Prediction of 30-Day Readmission in Hospitalized Older Adults Using Comprehensive Geriatric Assessment and LACE Index and HOSPITAL Score
Abstract
1. Introduction
2. Materials and Methods
| Cut-Off and Interpretation | |
|---|---|
| Mini-Mental State Examination (MMSE) | 22-item questionnaire on time and place orientation, registration, attention and calculation, recall, language, repetition, and constructional ability, with total score of 30. Patients are considered with cognitive impairment if ≤24 in the literate and ≤13 in the illiterate [23,25]. |
| Mini-Cog | Two-part exam on memory and orientation—three-item recall and clock drawing test (CDT) [36,37]. Patients are considered demented if there are 0 items recalled or clock drawing test is abnormal with 1–2 items being recalled. |
| 5-item Geriatric Depression Scale (GDS-5) | 5-item questionnaire on depressive symptoms with total score of 0–5 [26,38,39]. Patients are considered with depressive symptoms if points ≤2 and psychiatric consultation is suggested. |
| Barthel Index (BI) for Activities of Daily Living (ADL) | 10-item questionnaire on one’s ability of feeding, bathing, grooming, dressing, bowel control, bladder control, toilet use, transferring, and mobility on level surfaces and stairs [32]; total score of 0–100, from total dependence to complete independence. |
| Lawton–Brody scale for Instrumental Activities of Daily Living (IADL) | 8-item questionnaire on one’s ability of using a telephone, laundry, shopping, preparing food, housekeeping, using transportation, managing one’s own medication, and handling finance [33,40]; total score 0–8, from lower physical and cognitive function to higher function. |
| Mini-Nutritional Assessment (MNA) | 30-point questionnaire on dietary and nutritional status, with total score 0–30. Patients are considered with adequate nutritional status if scored ≥24 and malnutrition if scored <17; there is higher risk of malnutrition if scored between 17 and 23.5 [27,41]. |
| 6 m Walking Speed (6M) | Gait speed less than 1 m/s indicated low physical performance [42]. |
| Timed Up and Go test (TUG) | Time measured from standing up from a chair, walking for 3 m, returning to the chair, and sitting. Frailty and gait impairment is considered if the patient took more than 30 s to complete the test, and gait aid is required [31]. |
3. Results
3.1. Baseline Characteristics, CGA, and 30-Day Readmission
3.2. LACE Index and HOSPITAL Score and 30-Day Readmission
3.3. LACE Index and HOSPITAL Score in Subgroup Patients with Physical Limitation and Malnutrition and 30-Day Readmission
4. Discussion
4.1. CGA and Readmission
4.2. LACE/HOSPITAL and Readmission
4.3. Strength and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Low, L.L.; Liu, N.; Ong, M.E.H.; Ng, E.Y.; Ho, A.F.W.; Thumboo, J.; Lee, K.H. Performance of the LACE index to identify elderly patients at high risk for hospital readmission in Singapore. Medicine 2017, 96, e6728. [Google Scholar] [CrossRef] [PubMed]
- Kroch, E.; Duan, M.; Martin, J.; Bankowitz, R.A. Patient Factors Predictive of Hospital Readmissions Within 30 Days. J. Healthc. Qual. 2016, 38, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Council, N.D. Population Projections for the R.O.C. (Taiwan): 2018~2065. Available online: https://pop-proj.ndc.gov.tw/main_en/index.aspx (accessed on 10 August 2022).
- Christensen, K.; Doblhammer, G.; Rau, R.; Vaupel, J.W. Ageing populations: The challenges ahead. Lancet 2009, 374, 1196–1208. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.M.; Freiermuth, C.E.; Shepherd-Banigan, M.; Ragsdale, L.; Eucker, S.A.; Goldstein, K.; Hastings, S.N.; Rodriguez, R.L.; Fulton, J.; Ramos, K.; et al. Emergency Department Interventions for Older Adults: A Systematic Review. J. Am. Geriatr. Soc. 2019, 67, 1516–1525. [Google Scholar] [CrossRef]
