Abstract
Pediatric weight management is often hampered by poor engagement and adherence. Incentives based on loss have been shown to be more effective than gain-based incentives in improving outcomes among children with health conditions other than obesity. In preparation for a clinical trial comparing loss-framed to gain-framed incentives, a survey of youth and caregiver attitudes on weight management incentives, reasons for program attendance, and an economic evaluation of a theoretical trial were conducted. Ninety of 835 (11%) surveys were completed by caregiver and child. The economic evaluation showed that loss-framed incentives had a preferable incremental cost-effectiveness ratio (a lower value is considered preferable) than gain-based incentives. Most youth and caregivers felt a gain incentive would be superior, agreed that the full incentive should go to the youth (vs. the caregiver), and identified “improving health” as a top reason for pursuing weight management.
1. Introduction
Childhood obesity continues to be a major health issue, with its prevalence increasing at an alarming rate during the COVID-19 pandemic [1,2,3]. Pediatric weight management programs (PWMP) have been successful at improving the weight status of youths with obesity, but adherence and poor retention are common challenges [4,5]. Incentives have been helpful in improving adherence in both adults with health conditions and risky health behavior, such as smoking cessation, diabetes management, and obesity [6,7,8,9,10]. Additionally, incentives framed as a loss where individuals are given an incentive that loses value if a person does not adhere to a task are generally more effective than incentives framed as a gain where the incentive increases [11,12,13]. Gained-frame incentives in pediatric age groups have improved outcomes in the control of Type 1 Diabetes, improved food selection, and increased physical activity [14,15,16,17,18]. While loss appears to be a more powerful motivator in adolescents than gain, loss incentives have not been tested against gain-framed incentives in pediatric weight management [19].
Given the limited information on loss versus gain incentives, our group began planning a randomized controlled trial. With the preliminary studies described in this manuscript, we sought information on youth and caregiver attitudes toward incentives, reasons for weight management program attendance, and estimates of the cost-effectiveness of gain and loss-framed incentives.
2. Materials and Methods
This preliminary project was developed to gather data to assist with the design of a randomized controlled trial (RCT). It included two phases: (1) a survey to determine caregiver and youth attitudes about incentives and weight management, and (2) a cost-effectiveness analysis based on a theoretical study design using the survey results.
2.1. The Survey
An anonymous 24-item, investigator-created, caregiver-report survey and companion 15-item patient survey (Appendix A and Appendix B) were emailed to families of youth aged 12–18 years attending the Center for Better Health and Nutrition/Healthworks! PWMP between 1 April 2020 and 3 March 2021. The program has about 3000 patient visits per year. The survey was developed by a pediatrician with the American Board of Obesity Medicine Certification and two pediatric psychologists with expertise in adherence. Additionally, the survey was reviewed by members of the Childhood Obesity Multi-Program Analysis and Study System, a national pediatric practice-based network of about 25 pediatric weight management programs [20,21,22,23]. The questions were developed to help design how the incentives would be structured for a clinical trial comparing loss and gain-framed incentives as well as gaining more insight as to why families attend the program. Three email invitations to participate were sent in June 2021. The caregiver-report survey inquired about patient demographics (age, sex, race, ethnicity, healthcare insurance type, and caretaker-reported height and weight). Both caregiver- and child-report surveys included items assessing reasons for participating in lifestyle/weight management, attitudes regarding activities that should be rewarded, incentive amounts, how incentives would be portioned between caregiver and child, and whether how incentives were framed would increase PWMP adherence. The online survey was made available in English and Spanish via the secure REDCap platform. The study was approved by the Cincinnati Children’s Hospital Internal Review Board.
2.2. Theoretical Economic Evaluation
A decision analytic model was developed to compare the 6-month outcomes associated with three possible interventions: a control group (CG), a gain-framed incentive group (GG), and a loss-framed incentive group (LG). In the theoretical trial, all participants will receive a Fitbit tracker and internet-compatible electronic scale. Those in the control group will receive USD 10 per month regardless of participation. Youths in the GG and LG will receive a reward each month of a dollar amount equal to their adherence index. Those in the GG will have a virtual account that starts out at USD 0 each month and increases up to USD 100, depending on adherence. Those in the LG will have a virtual account that starts out at USD 100 and may decrease to as low as USD 0, depending on their adherence. The incentive scheme is summarized in Table 1.

Table 1.
Adherence Index/Incentive Scheme.
