One Word to Describe My Experience as a COVID-19 Survivor Six Months after Its Onset: Findings of a Qualitative Study
Abstract
:1. Introduction
Background
2. Materials and Methods
2.1. Study Design
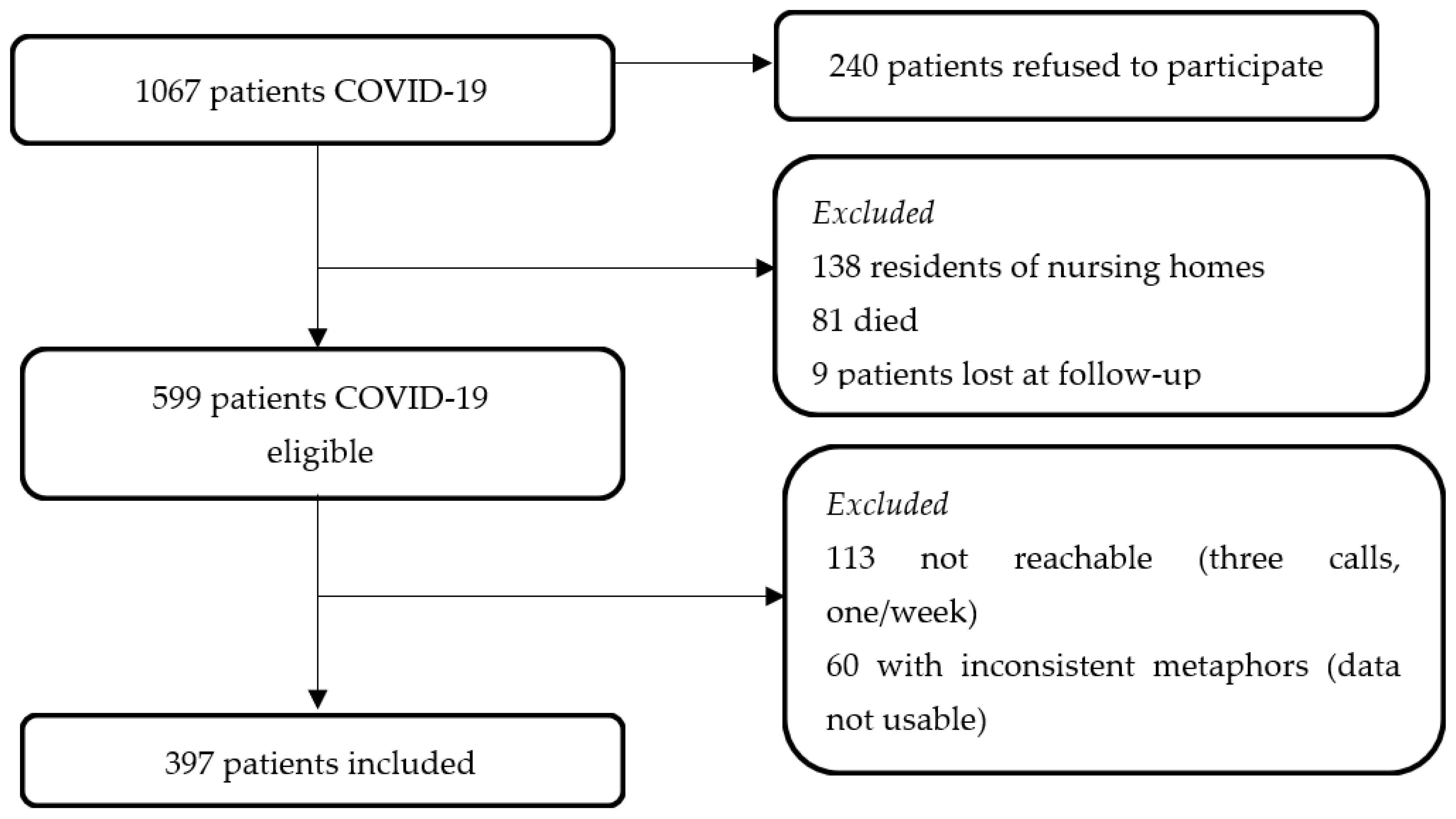
2.2. Setting and Participants
2.3. Data Collection Instrument and Method
2.4. Data Collection Rigour
2.5. Data Analysis
- (a)
- Selected: For those patients who expressed more than one metaphor, one was identified according to its intensity and capacity to condense the meaning of the whole experience.