- Pandey, A.; Ploubidis, G.B.; Clarke, L.; Dandona, L. Hospitalisation trends in India from serial cross-sectional nationwide surveys: 1995 to 2014. BMJ Open 2017, 7, e014188. [Google Scholar] [CrossRef]
- Fitriana, I.; Setiati, S.; Rizal, E.W.; Istanti, R.; Rinaldi, I.; Kojima, T.; Akishita, M.; Azwar, M.K. Malnutrition and depression as predictors for 30-day unplanned readmission in older patient: A prospective cohort study to develop 7-point scoring system. BMC Geriatr. 2021, 21, 256. [Google Scholar] [CrossRef]
- Ellis, G.; Gardner, M.; Tsiachristas, A.; Langhorne, P.; Burke, O.; Harwood, R.H.; Conroy, S.P.; Kircher, T.; Somme, D.; Saltvedt, I.; et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst. Rev. 2017, 9, Cd006211. [Google Scholar] [CrossRef]
- Chiang, L.Y.; Liu, J.; Flood, K.L.; Carroll, M.B.; Piccirillo, J.F.; Stark, S.; Wang, A.; Wildes, T.M. Geriatric assessment as predictors of hospital readmission in older adults with cancer. J. Geriatr. Oncol. 2015, 6, 254–261. [Google Scholar] [CrossRef]
- Greysen, S.R.; Stijacic Cenzer, I.; Auerbach, A.D.; Covinsky, K.E. Functional impairment and hospital readmission in Medicare seniors. JAMA Intern. Med. 2015, 175, 559–565. [Google Scholar] [CrossRef]
- Barnett, M.L.; Hsu, J.; McWilliams, J.M. Patient Characteristics and Differences in Hospital Readmission Rates. JAMA Intern. Med. 2015, 175, 1803–1812. [Google Scholar] [CrossRef]
- Visade, F.; Babykina, G.; Puisieux, F.; Bloch, F.; Charpentier, A.; Delecluse, C.; Loggia, G.; Lescure, P.; Attier-Żmudka, J.; Gaxatte, C.; et al. Risk Factors for Hospital Readmission and Death After Discharge of Older Adults from Acute Geriatric Units: Taking the Rank of Admission into Account. Clin. Interv. Aging 2021, 16, 1931–1941. [Google Scholar] [CrossRef]
- Bernabeu-Mora, R.; García-Guillamón, G.; Valera-Novella, E.; Giménez-Giménez, L.M.; Escolar-Reina, P.; Medina-Mirapeix, F. Frailty is a predictive factor of readmission within 90 days of hospitalization for acute exacerbations of chronic obstructive pulmonary disease: A longitudinal study. Ther. Adv. Respir. Dis. 2017, 11, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Hao, Q.; Zhou, L.; Dong, B.; Yang, M.; Dong, B.; Weil, Y. The role of frailty in predicting mortality and readmission in older adults in acute care wards: A prospective study. Sci. Rep. 2019, 9, 1207. [Google Scholar] [CrossRef]
- Lin, K.-P.; Chen, J.-H.; Lu, F.-P.; Wen, C.-J.; Chan, D.-C. The impact of early comprehensive geriatric screening on the readmission rate in an acute geriatric ward: A quasi-experimental study. BMC Geriatr. 2019, 19, 285. [Google Scholar] [CrossRef]
- Lin, C.; Hsu, S.; Lu, H.F.; Pan, L.F.; Yan, Y.H. Comparison of Back-Propagation Neural Network, LACE Index and HOSPITAL Score in Predicting All-Cause Risk of 30-Day Readmission. Risk Manag. Healthc. Policy 2021, 14, 3853–3864. [Google Scholar] [CrossRef]
- Low, L.L.; Liu, N.; Wang, S.; Thumboo, J.; Ong, M.E.; Lee, K.H. Predicting 30-Day Readmissions in an Asian Population: Building a Predictive Model by Incorporating Markers of Hospitalization Severity. PLoS ONE 2016, 11, e0167413. [Google Scholar] [CrossRef]
- Heppleston, E.; Fry, C.H.; Kelly, K.; Shepherd, B.; Wright, R.; Jones, G.; Robin, J.; Murray, P.; Fluck, D.; Han, T.S. LACE index predicts age-specific unplanned readmissions and mortality after hospital discharge. Aging Clin. Exp. Res. 2021, 33, 1041–1048. [Google Scholar] [CrossRef]
- Cotter, P.E.; Bhalla, V.K.; Wallis, S.J.; Biram, R.W.S. Predicting readmissions: Poor performance of the LACE index in an older UK population. Age Ageing 2012, 41, 784–789. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef]