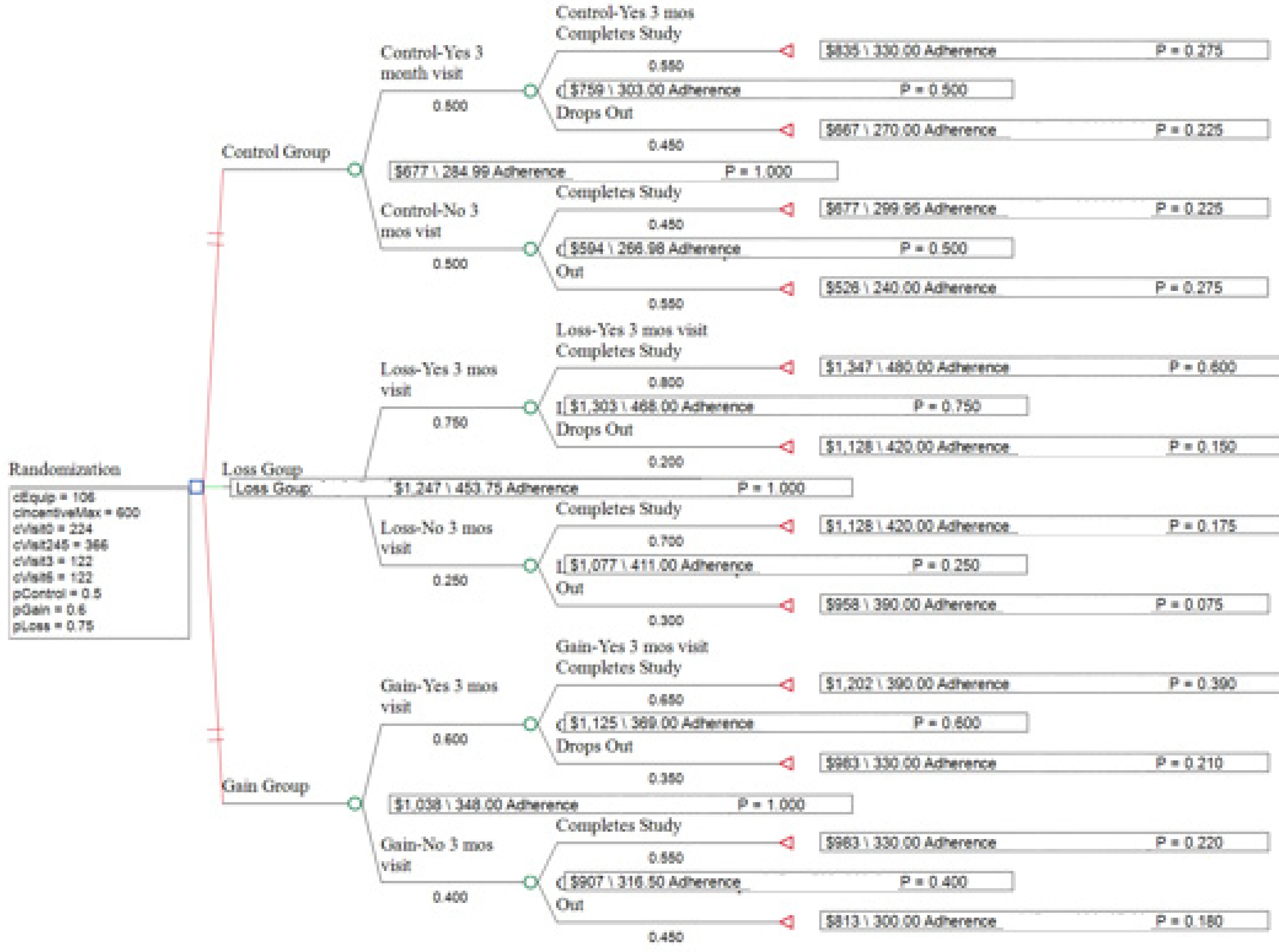
The hypothetical cohort included 60 youth (aged 12 to 18 years) with obesity. Following randomization, youth were classified as “attending a 3-month visit” or “not attending a 3-month visit.” After 3 months, youth in both categories could be classified as “completed study” or “dropped out” (see Figure 1). The probability of transitioning to each of these states was estimated from previous literature based on adult data by Patel et al. in comparing loss versus gain incentives in improving physical activity in cardiac patients and from adherence data from pediatric weight management clinics without the use of incentives (Table 2) [24,25,26].
Figure 1.
The TreeAge Diagram of the Study Strategies. Branches represent group randomization, the likelihood to keep the 3-month visit, and then completing study. Each branch has cost, adherence, and predicted probability.

Table 2.
Definitions and assumptions made for hypothetical cost-effective analysis.
