The Effect of Perceptions of Hookah Harmfulness and Addictiveness on the Age of Initiation of Hookah Use among Population Assessment of Tobacco and Health (PATH) Youth
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measures
2.2.1. Ever, Past 30-Day, and Fairly Regular Hookah Use
2.2.2. Exposures: Perceptions of Hookah Harmfulness and Addictiveness
2.2.3. Covariates
2.3. Age of Initiation of Hookah Use Outcomes
2.4. Statistical Analysis
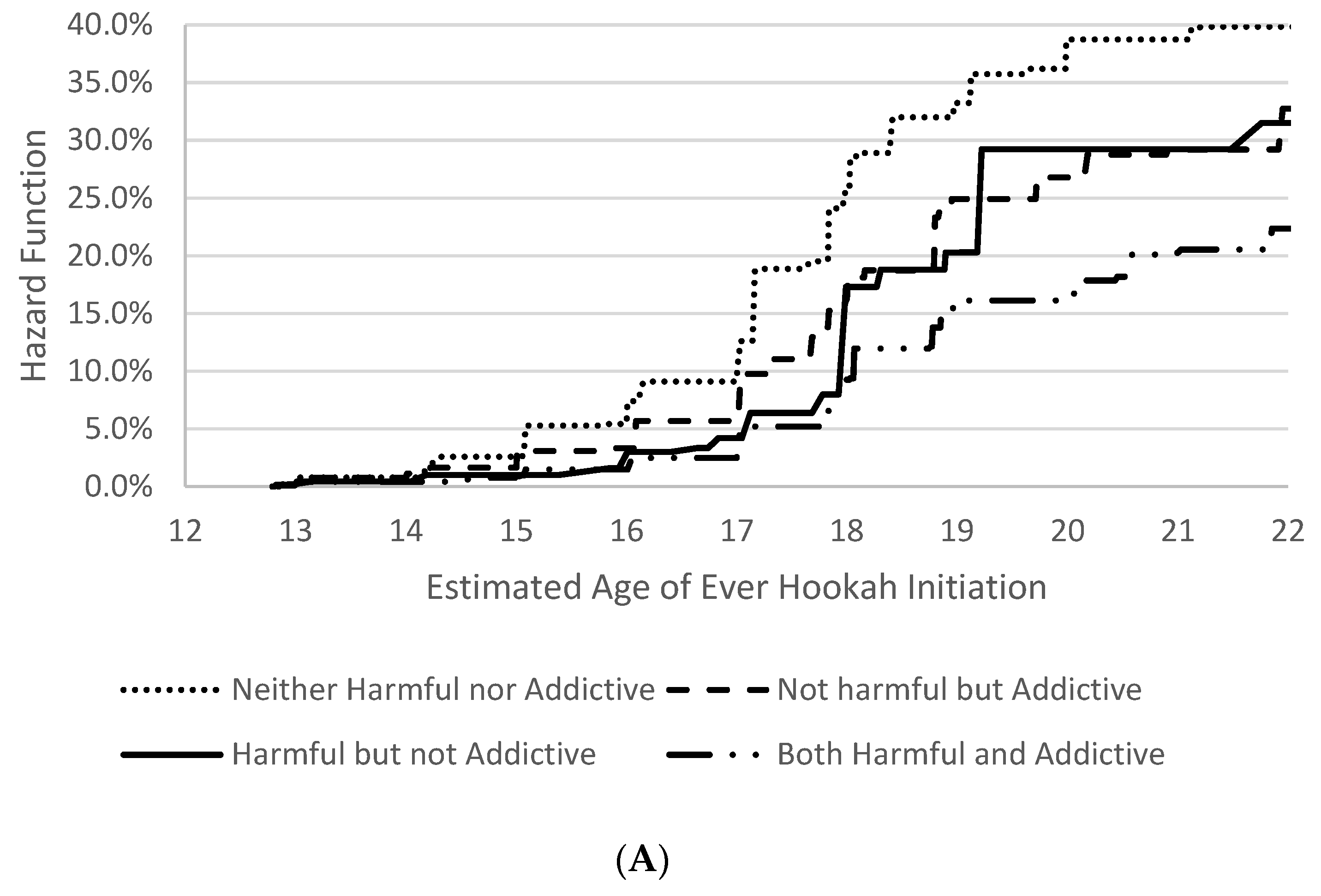
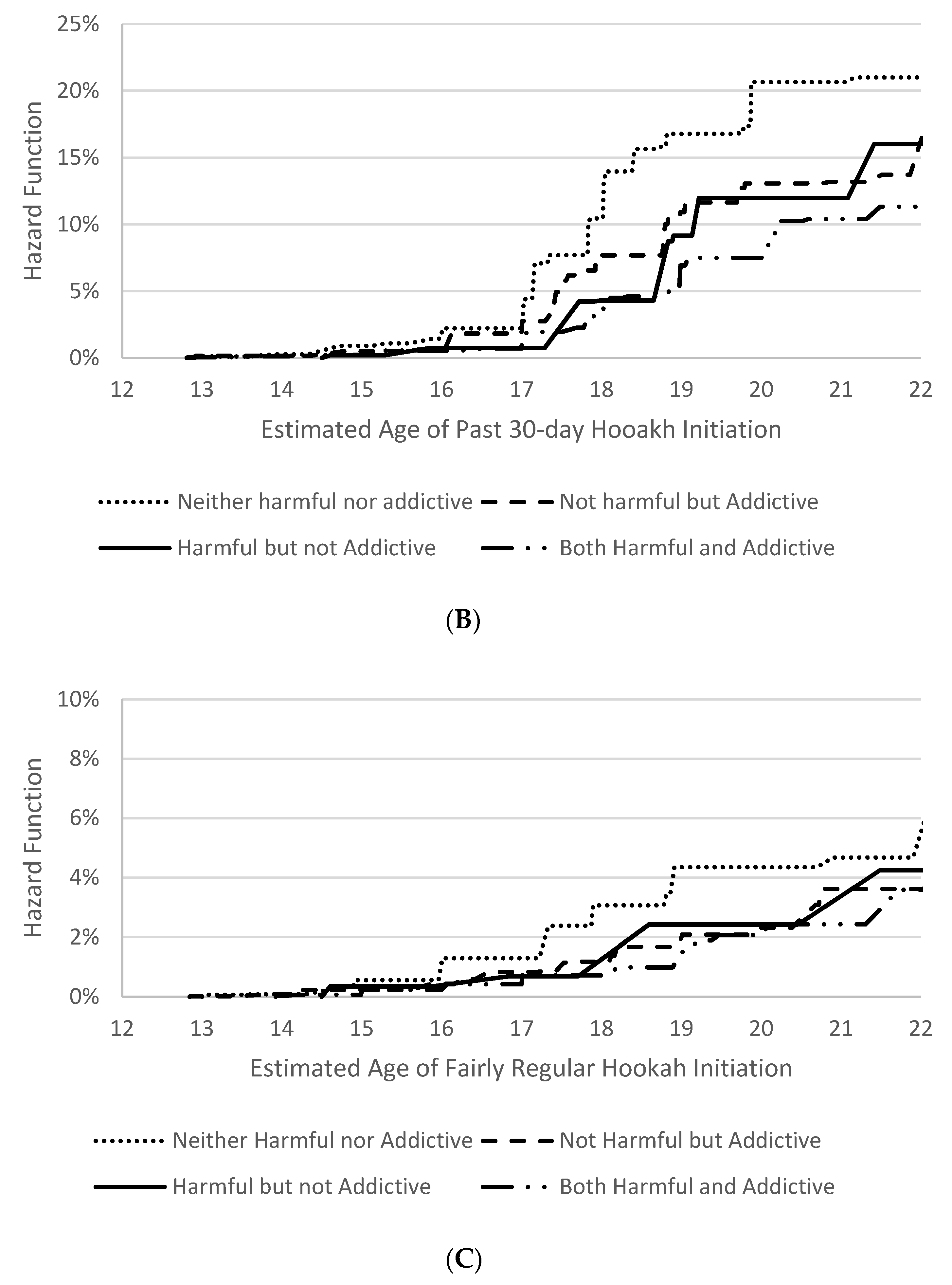
3. Results
4. Discussion
Strength and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Center for Chronic Disease Prevention Health Promotion Office on Smoking Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General; Centers for Disease Control and Prevention (US): Atlanta, GA, USA, 2014.
- National Center for Chronic Disease Prevention Health Promotion Office on Smoking Health. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General; Centers for Disease Control and Prevention (US): Atlanta, GA, USA, 2012.