- Lin, C.F.; Huang, Y.H.; Ju, L.Y.; Weng, S.C.; Lee, Y.S.; Chou, Y.Y.; Lin, C.S.; Lin, S.Y. Health-Related Quality of Life Measured by EQ-5D in Relation to Hospital Stay and Readmission in Elderly Patients Hospitalized for Acute Illness. Int. J. Environ. Res. Public Health 2020, 17, 5333. [Google Scholar] [CrossRef]
- Chao, Y.T.; Kuo, F.H.; Lee, Y.S.; Huang, Y.H.; Weng, S.C.; Chou, Y.Y.; Lin, C.S.; Lin, S.Y. Characteristics and Outcome Determinants of Hospitalized Older Patients with Cognitive Dysfunction. Int. J. Environ. Res. Public Health 2022, 19, 584. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.T.; Chang, W.Y.; Jang, Y. Psychometric and diagnostic properties of the Taiwan version of the Quick Mild Cognitive Impairment screen. PLoS ONE 2018, 13, e0207851. [Google Scholar] [CrossRef] [PubMed]
- Guo, N.W.; Liu, H.C.; Wong, P.F.; Liao, K.K.; Yan, S.H.; Lin, K.P.; Chang, C.Y.; Hsu, T.C. Chinese version and norms of the Mini-Mental State Examination. J. Rehabil. Med. Assoc. Taiwan. 1988, 16, 52–59. [Google Scholar]
- Brañez-Condorena, A.; Soriano-Moreno, D.R.; Navarro-Flores, A.; Solis-Chimoy, B.; Diaz-Barrera, M.E.; Taype-Rondan, A. Accuracy of the Geriatric Depression Scale (GDS)-4 and GDS-5 for the screening of depression among older adults: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0253899. [Google Scholar] [CrossRef]
- Vellas, B.; Villars, H.; Abellan, G.; Soto, M.E.; Rolland, Y.; Guigoz, Y.; Morley, J.E.; Chumlea, W.; Salva, A.; Rubenstein, L.Z.; et al. Overview of the MNA—Its history and challenges. J. Nutr. Health Aging 2006, 10, 456–463, discussion 463–455. [Google Scholar]
- Rubenstein, L.Z.; Harker, J.O.; Salvà, A.; Guigoz, Y.; Vellas, B. Screening for undernutrition in geriatric practice: Developing the short-form mini-nutritional assessment (MNA-SF). J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M366–M372. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Cesari, M.; Kritchevsky, S.B.; Penninx, B.W.; Nicklas, B.J.; Simonsick, E.M.; Newman, A.B.; Tylavsky, F.A.; Brach, J.S.; Satterfield, S.; Bauer, D.C.; et al. Prognostic value of usual gait speed in well-functioning older people--results from the Health, Aging and Body Composition Study. J. Am. Geriatr. Soc. 2005, 53, 1675–1680. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The barthel index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Lawton, M.P.; Brody, E.M.A. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef]
- van Walraven, C.; Dhalla, I.A.; Bell, C.; Etchells, E.; Stiell, I.G.; Zarnke, K.; Austin, P.C.; Forster, A.J. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. Cmaj 2010, 182, 551–557. [Google Scholar] [CrossRef]
- Donzé, J.; Aujesky, D.; Williams, D.; Schnipper, J.L. Potentially Avoidable 30-Day Hospital Readmissions in Medical Patients: Derivation and Validation of a Prediction Model. JAMA Intern. Med. 2013, 173, 632–638. [Google Scholar] [CrossRef]
- Fage, B.A.; Chan, C.C.; Gill, S.S.; Noel-Storr, A.H.; Herrmann, N.; Smailagic, N.; Nikolaou, V.; Seitz, D.P. Mini-Cog for the diagnosis of Alzheimer’s disease dementia and other dementias within a community setting. Cochrane Database Syst. Rev. 2015, 2, Cd010860. [Google Scholar] [CrossRef]
- Borson, S.; Scanlan, J.; Brush, M.; Vitaliano, P.; Dokmak, A. The mini-cog: A cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int. J. Geriatr. Psychiatry 2000, 15, 1021–1027. [Google Scholar] [CrossRef]
- Hoyl, M.T.; Alessi, C.A.; Harker, J.O.; Josephson, K.R.; Pietruszka, F.M.; Koelfgen, M.; Mervis, J.R.; Fitten, L.J.; Rubenstein, L.Z. Development and testing of a five-item version of the Geriatric Depression Scale. J. Am. Geriatr. Soc. 1999, 47, 873–878. [Google Scholar] [CrossRef]