Health outcome. The health outcome of interest (denominator of the ICER) was adherence as measured via an adherence index developed to rate the level of participation of all those enrolled in the study with input from a dietitian, an exercise physiologist, physicians, and psychologists (Table 1).
Additional assumptions are listed in Table 2. Costs are summarized in Table 3, with costs of equipment obtained from the purchase invoice and estimates of medical, dietitian, and exercise physiologist obtained from Medicare reimbursement on Clearhealthcosts.com [27].

Table 3.
Projected study costs.
2.3. Statistical Analysis
For the survey, descriptive statistics and comparisons of caregiver and youth responses were carried out using IBM® SPSS software (Armonk, NY, USA). For Likert scale responses, variables were dichotomized to 4, 5 vs. 1, 2, 3 and comparisons were made using chi-square analysis. For ranked order responses, differences were tested with Wilcoxon Rank Order analysis. Survey response data were dichotomized for questions with a Likert Scale response and the question on the reason for attending the program for ease of interpretation. A P value of less than 0.05 was considered significant. The effect size for differences between caretakers and youths was calculated as Eta-squared. A value of 0.01 to 0.059 was considered a small effect or association, 0.06 to 0.139 a medium effect, and greater than 0.14 a large effect. A sample size of 71 to 90 was determined using published criteria for a survey with a sampling error of 95% [28].
A decision tree for the study was created using TreeAge Pro 2022 software (Copyright 1988–2022 TreeAge Software, LLC, Williamstown, MA, USA) and the randomization process of the study protocol. The provider costs of visits 2, 4, and 5 were bundled together, as the probability of each of the visits was assumed to be equal for all branches in the analysis. A cost-effective analysis was estimated using the hypothesized values and one-way sensitivity analyses were performed varying the probability of adherence in the CG, LG, and GG by 10% higher and lower and for the maximum incentive with a range of USD 300 to USD 1200 for the entire study.
3. Results
3.1. Survey Results
In total, 90 of 835 (11%) surveys were returned. Most youths (55%) identified as Non-Hispanic White per caregiver report, with the remaining youth identifying as Black or African American (31%), Hispanic or Latino White (8%) and other (4%) per caregiver report. Sixty percent of families were insured through Medicaid. Youth’s mean age was 14.2 ± 1.8 years and mean percent of 95th percentile body mass index (BMI) was 128% ± 32%. Of the caregivers completing the survey, 88% were mothers, 3% were fathers, and 8% were other. Table 4 summarizes the results of the two top reasons listed by youths and their caregivers for attending the PWMP.

Table 4.
Reasons for participation in PWMP (ranked either most or 2nd most important).
Most youth and their caregivers chose “improve health” as one of their top responses. Table 5 shows youth and caregiver responses to attitudes on potential incentives and framing approaches. Most youths and caregivers favored most or all the reward going to the youths and believed the incentive would motivate attending clinic, meeting exercise step goals, and food logging.

Table 5.
Attitudes about incentives and overall health.
3.2. Economic Evaluation
Figure 1 shows the decision tree generated by TreeAge Software and Table 6 summarizes the costs, effectiveness, and cost-effectiveness of the three study strategies based on the assumptions made in Table 2. While the control group was the least expensive intervention, the loss group had a lower incremental cost-effectiveness ratio (ICER) than the gain group.

Table 6.
Costs, Effectiveness, and Cost-Effectiveness of Loss, Gain, and Control Groups Relative to Control.
4. Discussion
With our study, we present preliminary data for developing a reward scheme for a study of loss- and gain-framed incentives for patients enrolled in a PWMP. Using assumptions based on adherence and loss and gain incentive studies of other conditions, we conducted a hypothetical cost-effectiveness analysis which suggests that loss incentives may lead to better adherence and result in lower costs per improvement in adherence.
According to the survey responses, youths preferred compensation rates of about USD 1 per day for meeting daily physical activity and food logging goals and USD 30 per month for clinic visit attendance. Both caregivers and youth preferred that all the rewards go to the child. These findings are in contrast to those reported by Wright et al. in which a survey of parents of children in PWMP suggested the reward should be split evenly between parent and child for PWMP [29]. Contrary to Prospect Theory, which suggests loss is a more powerful motivator than gain, most of the youth and parents in our study believed that gain incentives will be more effective than loss incentives [30]. Similar to our findings, parents in the survey reported by Wright favored a gain-framed incentive [29]. Consistent with our results, Goldsmith et al. in a series of lab experiments in undergraduates and adults, demonstrated that while loss incentives were more motivating than gain incentives, participants falsely predicted that gain incentives would be more motivating than loss incentives [31]. Goldsmith suggests that a biased belief in a positive correlation between enjoyment and task motivation is the cause of the participants’ incorrect prediction. Guided by our survey results, we designed the incentive to be up to USD 30 for a clinical visit, USD 1 for food log reporting, and USD 1 for meeting the step goal, with the entire incentive going to the youths participating in the economic analysis of the planned study. Additionally, of interest is that the majority of youths and caregivers in our study endorsed, “improve health” as one of the top two reasons for PWMP attendance. More youths than caregivers selected, “improve appearance”.