- (b)
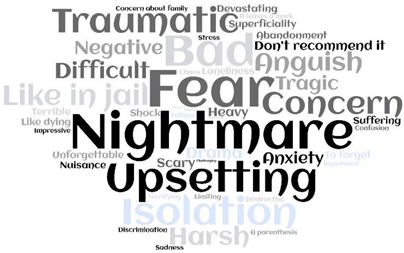
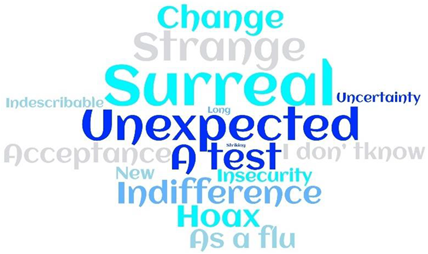
- Summarised: All metaphors were summarised in a single word expressing the ‘metaphor vehicle’ as the prototypical example of a given category [31]. A content analysis of each metaphor [37] was performed and then compared with each other. Their metaphorical qualities were checked; while some maintained their structure (e.g., ‘Nightmare’), others expressed mainly a process (e.g., ‘Rethinking’) or a feeling (e.g., ‘Fear’ or ‘Concern’). However, given that all the expressions that emerged reflected how patients categorise and make sense of their lived experience(s), all were retained as being able to express the quality required by the metaphors [31].
- (c)
- Categorised [35]: All were categorised into their emotional orientation (positive, neutral, or negative) according to the context of the expression reported by each participant.
- (d)
- Analysed: A corroborative counting technique was performed [38] using a free web program [39] considering the metaphor orientation (positive, negative, and neutral). Specifically, we used a free Word Cloud analysis to detect the frequency of the metaphors according to their orientation. This method identifies the most common words found in a data set and displays them in a cloud where the frequency of the methods (in our case) is indicated by the size of the font used to display the word [40]. Then, a descriptive analysis of the metaphors according to their orientation was performed [41]. Furthermore, a comparison within the same metaphor orientation was conducted across the different main characteristics of the patients using the chi-square test (χ2) for dichotomous variables. The statistical differences were set at p < 0.05. Data were analysed with SPSS version 26. The entire process was performed for all the metaphors expressed in an independent fashion by the three researchers; then, they agreed upon the findings to ensure an investigator triangulation of the data analysis [42].
3. Results
3.1. Participants
3.2. Metaphors
4. Discussion
4.1. Patients
4.2. Metaphors
4.3. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Del Rio, C.; Collins, L.F.; Malani, P. Long-term health consequences of COVID-19. JAMA 2020, 324, 1723–1724. [Google Scholar] [CrossRef] [PubMed]
- Dong, L.; Bouey, J. Public mental health crisis during COVID-19 pandemic, China. Emerg. Infect. Dis. 2020, 26, 1616. [Google Scholar] [CrossRef] [PubMed]
- Shaban, R.Z.; Nahidi, S.; Sotomayor-Castillo, C.; Li, C.; Gilroy, N.; O’Sullivan, M.V.; .Bag, S. SARS-CoV-2 infection and COVID-19: The lived experience and perceptions of patients in isolation and care in an Australian healthcare setting. Am. J. Infect. Control 2020, 48, 1445–1450. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, S.; Mehra, A.; Suri, V.; Malhotra, P.; Yaddanapudi, L.N.; Puri, G.D.; Grover, S. Lived experiences of the corona survivors (patients admitted in COVID wards): A narrative real-life documented summaries of internalized guilt, shame, stigma, anger. Asian J. Psychiatry 2020, 53, 102187. [Google Scholar] [CrossRef] [PubMed]
- Bryson, W.J. Long-term health-related quality of life concerns related to the COVID-19 pandemic: A call to action. Qual. Life Res. 2021, 30, 643–645. [Google Scholar] [CrossRef] [PubMed]
- Peghin, M.; Palese, A.; Venturini, M.; De Martino, M.; Gerussi, V.; Graziano, E.; Bontempo, G.; Marrella, F.; Tommasini, A.; Fabris, M.; et al. Post-COVID-19 symptoms 6 months after acute infection among hospitalized and non-hospitalized patients. Clin. Microbiol. Infect. 2021, 27, 1507–1513. [Google Scholar] [CrossRef] [PubMed]
