Behavior Modification Techniques on Patients with Chronic Pain in the Context of COVID-19 Telerehabilitation: An Umbrella Review
Abstract
:1. Introduction
2. Methods
2.1. Review Inclusion Criteria
2.1.1. Population
2.1.2. Intervention and Control
2.1.3. Outcomes
2.1.4. Study Design
2.2. Search Strategy
2.3. Selection Criteria and Data Extraction
2.4. Methodological Quality Assessment
2.4.1. Risk of Bias Assessment
2.4.2. Grading of Evidence
3. Results
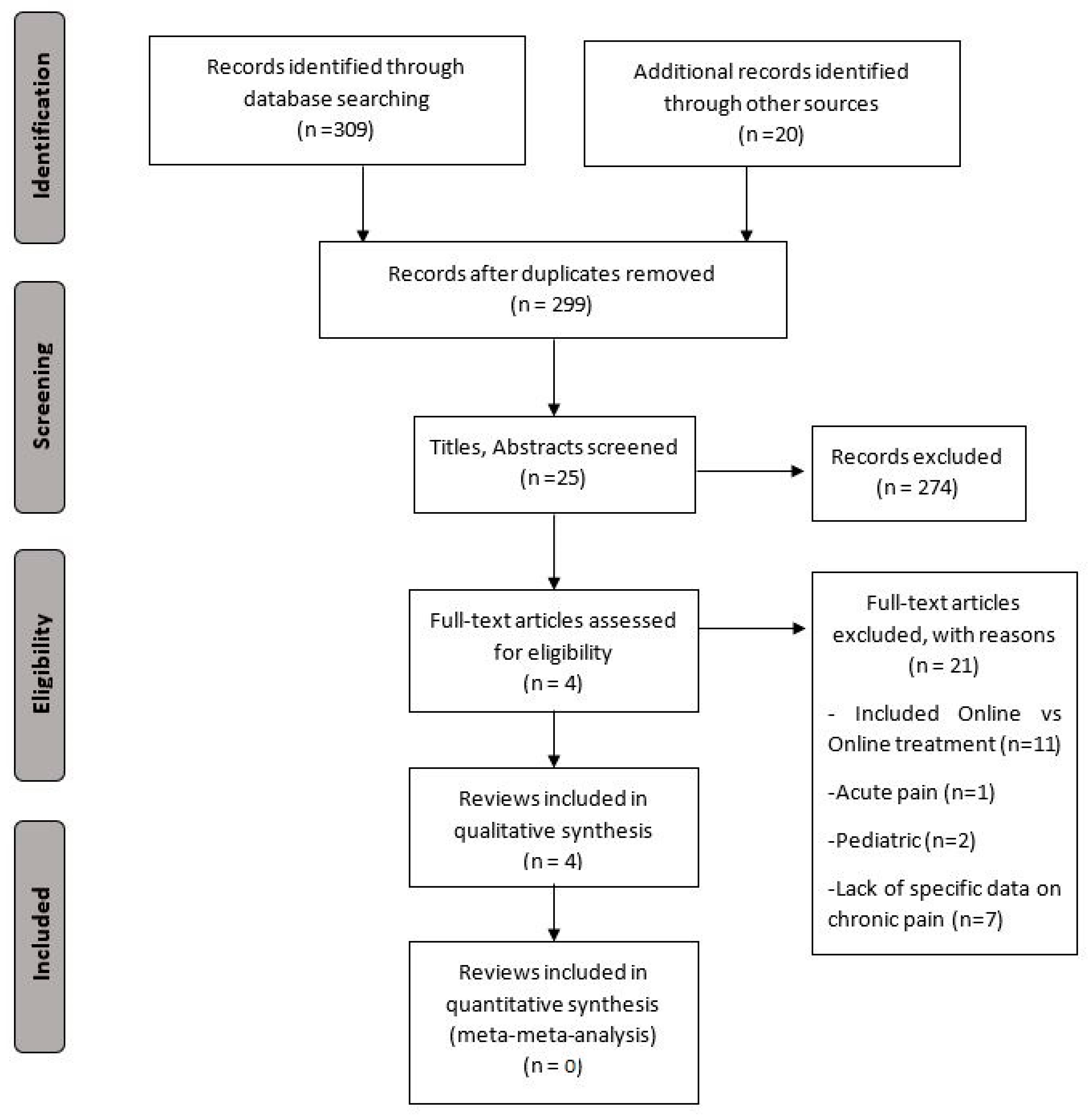
3.1. Study Selection
3.2. Characteristics of the Included Systematic Reviews
3.3. Results of the Methodological Quality
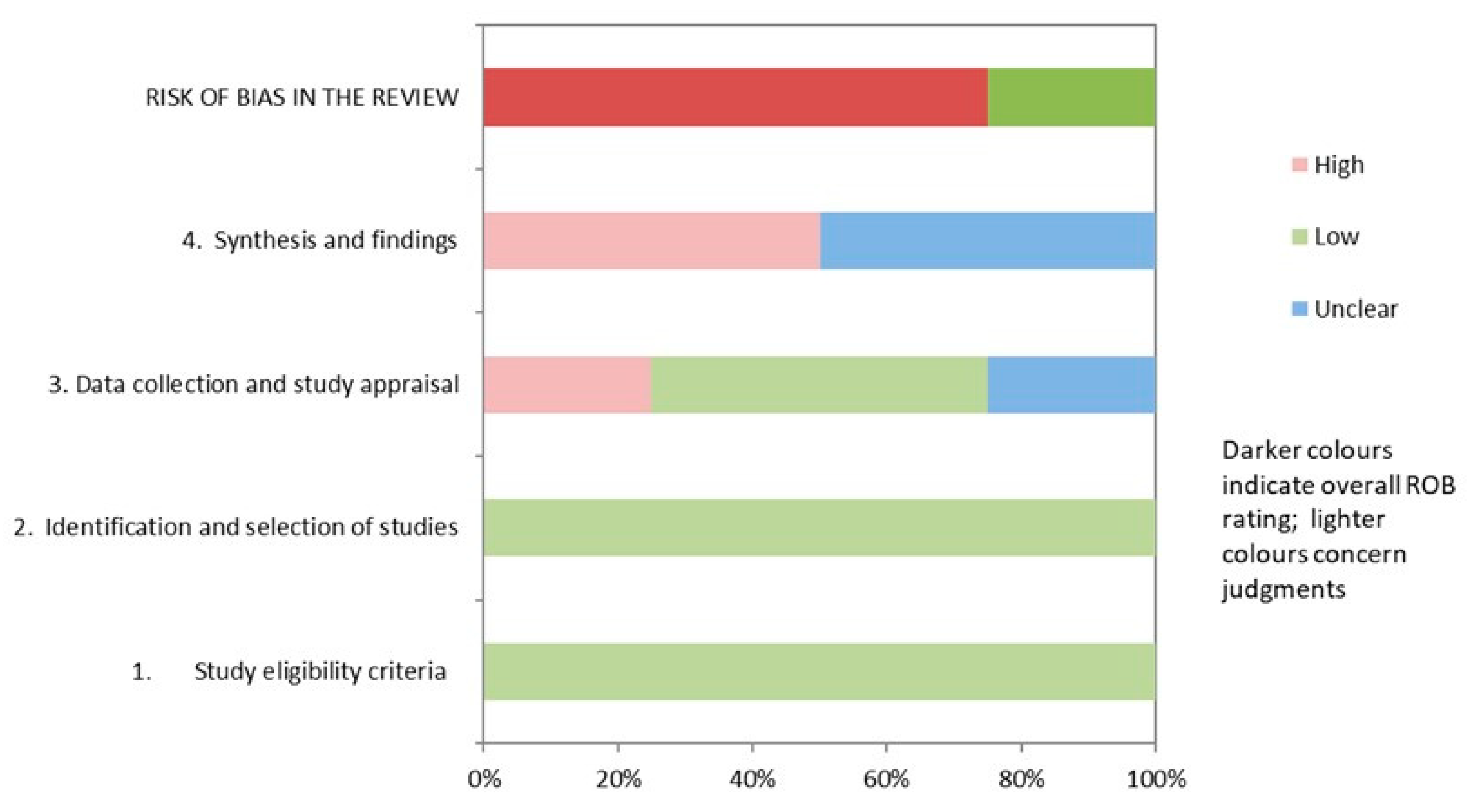
3.4. Results of Risk of Bias
3.5. Grading of Evidence Results
3.6. Qualitative Synthesis
3.6.1. Pain Intensity
3.6.2. Disability
3.6.3. Psychological Symptoms
3.6.4. Disease Impact
3.6.5. Physical Function
4. Discussion
4.1. Principal Results
4.2. Gap in the Literature
4.3. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A. PubMed Systematic Search Strategy
References
- Eccleston, C.; Blyth, F.M.; Dear, B.F.; Fisher, E.A.; Keefe, F.J.; Lynch, M.E.; Palermo, T.M.; Reid, M.C.; de Williams, A.C. Managing patients with chronic pain during the COVID-19 outbreak: Considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain 2020, 161, 889–893. [Google Scholar] [CrossRef] [PubMed]
- Lacasse, A.; Pagé, M.G.; Dassieu, L.; Sourial, N.; Janelle-Montcalm, A.; Dorais, M.; Nguena Nguefack, H.L.; Godbout-Parent, M.; Hudspith, M.; Moor, G.; et al. Impact of the COVID-19 pandemic on the pharmacological, physical, and psychological treatments of pain: Findings from the Chronic Pain & COVID-19 Pan-Canadian Study. Pain Rep. 2021, 6, e891. [Google Scholar] [PubMed]
- Nieto, R.; Pardo, R.; Sora, B.; Feliu-Soler, A.; Luciano, J.V. Impact of COVID-19 lockdown measures on Spanish people with chronic pain: An online study survey. J. Clin. Med. 2020, 9, 3558. [Google Scholar] [CrossRef] [PubMed]
- Karos, K.; McParland, J.L.; Bunzli, S.; Devan, H.; Hirsh, A.; Kapos, F.P.; Keogh, E.; Moore, D.; Tracy, L.M.; Ashton-James, C.E. The social threats of COVID-19 for people with chronic pain. Pain 2020, 161, 2229–2235. [Google Scholar] [CrossRef] [PubMed]
- Mechanic, O.J.; Persaud, Y.; Kimball, A.B. Telehealth Systems; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Du, S.; Hu, L.; Dong, J.; Xu, G.; Chen, X.; Jin, S.; Zhang, H.; Yin, H. Self-management program for chronic low back pain: A systematic review and meta-analysis. Patient Educ. Couns. 2017, 100, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Mullins, C.F.; Harmon, D.; O’Connor, T. Quantifying the impact of COVID-19 on chronic pain services in the Republic of Ireland. Ir. J. Med. Sci. 2021, 191, 7–11. [Google Scholar] [CrossRef]
