Flapless Decoronation: A Minimally Invasive Approach
Abstract
:1. Introduction
2. Materials and Methods
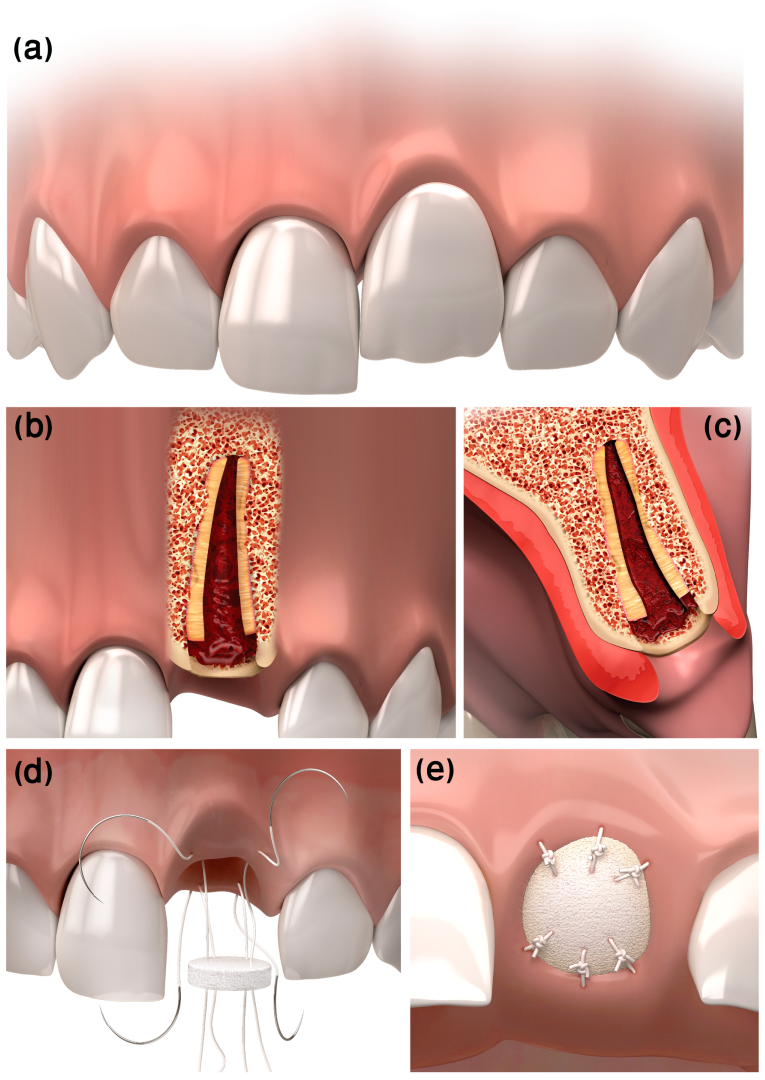
2.1. Description of the Technique
2.1.1. Ethical Considerations
2.1.2. Indications and Contra-Indications for Decoronation
- Age 7–10 (early mixed dentition)—decoronation should be performed within two years.
- Age 10–12 (late mixed dentition)—requires individual monitoring, since a rapid infraposition rate is expected when the patient reaches the pubertal growth spurt; decoronation is indicated upon infraposition diagnosis.