- Amdal, C.D.; Pe, M.; Falk, R.S.; Piccinin, C.; Bottomley, A.; Arraras, J.I.; Darlington, A.S.; Hofsø, K.; Holzner, B.; Jørgensen, N.; et al. Health-related quality of life issues, including symptoms, in patients with active COVID-19 or post COVID-19; a systematic literature review. Qual. Life Res. 2021, 30, 3367–3381. [Google Scholar] [CrossRef]
- Sun, N.; Wei, L.; Wang, H.; Wang, X.; Gao, M.; Hu, X.; Shi, S. Qualitative study of the psychological experience of COVID-19 patients during hospitalization. J. Affect. Disord. 2021, 278, 15–22. [Google Scholar] [CrossRef]
- Wang, J.Y.; Wei, L.L.; Li, H.T.; Zhang, Y.; Li, Q.Q.; Pan, Y.S.; Wei, H. A qualitative exploration of the psychological experience of patients hospitalized with COVID-19. Holist. Nurs. Pract. 2022, 36, 37–45. [Google Scholar] [CrossRef]
- Weerahandi, H.; Hochman, K.A.; Simon, E.; Blaum, C.; Chodosh, J.; Duan, E.; Garry, K.; Kahan, T.; Karmen-Tuohy, S.L.; Karpel, H.C.; et al. Post-discharge health status and symptoms in patients with severe COVID-19. J. Gen. Intern. Med. 2021, 36, 738–745. [Google Scholar] [CrossRef]
- Gamberini, L.; Mazzoli, C.A.; Sintonen, H.; Colombo, D.; Scaramuzzo, G.; Allegri, D.; Tonetti, T.; Zani, G.; Capozzi, C.; ICU-RER COVID-19 Collaboration; et al. Quality of life of COVID-19 critically ill survivors after ICU discharge: 90 days follow-up. Qual. Life Res. 2021, 30, 2805–2817. [Google Scholar] [CrossRef] [PubMed]
- Carfì, A.; Bernabei, R.; Landi, F. Persistent symptoms in patients after acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Kingstone, T.; Taylor, A.K.; O’Donnell, C.A.; Atherton, H.; Blane, D.N.; Chew-Graham, C.A. Finding the ‘right’ GP: A qualitative study of the experiences of people with long-COVID. BJGP Open 2020, 4, bjgpopen20X101143. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Hu, Y.; Xia, L.; Wen, L.; Ren, W.; Xia, W.; Chen, L. Psychological experience of patients with confirmed COVID-19 at the initial stage of pandemic in Wuhan, China: A qualitative study. BMC Public Health 2021, 21, 2257. [Google Scholar] [CrossRef]
- Kingsley, C.; Patel, S. Patient-reported outcome measures and patient-reported experience measures. BJA Educ. 2017, 17, 137–144. [Google Scholar] [CrossRef] [Green Version]
- Manary, M.P.; Boulding, W.; Staelin, R.; Glickman, S.W. The patient experience and health outcomes. N. Engl. J. Med. 2013, 368, 201–203. [Google Scholar] [CrossRef] [Green Version]
- Evans, S.; Mikocka-Walus, A.; Klas, A.; Olive, L.; Sciberras, E.; Karantzas, G.; Westrupp, E.M. From ‘It has stopped our lives’ to ‘Spending more time together has strengthened bonds’: The varied experiences of Australian families during COVID-19. Front. Psychol. 2020, 11, 2906. [Google Scholar] [CrossRef]
- Tan, R.; Yu, T.; Luo, K.; Teng, F.; Liu, Y.; Luo, J.; Hu, D. Experiences of clinical first-line nurses treating patients with COVID-19: A qualitative study. J. Nurs. Manag. 2020, 28, 1381–1390. [Google Scholar] [CrossRef]
- Sun, N.; Wei, L.; Shi, S.; Jiao, D.; Song, R.; Ma, L.; Wang, H. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am. J. Infect. Control 2020, 48, 592–598. [Google Scholar] [CrossRef]
- Suhail, A.; Iqbal, N.; Smith, J. Lived experiences of Indian Youth amid COVID-19 crisis: An interpretative phenomenological analysis. Int. J. Soc. Psychiatry 2020, 67, 559–566. [Google Scholar] [CrossRef]
- Jakovljevic, M.; Bjedov, S.; Jaksic, N.; Jakovljevic, I. COVID-19 pandemia and public and global mental health from the perspective of global health security. Psychiatr. Danub. 2020, 32, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, H.; Ortiz-Ospina, E.; Beltekian, D.; Mathieu, E.; Hasell, J.; Macdonald, B.; Giattino, C.; Appel, C.; Rodés-Guirao, L.; Roser, M. Coronavirus Pandemic (COVID-19). Available online: https://ourworldindata.org/coronavirus (accessed on 6 June 2021).