There are several limitations to our study. The survey response rate was only 11%, and results were derived from a single center, limiting generalizability and thus the results should be interpreted with caution. Additionally, weight, height, insurance status and race/ethnicity were self-report and we do not have comparison data for survey non-responders. A comparison with demographic data from a recent study from our center in 2020, suggests our sample had a larger percentage of white patients (55% versus 52%), and was somewhat higher socio-economic status based on a lower percentage of Medicaid insurance (60% versus 65%) [32]. Additionally, since the survey was anonymous, we do not have data reflecting program engagement such as the number of visits, length of time in the program, or show rate for clinic visits. It should be mentioned there is some discordance between caretaker results and their children. In constructing the incentive framework, we considered both youth and parent responses. With the economic evaluation of a simulated trial, there were multiple assumptions made that may not be the case in an actual clinical trial. Additionally, in the economic evaluation, the probabilities and visit costs were largely based on adult incentive studies and Medicare reimbursement data.
5. Conclusions
Youth with obesity participating in a PWMP and their caregivers report that incentives will motivate participation in all three major aspects of weight management. Contrary to behavioral economic theory, youth and their parents believe gain incentives are likely to be more effective than loss incentives. The results of our cost-effectiveness analysis suggest that loss-framed incentives may incur fewer costs per improvement in adherence. Additional research is needed to see if a loss or gain incentive is superior in improving adherence and to test the assumptions of our economic model. A randomized controlled trial comparing loss and gain-framed incentives to control is being conducted by our research group.
Author Contributions
Conceptualization—R.S., L.D., M.E.M. and N.A.K.; Methodology—R.S., L.D., M.E.M., N.A.K., R.K. and K.S.; Formal analysis—R.S., M.E.M., N.A.K. and F.S.; Resources—P.C.; Data curation—P.C.; Supervision—R.S.; Original draft preparation—R.S. and F.S.; Writing review and editing—R.S., R.K., K.S., M.E.M., L.D., P.C., F.S. and N.A.K.; Funding acquisition—R.S., M.E.M., L.D., N.A.K., R.K. and K.S. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported in part by a Place Outcomes Award from Cincinnati Children’s Hospital.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Cincinnati Children’s Hospital, protocol 2021-0085.
Informed Consent Statement
Given the low-risk nature of this project, completion of the survey was considered implicit consent.
Data Availability Statement
As per the policy of the Cincinnati Institutional Review Board, the survey data for this study is not publicly available.
Acknowledgments
We gratefully acknowledge the help of the Heart Institute Research Core in developing the study database and providing regulatory, data collection and management support, the members of the COMPASS Network for their review of the survey, and Peter Mallow for his instruction and review of the economic evaluation.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A. Parent/Guardian Survey
- My child is seen in the clinic at
- Cincinnati Children’s
- 2.
- My child’s sex is
- Female
- Male
- 3.
- My relationship with my child is:
- ○
- Mother
- ○
- Father
- ○
- Other type of guardian
- 4.
- My child is ___years old: drop down with
- 12
- 13
- 14
- 15
- 16
- 17
- 5.
- My child’s race is:
- White
- Black or African American
- Asian
- Native Hawaiian or other Pacific Islander
- American Indian or Alaska Native
- Other
- 6.
- Is your child Hispanic or Latino?
- Yes
- No
- Don’t know/not sure
- 7.
- About how tall is your child (drop down with Feet and Inches)
- 8.
- About how much does your child weigh in pounds (drop down)
- 9.
- What type of insurance does your child have?
- Medicaid
- Private Insurance
- Self-pay or none
- Other
- 10.
- What is your highest grade or year of school you have completed?
- Never attended school or only attended kindergarten
- Grades 1 through 8 (elementary)
- Grades 9 through 11 (some high school)
- Grade 12 or GED (high school graduate)
- College 1 year to 3 years (some college or technical school)
- College 4 years or more (college graduate)
- 11.