- Benedetti, A.; Wu, Y.; Levis, B.; Wilchesky, M.; Boruff, J.; Ioannidis, J.P.A.; Patten, S.B.; Cuijpers, P.; Shrier, I.; Gilbody, S.; et al. Diagnostic accuracy of the Geriatric Depression Scale-30, Geriatric Depression Scale-15, Geriatric Depression Scale-5 and Geriatric Depression Scale-4 for detecting major depression: Protocol for a systematic review and individual participant data meta-analysis. BMJ Open 2018, 8, e026598. [Google Scholar] [CrossRef]
- Graf, C. The Lawton instrumental activities of daily living scale. Am. J. Nurs. 2008, 108, 52–62, quiz 62–53. [Google Scholar] [CrossRef]
- Vellas, B.; Guigoz, Y.; Garry, P.J.; Nourhashemi, F.; Bennahum, D.; Lauque, S.; Albarede, J.L. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition 1999, 15, 116–122. [Google Scholar] [CrossRef]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e302. [Google Scholar] [CrossRef] [PubMed]
- Sharma, Y.; Miller, M.; Kaambwa, B.; Shahi, R.; Hakendorf, P.; Horwood, C.; Thompson, C. Malnutrition and its association with readmission and death within 7 days and 8-180 days postdischarge in older patients: A prospective observational study. BMJ Open 2017, 7, e018443. [Google Scholar] [CrossRef] [PubMed]
- Pereira, F.; Verloo, H.; Zhivko, T.; Di Giovanni, S.; Meyer-Massetti, C.; von Gunten, A.; Martins, M.M.; Wernli, B. Risk of 30-day hospital readmission associated with medical conditions and drug regimens of polymedicated, older inpatients discharged home: A registry-based cohort study. BMJ Open 2021, 11, e052755. [Google Scholar] [CrossRef] [PubMed]
- Turnbull, A.J.; Donaghy, E.; Salisbury, L.; Ramsay, P.; Rattray, J.; Walsh, T.; Lone, N. Polypharmacy and emergency readmission to hospital after critical illness: A population-level cohort study. Br. J. Anaesth. 2021, 126, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Counter, D.; Millar, J.W.T.; McLay, J.S. Hospital readmissions, mortality and potentially inappropriate prescribing: A retrospective study of older adults discharged from hospital. Br. J. Clin. Pharmacol. 2018, 84, 1757–1763. [Google Scholar] [CrossRef]
- Pazan, F.; Wehling, M. Polypharmacy in older adults: A narrative review of definitions, epidemiology and consequences. Eur. Geriatr. Med. 2021, 12, 443–452. [Google Scholar] [CrossRef]
- Pilotto, A.; Ferrucci, L.; Franceschi, M.; D’Ambrosio, L.P.; Scarcelli, C.; Cascavilla, L.; Paris, F.; Placentino, G.; Seripa, D.; Dallapiccola, B.; et al. Development and validation of a multidimensional prognostic index for one-year mortality from comprehensive geriatric assessment in hospitalized older patients. Rejuvenation Res. 2008, 11, 151–161. [Google Scholar] [CrossRef]
- Pilotto, A.; Veronese, N.; Daragjati, J.; Cruz-Jentoft, A.J.; Polidori, M.C.; Mattace-Raso, F.; Paccalin, M.; Topinkova, E.; Siri, G.; Greco, A.; et al. Using the Multidimensional Prognostic Index to Predict Clinical Outcomes of Hospitalized Older Persons: A Prospective, Multicenter, International Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2019, 74, 1643–1649. [Google Scholar] [CrossRef]
- Hansen, T.K.; Shahla, S.; Damsgaard, E.M.; Bossen, S.R.L.; Bruun, J.M.; Gregersen, M. Mortality and readmission risk can be predicted by the record-based Multidimensional Prognostic Index: A cohort study of medical inpatients older than 75 years. Eur. Geriatr. Med. 2021, 12, 253–261. [Google Scholar] [CrossRef]
- Dodson, J.A.; Arnold, S.V.; Gosch, K.L.; Gill, T.M.; Spertus, J.A.; Krumholz, H.M.; Rich, M.W.; Chaudhry, S.I.; Forman, D.E.; Masoudi, F.A.; et al. Slow Gait Speed and Risk of Mortality or Hospital Readmission After Myocardial Infarction in the Translational Research Investigating Underlying Disparities in Recovery from Acute Myocardial Infarction: Patients’ Health Status Registry. J. Am. Geriatr. Soc. 2016, 64, 596–601. [Google Scholar] [CrossRef]
- Hertzberg, D.; Luksha, Y.; Kus, I.; Eslampia, P.; Pickering, J.W.; Holzmann, M.J. Gait Speed at Discharge and Risk for Readmission or Death: A Prospective Study of an Emergency Ward Population. Open Access Emerg. Med. 2020, 12, 127–135. [Google Scholar] [CrossRef]