- Liu, N.; Zhang, F.; Wei, C.; Jia, Y.; Shang, Z.; Sun, L.; Wu, L.; Sun, Z.; Zhou, Y.; Wang, Y.; et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020, 287, 112921. [Google Scholar] [CrossRef] [PubMed]
- Sandelowski, M. Whatever happened to qualitative description? Res. Nurs. Health 2000, 23, 334–340. [Google Scholar] [CrossRef]
- O’Brien, B.C.; Harris, I.B.; Beckman, T.J.; Reed, D.A.; Cook, D.A. Standards for reporting qualitative research: A synthesis of recommendations. Acad. Med. 2014, 89, 1245–1251. [Google Scholar] [CrossRef]
- Stanley, B.L.; Zanin, A.C.; Avalos, B.L.; Tracy, S.J.; Town, S. Collective emotion during collective trauma: A metaphor analysis of the COVID-19 pandemic. Qual. Health Res. 2021, 31, 1890–1903. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Clinical Management of COVID-19: Interim Guidance, 25 January 2021 (No. WHO/2019-nCoV/clinical/2021.1). Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1 (accessed on 21 December 2021).
- Schmier, J.K.; Halpern, M.T.; Higashi, M.K.; Bakst, A. The quality of life impact of acute exacerbations of chronic bronchitis (AECB): A literature review. Qual. Life Res. 2005, 14, 329–347. [Google Scholar] [CrossRef]
- Lakoff, G.; Johnson, M. Metaphors We Live By; University of Chicago Press: Chicago, IL, USA, 1980. [Google Scholar]
- Miles, M.B.; Huberman, A.M. Qualitative Data Analysis: An Expanded Source Book, 2nd ed.; Sage: Beverly Hills, CA, USA, 1994. [Google Scholar]
- Gibbs, R.W. Categorization and metaphor understanding. Psychol. Rev. 1992, 99, 572–581. [Google Scholar] [CrossRef]
- Rodríguez, C.; Bélanger, E. Stories and metaphors in the sensemaking of multiple primary health care organizational identities. BMC Fam. Pract. 2014, 15, 41. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Process of Translation and Adaptation of Instruments. Available online: https://www.who.int/substance_abuse/research_tools/translation/en/ (accessed on 21 December 2021).
- Czarniawaska, B. Narratives of individual and organizational identities. Commun. Yearb. 1997, 17, 193–221. [Google Scholar]
- Steger, T. The stories metaphors tell: Metaphors as a tool to decipher tacit aspects in narratives. Field Methods 2007, 19, 3–23. [Google Scholar] [CrossRef]
- Gerhard, T. Bias: Considerations for research practice. Am. J. Health Syst. Pharm. 2008, 65, 2159–2168. [Google Scholar] [CrossRef] [PubMed]
- Vaismoradi, M.; Tutunen, H.; Bondas, T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013, 15, 398–405. [Google Scholar] [CrossRef]
- Hannah, D.R.; Lautsch, B.A. Counting in qualitative research: Why to conduct it, when to avoid it, and when to closet it. J. Manag. Inq. 2011, 20, 14–22. [Google Scholar] [CrossRef]
- Zygomatic (n.d.). Available online: https://www.wordclouds.com/ (accessed on 21 December 2021).