- Suso-Martí, L.; La Touche, R.; Herranz-Gómez, A.; Angulo-Díaz-Parreño, S.; Paris-Alemany, A.; Cuenca-Martínez, F. Effectiveness of telerehabilitation in physical therapist practice: An umbrella and mapping review with meta-meta-analysis. Phys. Ther. 2021, 101, pzab075. [Google Scholar] [CrossRef]
- Marotta, N.; Demeco, A.; Moggio, L.; Ammendolia, A. Why is telerehabilitation necessary? A pre-post COVID-19 comparative study of ICF activity and participation. J. Enabling Technol. 2021, 15, 117–121. [Google Scholar] [CrossRef]
- Turk, D.C.; Swanson, K.S.; Tunks, E.R. Psychological approaches in the treatment of chronic pain patients—When pills, scalpels, and needles are not enough. Can. J. Psychiatry 2008, 53, 213–223. [Google Scholar] [CrossRef] [Green Version]
- Sharp, T.J. Chronic pain: A reformulation of the cognitive-behavioural model. Behav. Res. Ther. 2001, 39, 787–800. [Google Scholar] [CrossRef]
- Macea, D.D.; Gajos, K.; Daglia Calil, Y.A.; Fregni, F. The efficacy of web-based cognitive behavioral Interventions for chronic pain: A systematic review and meta-analysis. J. Pain 2010, 11, 917–929. [Google Scholar] [CrossRef] [PubMed]
- Dario, A.B.; Moreti Cabral, A.; Almeida, L.; Ferreira, M.L.; Refshauge, K.; Simic, M.; Pappas, E.; Ferreira, P.H. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: A systematic review with meta-analysis. Spine J. 2017, 17, 1342–1351. [Google Scholar] [CrossRef] [PubMed]
- Ariza-Mateos, M.J.; Cabrera-Martos, I.; Prados-Román, E.; Granados-Santiago, M.; Rodríguez-Torres, J.; Carmen Valenza, M. A systematic review of internet-based interventions for women with chronic pain. Br. J. Occup. Ther. 2020, 84, 6–14. [Google Scholar] [CrossRef]
- White, V.; Linardon, J.; Stone, J.E.; Holmes-Truscott, E.; Olive, L.; Mikocka-Walus, A.; Hendrieckx, C.; Evans, S.; Speight, J. Online psychological interventions to reduce symptoms of depression, anxiety, and general distress in those with chronic health conditions: A systematic review and meta-analysis of randomized controlled trials. Psychol. Med. 2020, 52, 548–573. [Google Scholar] [CrossRef]
- Bougioukas, K.I.; Liakos, A.; Tsapas, A.; Ntzani, E.; Haidich, A.B. Preferred reporting items for overviews of systematic reviews including harms checklist: A pilot tool to be used for balanced reporting of benefits and harms. J. Clin. Epidemiol. 2018, 93, 9–24. [Google Scholar] [CrossRef] [PubMed]
- Stone, P.W. Popping the (PICO) question in research and evidence-based practice. Appl. Nurs. Res. 2002, 15, 197–198. [Google Scholar] [CrossRef]
- Moher, D.; Pham, B.; Jones, A.; Cook, D.J.; Jadad, A.R.; Moher, M.; Tugwell, P.; Klassen, T.P. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 1998, 352, 609–613. [Google Scholar] [CrossRef]
