How Do Physiotherapists Explain Influencing Factors to Chronic Low Back Pain? A Qualitative Study Using a Fictive Case of Chronic Non-Specific Low Back Pain
Abstract
1. Introduction
2. Materials and Methods
2.1. Sampling and Recruitment
2.2. Data Collection
2.3. Ethical Considerations
2.4. Data Analysis
3. Results
3.1. Descriptive Data
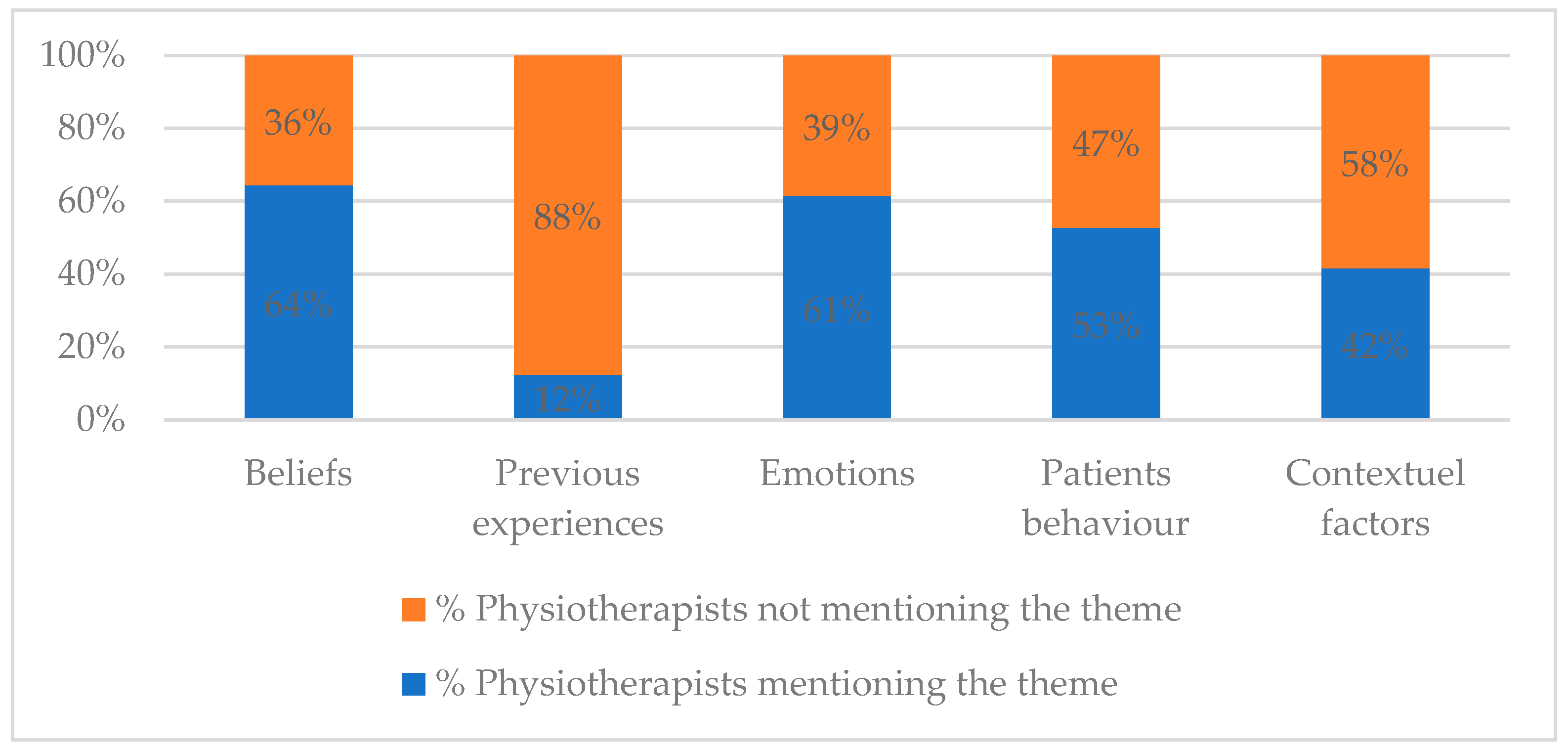
3.2. How Do Physiotherapists Explain Contributing Factors to Pain
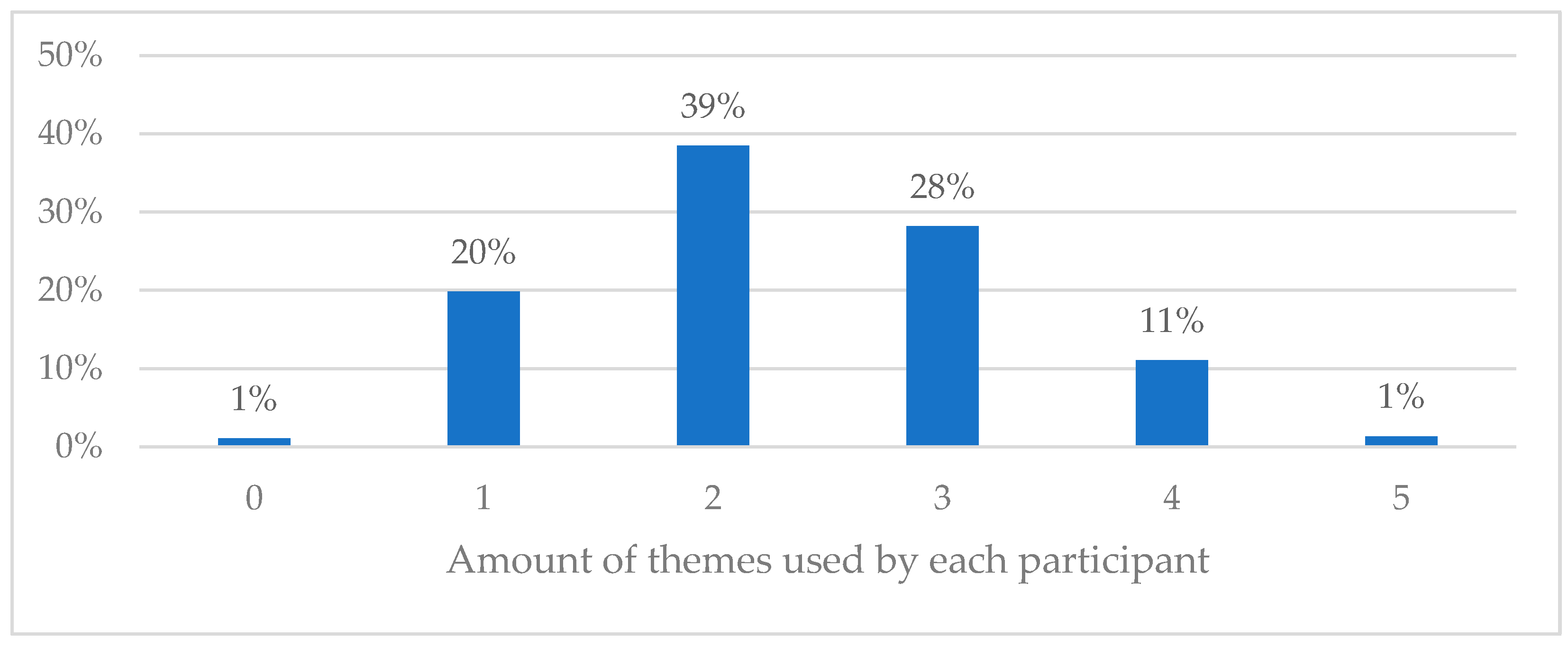
3.3. Use of Multiple Factors When Explaining Contributing Factors to Pain
3.4. Biopsychosocial vs. Biomedical Approach in Explaining the Pain
3.5. Reflective Analysis
4. Discussion
Strengths and Weaknesses
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Fictive Clinical Vignette Depicting a Patient with Chronic Non-Specific Low Back Pain
| A 68-year-old man comes to your practice. He complains of persistent low back pain (VAS score of 6/10). The pain is located at level L4/L5. During certain activities, the pain intensity can increase and in that moment the pain also radiates to the right buttock. In his life, he has never really practised any physical activity. The man lives alone. His wife died of cancer last year. This pain started a year ago after he had cleaned his car with a vacuum cleaner. The pain was very intense at that moment. His children advised him to rest so he would avoid further damage to his back. After a few days, the intense pain was still present. As he was really worried, he decided to consult his general practitioner. The general practitioner advised him not to worry and said that the pain would go away if he got enough