M.; Chou, P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr. Serv. 2004, 55, 1055–1057. [Google Scholar] [CrossRef]
- Watson, P. PTSD as a Public Mental Health Priority. Curr. Psychiatry Rep. 2019, 21, 61. [Google Scholar] [CrossRef]
- Qi, W.; Gevonden, M.; Shalev, A. Prevention of Post-Traumatic Stress Disorder After Trauma: Current Evidence and Future Directions. Curr. Psychiatry Rep. 2016, 18, 20. [Google Scholar] [CrossRef] [Green Version]
- Roberts, N.P.; Kitchiner, N.J.; Kenardy, J.; Lewis, C.E.; Bisson, J.I. Early psychological intervention following recent trauma: A systematic review and meta-analysis. Eur. J. Psychotraumatol. 2019, 10, 1695486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brooks, S.; Amlôt, R.; Rubin, G.J.; Greenberg, N. Psychological resilience and post-traumatic growth in disaster-exposed organisations: Overview of the literature. BMJ Mil Health 2020, 166, 52–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Support Based on Psychological First Aid Principles in People Recently Exposed to a Traumatic Event. In WHO mhGAP Action Programme; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Norwood, A.E.; Ursano, R.J.; Fullerton, C.S. Disaster psychiatry: Principles and practice. Psychiatr. Q. 2000, 71, 207–226. [Google Scholar] [CrossRef] [PubMed]
- Nussbaum, A. The Pocket Guide to the DSM-5TM Diagnostic Exam; American Psychiatric Publishing Inc.: Arlinghton, VA, USA, 2013. [Google Scholar]
- Maslach. Burnout Inventory Manual, 2nd ed.; Consulting Psychologists Press: Palo Alto, CA, USA, 1986. [Google Scholar]
- Faye-Dumanget, C.; Carré, J.; Le Borgne, M.; Boudoukha, P.A.H. French validation of the Maslach Burnout Inventory-Student Survey (MBI-SS). J. Eval. Clin. Pract. 2017, 23, 1247. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Brunet, A.; Weiss, D.S.; Metzler, T.J.; Best, S.R.; Neylan, T.C.; Rogers, C.; Fagan, J.; Marmar, C.R. The Peritraumatic Distress Inventory: A proposed Measure of PTSD criterion A2. Am. J. Psychiatry 2001, 158, 1480–1485. [Google Scholar] [CrossRef] [Green Version]
- Jehel, L.; Brunet, A.; Paterniti, S.; Guelfi, J.D. Validation of the French version of the Peritraumatic Distress Inventory. Can. J. Psychiatry 2005, 50, 67–71. [Google Scholar] [CrossRef] [Green Version]
- Marmar, C.R.; Weiss, D.S.; Metzler, T.J. The Peritraumatic Dissociative Experiences Questionnaire. In Assessing Psychological Trauma and Posttraumatic Stress Disorder; Wilson, J.P., Marmar, C.R., Eds.; The Guilford Press: New York, NY, USA, 1997; pp. 412–428. [Google Scholar]
- Birmes, P.; Brunet, A.; Benoit, M.; Defer, S.; Hatton, L.; Sztulman, H.; Schmitt, L. Validation of the Peritraumatic Dissociative Experiences Questionnaire self-report version in two samples of French-speaking individuals exposed to trauma. Eur. Psychiatry 2005, 20, 145–151. [Google Scholar] [CrossRef]
- Ashbaugh, A.R.; Houle-Johnson, S.; Herbert, C.; El-Hage, W.; Brunet, A. Psychometric Validation of the English and French Versions of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5). PLoS ONE 2016, 11, e0161645. [Google Scholar] [CrossRef]
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD Checklist for DSM-5 (PCL-5). 2013. Available online: www.ptsd.va.gov (accessed on 19 May 2021).