- Barton, C.J.; Webster, K.E.; Menz, H. Evaluation of the scope and quality of systematic reviews on nonpharmacological conservative treatment for patellofemoral pain syndrome. J. Orthop. Sports Phys. Ther. 2008, 38, 529–541. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Whiting, P.; Savović, J.; Higgins, J.P.T.; Caldwell, D.M.; Reeves, B.C.; Shea, B.; Davies, P.; Kleijnen, J.; Churchill, R. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J. Clin. Epidemiol. 2016, 69, 225–234. [Google Scholar] [CrossRef] [Green Version]
- Torres, A.; Tennant, B.; Ribeiro-Lucas, I.; Vaux-Bjerke, A.; Piercy, K.; Bloodgood, B. Umbrella and systematic review methodology to support the 2018 physical activity guidelines advisory committee. J. Phys. Act. Health 2018, 15, 805–810. [Google Scholar] [CrossRef] [PubMed]
- Turk, D.C.; Okifuji, A. Psychological factors in chronic pain: Evolution and revolution. J. Consult. Clin. Psychol. 2002, 70, 678–690. [Google Scholar] [CrossRef] [PubMed]
- Hoaas, H.; Andreassen, H.K.; Lien, L.A.; Hjalmarsen, A.; Zanaboni, P. Adherence and factors affecting satisfaction in long-term telerehabilitation for patients with chronic obstructive pulmonary disease: A mixed methods study. BMC Med. Inform. Decis. Mak. 2016, 16, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wildevuur, S.E.; Simonse, L.W.L. Information and communication technology—Enabled person-centered care for the “Big Five” chronic conditions: Scoping review. J. Med. Internet Res. 2015, 17, e77. [Google Scholar] [CrossRef] [PubMed]
- Morral, A.; Urrutia, G.; Bonfill, X. Placebo effect and therapeutic context: A challenge in clinical research. Med. Clin. (Barc) 2017, 149, 26–31. [Google Scholar] [CrossRef] [PubMed]
| Study | Number of Studies, Study Design (Sample) | Patient Characteristics | Intervention (Type of Technology) and Control Group | Outcomes | ||
|---|---|---|---|---|---|---|
| Nº of Studies Includes in Meta-Analysis (Participants) | Scales of Measurement | Results | ||||
| Ariza-Mateos et al. [14] | 7 RCTs a (n = 562) | Fibromyalgia, chronic widespread pain, or chronic primary headaches 100%F b Age: 32.5 to 53.5 yrs c | Intervention ACT d, CBT e, self-management, exercise, exposure therapy, and mindfulness (Internet-based or mobile-based) Control Control intervention or in-person treatment | Pain intensity | ||
| N/A f | VAS g, McGill Pain Questionnaire, DASS-21 h | t-BMT i seemed to be effective to improve pain intensity in women with chronic pain. | ||||
| Pain-related fear of movement | ||||||
| N/A | Tampa scale of kinesiophobia | t-BMT seemed to be effective to improve pain/fear avoidance in women with chronic pain | ||||
| Disease impact | ||||||