rest. However, the pain did not improve much in the following weeks. He agreed with his general practitioner to see a physiotherapist. The latter explained that he needed to strengthen his back and abdominal muscles to keep his vertebrae in place. The physiotherapist also showed him how to correctly bend forward to prevent damage to his back and told him which movements to avoid. Despite following the advice of the physiotherapist, the pain persists. His general practitioner prescribed physiotherapy again. Since the previous physiotherapy sessions did not lead to any improvement, he now consults you to have his back examined and treated. |
References
- Bartholomeeusen, S.; Van Zundert, J.; Truyers, C.; Buntinx, F.; Paulus, D. Higher Incidence of Common Diagnoses in Patients with Low Back Pain in Primary Care. Pain Pract. 2011, 12, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Andersson, G. Epidemiological features of chronic low-back pain. Lancet 1999, 354, 581–585. [Google Scholar] [CrossRef]
- Meucci, R.; Fassa, G.; Faria, N. Prevalence of chronic low back pain: Systematic review. Rev. Saude. Publica. 2015, 49, 1. [Google Scholar] [CrossRef]
- James, S.; Abate, D.; Abate, K.; Abay, S.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef] [PubMed]
- Raja, S.; Carr, D.; Finnerup, N.; Flor, H.; Gibson, S.; Keefe, F.; Mogil, J.; Ringkamp, M.; Sluka, K.; Song, X.; et al. The Revised IASP definition of pain: Concepts, challenges, and compromises. Pain 2020, 161, 1976–1982. [Google Scholar] [CrossRef]