- Sharma, E.; Bansal-Travers, M.; Edwards, K.C.; Halenar, M.J.; Taylor, K.A.; Kasza, K.A.; Day, H.; Hammad, H.T.; Anic, G.; Limpert, J.; et al. Longitudinal pathways of exclusive and polytobacco hookah use among youth, young adults and adults in the USA: Findings from the PATH Study Waves 1–3 (2013–2016). Tob. Control 2020, 29, s155–s162. [Google Scholar] [CrossRef]
- Pérez, A.; Kuk, A.E.; Bluestein, M.A.; Harrell, M.B.; Perry, C.L.; Chen, B. Prospective estimation of the age of initiation of hookah use among youth: Findings from the Population Assessment of Tobacco and Health (PATH) study waves 1–4 (2013–2017). Addict. Behav. 2021, 117, 106838. [Google Scholar] [CrossRef] [PubMed]
- Gentzke, A.S.; Wang, T.W.; Jamal, A.; Park-Lee, E.; Ren, C.; Cullen, K.A.; Neff, L. Tobacco product use among middle and high school students—United States, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1881–1888. [Google Scholar] [CrossRef] [PubMed]
- Meier, E.M.; Tackett, A.P.; Miller, M.B.; Grant, D.M.; Wagener, T.L. Which nicotine products are gateways to regular use? First-tried tobacco and current use in college students. Am. J. Prev. Med. 2015, 48, S86–S93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, T.W.; Gentzke, A.S.; Creamer, M.R.; Cullen, K.A.; Holder-Hayes, E.; Sawdey, M.D.; Anic, G.M.; Portnoy, D.; Hu, S.; Homa, D.M.; et al. Tobacco product use and associated factors among middle and high school students—United States, 2019. MMWR Surveill. Summ. 2019, 68, 1–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blank, M.D.; Cobb, C.O.; Kilgalen, B.; Austin, J.; Weaver, M.F.; Shihadeh, A.; Eissenberg, T. Acute effects of waterpipe tobacco smoking: A double-blind, placebo-control study. Drug Alcohol Depend. 2011, 116, 102–109. [Google Scholar] [CrossRef] [Green Version]
- Fitzpatrick, M.; Johnson, A.C.; Tercyak, K.P.; Hawkins, K.B.; Villanti, A.C.; Mays, D. Adolescent beliefs about hookah and hookah tobacco use and implications for preventing use. Prev. Chronic Dis. 2019, 16, E05. [Google Scholar] [CrossRef]
- World Health Organization and Regional Office for the Eastern Mediterranean. Tobacco Use in Shisha: Studies on Waterpipe Smoking in Egypt; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Ansari, H. Hookah use among youth and young adults: A public health challenge. Health Scope 2014, 3, 20632. [Google Scholar] [CrossRef]
- Noland, M.; Ickes, M.J.; Rayens, M.K.; Butler, K.; Wiggins, A.T.; Hahn, E.J. Social influences on use of cigarettes, e-cigarettes, and hookah by college students. J. Am. Coll. Health 2016, 64, 319–328. [Google Scholar] [CrossRef]
- Akl, E.A.; Gaddam, S.; Gunukula, S.K.; Honeine, R.; Jaoude, P.A.; Irani, J. The effects of waterpipe tobacco smoking on health outcomes: A systematic review. Int. J. Epidemiol. 2010, 39, 834–857. [Google Scholar] [CrossRef] [Green Version]