2.1.3. Clinical Procedure
3. Technique Demonstration
3.1. Case 1
- Dental history
- Clinical procedure
- Follow-up
3.2. Case 2
- Dental history
- Clinical procedure
- Follow-up
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Andreasen, J.; Ravn, J. Epidemiology of traumatic dental injuries to primary and permanent teeth in a Danish population sample. Int. J. Oral Surg. 1972, 1, 235–239. [Google Scholar] [CrossRef] [PubMed]
- Ravn, J.J. Dental injuries in Copenhagen schoolchildren, school years 1967-1972. Community Dent. Oral Epidemiol. 1974, 2, 231–245. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Bakland, L.K.; Matras, R.C.; Andreasen, F.M. Traumatic intrusion of permanent teeth. Part 1. An epidemiological study of 216 intruded permanent teeth. Dent. Traumatol. 2006, 22, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Borssen, E.; Holm, A.-K. Traumatic dental injuries in a cohort of 16-year-olds in northern Sweden. Dent. Traumatol. 1997, 13, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Fouad, A.F.; Abbott, P.V.; Tsilingaridis, G.; Cohenca, N.; Lauridsen, E.; Bourguignon, C.; O’Connell, A.; Flores, M.T.; Day, P.F.; Hicks, L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent. Traumatol. 2020, 36, 331–342. [Google Scholar] [CrossRef]
- Malmgren, B. Ridge Preservation/Decoronation. J. Endod. 2013, 39, S67–S72. [Google Scholar] [CrossRef]
- Albertsson, J.; Lauridsen, E.; Andreasen, J.O.; Gerds, T.A.; Andersson, L. The risks of ankylosis of 89 avulsed human teeth stored in saliva prior to replantation—A re-evaluation of a long-term clinical study. Dent. Traumatol. 2021, 37, 537–545. [Google Scholar] [CrossRef]
- Andersson, L.; Bodin, I.; Sorensen, S. Progression of root resorption following replantation of human teeth after extended extraoral storage. Dent. Traumatol. 1989, 5, 38–47. [Google Scholar] [CrossRef]
- Lin, S.; Schwarz-Arad, D.; Ashkenazi, M. Alveolar Bone Width Preservation after Decoronation of Ankylosed Anterior Incisors. J. Endod. 2013, 39, 1542–1544. [Google Scholar] [CrossRef]
- Malmgren, B.; Cvek, M.; Lundberg, M.; Frykholm, A. Surgical treatment of ankylosed and infrapositioned reimplanted incisors in adolescents. Eur. J. Oral Sci. 1984, 92, 391–399. [Google Scholar] [CrossRef]
- Gound, T.; O’Neal, R.B.; del Rio, C.E.; Levin, M.P. Submergence of roots for alveolar bone preservation: II. Reimplanted endodontically treated roots. Oral Surg. Oral Med. Oral Pathol. 1978, 46, 114–122. [Google Scholar] [CrossRef]
- O’Neal, R.B.; Gound, T.; Levin, M.P.; del Rio, C.E. Submergence of roots for alveolar bone preservation: I. Endodontically treated roots. Oral Surg. Oral Med. Oral Pathol. 1978, 45, 803–810. [Google Scholar] [CrossRef]
- Agel, M.; Alani, A. The paediatric dentistry-restorative dentistry interface. Br. Dent. J. 2022, 233, 475–482. [Google Scholar] [CrossRef]
- Malmgren, B. Decoronation: How, why, and when? J. Calif. Dent. Assoc. 2000, 28, 846–854. [Google Scholar]
- Malmgren, B.; Malmgren, O. Rate of infraposition of reimplanted ankylosed incisors related to age and growth in children and adolescents. Dent. Traumatol. 2002, 18, 28–36. [Google Scholar] [CrossRef] [Green Version]
- Malmgren, B.; Tsilingaridis, G.; Malmgren, O. Long-term follow up of 103 ankylosed permanent incisors surgically treated with decoronation—A retrospective cohort study. Dent. Traumatol. 2015, 31, 184–189. [Google Scholar] [CrossRef]
- Lakshmi, M.R.; Gottumukkala, S.N.V.S.; Penmetsa, G.S.; Ramesh, K.S.V.; Kumar, P.M.; Vamsi, E.S.; Mounica, M.B. Clinical outcomes of root coverage using porcine-derived collagen matrix with modified coronally advanced tunnel technique (MCAT) in multiple gingival recessions in smokers—A randomized controlled clinical trial. Clin. Oral Investig. 2022, 1–11. [Google Scholar] [CrossRef]
- Liu, C.-J.; Fang, K.-H.; Chang, C.-C.; Lin, E.-T.; Chang, G.-H.; Shen, J.-H.; Chen, Y.-T.; Tsai, Y.-T. Application of “parachute” technique for free flap reconstruction in advanced tongue cancer after ablation without lip-jaw splitting: A retrospective case study. Medicine 2019, 98, e16728. [Google Scholar] [CrossRef]