| N/A | Fibromyalgia impact questionnaire; fibromyalgia impact questionnaire—revised | t-BMT seemed to be effective to improve the impact of fibromyalgia on women with chronic pain | ||||
| Psychological distress | ||||||
| N/A | HADS j, GAD-7 k | t-BMT seemed to be effective to improve anxiety and depression in women with chronic pain. | ||||
| White et al. [15] | 15 RCTs | Chronic pain, fibromyalgia, and chronic headache/ migraine 18 to 100%F | Intervention Psychology-based interventions (Internet-based) Control Usual care or waiting list | Depressive symptoms | ||
| Chronic pain: 8 RCTs Fibromyalgia: 4 RCTsHeadache/ migraine: 3 RCTs | HADS, PHQ l, CES-D m, BDI n | t-BMT showed a trivial effect size on migraine/headache (Hedge’s g = 0.142; SE o = 0.120), small effect size in chronic pain patients (Hedge’s g = 0.372; SE = 0.128), and a moderate effect size on fibromyalgia (Hedge’s g = 0.679; SE = 0.259) and depressive symptoms. | ||||
| Anxiety | ||||||
| Chronic pain: 7 RCTs Headache/migraine: 2 RCTs | HADS, GAD-7, DASS p | t-BMT showed a small effect size on patients with chronic pain (Hedge’s g = 0.236; SE = 0.090) and on patients with migraine/ headache (Hedge’s g = 0.422; SE = 0.301) or anxiety. | ||||
| Darío et al. [13] | 4 RCTs (n = 1342) | Chronic LBP q 13 to 68%F Age: 46 to 51 yrs | Intervention Behavioral intervention, CBT, exercise feedback, e-community (Internet-based) Control Usual care, e-mail, equivalent in-person intervention, magazine subscription | Pain intensity | ||
| Short term: 4 RCTs Medium term: 2 RCTs | N/R r | Non-significant effect of t-BMT on pain intensity in the short term (SMD s = −0.05; 95%CI t −0.10,0.00) and medium term (SMD = −0.01; 95%CI −0.74, 0.72). | ||||
| Disability | ||||||
| Short term: 4 RCTs Medium term: 2 RCTs | N/R | Trivial effect size of t-BMT on disability in the short term (SMD = −0.04; 95%CI −0.07, −0.02), but non-significant in the medium term (SMD = 0.00; 95%CI −0.06, 0.07). | ||||
| Physical function | ||||||
| N/A | N/R | t-BMT did not seem to be superior to the control group in improving physical function. | ||||
| Du et al. [6] | 3 RCTs (n = 590) | Chronic LBP 60.6 to 83.0%F Age: 21.0 to 44.6 yrs | Intervention Self-management (Internet-based) Control Waiting list or usual care | Pain intensity | ||
| 3 RCTs | N/R | Small effect size of t-BMT on pain intensity (SMD = −0.26; 95% CI −0.42, −0.09). | ||||
| Disability | ||||||
| 3 RCTs | N/R | Small effect size of t-BMT on disability (SMD = −0.34; 95% CI −0.50, −0.17). | ||||
| Author, Year | Intervention Group | Electronic Format | Control Group | Frequency | Intervention Duration |
|---|---|---|---|---|---|