- Waziry, R.; Jawad, M.; Ballout, R.A.; Al Akel, M.; Akl, E.A. The effects of waterpipe tobacco smoking on health outcomes: An updated systematic review and meta-analysis: Table 1. Int. J. Epidemiol. 2016, 46, 32–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cobb, C.; Ward, K.D.; Maziak, W.; Shihadeh, A.L.; Eissenberg, T. Waterpipe Tobacco Smoking: An emerging health crisis in the United States. Am. J. Health Behav. 2010, 34, 275–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alarabi, A.; Karim, Z.A.; Ramirez, J.E.M.; Hernandez, K.R.; Lozano, P.A.; Rivera, J.O.; Alshbool, F.Z.; Khasawneh, F.T. Short-term exposure to waterpipe/hookah smoke triggers a hyperactive platelet activation state and increases the risk of thrombogenesis. Arter. Thromb. Vasc. Biol. 2020, 40, 335–349. [Google Scholar] [CrossRef] [PubMed]
- Hair, E.; Rath, J.; Pitzer, L.; Emelle, B.; Ganz, O.; Halenar, M.; Cantrell, J.; Vallone, D. Trajectories of hookah use: Harm perceptions from youth to young adulthood. Am. J. Health Behav. 2017, 41, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Jacob, P.; Abu Raddaha, A.; Dempsey, D.; Havel, C.; Peng, M.; Yu, L.; Benowitz, N.L. Nicotine, carbon monoxide, and carcinogen exposure after a single use of a water pipe. Cancer Epidemiol. Biomark. Prev. 2011, 20, 2345–2353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sutfin, E.L.; McCoy, T.P.; Reboussin, B.A.; Wagoner, K.G.; Spangler, J.; Wolfson, M. Prevalence and correlates of waterpipe tobacco smoking by college students in North Carolina. Drug Alcohol Depend. 2011, 115, 131–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parker, M.A.; Villanti, A.C.; Quisenberry, A.J.; Stanton, C.A.; Doogan, N.J.; Redner, R.; Gaalema, D.E.; Kurti, A.N.; Nighbor, T.; Roberts, M.E.; et al. Tobacco product harm perceptions and new use. Pediatrics 2018, 142, e20181505. [Google Scholar] [CrossRef] [Green Version]
- Strong, D.R.; Leas, E.; Elton-Marshall, T.; Wackowski, O.; Travers, M.; Bansal-Travers, M.; Hyland, A.; White, M.; Noble, M.; Cummings, K.M.; et al. Harm perceptions and tobacco use initiation among youth in Wave 1 and 2 of the Population Assessment of Tobacco and Health (PATH) study. Prev. Med. 2019, 123, 185–191. [Google Scholar] [CrossRef]
- National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General; Centers for Disease Control and Prevention (US): Atlanta, GA, USA, 2016.
- National Addiction & HIV Data Archive Program. Population Assessment of Tobacco and Health (PATH) Study [United States] Restricted-Use Files (ICPSR 36231); Inter-University Consortium for Political and Social Research: Ann Arbor, MI, USA, 2021. [Google Scholar] [CrossRef]
- Pérez, A.; N’Hpang, R.S.; Callahan, E.; Bluestein, M.; Kuk, A.E.; Chen, B.; Perry, C.L.; Harrell, M.B. Age at Initiation of cigarette use in a nationally representative sample of US youth, 2013–2017. JAMA Netw. Open 2021, 4, e210218. [Google Scholar] [CrossRef]
- Pérez, A.; Bluestein, M.A.; Kuk, A.E.; Chen, B. Age of e-cigarette initiation in USA young adults: Findings from the Population Assessment of Tobacco and Health (PATH) study (2013–2017). PLoS ONE 2021, 16, e0261243. [Google Scholar] [CrossRef]
- Chen, B.; Sterling, K.L.; Bluestein, M.A.; Kuk, A.E.; Harrell, M.B.; Perry, C.L.; Pérez, A. Age of initiation of cigarillos, filtered cigars and/or traditional cigars among youth: Findings from the Population Assessment of Tobacco and Health (PATH) study, 2013–2017. PLoS ONE 2020, 15, e0243372. [Google Scholar] [CrossRef] [PubMed]