- Dhillon, R.J.; Hasni, S. Pathogenesis and Management of Sarcopenia. Clin. Geriatr. Med. 2017, 33, 17–26. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Baldwin, M.; Polissar, N.L.; Gruber, W. Predicting the probability for falls in community-dwelling older adults. Phys. Ther. 1997, 77, 812–819. [Google Scholar] [CrossRef]
- Olson, C.H.; Dey, S.; Kumar, V.; Monsen, K.A.; Westra, B.L. Clustering of elderly patient subgroups to identify medication-related readmission risks. Int. J. Med. Inform. 2016, 85, 43–52. [Google Scholar] [CrossRef]
- Thunander Sundbom, L.; Bingefors, K. Women and men report different behaviours in, and reasons for medication non-adherence: A nationwide Swedish survey. Pharm. Pract. (Granada) 2012, 10, 207–221. [Google Scholar] [CrossRef]
- Han, T.S.; Fluck, D.; Fry, C.H. Validity of the LACE index for identifying frequent early readmissions after hospital discharge in children. Eur. J. Pediatr. 2021, 180, 1571–1579. [Google Scholar] [CrossRef]
- Khan, H.; Greene, S.J.; Fonarow, G.C.; Kalogeropoulos, A.P.; Ambrosy, A.P.; Maggioni, A.P.; Zannad, F.; Konstam, M.A.; Swedberg, K.; Yancy, C.W.; et al. Length of hospital stay and 30-day readmission following heart failure hospitalization: Insights from the EVEREST trial. Eur. J. Heart Fail. 2015, 17, 1022–1031. [Google Scholar] [CrossRef]
- Kaboli, P.J.; Go, J.T.; Hockenberry, J.; Glasgow, J.M.; Johnson, S.R.; Rosenthal, G.E.; Jones, M.P.; Vaughan-Sarrazin, M. Associations between reduced hospital length of stay and 30-day readmission rate and mortality: 14-year experience in 129 Veterans Affairs hospitals. Ann. Intern. Med. 2012, 157, 837–845. [Google Scholar] [CrossRef]
- Aubert, C.E.; Schnipper, J.L.; Fankhauser, N.; Marques-Vidal, P.; Stirnemann, J.; Auerbach, A.D.; Zimlichman, E.; Kripalani, S.; Vasilevskis, E.E.; Robinson, E.; et al. Patterns of multimorbidity associated with 30-day readmission: A multinational study. BMC Public Health 2019, 19, 738. [Google Scholar] [CrossRef]
- Bähler, C.; Huber, C.A.; Brüngger, B.; Reich, O. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: A claims data based observational study. BMC Health Serv. Res. 2015, 15, 23. [Google Scholar] [CrossRef]
- van Oostrom, S.H.; Picavet, H.S.; de Bruin, S.R.; Stirbu, I.; Korevaar, J.C.; Schellevis, F.G.; Baan, C.A. Multimorbidity of chronic diseases and health care utilization in general practice. BMC Fam. Pract. 2014, 15, 61. [Google Scholar] [CrossRef] [PubMed]
- van den Bussche, H.; Schön, G.; Kolonko, T.; Hansen, H.; Wegscheider, K.; Glaeske, G.; Koller, D. Patterns of ambulatory medical care utilization in elderly patients with special reference to chronic diseases and multimorbidity--results from a claims data based observational study in Germany. BMC Geriatr. 2011, 11, 54. [Google Scholar] [CrossRef]
- Lehnert, T.; Heider, D.; Leicht, H.; Heinrich, S.; Corrieri, S.; Luppa, M.; Riedel-Heller, S.; König, H.H. Review: Health care utilization and costs of elderly persons with multiple chronic conditions. Med. Care Res. Rev. 2011, 68, 387–420. [Google Scholar] [CrossRef] [PubMed]
- Breen, K.; Finnegan, L.; Vuckovic, K.; Fink, A.; Rosamond, W.; DeVon, H.A. Multimorbidity in Patients With Acute Coronary Syndrome Is Associated With Greater Mortality, Higher Readmission Rates, and Increased Length of Stay: A Systematic Review. J. Cardiovasc. Nurs. 2020, 35, E99–E110. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.M.; Wallace, E.; O’Dowd, T.; Fortin, M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst. Rev. 2021, 1, Cd006560. [Google Scholar] [CrossRef] [PubMed]