- Hsieh, H.-F.; Shannon, S.E. Three Approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Di Tella, M.; Romeo, A.; Benfante, A.; Castelli, L. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J. Eval. Clin. Pract. 2020, 26, 1583–1587. [Google Scholar] [CrossRef] [PubMed]
- Simione, L.; Gnagnarella, C. Differences between health workers and general population in risk perception, behaviors, and psychological distress related to COVID-19 spread in Italy. Front. Psychol. 2020, 11, 2166. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Palamenghi, L.; Graffigna, G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020, 290, 113129. [Google Scholar] [CrossRef] [PubMed]
- Geoffroy, P.A.; Le Goanvic, V.; Sabbagh, O.; Richoux, C.; Weinstein, A.; Dufayet, G.; Lejoyeux, M. Psychological Support System for Hospital Workers during the COVID-19 Outbreak: Rapid Design and Implementation of the COVID-Psy Hotline. Front. Psychiatry 2020, 11, 511. [Google Scholar] [CrossRef] [PubMed]
- Rolling, J.; Mengin, A.C.; Palacio, C.; Mastelli, D.; Fath, M.; Gras, A.; Von Hunolstein, J.J.; Schröder, C.M.; Vidailhet, P. COVID-19: Mental Health Prevention and Care for Healthcare Professionals. Front. Psychiatry 2021, 12, 566740. [Google Scholar] [CrossRef] [PubMed]
- Belli, S.; Alonso, C. COVID-19 pandemic and emotional contagion. Digithum 2021, 27, 1–9. [Google Scholar] [CrossRef]
- Rebughini, P. A sociology of anxiety: Western modern legacy and the COVID-19 outbreak. Int. Sociol. 2021, 36, 554–568. [Google Scholar] [CrossRef]
- Substances Abuses and Mental Health Services Administration. Phases of Disaster. Available online: https://www.samhsa.gov/dtac/recovering-disasters/phases-disaster (accessed on 17 May 2021).

| Total (N = 18); N(%) | |
|---|---|
| Socio-Demographic Characteristics | |
| Age (mean, min-max) | 40,67; [25–58] |
| Gender | |
| - Female | 14 (77.78) |
| - Male | 4 (22.22) |
| Profession | |
| - Physician | 2 (11.11) |
| - Nurse | 9 (50) |
| - Medical student | 2 (11.11) |
| - Other healthcare worker | 4 (22.22) |
| - Administrative hospital staff | 1 (5.55) |
| Marital status | |
| - Single | 3 (16.67) |
| - Married or living as a couple | 15 (83.33) |
| Entourage support | |
| - Yes | 15 (83.33) |
| - No | 3 (16.67) |
| Working in COVID-19 ward | |
| - Yes | 13 (72.22) |
| - No | 5 (27.78) |
| Clinical data | |
| Medical history | |
| - Yes | 8 (44.44) |
| - No | 7 (55.56) |
| Psychiatric history | |
| - Yes | 7 (38.89) |
| - No | 11 (61.11) |
| - No information | |
| Current psychotropic medication | |
| - Yes | 2 (11.11) |
| - No | 16 (88.89) |
| Trauma history | |
| - Yes | 9 (50) |
| - No | 9 (50) |
| SARS-CoV-2 contamination | |
| - Yes | 4 (22.22) |
| - No | 14 (77.78) |
| Medical risk factors for severe COVID-19 form * | |
| - Yes | 2 (11.11) |
| - No | 16 (88.89) |
| Number of sessions by healthcare worker (HCW) | µ = 2.68; [−1; 11] |
| Characteristics of the follow-up | |
| Duration of consultation | µ = 89 min (45–150 min) |
| Referral to a psychiatrist or a psychologist follow-up | |
| - Yes | 5 (27.78) |
| - No | 13 (72.22) |
| Sick leave | |
| - Yes | 7 (38.89) |
| - No | 11 (61.11) |
| Prescription of a psychotropic medication in the context of CovidPsy consultation | |
| - Anxiolytic medication | 11 (61.11) |
| - Antidepressant medication | 2 (11.11) |
| - No psychotropic prescription | 7 (38.89) |
| PDEQ (n = 14) | |
|---|---|
| PDEQ score (mean, min-max) | 21.85 (9–39) |
| - Positive PDEQ (N, %)) | 11 (78.57) |
| - PDI (n = 14) | |
| PDI score (mean, min-max) | 28.14 (1–51) |