- Miller, S.C. Textbook of Periodontia (Oral Medicine), 3rd ed.; Blakiston: Philadelphia, PA, USA, 1950; p. xviii. 900p. [Google Scholar]
- Jung, R.E.; Philipp, A.; Annen, B.M.; Signorelli, L.; Thoma, D.; Hämmerle, C.H.; Attin, T.; Schmidlin, P.R. Radiographic evaluation of different techniques for ridge preservation after tooth extraction: A randomized controlled clinical trial. J. Clin. Periodontol. 2012, 40, 90–98. [Google Scholar] [CrossRef]
- Clark, D.; Levin, L. In the Dental Implant Era, Why Do We Still Bother Saving Teeth? J. Endod. 2019, 45, S57–S65. [Google Scholar] [CrossRef]
- Díaz, J.A.; Sandoval, H.P.; Pineda, P.I.; Junod, P.A. Conservative treatment of an ankylosed tooth after delayed replantation: A case report. Dent. Traumatol. 2007, 23, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Sala, M.; Mendoza-Mendoza, A.; Yañez-Vico, R.-M. Decoronation: An Alternative Treatment for Replacement Root Resorption. Case Rep. Dent. 2017, 2017, 2826948. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, L.; Wang, M.; Xue, L.; Zhou, W.; Zhang, X.; Jin, L.; Xia, D.; Gong, Y. A retrospective analysis of the optimal time and psychological impact of decoronation in children and adolescents. Dent. Traumatol. 2021, 37, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Mohadeb, J.V.N.; Somar, M.; He, H. Effectiveness of decoronation technique in the treatment of ankylosis: A systematic review. Dent. Traumatol. 2015, 32, 255–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Einy, S.; Kridin, K.; Kaufman, A.Y.; Cohenca, N. Immediate post-operative rehabilitation after decoronation. A systematic review. Dent. Traumatol. 2019, 36, 141–150. [Google Scholar] [CrossRef]
- Thilander, B. Basic mechanisms in craniofacial growth. Acta Odontol. Scand. 1995, 53, 144–151. [Google Scholar] [CrossRef]
- Amler, M.H.; Johnson, P.L.; Salman, I. Histological and histochemical investigation of human alveolar socket healing in undisturbed extraction wounds. J. Am. Dent. Assoc. 1960, 61, 32–44. [Google Scholar] [CrossRef]
- Araujo, M.G.; Lindhe, J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J. Clin. Periodontol. 2005, 32, 212–218. [Google Scholar] [CrossRef]
- Fickl, S.; Zuhr, O.; Wachtel, H.; Kebschull, M.; Hürzeler, M.B. Hard tissue alterations after socket preservation with additional buccal overbuilding: A study in the beagle dog. J. Clin. Periodontol. 2009, 36, 898–904. [Google Scholar] [CrossRef]
- Pietrokovski, J.; Massler, M. Alveolar ridge resorption following tooth extraction. J. Prosthet. Dent. 1967, 17, 21–27. [Google Scholar] [CrossRef]
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics Restor. Dent. 2003, 23, 313–323. [Google Scholar]
- Krastl, G.; Krug, R.; Nolte, D.; Kielbassa, A.M. Traumatized teeth: Clinical practice guideline for the interim management of teeth with various poor prognosis scenarios in growing patients. Quintessence Int. 2022, 53, 722–731. [Google Scholar] [CrossRef]
- Bruno, J.F. Connective tissue graft technique assuring wide root coverage. Int. J. Periodontics Restor. Dent. 1994, 14, 126–137. [Google Scholar]
- Joly, J.C.; Carvalho, A.M.; Da Silva, R.C.; Ciotti, D.L.; Cury, P.R. Root Coverage in Isolated Gingival Recessions Using Autograft Versus Allograft: A Pilot Study. J. Periodontol. 2007, 78, 1017–1022. [Google Scholar] [CrossRef]
- Cortellini, P.; Tonetti, M.; Baldi, C.; Francetti, L.; Rasperini, G.; Rotundo, R.; Nieri, M.; Franceschi, D.; Labriola, A.; Prato, G.P. Does placement of a connective tissue graft improve the outcomes of coronally advanced flap for coverage of single gingival recessions in upper anterior teeth? A multi-centre, randomized, double-blind, clinical trial. J. Clin. Periodontol. 2009, 36, 68–79. [Google Scholar] [CrossRef]