- The reasons that I want my child to take part in a weight management program are (please rank in order of importance):
__Improve my child’s health
__Get fitter or stronger
__Improve my child’s appearance
__Improve my child’s weight status
__Keep up with friends or family during sports or other activities
__I don’t want my child to participate in a weight management program
__Other:_________________
- 12.
- How concerned are you about your child’s health on a scale from 1 to 5? Pick one.
__1 (not concerned at all)
__2 (slightly concerned)
__3 (neutral)
__4 (very concerned)
__5 (extremely concerned)
Imagine your child is participating in a weight management program where they “earn” money by doing different things to take care of your health or weight. We want to learn about how you would feel about different parts of the program. Please tell us how much you agree or disagree with the following statements.
- 13.
- Please tell us how much you agree or disagree with the following statement: “Earning a reward would make it more likely for my child to come to a weight management clinic.”
- Strongly agree
- Agree
- Unsure (Neither agree or disagree)
- Disagree
- Strongly disagree
- 14.
- How much do you think your child should earn each time they come to their regular clinic visit?
- $0 (I do not think my child should earn rewards for coming to clinic)
- $10
- $20
- $30
- $40
- $50
- 15.
- How much do you agree or disagree with the following statement? “Earning a money reward would make my child more likely to exercise or be more physically active so that they can meet their goals.”
- Strongly agree
- Agree
- Unsure (Neither agree or disagree)
- Disagree
- Strongly disagree
- 16.
- How much do you think your child should earn each day that they meet their exercise or physical activity goal?
- $0 per day (I do not think my child should earn rewards for meeting their exercise or physical activity goal)
- $0.25 per day
- $0.50 per day
- $0.75 per day
- $1.00 per day
- 17.
- How much do you agree or disagree with the following statement? “Earning a reward would make my child more likely to fill out a short food dairy each day about what they have eaten.”
- Strongly agree
- Agree
- Neither agree or disagree
- Disagree
- Strongly disagree
- 18.
- How much do you think your child should earn each day that they fill out their food diary about eating?
- $0 per day (I do not think my child should earn rewards for filling out an food diary)
- $0.25 per day
- $0.50 per day
- $0.75 per day
- $1.00 per day
- 19.
- There are different ways that we could split up the reward between you and your child. Which would you like best?
- I get all of the reward
- I get most of the reward and my child gets the rest
- I get half of the reward and my child gets half
- My child gets most of the reward and I get the rest
- My child gets all of the reward
- 20.
- Imagine that in this program, you and your child split the reward. If this is how the rewards worked, would you want to participate?
- Yes
- No
If NO—Why not? What would be bad or hard about splitting the reward?
_____________________________________________________
- 21.
- Imagine you are participating in a program where your child could earn a different amount of money for doing the activities mentioned at the beginning of the survey (going to clinic, exercising, completing food diary questions). We want to know which activity you think your child should earn the most money for. Please rank the activities below by numbering them 1, 2, and 3, with 1 for the most money earned and 3 for the least money earned.
____Meeting a daily exercise goal
____Filling out a food diaryabout the amount of fruits, vegetables and sugary drinks they have each day
____Coming to my weight management clinic appointments
- 22.
- There are different ways your child could earn rewards. Which would motivate your child the most?
- A program where your child starts with nothing and earns money each time they come to clinic, meet their exercise goal, or fill out a food diary about what they are eating. For example, your child starts with $0 and can earn up to $50 in a month.
- A program where your child starts with the biggest possible reward and loses money each time they do not come to clinic, meet their exercise goal, or fill out a food diary about what they are eating. For example, your child starts with $50 and could end up with $0 to $50 in a month, depending on how much money they lose.
- I would prefer both reward programs the same amount.
- I would not prefer either of these reward programs.
- 23.
- Is there anything else we could do to make you and your child want to participate more in a weight management program?
- 24.
- Is there anything else we should think about as we design this program, especially in terms of rewards?
Appendix B. Patient Survey
- Kids like you take part in a weight management program for different reasons. We want to know what reasons are important to YOU. Please rank the reasons below from 1 (most important) to 5 (least important) to tell us why you might want to take part in a weight management program:
__Improve my health
__Get fitter or stronger
__Improve my appearance
__Change my weight
__Keep up with friends or family during sports or other activities
__Have help with my eating or exercise goals
__I don’t want to participate in a weight management program
__Other:_________________
- 2.
- How concerned are you about your health or weight on a scale from 1 to 5? Pick one.
__1 (not concerned at all)
__2 (slightly concerned)
__3 (neutral)
__4 (very concerned)
__5 (extremely concerned)
Imagine you are participating in a weight management program where you “earn” money by doing different things to take care of your health or weight. We want to learn about how you would feel about different parts of the program. Please tell us how much you agree or disagree with the following statements.