- McLaughlin, P.; Hurley, M.; Chowdary, P.; Stephensen, D.; Khair, K. The experiences and beliefs of people with severe haemophilia and healthcare professionals on pain management, and their views of using exercise as an aspect of intervention: A qualitative study. Disabil. Rehabil. 2021, 44, 8420–8428. [Google Scholar] [CrossRef]
- Linton, S.J. A review of psychological risk factors in back and neck pain. Spine 2000, 25, 1148–1156. [Google Scholar] [CrossRef] [PubMed]
- Andersen, J.; Haahr, J.; Frost, P. Risk factors for more severe regional musculoskeletal symptoms: A two-year prospective study of a general working population. Arthritis. Rheumatol. 2007, 56, 1355–1364. [Google Scholar] [CrossRef]
- Cotchett, M.; Frescos, N.; Whittaker, G.; Bonanno, D. Psychological factors associated with foot and ankle pain: A mixed methods systematic review. J. Foot Ankle Res. 2022, 15, 10. [Google Scholar] [CrossRef]
- Demoulin, C.; Roussel, N.; Marty, M.; Mathy, C.; Genevay, S.; Henrotin, Y.; Tomasella, M.; Mahieu, G.; Vanderthommen, M. Les Croyances délétères des patients lombalgiques. Revue narrative de la littérature. Rev. Med. Liège 2016, 71, 40–46. [Google Scholar]
- Van Wambeke, P.; Desomer, A.; Ailliet, L.; Berquin, A.; Demoulin, C.; Depreitere, B.; Dewachter, J.; Dolphens, M.; Forget, P.; Fraselle, V.; et al. Low back pain and radicular pain: Evaluation and management. In Good Clinical Practice (GCP); KCE Reports 287; Belgian Health Care Knowledge Centre (KCE): Brussels, Belgium, 2017. Available online: https://kce.fgov.be/sites/default/files/2021-11/KCE_287_Low_back_pain_Report.pdf (accessed on 7 April 2021).
- NICE Guideline: Low Back Pain and Sciatica in Over 16s: Assessment and Managent; National Institute for Health and Care Excellence: London, UK, 2020.