- Pérez, A.; Kuk, A.E.; Bluestein, M.A.; Chen, B.; Sterling, K.L.; Harrell, M.B. Age of initiation of hookah use among young adults: Findings from the Population Assessment of Tobacco and Health (PATH) study, 2013–2017. PLoS ONE 2021, 16, e0258422. [Google Scholar] [CrossRef] [PubMed]
- Pérez, A.; Kuk, A.E.; Bluestein, M.A.; Penedo, E.; N’Hpang, R.S.; Chen, B.; Perry, C.L.; Sterling, K.L.; Harrell, M.B. Prospective estimation of the age of initiation of cigarettes among young adults (18–24 years old): Findings from the Population Assessment of Tobacco and Health (PATH) waves 1–4 (2013–2017). PLoS ONE 2021, 16, e0251246. [Google Scholar] [CrossRef] [PubMed]
- Pérez, A.; Bluestein, M.A.; Kuk, A.E.; Chen, B.; Sterling, K.L.; Harrell, M.B. Age of onset of susceptibility to different tobacco products among non-susceptible US young adults: Findings from the population assessment of tobacco and health study waves 2–4 (2014–2017). Tob. Use Insights 2021, 14. [Google Scholar] [CrossRef] [PubMed]
- Pérez, A.; Bluestein, M.; Chen, B.; Perry, C.L.; Harrell, M.B. Prospectively estimating the age of initiation of e-cigarettes among U.S. youth: Findings from the population assessment of tobacco and health (path) study, 2013–2017. J. Biom. Biostat. 2020, 11. [Google Scholar] [CrossRef]
- Pérez, A.; Kuk, A.E.; Bluestein, M.A.; Sia, H.M.S.; Chen, B. Age of Initiation of dual tobacco use and binge drinking among youth (12–17 years old): Findings from the Population Assessment of Tobacco and Health (PATH) study. Int. J. Environ. Res. Public Health 2021, 18, 12985. [Google Scholar] [CrossRef] [PubMed]
- Judkins, D.R. Fay’s method for variance estimation. J. Off. Stat. 1990, 6, 223–239. [Google Scholar]
- Finkelstein, D. A Proportional hazards model for interval-censored failure time data. Biometrics 1986, 42, 845. [Google Scholar] [CrossRef]
- Ng, M.P. A modification of Peto’s nonparametric estimation of survival curves for interval-censored data. Biometrics 2002, 58, 439–442. [Google Scholar] [CrossRef]
- Goodall, R.L.; Dunn, D.T.; Babiker, A.G. Interval-censored survival time data: Confidence intervals for the non-parametric survivor function. Stat. Med. 2004, 23, 1131–1145. [Google Scholar] [CrossRef]
- Turnbull, B.W. The empirical distribution function with arbitrarily grouped, censored and truncated data. J. R. Stat. Soc. Ser. B 1976, 38, 290–295. [Google Scholar] [CrossRef] [Green Version]
- Szklo, M.; Nieto, F.J.; Reilly, T.; Parker, K.E. Epidemiology: Beyond the Basics, 3rd ed.; Jones & Bartlett Learning: Burlington, MA, USA, 2014. [Google Scholar]
| Total | n = 21,968; N = 40,343,800 | ||
|---|---|---|---|
| n (N) | Weighted % (SE) | ||
| First wave of PATH ¥ participation | Wave 1 (2013–2014) | 12,585 (22,894,057) | 56.7% (0.11) |
| Wave 2 (2014–2015) | 2071 (4,079,970) | 10.1% (0.08) | |
| Wave 3 (2015–2016) | 2012 (4,142,408) | 10.3% (0.11) | |
| Wave 4 (2016–2017) | 5300 (9,227,366) | 22.9% (0.10) | |
| Age at entry into study (SE) | Weighted mean (SE) | 13.7 (0.005) | |
| Sex | Female | 10,587 (19,612,356) | 48.6% (0.12) |
| Male | 11,372 (20,711,496) | 51.3% (0.12) | |
| Missing | 9 (19,949) | 0.1% (0.02) | |
| Race/ethnicity | Non-Hispanic White | 10,492 (21,491,690) | 53.3% (0.14) |