- Zucchelli, G.; Tavelli, L.; Barootchi, S.; Stefanini, M.; Rasperini, G.; Valles, C.; Nart, J.; Wang, H. The influence of tooth location on the outcomes of multiple adjacent gingival recessions treated with coronally advanced flap: A multicenter re-analysis study. J. Periodontol. 2019, 90, 1244–1251. [Google Scholar] [CrossRef]
- Barone, A.; Toti, P.; Piattelli, A.; Iezzi, G.; Derchi, G.; Covani, U. Extraction Socket Healing in Humans After Ridge Preservation Techniques: Comparison Between Flapless and Flapped Procedures in a Randomized Clinical Trial. J. Periodontol. 2014, 85, 14–23. [Google Scholar] [CrossRef]
- Klingberg, G.; Arnrup, K. Dental Fear and Behavior Management Problems. In Pediatric Dentistry: A Clinical Approach, 3rd ed.; Koch, G., Poulsen, S., Espelid, I., Haubek, D., Eds.; Wiley-Blackwell: Chichester, UK, 2017; pp. 55–65. [Google Scholar]
- Warrilow, L.; Gohil, T.; Casaus, A. Replacement Resorption in Children: The Root of All Evil? Prim. Dent. J. 2021, 10, 52–56. [Google Scholar] [CrossRef]
- Natto, Z.S.; Parashis, A.; Steffensen, B.; Ganguly, R.; Finkelman, M.D.; Jeong, Y.N. Efficacy of collagen matrix seal and collagen sponge on ridge preservation in combination with bone allograft: A randomized controlled clinical trial. J. Clin. Periodontol. 2017, 44, 649–659. [Google Scholar] [CrossRef]
- Spinato, S.; Galindo-Moreno, P.; Zaffe, D.; Bernardello, F.; Soardi, C.M. Is socket healing conditioned by buccal plate thickness? A clinical and histologic study 4 months after mineralized human bone allografting. Clin. Oral Implant. Res. 2012, 25, e120–e126. [Google Scholar] [CrossRef]
- Jung, R.E.; Hürzeler, M.B.; Thoma, D.S.; Khraisat, A.; Hämmerle, C.H.F. Local tolerance and efficiency of two prototype collagen matrices to increase the width of keratinized tissue. J. Clin. Periodontol. 2010, 38, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Rotundo, R.; Genzano, L.; Patel, D.; D’Aiuto, F.; Nieri, M. Adjunctive benefit of a xenogenic collagen matrix associated with coronally advanced flap for the treatment of multiple gingival recessions: A superiority, assessor-blind, randomized clinical trial. J. Clin. Periodontol. 2019, 46, 1013–1023. [Google Scholar] [CrossRef] [PubMed]
- Zannis, K.; Mitchell-Heggs, L.; Di Nitto, V.; Kirsch, M.E.; Noghin, M.; Ghorayeb, G.; Lessana, A. Correction of anterior mitral prolapse: The parachute technique. J. Thorac. Cardiovasc. Surg. 2012, 143, S24–S28. [Google Scholar] [CrossRef] [PubMed]
- Motomiya, M.; Watanabe, N.; Kawamura, D.; Yasui, K.; Adachi, A.; Iwasaki, N. Reliable free flaps using the microscopic parachute end-to-side technique in severe extremity injuries. J. Plast. Reconstr. Aesthetic Surg. 2020, 73, 2239–2260. [Google Scholar] [CrossRef]
- Walker, R.R. Use of the inverted parachute retraction suture for epidermal cyst removal. J. Am. Acad. Dermatol. 2018, 78, e7–e8. [Google Scholar] [CrossRef]













Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shay, B.; Mijiritsky, E.; Bronstein, M.; Govani-Levi, M.; Ben Simhon, T.; Chackartchi, T. Flapless Decoronation: A Minimally Invasive Approach. Int. J. Environ. Res. Public Health 2023, 20, 603. https://doi.org/10.3390/ijerph20010603
Shay B, Mijiritsky E, Bronstein M, Govani-Levi M, Ben Simhon T, Chackartchi T. Flapless Decoronation: A Minimally Invasive Approach. International Journal of Environmental Research and Public Health. 2023; 20(1):603. https://doi.org/10.3390/ijerph20010603
Chicago/Turabian StyleShay, Boaz, Eitan Mijiritsky, Meital Bronstein, Mor Govani-Levi, Tal Ben Simhon, and Tali Chackartchi. 2023. "Flapless Decoronation: A Minimally Invasive Approach" International Journal of Environmental Research and Public Health 20, no. 1: 603. https://doi.org/10.3390/ijerph20010603
APA StyleShay, B., Mijiritsky, E., Bronstein, M., Govani-Levi, M., Ben Simhon, T., & Chackartchi, T. (2023). Flapless Decoronation: A Minimally Invasive Approach. International Journal of Environmental Research and Public Health, 20(1), 603. https://doi.org/10.3390/ijerph20010603