- Dobler, C.C.; Hakim, M.; Singh, S.; Jennings, M.; Waterer, G.; Garden, F.L. Ability of the LACE index to predict 30-day hospital readmissions in patients with community-acquired pneumonia. ERJ Open Res. 2020, 6, 00301-2019. [Google Scholar] [CrossRef]
- Hakim, M.A.; Garden, F.L.; Jennings, M.D.; Dobler, C.C. Performance of the LACE index to predict 30-day hospital readmissions in patients with chronic obstructive pulmonary disease. Clin. Epidemiol. 2018, 10, 51–59. [Google Scholar] [CrossRef]
- Rajaguru, V.; Kim, T.H.; Han, W.; Shin, J.; Lee, S.G. LACE Index to Predict the High Risk of 30-Day Readmission in Patients With Acute Myocardial Infarction at a University Affiliated Hospital. Front. Cardiovasc. Med. 2022, 9, 925965. [Google Scholar] [CrossRef]
- Winter, E.; Glauser, G.; Caplan, I.F.; Goodrich, S.; McClintock, S.D.; Kovach, S.J., 3rd; Fosnot, J.; Serletti, J.M.; Malhotra, N.R. LACE+ index as a predictor of 90-day plastic surgery outcomes. Am. J. Manag. Care 2020, 26, e113–e120. [Google Scholar] [CrossRef]
- Cooksley, T.; Nanayakkara, P.W.; Nickel, C.H.; Subbe, C.P.; Kellett, J.; Kidney, R.; Merten, H.; Van Galen, L.; Henriksen, D.P.; Lassen, A.T.; et al. Readmissions of medical patients: An external validation of two existing prediction scores. Qjm 2016, 109, 245–248. [Google Scholar] [CrossRef]
- Hansen, L.O.; Young, R.S.; Hinami, K.; Leung, A.; Williams, M.V. Interventions to reduce 30-day rehospitalization: A systematic review. Ann. Intern. Med. 2011, 155, 520–528. [Google Scholar] [CrossRef]
- Fried, T.R.; Bradley, E.H.; Williams, C.S.; Tinetti, M.E. Functional Disability and Health Care Expenditures for Older Persons. Arch. Intern. Med. 2001, 161, 2602–2607. [Google Scholar] [CrossRef]
- Kaegi-Braun, N.; Mueller, M.; Schuetz, P.; Mueller, B.; Kutz, A. Evaluation of Nutritional Support and In-Hospital Mortality in Patients With Malnutrition. JAMA Netw. Open 2021, 4, e2033433. [Google Scholar] [CrossRef]
- Starfield, B.; Lemke, K.W.; Herbert, R.; Pavlovich, W.D.; Anderson, G. Comorbidity and the use of primary care and specialist care in the elderly. Ann. Fam. Med. 2005, 3, 215–222. [Google Scholar] [CrossRef]
- Li, C.M.; Chen, C.Y.; Li, C.Y.; Wang, W.D.; Wu, S.C. The effectiveness of a comprehensive geriatric assessment intervention program for frailty in community-dwelling older people: A randomized, controlled trial. Arch. Gerontol. Geriatr. 2010, 50 (Suppl. S1), S39–S42. [Google Scholar] [CrossRef]
- Walston, J.; Buta, B.; Xue, Q.L. Frailty Screening and Interventions: Considerations for Clinical Practice. Clin. Geriatr. Med. 2018, 34, 25–38. [Google Scholar] [CrossRef]
- Dent, E.; Martin, F.C.; Bergman, H.; Woo, J.; Romero-Ortuno, R.; Walston, J.D. Management of frailty: Opportunities, challenges, and future directions. Lancet 2019, 394, 1376–1386. [Google Scholar] [CrossRef]
- Theou, O.; Stathokostas, L.; Roland, K.P.; Jakobi, J.M.; Patterson, C.; Vandervoort, A.A.; Jones, G.R. The effectiveness of exercise interventions for the management of frailty: A systematic review. J. Aging Res. 2011, 2011, 569194. [Google Scholar] [CrossRef]
- Cameron, I.D.; Fairhall, N.; Langron, C.; Lockwood, K.; Monaghan, N.; Aggar, C.; Sherrington, C.; Lord, S.R.; Kurrle, S.E. A multifactorial interdisciplinary intervention reduces frailty in older people: Randomized trial. BMC Med. 2013, 11, 65. [Google Scholar] [CrossRef]
- Palmer, K.; Onder, G. Comprehensive geriatric assessment: Benefits and limitations. Eur. J. Intern. Med. 2018, 54, e8–e9. [Google Scholar] [CrossRef]
- Morley, J.E. Rapid Geriatric Assessment: Secondary Prevention to Stop Age-Associated Disability. Clin. Geriatr. Med. 2017, 33, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Little, M.O. The Rapid Geriatric Assessment: A Quick Screen for Geriatric Syndromes. Mo. Med. 2017, 114, 101–104. [Google Scholar] [PubMed]