- 3.
- How much you agree or disagree with this statement: “Earning a reward would make me more likely to come to a weight management clinic.”
- Strongly agree
- Agree
- Unsure (Neither agree or disagree)
- Disagree
- Strongly disagree
- 4.
- How much do you think you should earn each time you come to your regular clinic visit?
- $0 (I do not think I should earn rewards for coming to clinic)
- $10
- $20
- $30
- $40
- $50
- 5.
- How much do you agree or disagree with this statement: “Earning a reward would make me more likely to exercise or be more physically active.”
- Strongly agree
- Agree
- Unsure (Neither agree or disagree)
- Disagree
- Strongly disagree
- 6.
- How much do you think you should earn each day that you meet your exercise or physical activity goal?
- $0 per day (I do not think I should earn rewards for meeting my exercise or physical activity goal)
- $0.25 per day
- $0.50 per day
- $0.75 per day
- $1.00 per day
- 7.
- How much do you agree or disagree with this statement: “Earning a reward would make me more likely to fill out a short food diary each day about what I’ve eaten.”
- Strongly agree
- Agree
- Unsure (Neither agree or disagree)
- Disagree
- Strongly disagree
- 8.
- How much do you think you should earn each day that you fill out a short food diary about your eating?
- $0 per day (I do not think I should earn rewards for filling out a food diary)
- $0.25 per day
- $0.50 per day
- $0.75 per day
- $1.00 per day
- 9.
- There are different ways that we could split up the rewards you earn between you and your parent or guardian. Which would YOU like best?
- I get all of the reward
- I get most of the reward and my parent/guardian gets the rest
- I get half of the reward and my parent/guardian gets half
- My parent/guardian gets most of the reward and I get the rest
- My parent/guardian gets all of the reward
- 10.
- Imagine that in this program, you and your parent/guardian were asked to split the reward you earned. If this is how the rewards worked, would you want to participate?
- Yes
- No
If NO, why not? What would be bad or hard about splitting the reward?
_____________________________________________________
- 11.
- Imagine you are participating in a program where you could earn a different amount of money for doing the activities mentioned at the beginning of the survey (going to clinic, exercising, completing a short food diary each day). We want to know which activity you think you should earn the most money for. Please rank the activities below by numbering them 1, 2, and 3, with 1 for the most money earned and 3 for the least money earned.
____Meeting a daily exercise
____Filling out a short food diary about the number of fruits, vegetables, and sugary drinks I have each day
____Coming to my weight management clinic appointments
- 12.
- It can be difficult to share how much we exercise and what we eat, especially if it means losing a reward. Imagine you were in a study where you were asked about how much you exercise and what you eat every day and could earn or lose rewards based on your answers. How difficult do you think it would be to tell the researchers exactly what you did?
- Not at all difficult
- A little difficult
- Fairly difficult
- Very difficult
- Extremely difficult
- 13.
- There are different ways you could earn rewards. Which would motivate you the most?
- A program where I start with nothing and earn money each time I come to clinic, exercise, and fill out a food diary about what I’m eating. For example, I start with $0 and can earn up to $50 in a month.
- A program where I start with the biggest possible reward and lose money each time I do not come to clinic, exercise, or fill out a food diary about what I’m eating. For example, I start with $50 and end up with $0 to $50 in a month, depending on how much I lose.
- I would prefer both reward programs the same amount.
- I would not prefer either of these reward programs.
- 14.
- Is there anything else we could do to make you want to participate more in a weight management program?
- 15.
- Is there anything else we should think about as we design this program, especially in terms of rewards?