- Almeida, M.; Saragiotto, B.; Richards, B.; Maher, C. Primary care management of non-specific low back pain: Key messages from recent clinical guidelines. MJA 2018, 208, 272–275. [Google Scholar] [PubMed]
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, D.; O’Mara, J.; Boden, S.; Lauerman, W.; Jacobson, A.; Platenberg, C.; Schellinger, D.; Wiesel, S. The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects: A seven-year follow-up study. J Bone Jt. Surg. Am. 2001, 83, 1306–1311. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Hanckock, J.; Kongsted, A.; Louw, Q.; Ferreira, M.; Genevay, S.; Hoy, D.; Karppinen, J.; Pranksy, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Deyo, R.; Weinstein, J. Low back pain. N. Engl. J. Med. 2001, 344, 363–370. [Google Scholar] [CrossRef]
- Airaksinen, O.; Brox, J.; Cedraschi, C.; Hildebrandt, J.; Klaber-Moffett, J.; Kovacs, F.; Mannion, A.; Reis, S.; Staal, J.; Ursin, H.; et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur. Spine J. 2006, 15, 192–300. [Google Scholar] [CrossRef]
- Poitras, S.; Durand, M.-J.; Côté, A.-M.; Tousignant, M. Guidelines on Low Back Pain Disability. Spine 2012, 37, 1252–1259. [Google Scholar] [CrossRef] [PubMed]
- Van Tulder, M.; Becker, B.; Becker, A.; Bekkering, T.; Breen, A.; Gil del Real, M.; Hutchinson, A.; Koes, B.; Malmivaara, A. Chapter 3 European guidelines for the management of acute nonspecific low back pain in primary care. Euro. Spine J. 2006, 15, 169–191. [Google Scholar] [CrossRef]
- Morton, L.; de Bruin, M.; Krajewska, M.; Whibley, D.; Macfarlane, G. Beliefs about back pain and pain management behaviours, and their associations in the general population: A systematic review. Eur. J. Pain 2019, 23, 15–30. [Google Scholar] [CrossRef]
- Roussel, N.; Hedwig, N.; Kuppens, K.; Leysen, M.; Kerckhofs, E.; Nijs, J.; Beetsma, A.; Van Wilgen, C. History taking by physiotherapists with low back pain patients: Are illness perceptions addressed properly? Disabil. Rehabil. 2016, 38, 1268–1279. [Google Scholar] [CrossRef]
- Shaw, W.; Pranksy, G.; Winters, T.; Tveito, T.; Larson, S.; Roter, D. Does the presence of psychosocial “yellow flags” alter patient-provider communication for work-related, acute low back pain? J. Occup. Env. Med. 2009, 51, 1032–1040. [Google Scholar] [CrossRef] [PubMed]
- Slatman, S.; Mossink, A.; Jansen, D.; Broeks, J.; van der Lugt, P.; Prosman, G.-J.; Oude Nijeweme-d’Hollosy, W. Factors used by general practitioners for referring patients with chronic musculoskeletal pain: A qualitative study. BMC Prim. Care 2022, 23, 126. [Google Scholar] [CrossRef] [PubMed]
- Darlow, B.; Fullen, B.; Dean, S.; Baxter, G.; Dowell, A. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: A systematic review. Eur. J. Pain 2012, 16, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Mescouto, K.; Olson, R.; Hodges, P.; Costa, N.; Patton, M.; Evans, K.; Walsh, K.; Lonergan, K.; Setchell, J. Physiotherapists Both Reproduce and Resist Biomedical Dominance when Working With People With Low Back Pain: A Qualitative Study Towards New Praxis. Qual. Health Res. 2022, 32, 902–915. [Google Scholar] [CrossRef]