| Hispanic | 6332 (9,250,260) | 22.9% (0.11) | |
| Non-Hispanic Black | 3000 (5,520,016) | 13.7% (0.08) | |
| Non-Hispanic Other 1 | 2098 (3,999,530) | 9.9% (0.10) | |
| Missing | 46 (82,304) | 0.2% (0.04) | |
| Ever use of cigarettes prior to | Yes | 3922 (7,036,954) | 17.4% (0.37) |
| hookah initiation | No | 18,026 (33,271,260) | 82.5% (0.37) |
| Missing | 20 (35,586) | 0.1% (0.02) | |
| Ever use of e-cigarettes prior to | Yes | 6317 (11,670,433) | 28.9% (0.47) |
| hookah initiation | No | 15,463 (28,276,108) | 70.1% (0.47) |
| Missing | 188 (397,259) | 1.0% (0.07) | |
| Ever use of any cigar products prior | Yes | 2557 (4,655,341) | 11.5% (0.27) |
| to hookah initiation | No | 19,206 (35,302,536) | 87.5% (0.28) |
| Missing | 205 (24,938) | 1.0% (0.06) | |
| Ever use of smokeless tobacco prior | Yes | 1224 (2,292,428) | 5.7% (0.23) |
| to hookah initiation | No | 20,595 (37,777,447) | 93.6% (0.25) |
| Missing | 149 (273,925) | 0.7% (0.06) | |
| Perception of harmfulness | No/little harm | 2293 (4,155,555) | 10.3% (0.30) |
| Some harm | 4721 (8,634,302) | 21.4% (0.37) | |
| A lot of harm | 8004 (14,723,395) | 36.5% (0.36) | |
| Don’t know | 384 (738,425) | 1.8% (0.10) | |
| Not heard of hookah | 6554 (12,072,899) | 29.9% (0.48) | |
| Missing | 12 (19,224) | ||
| Perception of addictiveness | Very/somewhat unlikely | 1358 (2,461,298) | 6.1% (0.17) |
| Neither likely nor unlikely | 2043 (3,707,919) | 9.2% (0.24) | |
| Somewhat/very likely | 11,228 (20,605,841) | 51.1% (0.39) | |
| Don’t know | 769 (1,464,765) | 3.6% (0.15) | |
| Not heard of hookah | 6554 (12,072,899) | 29.9% (0.48) | |
| Missing | 16 (31,077) | ||
| Ever Use ¥ | Past 30-Day Use ¥ | Fairly Regular Use ¥ | |
|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |
| Perception of Harmfulness | |||
| A lot of harm | 1.00 | 1.00 | 1.00 |
| Some harm | 1.59 (1.41–1.80) | 1.41 (1.13–1.76) | 1.29 (0.84–1.97) |
| No/little harm | 2.66 (2.29–3.09) | 2.74 (2.23–3.38) | 2.45 (1.56–3.86) |
| Don’t know | 1.80 (1.29–2.52) | 1.53 (0.92–2.54) | 1.88 (0.52–6.76) |
| Never heard of hookah | 0.69 (0.58–0.81) | 0.67 (0.52–0.85) | 0.83 (0.52–1.33) |
| Sex | |||
| Female | 1.00 | 1.00 | 1.00 |
| Male | 0.91 (0.83–0.99) | 0.93 (0.80–1.07) | 0.81 (0.59–1.11) |
| Race/ethnicity | |||
| Non-Hispanic White | 1.00 | 1.00 | 1.00 |
| Hispanic | 1.14 (0.98–1.33) | 1.38 (1.14–1.67) | 1.75 (1.26–2.43) |
| Non-Hispanic Black | 1.16 (1.02–1.32) | 1.58 (1.29–1.94) | 1.48 (0.95–2.30) |
| Non-Hispanic Other 1 | 1.09 (0.91–1.29) | 1.52 (1.19–1.93) | 1.16 (0.65–2.07) |
| Ever use of other tobacco products prior to hookah initiation | |||
| Cigarette use—No | 1.00 | 1.00 | 1.00 |
| Cigarette use—Yes | 1.37 (1.19–1.58) | 1.22 (0.98–1.53) | 1.83 (1.20–2.79) |
| E-cigarette use—No | 1.00 | 1.00 | 1.00 |
| E-cigarette use—Yes | 0.71 (0.64–0.79) | 0.78 (0.64–0.94) | 0.77 (0.55–1.08) |
| Any cigar use—No | 1.00 | 1.00 | 1.00 |
| Any cigar use—Yes | 0.92 (0.79–1.06) | 0.93 (0.73–1.18) | 0.89 (0.57–1.41) |
| Smokeless tobacco use—No | 1.00 | 1.00 | 1.00 |
| Smokeless tobacco use—Yes | 1.06 (0.88–1.29) | 1.15 (0.88–1.50) | 1.13 (0.60–1.08) |
| Model 4 | Model 5 | Model 6 | |