- Williams, G.R.; Deal, A.M.; Jolly, T.A.; Alston, S.M.; Gordon, B.B.; Dixon, S.A.; Olajide, O.A.; Chris Taylor, W.; Messino, M.J.; Muss, H.B. Feasibility of geriatric assessment in community oncology clinics. J. Geriatr. Oncol. 2014, 5, 245–251. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total (n = 1509) | Non-Readmitted (n = 1276) | Readmitted (n = 233) | p Value |
|---|---|---|---|---|
| Sociodemographic | ||||
| Age (years) | 82 (75–87) | 82 (75–87) | 82 (74.5–87) | 0.768 |
| Sex, n (%) | 0.040 * | |||
| Male | 929 (61.56%) | 771 (60.4%) | 158 (67.8%) | |
| Female | 580 (38.44%) | 505 (39.6%) | 75 (32.2%) | |
| Living situation, n (%) | 0.846 | |||
| Alone | 137 (9.08%) | 117 (9.2%) | 20 (8.6%) | |
| With relatives | 1230 (81.51%) | 1037 (81.3%) | 193 (82.8%) | |
| Others | 142 (9.41%) | 122 (9.6%) | 20 (8.6%) | |
| Educational level | 0.362 | |||
| Illiterate | 398 (26.38%) | 346 (27.1%) | 52 (22.3%) | |
| Literate or primary school | 576 (38.17%) | 477 (37.4%) | 99 (42.5%) | |
| Junior to senior high school | 376 (24.92%) | 317 (24.8%) | 59 (25.3%) | |
| University | 159 (10.54%) | 136 (10.7%) | 23 (9.9%) | |
| Marital status, n(%) | 0.281 | |||
| Single | 46 (3.05%) | 42 (3.3%) | 4 (1.7%) | |
| Married | 1463 (96.95%) | 1234 (96.7%) | 229 (98.3%) | |
| Age-adjusted Charlson Comorbidity Index (ACCI) | 2 (1–3) | 2 (1–3) | 3 (2–4) | 0.005 ** |
| CGA upon admission | ||||
| ADL | 50 (15–75) | 50 (15–75) | 40 (10–67.5) | 0.005 ** |
| IADL | 1 (0–4) | 2 (0–4) | 1 (0–3) | 0.008 ** |
| MMSE | 21 (15–26) | 21 (15–26) | 20 (16–26) | 0.895 |
| MNA | 21 (16.5–24) | 21 (16.5–24.5) | 19.5 (16–23.5) | 0.005 ** |
| TUG | 19.2 (13.6–27.28) | 18.8 (13.3–26.83) | 20.24 (15.37–29.95) | 0.070 |
| Mini-cog | 1 (0–1) | 1 (0–1) | 1 (0–1) | 0.279 |
| GDS | 1 (0–2) | 1 (0–2) | 1 (0–3) | 0.144 |
| 6M | 13 (9–20) | 12.7 (9–20) | 14.3 (8.88–20.19) | 0.440 |
| Gait ability | 0.001 ** | |||
| 0–1 | 1029 (68.19%) | 894 (70.1%) | 135 (57.9%) | |
| 2–3 | 269 (17.83%) | 213 (16.7%) | 56 (24.0%) | |
| 4 | 211 (13.98%) | 169 (13.2%) | 42 (18.0%) | |
| Hospital score | 4 (4–5) | 4 (4–5) | 5 (4–5) | <0.001 ** |
| Hospital score > 5 | 213 (14.12%) | 157 (12.3%) | 56 (24.0%) | <0.001 ** |
| LACE index | 11 (9–13) | 11 (9–13) | 12 (10–14) | <0.001 ** |
| LACE index > 15 | 137 (9.08%) | 97 (7.6%) | 40 (17.2%) | <0.001 ** |
| Length of stay | 10 (7–16) | 10 (7–15) | 11 (8–17) | 0.005 ** |
| Length of stay ≥ 14 | 517 (34.26%) | 424 (33.2%) | 93 (39.9%) | 0.057 |
| N of hospitalization in 6 months prior to index admission | <0.001 ** | |||
| No | 1157 (76.67%) | 998 (78.2%) | 159 (68.2%) | |
| 1 | 238 (15.77%) | 201 (15.8%) | 37 (15.9%) | |
| 2 | 70 (4.64%) | 53 (4.2%) | 17 (7.3%) | |
| ≥3 | 44 (2.92%) | 24 (1.9%) | 20 (8.6%) | |
| N of ER visits in 6 months prior to index admission | <0.001 ** | |||
| No | 385 (25.51%) | 336 (26.3%) | 49 (21.0%) | |
| 1 | 695 (46.06%) | 604 (47.3%) | 91 (39.1%) | |
| 2 | 231 (15.31%) | 194 (15.2%) | 37 (15.9%) | |
| 3 | 99 (6.56%) | 80 (6.3%) | 19 (8.2%) | |
| ≥4 | 99 (6.56%) | 62 (4.9%) | 37 (15.9%) | |
| Laboratory data | ||||
| Serum Creatinine | 1.02 (0.78–1.5) | 1 (0.76–1.48) | 1.11 (0.8–1.69) | 0.023 * |
| Serum hemoglobin | 11.2 (9.7–12.7) | 11.2 (9.7–12.7) | 10.9 (9.55–12.65) | 0.189 |
| Serum Sodium | 139 (136–141) | 139 (136–142) | 138 (135–141) | 0.045 * |
| Univariate | Multivariate (HOSPITAL Score) | Multivariate (LACE Index) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95%CI | p Value | OR | 95%CI | p Value | OR | 95%CI | p Value | |
| Age | 1.00 | (0.98–1.02) | 0.838 | 0.98 | (0.97–1.00) | 0.101 | 0.98 | (0.97–1.00) | 0.123 |
| Sex | |||||||||
| Male | ref | ref | ref | ||||||
| Female | 0.72 | (0.54–0.98) | 0.034 * | 0.67 | (0.49–0.92) | 0.012 * | 0.70 | (0.51–0.95) | 0.023 * |
| Hospital score | 1.36 | (1.21–1.53) | <0.001 ** | 1.33 | (1.17–1.50) | <0.001 ** | |||