- Demoulin, C.; Gabriel, L.; Nève de Mévergnies, O.; Henket, L.; Roussel, N.; Goubert, L.; Vanderthommen, M.; Pitance, L. Several low back pain-related misbeliefs are still around in 2020: A cross-sectional survey in Belgium. Physiother. Res. Int. 2021, 27, e1927. [Google Scholar] [CrossRef]
- Guillaume, C.; Ludovic, D.; Arnaud, L.; Ben, D.; Claude, P. Physiotherapists’ attitudes and beliefs about low back pain influence their clinical decisions and advice. Musculoskelet. Sci. Pract. 2021, 53, 102382. [Google Scholar] [CrossRef]
- Gardner, T.; Refshauge, K.; Smith, L.; McAuley, J.; Hübscher, M.; Goodall, S. Physiotherapists’ beliefs and attitudes influence clinical practice in chronic low back pain: A systematic review of quantitative and qualitative studies. J. Physiother. 2017, 63, 132–143. [Google Scholar] [CrossRef]
- Buchbinder, R.; Jolley, D.; Wyatt, M. Population based intervention to change back pain beliefs and disability: Three part evaluation. BMJ 2001, 322, 1516–1520. [Google Scholar] [CrossRef]
- Derebery, V.; Giang, G.; Saracino, G.; Fogarty, T. Evaluation of the Impact of a Low Back Pain Educational Intervention on Physicians’ Practice Patterns and Patients’ Outcomes. JOEM 2002, 44, 977–984. [Google Scholar] [CrossRef][Green Version]
- Latimer, J.; Maher, C.; Refshauge, K. The Attitudes and Beliefs of Physiotherapy Students to Chronic Back Pain. Clin. J. Pain. 2004, 20, 45–50. [Google Scholar] [CrossRef]
- Harris, J.; Elliot, T.; Davis, B.; Chabal, C.; Fulginiti, J.; Fine, P. Educating Generalist Physicians about Chronic Pain: Live Experts and Online Education Can Provide Durable Benefits. Pain Med. 2008, 9, 555–563. [Google Scholar] [CrossRef] [PubMed]
- Evans, D.; Breen, A.; Pincus, T.; Sim, J.; Underwood, M.; Vogel, S.; Foster, N. The Effectiveness of a Posted Information Package on the Beliefs and Behavior of Musculoskeletal Practitioners. SPINE 2010, 35, 858–866. [Google Scholar] [CrossRef]
- Domenech, J.; Sánchez-Zuriaga, D.; Segura-Ortí, E.; Espejo-Tort, B.; Lisón, J. Impact of biomedical and biopsychosocial training sessions on the attitudes, beliefs, and recommendations of health care providers about low back pain: A randomised clinical trial. Pain 2011, 152, 2557–2563. [Google Scholar] [CrossRef] [PubMed]
- Evans, L.; Whitham, J.; Trotter, D.; Filtz, K. An Evaluation of Family Medicine Residents’ Attitudes Before and After a PCMH Innovation for Patients With Chronic Pain. Fam. Med. 2011, 43, 702–711. [Google Scholar] [PubMed]
- Slater, H.; Briggs, A.; Smith, A.; Bunzli, S.; Davies, S.; Quinter, J. Implementing Evidence-Informed Policy into Practice for Health Care Professionals Managing People with Low Back Pain in Australian Rural Settings: A Preliminary Prospective Single-Cohort Study. Pain Med. 2014, 15, 1657–1668. [Google Scholar] [CrossRef]
- Slater, H.; Davies, J.; Parsons, R.; Quinter, J.; Schug, S. A Policy-into-Practice Intervention to Increase the Uptake of Evidence-Based Management of Low Back Pain in Primary Care: A Prospective Cohort Study. PLoS ONE 2012, 7, e38037. [Google Scholar] [CrossRef]
- Shaheed, C.; Graves, J.; Maher, C. The effects of a brief educational intervention on medical students’ knowledge, attitudes and beliefs towards low back pain. Scand. J. Pain 2017, 16, 101–104. [Google Scholar] [CrossRef]