| Perception of Addictiveness | |||
| Somewhat/very likely | 1.00 | 1.00 | 1.00 |
| Neither likely nor unlikely | 1.62 (1.45–1.81) | 1.65 (1.36–2.01) | 1.71 (1.12–2.62) |
| Very/somewhat unlikely | 1.98 (1.67–2.33) | 1.97 (1.61–2.41) | 1.93 (1.19–3.13) |
| Don’t know | 1.39 (1.15–1.69) | 1.24 (0.89–1.72) | 1.02 (0.44–2.34) |
| Never heard of hookah | 0.53 (0.47–0.61) | 0.53 (0.44–0.66) | 0.71 (0.47–1.08) |
| Sex | |||
| Female | 1.00 | 1.00 | 1.00 |
| Male | 0.89 (0.81–0.97) | 0.89 (0.78–1.04) | 0.81 (0.59–1.11) |
| Race/ethnicity | |||
| Non-Hispanic White | 1.00 | 1.00 | 1.00 |
| Hispanic | 1.15 (0.98–1.34) | 1.39 (1.15–1.69) | 1.77 (1.27–2.47) |
| Non-Hispanic Black | 1.19 (1.04–1.37) | 1.63 (1.31–2.02) | 1.49 (0.95–2.36) |
| Non-Hispanic Other 1 | 1.07 (0.89–1.29) | 1.50 (1.17–1.94) | 1.17 (0.66–2.08) |
| Ever use of other tobacco products prior to hookah initiation | |||
| Cigarette use—No | 1.00 | 1.00 | 1.00 |
| Cigarette use—Yes | 1.35 (1.18–1.57) | 1.19 (0.95–1.51) | 1.78 (1.15–2.74) |
| E-cigarette use—No | 1.00 | 1.00 | 1.00 |
| E-cigarette use—Yes | 0.72 (0.65–0.81) | 0.79 (0.65–0.96) | 0.78 (0.56–1.09) |
| Any cigar use—No | 1.00 | 1.00 | 1.00 |
| Any cigar use—Yes | 0.93 (0.80–1.08) | 0.93 (0.73–1.19) | 0.89 (0.56–1.40) |
| Smokeless tobacco use—No | 1.00 | 1.00 | 1.00 |
| Smokeless tobacco use—Yes | 1.07 (0.89–1.29) | 1.17 (0.89–1.52) | 1.16 (0.62–2.17) |
| Total | n = 14,492; N = 26,515,180 | ||
|---|---|---|---|
| n (N) | Weighted % (SE) | ||
| First wave of PATH ¥ participation | Wave 1 (2013–2014) | 6824 (12,429,639) | 46.9% (0.29) |
| Wave 2 (2014–2015) | 703 (1,389,820) | 5.2% (0.17) | |
| Wave 3 (2015–2016) | 1872 (3,838,256) | 14.5% (0.19) | |
| Wave 4 (2016–2017) | 5093 (8,857,465) | 33.4% (0.27) | |
| Age at entry into study (SE) | Weighted mean (SE) | 13.9 (0.009) | |
| Sex | Female | 7163 (13,290,977) | 49.8% (0.27) |
| Male | 7326 (13,216,365) | 50.1% (0.27) | |
| Missing | 3 (7838) | 0.1% (0.02) | |
| Race/ethnicity | Non-Hispanic White | 6606 (13,580,180) | 51.2% (0.29) |
| Hispanic | 4435 (6,515,941) | 24.6% (0.27) | |
| Non-Hispanic Black | 1980 (3,644,534) | 13.7% (0.21) | |
| Non-Hispanic Other 1 | 1445 (2,730,255) | 10.3% (0.19) | |
| Missing | 26 (44,270) | 0.2% (0.04) | |
| Ever use of cigarettes prior to hookah initiation | Yes | 2689 (4,802,141) | 18.1% (0.42) |
| No | 11,794 (21,699,339) | 81.8% (0.42) | |
| Missing | 9 (13,700) | 0.1% (0.02) | |
| Ever use of e-cigarettes prior to hookah initiation | Yes | 4303 (7,903,090) | 29.8% (0.54) |
| No | 10,022 (18,258,492) | 68.9% (0.53) | |
| Missing | 167 (353,598) | 1.3% (0.11) | |
| Ever use of any cigar products prior to hookah initiation | Yes | 1783 (3,242,870) | 12.2% (0.31) |
| No | 12,635 (23,134,768) | 87.3% (0.32) | |
| Missing | 74 (137,542) | 0.5% (0.06) | |
| Ever use of smokeless tobacco prior to hookah initiation | Yes | 776 (1,455,018) | 5.5% (0.27) |
| No | 13,619 (24,887,149) | 93.9% (0.28) | |
| Missing | 97 (173,014) | 0.6% (0.06) | |
| Interaction of perceptions of harmfulness and addictiveness of hookah | Neither harmful nor addictive | 2508 (4,550,031) | 17.2% (0.39) |
| Addictive but not harmful | 4258 (7,778,990) | 29.3% (0.45) | |