| - Positive PDI (N,%) | 11 (78.57) |
| - PCL-5 (n = 4) | |
| Positive PCL-5 (N, %) | 4 (100) |
| - PCL-5 (mean, min-max) | 30 (33–47) |
| - HADS-A (n = 16) | |
| Positive HADS-A (N, %) | 11 (68.75) |
| - HADS-A (mean, min-max) | 13.25 (6–20) |
| - HADS-D (n = 16) | |
| Positive HADS-D (N, %) | 5 (31.25) |
| - HADS-D (mean, min-max) | 8.31 (1–16) |
| - MBI-HSS (n = 17) | |
| MBI-EE (N, %) | |
| - Low level (sub-score ≤ 21) (N, %) | 7 (41.8) |
| ◦ Moderate (21 < sub-score ≤ 32) | 6 (35.29) |
| ◦ High level (sub-score > 32) | 4 (23.53) |
| ◦ MBI-DP (N, %) | |
| - Low level (sub-score ≤ 6) | 10 (58.82) |
| ◦ Moderate (21 < sub-score ≤ 12) | 3 (17.65) |
| ◦ High level (>12) | 4 (23.53) |
| ◦ MBI-PA (N, %) | |
| - Low level (sub-score ≤ 22) | 2 (11.76) |
| ◦ Moderate (22 < sub-score ≤ 32) | 6 (35.29) |
| ◦ High level (sub-score > 32) | 9 (52.94) |
| Perceived Difficulties at Work in Link with COVID-19 Outbreak (N = 18) | N(%) |
|---|---|
| Traumatic stressors | |
| - Fear of contamination at work | 7 (38.89) |
| - Feeling insecure | 6 (33.33) |
| - Multiple deaths of patients | 9 (50) |
| - Feeling of guilty | 2 (11.11) |
| Work related stress | |
| - Work change imposed by the COVID-19 context | 8 (44.44) |
| - Lack of recognition | 5 (27.78) |
| - Feeling abandoned by hierarchy | 9 (50) |
| - Feeling of incompetence | 4 (22.22) |
| - Conflict of values | 2 (11.11) |
| - Feeling of failure | 2 (11.11) |
| - Isolation | 6 (33.33) |
| - No perceived support by the hierarchy | 3 (16.67) |
| MBI−EE | MBI−DP | |
|---|---|---|
| Lack of recognitiong | 0.94; [−17.26; 16.26] | 0.001 **; [−30.57; −9.10] |
| Conflict of values | 0.02 *; [4.08; 37.05] | 0.0009 ***; [−23.94; −7.59] |
| Feelings of incompetence | 0.02 *; [3.07; 29.10] | 0.25; [−14.13; 3.97] |
| Feelings of abandonment | 0.62; [−10.58; 17.02] | 0.96; [−7.53; 7.86] |
| Difficulties with service change | 0.19; [−5.55; 25.51] | 1; [−12.18; 12.18] |
| Feelings of isolation | 0.94; [−14.6372; 13.6372] | 0.62; [−10.36; 6.36] |
| No perceived support by hierarchy | 0.07; [−28.89; 1.32] | 0.62; [−10.36; 6.36] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benzakour, L.; Langlois, G.; Marini, V.; Groz, A.; Chiabotto, C.; Apetrei, D.; Corneau, B.; Bondolfi, G. Implementation of a Psychiatric Consultation for Healthcare Workers during First Wave of COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2022, 19, 4780. https://doi.org/10.3390/ijerph19084780
Benzakour L, Langlois G, Marini V, Groz A, Chiabotto C, Apetrei D, Corneau B, Bondolfi G. Implementation of a Psychiatric Consultation for Healthcare Workers during First Wave of COVID-19 Outbreak. International Journal of Environmental Research and Public Health. 2022; 19(8):4780. https://doi.org/10.3390/ijerph19084780
Chicago/Turabian StyleBenzakour, Lamyae, Gérard Langlois, Verena Marini, Alexandra Groz, Chiara Chiabotto, Diana Apetrei, Bruno Corneau, and Guido Bondolfi. 2022. "Implementation of a Psychiatric Consultation for Healthcare Workers during First Wave of COVID-19 Outbreak" International Journal of Environmental Research and Public Health 19, no. 8: 4780. https://doi.org/10.3390/ijerph19084780
APA StyleBenzakour, L., Langlois, G., Marini, V., Groz, A., Chiabotto, C., Apetrei, D., Corneau, B., & Bondolfi, G. (2022). Implementation of a Psychiatric Consultation for Healthcare Workers during First Wave of COVID-19 Outbreak. International Journal of Environmental Research and Public Health, 19(8), 4780. https://doi.org/10.3390/ijerph19084780