- McNaught, C.; Lam, P. Using Wordle as a supplementary research tool. Qual. Rep. 2010, 15, 630–643. [Google Scholar] [CrossRef]
- Ambrosi, E.; Canzan, F. Introduzione alla ricerca qualitativa: I principali metodi e sistemi di campionamento [Introduction to qualitative research: The main approaches and designs]. Assist. Inferm. Ric. 2013, 32, 178–187. [Google Scholar] [PubMed]
- Carter, N.; Bryant-Lukosius, D.; DiCenso, A.; Blythe, J.; Neville, A.J. The use of triangulation in qualitative research. Oncol. Nurs. Forum. 2014, 41, 545–547. [Google Scholar] [CrossRef] [PubMed]
- Galehdar, N.; Toulabi, T.; Kamran, A.; Heydari, H. Exploring nurses’ perception about the care needs of patients with COVID-19: A qualitative study. BMC Nurs. 2020, 19, 119. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Tarsitani, L.; Vassalini, P.; Koukopoulos, A.; Borrazzo, C.; Alessi, F.; Di Nicolantonio, C.; Serra, R.; Alessandri, F.; Ceccarelli, G.; Mastroianni, C.M.; et al. Post-traumatic Stress Disorder Among COVID-19 Survivors at 3-Month Follow-up After Hospital Discharge. J. Gen. Intern. Med. 2021, 36, 1702–1707. [Google Scholar] [CrossRef]
- Olsman, E.; Veneberg, B.; van Alfen, C.; Touwen, D. The value of metaphorical reasoning in bioethics: An empirical-ethical study. Nurs. Ethics 2019, 26, 50–60. [Google Scholar] [CrossRef] [Green Version]
- Weaver, K. Transforming Metaphors: Engaging the Authentic Self in Nursing Education. International. Glob. J. Interdiscip. Soc. Sci. 2010, 4, 1–12. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Chew, Q.H.; Wei, K.C.; Vasoo, S.; Chua, H.C.; Sim, K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: Practical considerations for the COVID-19 pandemic. Trop. J. Pharm. Res. 2020, 61, 350–356. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.; Landry, C.A.; Paluszek, M.M.; Fergus, T.A.; McKay, D.; Asmundson, G.J. COVID stress syndrome: Concept, structure, and correlates. Depress. Anxiety 2020, 37, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Vazquez, C.; Valiente, C.; García, F.E.; Contreras, A.; Peinado, V.; Trucharte, A.; Bentall, R.P. Post-Traumatic Growth and Stress-Related Responses During the COVID-19 Pandemic in a National Representative Sample: The Role of Positive Core Beliefs About the World and Others. J. Happiness Stud. 2021, 22, 2915–2935. [Google Scholar] [CrossRef]
- Venuleo, C.; Marinaci, T.; Gennaro, A.; Palmieri, A. The Meaning of Living in the Time of COVID-19. A Large Sample Narrative Inquiry. Front. Psychol. 2020, 11, 577077. [Google Scholar] [CrossRef]
- Forestier, B.; Anthoine, E.; Reguiai, Z.; Fohrer, C.; Blanchin, M. A systematic review of dimensions evaluating patient experience in chronic illness. Health Qual. Life Outcomes 2019, 17, 19. [Google Scholar] [CrossRef] [Green Version]
- Sisto, A.; Vicinanza, F.; Campanozzi, L.L.; Ricci, G.; Tartaglini, D.; Tambone, V. Towards a transversal definition of psychological resilience: A literature review. Medicina 2019, 55, 745. [Google Scholar] [CrossRef] [Green Version]
- Boldrini, M.; Canoll, P.D.; Klein, R.S. How COVID-19 Affects the Brain. JAMA Psychiatry 2021, 78, 682–683. [Google Scholar] [CrossRef]
- Fuller, H.R.; Huseth-Zosel, A. Lessons in resilience: Initial coping among older adults during the COVID-19 pandemic. Gerontology 2021, 61, 114–125. [Google Scholar] [CrossRef]