| Ariza-Mateos et al. [14] | - 45 min exercise (aerobic, strength, and stretching training) and education about the disease; - 120 min CBT a (education about the disease; relaxation and breathing training); - Online lessons (information, cognitive therapy, and pain management); - Exposure therapy (education, case examples, mindfulness exercises, and treatment based on goals); - Acceptance and commitment therapy (education, values, cognitive defusion, mindfulness, willingness and committed action, feedback, and daily diaries); - Mindfulness-based stress reduction. | Internet-based and smartphone-delivered | Control group or in-person intervention | 2 to 10 times per week | 8 to 10 weeks |
| White et al. [15] | - CBT (Information, feedback, goal setting, conversation with the therapist, homework, answering questions, patient discussion of experiences, questionnaire to target information, relaxation, watching videos/demonstrations); - Education; - Self-management (feedback, goal setting, watching videos, online workshops, participation in a discussion board, questionnaire to target information); - Questionnaires targeting information or feedback, reminders, listening to real or simulated patients’ experiences, goal setting, skills, motivational messages, feedback graphs, homework or answering questions, watching videos/demonstrations, conversation with the therapist; - Mp3 b audio recordings; - Relaxation; - Mindfulness; - Writing exercises. | Internet-based | Usual care or waiting list | N/R c | 4 weeks to 6 months |
| Dario et al. [13] | - E-mail discussion group, videotape about behavior changes, and book; - Self-management and CBT; - Pedometer + E-community, web-based walking program, and goal setting; - E-community, self-monitoring, and goals. | Internet-based | Subscription to a non-health magazine, LBP d guide, pedometer only, and usual care | N/R | 4 weeks to 12 months |
| Du et al. [6] | - Self-help treatment (education, cognitive skill, behavioral rehearsal, generalization, and maintenance); - CBT (cognitive therapy, behavioral activation, ACT e, and mindfulness-based stress reduction); - Self-tailored cognitive-behavioral approach (prevention of pain behaviors). | Internet-based | Waiting list | N/R | 3 to 8 weeks |
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ariza-Mateos et al. [14] | 2 | 2 | 0 | 2 | 0 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 19 |
| White et al. [15] | 2 | 2 | 1 | 2 | 0 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 19 |
| Dario et al. [13] | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 1 | 2 | 2 | 2 | 1 | 0 | 20 |
| Du et al. [6] | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 23 |
| Study | Phase 2 | Phase 3 | |||
|---|---|---|---|---|---|
| 1. Study Eligibility Criteria | 2. Identification and Selection of Studies | 3. Data Collection and Study Appraisal | 4. Synthesis and Findings | Risk of Bias in the Review | |