References
- Lange, S.J.; Kompaniyets, L.; Freedman, D.S.; Kraus, E.M.; Porter, R.; Blanck, H.M.; Goodman, A.B. Longitudinal trends in body mass index before and during the COVID-19 pandemic among persons aged 2–19 years—United States, 2018–2020. Morb. Mortal. Wkly. Rep. 2021, 70, 1278. [Google Scholar] [CrossRef]
- Siegel, R.; Khoury, P.; Spooner, S.A.; Stackpole, K.; Allen, N.; Kirk, S.; Kharofa, R. Body mass index increased at a large midwestern children’s hospital during the COVID-19 pandemic. Child. Obes. 2022. [Google Scholar] [CrossRef]
- Woolford, S.J.; Sidell, M.; Li, X.; Else, V.; Young, D.R.; Resnicow, K.; Koebnick, C. Changes in body mass index among children and adolescents during the COVID-19 pandemic. Jama 2021, 326, 1434–1436. [Google Scholar] [CrossRef]
- Denzer, C.; Reithofer, E.; Wabitsch, M.; Widhalm, K. The outcome of childhood obesity management depends highly upon patient compliance. Eur. J. Pediatr. 2004, 163, 99–104. [Google Scholar] [CrossRef]
- Zeller, M.; Kirk, S.; Claytor, R.; Khoury, P.; Grieme, J.; Santangelo, M.; Daniels, S. Predictors of attrition from a pediatric weight management program. J. Pediatr. 2004, 144, 466–470. [Google Scholar] [CrossRef]
- Gibson, D.G.; Ochieng, B.; Kagucia, E.W.; Were, J.; Hayford, K.; Moulton, L.H.; Levine, O.S.; Odhiambo, F.; O’Brien, K.L.; Feikin, D.R. Mobile phone-delivered reminders and incentives to improve childhood immunisation coverage and timeliness in Kenya (M-SIMU): A cluster randomised controlled trial. Lancet Glob. Health 2017, 5, e428–e438. [Google Scholar] [CrossRef]
- Paul-Ebhohimhen, V.; Avenell, A. Systematic review of the use of financial incentives in treatments for obesity and overweight. Obes. Rev. 2008, 9, 355–367. [Google Scholar] [CrossRef]
- Tulsky, J.P.; Pilote, L.; Hahn, J.A.; Zolopa, A.J.; Burke, M.; Chesney, M.; Moss, A.R. Adherence to isoniazid prophylaxis in the homeless: A randomized controlled trial. Arch. Intern. Med. 2000, 160, 697–702. [Google Scholar] [CrossRef]
- Volpp, K.G.; John, L.K.; Troxel, A.B.; Norton, L.; Fassbender, J.; Loewenstein, G. Financial incentive–based approaches for weight loss: A randomized trial. Jama 2008, 300, 2631–2637. [Google Scholar] [CrossRef]
- Wall, J.; Mhurchu, C.N.; Blakely, T.; Rodgers, A.; Wilton, J. Effectiveness of monetary incentives in modifying dietary behavior: A review of randomized, controlled trials. Nutr. Rev. 2006, 64, 518–531. [Google Scholar] [CrossRef]
- Chokshi, N.P.; Adusumalli, S.; Small, D.S.; Morris, A.; Feingold, J.; Ha, Y.P.; Lynch, M.D.; Rareshide, C.A.; Hilbert, V.; Patel, M.S. Loss-framed financial incentives and personalized goal-setting to increase physical activity among ischemic heart disease patients using wearable devices: The ACTIVE REWARD randomized trial. J. Am. Heart Assoc. 2018, 7, e009173. [Google Scholar] [CrossRef]
- Romanowich, P.; Lamb, R. The effect of framing incentives as either losses or gains with contingency management for smoking cessation. Addict. Behav. 2013, 38, 2084–2088. [Google Scholar] [CrossRef]
- Vajravelu, M.E.; Hitt, T.A.; Mak, N.; Edwards, A.; Mitchell, J.; Schwartz, L.; Kelly, A.; Amaral, S. Text messages and financial incentives to increase physical activity in adolescents with prediabetes and type 2 diabetes: Web-based group interviews to inform intervention design. JMIR Diabetes 2022, 7, e33082. [Google Scholar] [CrossRef]
- Corepal, R.; Tully, M.A.; Kee, F.; Miller, S.J.; Hunter, R.F. Behavioural incentive interventions for health behaviour change in young people (5–18 years old): A systematic review and meta-analysis. Prev. Med. 2018, 110, 55–66. [Google Scholar] [CrossRef]
- Hudgens, M.E.; Barnes, A.S.; Lockhart, M.K.; Ellsworth, S.C.; Beckford, M.; Siegel, R.M. Small prizes improve food selection in a school cafeteria without increasing waste. Clin. Pediatr. 2017, 56, 123–126. [Google Scholar] [CrossRef]
- Short, K.R.; Chadwick, J.Q.; Cannady, T.K.; Branam, D.E.; Wharton, D.F.; Tullier, M.A.; Thompson, D.M.; Copeland, K.C. Using financial incentives to promote physical activity in American Indian adolescents: A randomized controlled trial. PloS ONE 2018, 13, e0198390. [Google Scholar] [CrossRef]