- Yeung, G.T.; Fung, H.H. Social support and life satisfaction among Hong Kong Chinese older adults: Family first? Eur. J. Ageing 2007, 4, 219–227. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hellmuth, J.; Barnett, T.A.; Asken, B.M.; Kelly, J.D.; Torres, L.; Stephens, M.L.; Greenhouse, B.; Martin, J.N.; Chow, F.C.; Deeks, S.G.; et al. Persistent COVID-19-associated neurocognitive symptoms in non-hospitalized patients. J. Neurovirol. 2021, 27, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Ambrosi, E.; Canzan, F.; Di Giulio, P.; Mortari, L.; Palese, A.; Tognoni, G.; Saiani, L. A cura di. L’emergenza COVID-19 nelle parole degli infermieri [The COVID-19 emergency in the words of the nurses]. Assist. Inferm. Ric. 2020, 39, 66–108. [Google Scholar] [PubMed]
- Cengia, M.G.; Di Falco, A.; Allegrini, E.; Ambrosi, E.; Brugnaro, L.; Zambon, A.; Saiani, L.; Grassetti, L.; Palese, A. Occurrence and reasons for unfinished nursing care between COVID-19 and non-COVID-19 patients. Int. Nurs. Rev. 2022. [Google Scholar] [CrossRef] [PubMed]
| At the COVID-19 Onset | N = 397 (%) |
|---|---|
| Gender | |
| Female | 206 (51.9) |
| Male | 191 (48.1) |
| Age (years), mean (CI 95%) | 52.6 (50.4–53.6) |
| Nationality | |
| Italian | 366 (92.2) |
| Non-Italian | 31 (7.8) |
| Education | |
| None | 1 (0.3) |
| Primary School | 22 (5.5) |
| Middle School | 65 (16.4) |
| High School | 160 (40.3) |
| Bachelor’s Degree | 83 (20.9) |
| Ph.D. | 3 (0.8) |
| Missing | 63 (15.9) |
| COVID-19 severity, WHO scale [27] | |
| Asymptomatic | 51 (12.8) |
| Mild disease (without pneumonia) | 261 (65.7) |
| Moderate disease (pneumonia) | 60 (15.1) |
| Severe disease (severe pneumonia) | 13 (3.3) |
| Critical disease, including acute respiratory distress syndrome (ARDS), sepsis and/or septic shock | 9 (2.2) |
| Missing | 3 (0.8) |
| Hospitalised for COVID-19 | |
| Yes | 101 (25.4) |
| Department(s)/units § | |
| Infectious Disease | 83 (82.2) |
| COVID-19 | 17 (16.8) |
| Intensive Care | 14 (13.9) |
| Pneumology | 11 (10.9) |
| Hospitalisation (days), mean (CI 95%) | 10.1 (8.0–12.3) |
| Previous comorbidities | |
| Yes | 207 (52.1) |
| Infected by whom | |
| I don’t know | 128 (32.2) |
| Family members | 229 (57.7) |
| Colleagues | 32 (8.1) |
| Family members and colleagues | 8 (2.0) |
| COVID-19 symptoms at the COVID-19 onset | |
| Yes | 350 (88.2) |
| No | 47 (11.8) |
| Symptoms, number, mean (CI 95%) | 4.75 (4.51–5.0) |
| Among symptoms, dyspnoea | 114 (32.6) |
| At six months after the COVID-19 onset | |
| Feeling completely healed | |
| Yes | 294 (70.0) |
| No | 88 (22.2) |
| Uncertain | 15 (3.8) |
| Persisting COVID-19 symptoms | |
| Yes | 128 (32.2) |
| No | 250 (63.0) |
| Uncertain | 19 (4.8) |
| Negative-Oriented 248 (62.5%) | Neutral-Oriented 95 (23.9%) | Positive-Oriented 54 (13.6%) |
|---|---|---|
 |  |  |
| At the COVID-19 Onset | Negative-Oriented | Neutral-Oriented | Positive-Oriented | p-Value |
|---|---|---|---|---|
| N = 248 (%) | N = 95 (%) | N = 54 (%) | ||
| Gender | <0.001 | |||
| Female | 148 (59.7) | 35 (36.8) | 23 (42.6) | |
| Male | 100 (40.3) | 60 (63.2) | 31 (57.4) | |
| Age (years), mean (CI 95%) | 53.9 (52.04–55.93) | 49.5 (46.11–52.92) | 54.8 (50.53–59.24) | 0.044 |
| Nationality | ||||
| Italian | 227 (91.5) | 88 (92.6) | 51 (94.4) | 0.754 |
| Not Italian | 21 (8.5) | 7 (7.4) | 3 (5.6) | |
| Education | 208/248 | 79/95 | 47/54 | |
| None | 1 (0.5) | 0 (-) | 0 (-) | 0.94 |
| Primary School | 13 (6.3) | 6 (7.6) | 3 (6.4) | |