| Harmful but not addictive | 856 (1,552,431) | 5.9% (0.20) | |
| Both harmful and addictive | 6870 (12,633,727) | 47.6% (0.61) | |
| Ever Use ¥ | Past 30-Day Use ¥ | Fairly Regular Use ¥ | |
|---|---|---|---|
| Model 7 | Model 8 | Model 9 | |
| Interaction of perceptions of hookah harmfulness and addictiveness | |||
| Both harmful and addictive | 1.00 | 1.00 | 1.00 |
| Harmful but not addictive | 1.55 (1.18–2.03) | 1.28 (0.85–1.94) | 1.44 (0.58–3.59) |
| Addictive but not harmful | 1.81 (1.56–2.10) | 1.66 (1.32–2.09) | 1.47 (0.89–2.43) |
| Neither harmful nor addictive | 2.73 (2.35–3.16) | 2.66 (2.10–3.37) | 2.42 (1.46–4.03) |
| Sex | |||
| Female | 1.00 | 1.00 | 1.00 |
| Male | 0.90 (0.82–0.99) | 0.95 (0.81–1.11) | 0.75 (0.51–1.10) |
| Race/ethnicity | |||
| Non-Hispanic White | 1.00 | 1.00 | 1.00 |
| Hispanic | 1.10 (0.94–1.29) | 1.37 (1.11–1.68) | 1.67 (1.14–2.44) |
| Non-Hispanic Black | 1.11 (0.95–1.29) | 1.52 (1.18–1.95) | 1.08 (0.57–2.03) |
| Non-Hispanic Other 1 | 1.12 (0.91–1.37) | 1.63 (1.24–2.14) | 1.30 (0.70–2.42) |
| Previous ever use of other tobacco products | |||
| Cigarette use—No | 1.00 | 1.00 | 1.00 |
| Cigarette use—Yes | 1.18 (1.02–1.38) | 1.02 (0.79–1.31) | 1.44 (0.89–2.34) |
| E-cigarette use—No | 1.00 | 1.00 | 1.00 |
| E-cigarette use—Yes | 0.73 (0.65–0.83) | 0.79 (0.63–0.98) | 0.68 (0.47–0.99) |
| Any cigar use—No | 1.00 | 1.00 | 1.00 |
| Any cigar use—Yes | 0.92 (0.79–1.07) | 0.91 (0.69–1.20) | 0.92 (0.55–1.53) |
| Smokeless tobacco use—No | 1.00 | 1.00 | 1.00 |
| Smokeless tobacco use—Yes | 1.03 (0.82–1.29) | 1.12 (0.79–1.57) | 1.52 (0.78–2.97) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuk, A.E.; Bluestein, M.A.; Chen, B.; Harrell, M.; Spells, C.E.; Atem, F.; Pérez, A. The Effect of Perceptions of Hookah Harmfulness and Addictiveness on the Age of Initiation of Hookah Use among Population Assessment of Tobacco and Health (PATH) Youth. Int. J. Environ. Res. Public Health 2022, 19, 5034. https://doi.org/10.3390/ijerph19095034
Kuk AE, Bluestein MA, Chen B, Harrell M, Spells CE, Atem F, Pérez A. The Effect of Perceptions of Hookah Harmfulness and Addictiveness on the Age of Initiation of Hookah Use among Population Assessment of Tobacco and Health (PATH) Youth. International Journal of Environmental Research and Public Health. 2022; 19(9):5034. https://doi.org/10.3390/ijerph19095034
Chicago/Turabian StyleKuk, Arnold E., Meagan A. Bluestein, Baojiang Chen, Melissa Harrell, Charles E. Spells, Folefac Atem, and Adriana Pérez. 2022. "The Effect of Perceptions of Hookah Harmfulness and Addictiveness on the Age of Initiation of Hookah Use among Population Assessment of Tobacco and Health (PATH) Youth" International Journal of Environmental Research and Public Health 19, no. 9: 5034. https://doi.org/10.3390/ijerph19095034
APA StyleKuk, A. E., Bluestein, M. A., Chen, B., Harrell, M., Spells, C. E., Atem, F., & Pérez, A. (2022). The Effect of Perceptions of Hookah Harmfulness and Addictiveness on the Age of Initiation of Hookah Use among Population Assessment of Tobacco and Health (PATH) Youth. International Journal of Environmental Research and Public Health, 19(9), 5034. https://doi.org/10.3390/ijerph19095034