- Wagner, J.A.; Petry, N.M.; Weyman, K.; Tichy, E.; Cengiz, E.; Zajac, K.; Tamborlane, W.V. Glucose management for rewards: A randomized trial to improve glucose monitoring and associated self-management behaviors in adolescents with type 1 diabetes. Pediatr. Diabetes 2019, 20, 997–1006. [Google Scholar] [CrossRef]
- Wong, C.A.; Miller, V.A.; Murphy, K.; Small, D.; Ford, C.A.; Willi, S.M.; Feingold, J.; Morris, A.; Ha, Y.P.; Zhu, J.; et al. Effect of financial incentives on glucose monitoring adherence and glycemic control among adolescents and young adults with type 1 diabetes: A randomized clinical trial. JAMA Pediatr. 2017, 171, 1176–1183. [Google Scholar] [CrossRef]
- Cho, H.; Boster, F.J. Effects of gain versus loss frame antidrug ads on adolescents. J. Commun. 2008, 58, 428–446. [Google Scholar] [CrossRef]
- Moore, J.; Haemer, M.; Mirza, N.; Z Weatherall, Y.; Han, J.; Mangarelli, C.; Hawkins, M.J.; Xanthakos, S.; Siegel, R. Pilot testing of a patient decision aid for adolescents with severe obesity in US pediatric weight management programs within the COMPASS network. Int. J. Environ. Res. Public Health 2019, 16, 1776. [Google Scholar] [CrossRef]
- Phan, T.-L.T.; Tucker, J.M.; Siegel, R.; Christison, A.L.; Stratbucker, W.; Werk, L.N.; Hossain, J.; Datto, G.; Gentile, D.A.; Stubblefield, S. Electronic gaming characteristics associated with class 3 severe obesity in youth who attend the pediatric weight management programs of the COMPASS Network. Child. Obes. 2019, 15, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.; Fals, A.; Mirza, N.; Datto, G.; Stratbucker, W.; Ievers-Landis, C.E.; Christison, A.; Wang, Y.; Woolford, S.J. Social/electronic media use of children and adolescents who attend the pediatric weight management programs of the compass network. Child. Obes. 2015, 11, 624–629. [Google Scholar] [CrossRef] [PubMed]
- Stubblefield, S.; Datto, G.; Phan, T.-L.T.; Werk, L.N.; Stackpole, K.; Siegel, R.; Stratbucker, W.; Tucker, J.M.; Christison, A.L.; Hossain, J.; et al. Problem video gaming among children enrolled in tertiary weight management programs. Cyberpsychology Behav. Soc. Netw. 2017, 20, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.S.; Asch, D.A.; Rosin, R.; Small, D.S.; Bellamy, S.L.; Heuer, J.; Sproat, S.; Hyson, C.; Haff, N.; Lee, S.M.; et al. Framing financial incentives to increase physical activity among overweight and obese adults: A randomized, controlled trial. Ann. Intern. Med. 2016, 164, 385–394. [Google Scholar] [CrossRef]
- Siegel, R.M.; Neidhard, M.S.; Kirk, S. A comparison of low glycemic index and staged portion-controlled diets in improving BMI of obese children in a pediatric weight management program. Clin. Pediatr. 2011, 50, 459–461. [Google Scholar] [CrossRef]
- Skelton, J.; Beech, B. Attrition in paediatric weight management: A review of the literature and new directions. Obes. Rev. 2011, 12, e273–e281. [Google Scholar] [CrossRef]
- Clearhealthcosts. Available online: https://clearhealthcosts.com/ (accessed on 21 December 2022).
- Price, J.H.; Daek, J.A.; Murnan, J.; Dimmig, J.; Akpanudo, S. Power analysis in survey research: Importance and use for health educators. Am. J. Health Educ. 2005, 36, 202–209. [Google Scholar] [CrossRef]
- Wright, D.R.; Saelens, B.E.; Fontes, A.; Lavelle, T.A. Assessment of parents’ preferences for incentives to promote engagement in family-based childhood obesity treatment. JAMA Netw. Open 2019, 2, e191490. [Google Scholar] [CrossRef]
- Tversky, A.; Kahneman, D. Loss aversion in riskless choice: A reference-dependent model. Q. J. Econ. 1991, 106, 1039–1061. [Google Scholar] [CrossRef]
- Goldsmith, K.; Dhar, R. Negativity bias and task motivation: Testing the effectiveness of positively versus negatively framed incentives. J. Exp. Psychol. Appl. 2013, 19, 358. [Google Scholar] [CrossRef]
- Siegel, R.; Stackpole, K.; Kirk, S.; Kharofa, R. Families chose in-person visits over telehealth for pediatric weight management during the COVID-19 pandemic. Child. Obes. 2022, 18, 572–575. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).