| Middle School | 38 (18.3) | 18 (22.8) | 9 (19.1) | |
| High School | 98 (47.1) | 39 (49.4) | 23 (48.9) | |
| Bachelor’s Degree | 55 (26.4) | 16 (20.3) | 12 (25.5) | |
| Ph.D. | 3 (1.4) | 0 (-) | 0 (-) | |
| Severity of COVID-19 disease, WHO scale [27] | ||||
| Asymptomatic | 30 (12.1) | 14 (14.7) | 7 (13.0) | 0.537 |
| Mild disease (without pneumonia) | 162 (65.3) | 65 (68.4) | 34 (63.0) | |
| Moderate disease (pneumonia) | 39 (15.7) | 15 (15.8) | 6 (11.1) | |
| Severe disease (severe pneumonia) | 8 (3.2) | 1 (1.1) | 4 (7.4) | |
| Critical disease, including acute respiratory distress syndrome (ARDS), sepsis and/or septic shock | 7 (2.9) | 0 (-) | 2 (3.7) | |
| Missing | 2 (0.8) | 0 (-) | 1 (1.8) | |
| Hospitalised for COVID-19 | 65 (26.2) | 22 (23.2) | 12 (24.1) | 0.827 |
| In Intensive Care Units | 10 (4.0) | 1 (1.1) | 3 (5.6) | 0.28 |
| Hospitalisation (days), mean (CI 95%) | 9.9 (7.67–12.15) | 7.19 (2.08–12.30) | 12.14 (2.59–21.70) | 0.396 |
| Infected by whom | 0.22 | |||
| I don’t know | 76 (30.6) | 34 (35.8) | 18 (33.3) | |
| Family members | 152 (61.3) | 50 (52.6) | 27 (50) | |
| Colleagues | 16 (6.5) | 10 (10.5) | 6 (11.1) | |
| Family members and Colleagues | 4 (1.6) | 1 (1.1) | 3 (5.6) | |
| COVID-19 symptoms at the onset | ||||
| Yes | 219 (88.3) | 78 (82.1) | 53 (98.1) | 0.014 |
| Symptoms, number, mean (CI 95%) | 4.85 (4.54–5.15) | 4.51(4.03–5.00) | 4.74 (4.01–5.46) | 0.54 |
| Among symptoms, dyspnoea | 73 (29.4) | 26 (27.4) | 15 (27.8) | 0.918 |
| Comorbidities | 137 (55.5) | 46 (48.4) | 24 (44.5) | 0.234 |
| At six months after COVID-19 onset | ||||
| Feeling healed/recovered | ||||
| Yes | 183 (76.3) | 69 (78.4) | 42 (77.8) | 0.908 |
| No | 57 (23.7) | 19 (21.6) | 12 (22.2) | |
| Persisting COVID-19 symptoms | ||||
| Yes | 156 (65.0) | 55 (64.0) | 39 (75.0) | 0.342 |
| No | 84 (35.0) | 31 (36.0) | 13 (25.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palese, A.; Peghin, M.; Bressan, V.; Venturini, M.; Gerussi, V.; Bontempo, G.; Graziano, E.; Visintini, E.; Tascini, C. One Word to Describe My Experience as a COVID-19 Survivor Six Months after Its Onset: Findings of a Qualitative Study. Int. J. Environ. Res. Public Health 2022, 19, 4954. https://doi.org/10.3390/ijerph19094954
Palese A, Peghin M, Bressan V, Venturini M, Gerussi V, Bontempo G, Graziano E, Visintini E, Tascini C. One Word to Describe My Experience as a COVID-19 Survivor Six Months after Its Onset: Findings of a Qualitative Study. International Journal of Environmental Research and Public Health. 2022; 19(9):4954. https://doi.org/10.3390/ijerph19094954
Chicago/Turabian StylePalese, Alvisa, Maddalena Peghin, Valentina Bressan, Margherita Venturini, Valentina Gerussi, Giulia Bontempo, Elena Graziano, Erica Visintini, and Carlo Tascini. 2022. "One Word to Describe My Experience as a COVID-19 Survivor Six Months after Its Onset: Findings of a Qualitative Study" International Journal of Environmental Research and Public Health 19, no. 9: 4954. https://doi.org/10.3390/ijerph19094954
APA StylePalese, A., Peghin, M., Bressan, V., Venturini, M., Gerussi, V., Bontempo, G., Graziano, E., Visintini, E., & Tascini, C. (2022). One Word to Describe My Experience as a COVID-19 Survivor Six Months after Its Onset: Findings of a Qualitative Study. International Journal of Environmental Research and Public Health, 19(9), 4954. https://doi.org/10.3390/ijerph19094954