| Ariza-Mateos et al. [14] | ☺a | ☺ | ☹b | ?c | ☹ |
| White et al. [15] | ☺ | ☺ | ? | ☹ | ☹ |
| Dario et al. [13] | ☺ | ☺ | ☺ | ☹ | ☹ |
| Du et al. [6] | ☺ | ☺ | ☺ | ? | ☺ |
| 2018 Physical Activity Guidelines Advisory Committee Grading Criteria | Grade | |||||
|---|---|---|---|---|---|---|
| Systematic Review Research Questions | Applicability | Generalizability | Risk of Bias or Study Limitations | Quantity and Consistency | Magnitude and Precisionof Effect | |
| Pain Intensity | Strong | Limited | Limited | Limited | Not assignable | Limited |
| Disability | Strong | Limited | Limited | Limited | Not assignable | Limited |
| Pain-related fear of movement | Moderate | Limited | Limited | Limited | Not assignable | Limited |
| Disease impact | Moderate | Limited | Limited | Limited | Not assignable | Limited |
| Psychological distress | Moderate | Limited | Limited | Limited | Not assignable | Limited |
| Depressive symptoms | Strong | Limited | Limited | Limited | Not assignable | Limited |
| Anxiety symptoms | Strong | Limited | Limited | Limited | Not assignable | Limited |
| Physical function | Strong | Limited | Limited | Limited | Not assignable | Limited |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuenca-Martínez, F.; Calatayud, J.; Suso-Martí, L.; Varangot-Reille, C.; Herranz-Gómez, A.; Blanco-Díaz, M.; Casaña, J. Behavior Modification Techniques on Patients with Chronic Pain in the Context of COVID-19 Telerehabilitation: An Umbrella Review. Int. J. Environ. Res. Public Health 2022, 19, 5260. https://doi.org/10.3390/ijerph19095260
Cuenca-Martínez F, Calatayud J, Suso-Martí L, Varangot-Reille C, Herranz-Gómez A, Blanco-Díaz M, Casaña J. Behavior Modification Techniques on Patients with Chronic Pain in the Context of COVID-19 Telerehabilitation: An Umbrella Review. International Journal of Environmental Research and Public Health. 2022; 19(9):5260. https://doi.org/10.3390/ijerph19095260
Chicago/Turabian StyleCuenca-Martínez, Ferran, Joaquín Calatayud, Luis Suso-Martí, Clovis Varangot-Reille, Aida Herranz-Gómez, María Blanco-Díaz, and José Casaña. 2022. "Behavior Modification Techniques on Patients with Chronic Pain in the Context of COVID-19 Telerehabilitation: An Umbrella Review" International Journal of Environmental Research and Public Health 19, no. 9: 5260. https://doi.org/10.3390/ijerph19095260
APA StyleCuenca-Martínez, F., Calatayud, J., Suso-Martí, L., Varangot-Reille, C., Herranz-Gómez, A., Blanco-Díaz, M., & Casaña, J. (2022). Behavior Modification Techniques on Patients with Chronic Pain in the Context of COVID-19 Telerehabilitation: An Umbrella Review. International Journal of Environmental Research and Public Health, 19(9), 5260. https://doi.org/10.3390/ijerph19095260