- Colleary, G.; O’Sullivan, K.; Griffin, D.; Ryan, C.; Martin, D. Effect of pain neurophysiology education on physiotherapy students’ understanding of chronic pain, clinical recommendations and attitudes towards people with chronic pain: A randomised controlled trial. Physiotherapy 2017, 103, 423–429. [Google Scholar] [CrossRef]
- Fitzgerald, K.; Fleischmann, M.; Vaughan, B.; de Waal, K.; Slater, S.; Harbis, J. Changes in pain knowledge, attitudes and beliefs of osteopathy students after completing a clinically focused pain education module. Chiropr. Man. Ther. 2018, 26, 42. [Google Scholar] [CrossRef]
- Dillman, D.; Smyth, J.; Christian, L. Internet, Phone, Mail, and Mixed-Mode Surveys: The Tailored Design Method; Wiley: Hoboken, NJ, USA, 2014; ISBN 978-1-118-45614-9. [Google Scholar]
- Gale, N.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 2013, 13, 1–8. [Google Scholar] [CrossRef]
- Bazeley, P. Integration through Data Transformation 1: Qualitative Data to Statistical Variables; SAGE Publications Ltd.: Thousand Oaks, CA, USA, 2018. [Google Scholar] [CrossRef]
- Maxwell, J. Using Numbers in Qualitative Research. Qual. Inq. 2010, 16, 475–482. [Google Scholar] [CrossRef]
- Treede, R.D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019, 160, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Treede, R.D. The International Association for the Study of Pain definition of pain: As valid in 2018 as in 1979, but in need of regularly updated footnotes. Pain Rep. 2018, 3, e643. [Google Scholar] [CrossRef] [PubMed]
- Engel, G. The need for a new medical model: A challenge for biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Engel, G. The Biopsychosocial model and the education of health professionals. Gen. Hosp. Psychiatry 1979, 1, 156–165. [Google Scholar] [CrossRef]
- Lim, Y.Z.; Chou, L.; Au, R.T.; Seneviwickrama, K.M.D.; Cicuttini, F.M.; Briggs, A.M.; Sullivan, K.; Urquhart, D.M.; Wluka, A.E. People with low back pain want clear, consistent and personalised information on prognosis, treatment options and self-management strategies: A systematic review. J. Physiother. 2019, 65, 124–135. [Google Scholar] [CrossRef]
- Saragiotto, B.; de Almeida, M.; Yarnato, T.; Maher, C. Multidisciplinary Biopsychosocial Rehabilitation for Nonspecific Chronic Low Back Pain. Phys. Ther. 2016, 96, 759–763. [Google Scholar] [CrossRef]
- Kamper, S.J.; Apeldoorn, A.T.; Chiarotto, A.; Smeets, R.J.; Ostelo, R.W.; Guzman, J.; van Tulder, M.W. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ 2015, 350, h444. [Google Scholar] [CrossRef]
- Pierobon, A.; Policastro, P.; Soliño, S.; Andreu, M.; Novoa, G.; Raguzzi, I.; Villalba, F.; Darlow, B. Beliefs and attitudes about low back pain in Argentina: A cross-sectional survey using social media. Musculoskelet. Sci. Pract. 2020, 49, 102183. [Google Scholar] [CrossRef]
- NICE. Chronic Pain (Primary and Secondary) in Over 16s: Assessment of All Chronic Pain and Management of Chronic Primary Pain. Available online: https://www.nice.org.uk/guidance/ng193 (accessed on 7 April 2021).