| LACE index | 1.12 | (1.07–1.18) | <0.001 ** | 1.10 | (1.05–1.16) | <0.001 ** | |||
| Gait ability | |||||||||
| 0–1 | ref | ref | ref | ||||||
| 2–3 | 1.74 | (1.23–2.46) | 0.002 ** | 1.51 | (1.01–2.25) | 0.043 * | 1.47 | (0.99–2.19) | 0.057 |
| 4 | 1.65 | (1.12–2.41) | 0.011 * | 1.25 | (0.77–2.05) | 0.370 | 1.23 | (0.75–2.01) | 0.410 |
| Assessment upon admission | |||||||||
| ADL | 0.99 | (0.99–1.00) | 0.005 ** | 1.00 | (0.99–1.01) | 0.628 | 1.00 | (0.99–1.01) | 0.715 |
| MNA | 0.96 | (0.94–0.99) | 0.006 ** | 1.00 | (0.96–1.04) | 0.828 | 0.99 | (0.96–1.03) | 0.772 |
| Sensitivity | Specificity | |
|---|---|---|
| LACE index | ||
| 3 | 0.0% | 99.6% |
| 4 | 0.4% | 99.2% |
| 5 | 1.3% | 97.6% |
| 6 | 2.1% | 96.0% |
| 7 | 3.4% | 94.4% |
| 8 | 5.2% | 92.8% |
| 9 | 6.9% | 89.6% |
| 10 | 15.9% | 86.8% |
| 11 | 9.0% | 87.2% |
| 12 | 12.9% | 88.0% |
| 13 | 10.3% | 90.0% |
| 14 | 8.6% | 90.0% |
| 15 | 6.9% | 96.3% |
| 16 | 8.6% | 95.8% |
| 17 | 5.2% | 97.9% |
| 18 | 0.9% | 99.5% |
| 19 | 2.6% | 99.2% |
| Hospital score | ||
| 1 | 0.9% | 98.0% |
| 2 | 1.7% | 95.5% |
| 3 | 10.7% | 86.8% |
| 4 | 26.6% | 66.2% |
| 5 | 36.1% | 65.8% |
| 6 | 15.0% | 91.2% |
| 7 | 6.0% | 97.4% |
| 8 | 1.7% | 99.1% |
| 9 | 0.9% | 100% |
| 10 | 0.4% | 100% |
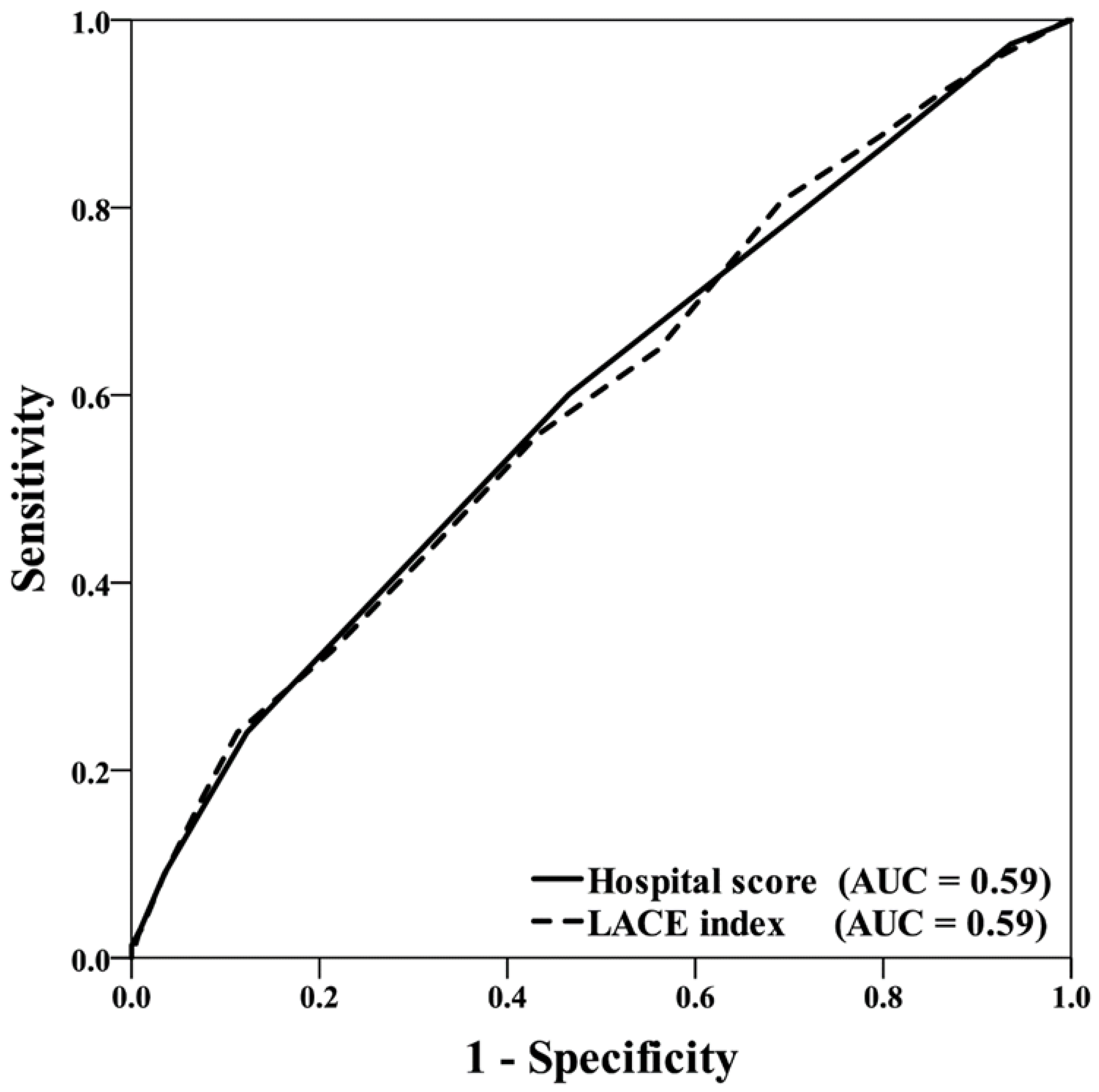
| HOSPITAL Score | LACE Index | |||||
|---|---|---|---|---|---|---|
| AUC | (95%CI) | p Value | AUC | (95%CI) | p Value | |
| Overall | 0.59 | (0.55–0.63) | <0.001 ** | 0.59 | (0.55–0.63) | <0.001 ** |
| MNA < 24 | 0.59 | (0.54–0.63) | <0.001 ** | 0.59 | (0.54–0.64) | <0.001 ** |
| MNA ≥ 24 | 0.60 | (0.52–0.67) | 0.020 * | 0.58 | (0.50–0.66) | 0.052 |
| ADL (upon admission) < 60 | 0.59 | (0.54–0.64) | <0.001 ** | 0.60 | (0.55–0.65) | <0.001 ** |
| ADL (upon admission) ≥ 60 | 0.58 | (0.51–0.65) | 0.024 * | 0.56 | (0.50–0.63) | 0.072 |
| Gait ability 0–1 | 0.58 | (0.52–0.63) | 0.003 ** | 0.57 | (0.52–0.63) | 0.005 * |
| Gait ability≥ 2 | 0.58 | (0.51–0.64) | 0.019 * | 0.58 | (0.51–0.64) | 0.017 * |
| Age < 85 | 0.58 | (0.53–0.63) | 0.002 ** | 0.58 | (0.53–0.63) | 0.002 ** |
| Age ≥ 85 | 0.62 | (0.55–0.68) | 0.001 ** | 0.61 | (0.55–0.68) | 0.001 ** |
| Male | 0.60 | (0.55–0.65) | <0.001 ** | 0.61 | (0.56–0.66) | <0.001 ** |
| Female | 0.59 | (0.51–0.66) | 0.017 * | 0.55 | (0.48–0.63) | 0.133 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, C.-H.; Chou, Y.-Y.; Lee, Y.-S.; Weng, S.-C.; Lin, C.-F.; Kuo, F.-H.; Hsu, P.-S.; Lin, S.-Y. Prediction of 30-Day Readmission in Hospitalized Older Adults Using Comprehensive Geriatric Assessment and LACE Index and HOSPITAL Score. Int. J. Environ. Res. Public Health 2023, 20, 348. https://doi.org/10.3390/ijerph20010348
Sun C-H, Chou Y-Y, Lee Y-S, Weng S-C, Lin C-F, Kuo F-H, Hsu P-S, Lin S-Y. Prediction of 30-Day Readmission in Hospitalized Older Adults Using Comprehensive Geriatric Assessment and LACE Index and HOSPITAL Score. International Journal of Environmental Research and Public Health. 2023; 20(1):348. https://doi.org/10.3390/ijerph20010348
Chicago/Turabian StyleSun, Chia-Hui, Yin-Yi Chou, Yu-Shan Lee, Shuo-Chun Weng, Cheng-Fu Lin, Fu-Hsuan Kuo, Pi-Shan Hsu, and Shih-Yi Lin. 2023. "Prediction of 30-Day Readmission in Hospitalized Older Adults Using Comprehensive Geriatric Assessment and LACE Index and HOSPITAL Score" International Journal of Environmental Research and Public Health 20, no. 1: 348. https://doi.org/10.3390/ijerph20010348
APA StyleSun, C.-H., Chou, Y.-Y., Lee, Y.-S., Weng, S.-C., Lin, C.-F., Kuo, F.-H., Hsu, P.-S., & Lin, S.-Y. (2023). Prediction of 30-Day Readmission in Hospitalized Older Adults Using Comprehensive Geriatric Assessment and LACE Index and HOSPITAL Score. International Journal of Environmental Research and Public Health, 20(1), 348. https://doi.org/10.3390/ijerph20010348