- Harris, J.; Fulginiti, J.; Gordon, P.; Elliot, T.; Davis, B.; Chabal, C.; Kutob, R. KnowPain-50: A tool for assessing physician pain management education. Pain Med. 2008, 9, 542–554. [Google Scholar] [CrossRef][Green Version]
- Darlow, B.; Perry, M.; Mathieson, F.; Stanley, J.; Melloh, M.; Marsh, R. The development and exploratory analysis of the Back Pain Attitudes Questionnaire (Back-PAQ). BMJ Open. 2014, 4, e005251. [Google Scholar] [CrossRef] [PubMed]
- Houben, R.; Vlaeyen, J.; Peters, M.; Ostelo, R.; Wolters, P.; Stomp-van den Berg, S. Health care providers’ attitudes and beliefs towards common low back pain: Factor structure and psychometric properties of the HC-PAIRS. Clin. J. Pain. 2004, 20, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Vlaeyen, J.; Crombez, G. Fear of movement/(re)injury, avoidance and pain disability in chronic low back pain patients. Man. Ther. 1999, 4, 187–195. [Google Scholar] [CrossRef]
- Wertli, M.; Rasmussen-Barr, E.; Weiser, S.; Bachmann, L.; Brunner, F. The role of fear avoidance beliefs as a prognostic factor for outcome in patients with nonspecific low back pain: A systematic review. Spine J. 2014, 14, 816–836. [Google Scholar] [CrossRef]
- Aleena, A.; Eslavath, R.; Romate, J.; Allen, J. Determinants of quality of life in individuals with chronic low back pain: A systematic review. Health Psychol. Behav. Med. 2022, 10, 124–144. [Google Scholar] [CrossRef]
- Hayden, J.; Ellis, J.; Ogilvie, R.; Malmivaara, A.; van Tulder, M. Exercise therapy for chronic low back pain. Cochrane Database Syst. Rev. 2021, 9, CD009790. [Google Scholar] [CrossRef]
- Slade, S.; Patel, S.; Underwood, M.; Keating, J. What are patient beliefs and perceptions about exercise for nonspecific chronic low back pain? A systematic review of qualitative studies. Clin. J. Pain. 2014, 30, 995–1005. [Google Scholar] [CrossRef] [PubMed]
- Belavy, D.; Van Oosterwijck, J.; Clarkson, M.; Dhondt, E.; Mundell, N.; Miller, C.; Owen, P. Pain sensitivity is reduced by exercise training: Evidence from a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2021, 120, 100–108. [Google Scholar] [CrossRef]
- Toye, F.; Barker, K. ‘I can’t see any reason for stopping doing anything, but I might have to do it differently’—Restoring hope to patients with persistent non-specific low back pain—A qualitative study. Disabil. Rehabil. 2012, 34, 894–903. [Google Scholar] [CrossRef]
- Zadro, J.; Shirley, D.; Duncan, G.; Ferreira, P. Familial factors predicting recovery and maintenance of physical actitivity in people with low back pain: Insights from a population-based twin study. Euro. J. Pain. 2018, 23, 367–377. [Google Scholar] [CrossRef]
- Zangoni, G.; Thomson, O. ‘I need to do another course’—Italian physiotherapists’ knowledge and beliefs when assessing psychosocial factors in patients presenting with chronic low back pain. Musculoskelet. Sci. Pract. 2017, 27, 71–77. [Google Scholar] [CrossRef] [PubMed]
- França, A.; dos Santos, V.; Filho, R.; Pires, K.; Lagoa, K.; Martins, W. ‘It’s very complicated’: Perspectives and beliefs of newly graduated physiotherapists about the biopsychosocial model for treating people experiencing non-specific low back pain in Brazil. Musculoskelet. Sci. Pract. 2019, 42, 84–89. [Google Scholar] [CrossRef]
- Synnott, A.; O’Keeffe, M.; Bunzli, S.; Dankaerts, W.; O’Sullivan, P.; O’Sullivan, K. Physiotherapists may stigmatise or feel unprepared to treat people with low back pain and psychosocial factors that influence recovery: A systematic review. J. Physiother. 2015, 61, 68–76. [Google Scholar] [CrossRef]
- Cowell, I.; O’Sullivan, P.; O’Sullivan, K.; Poyton, R.; McGregor, A.; Murtagh, G. The perspectives of physiotherapists on managing nonspecific low back pain following a training programme in cognitive functional therapy: A qualitative study. Musculoskelet. Care 2018, 17, 79–90. [Google Scholar] [CrossRef]
- Smith, B.; Fors, E.; Korwisi, B.; Barke, A.; Cameron, P.; Colvin, L.; Richardson, C.; Rief, W.; Treede, R. The IASP classification of chronic pain for ICD-11: Applicability in primary care. Pain 2019, 160, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Rainville, J.; Carslon, N.; Polatin, P.; Gatchel, R.; Indahl, A. Exploration of Physicians’ Recommendations for Activities in Chronic Low Back Pain. SPINE 2000, 25, 2210–2220. [Google Scholar] [CrossRef]
- Bombardier, C.; Jansz, G.; Maetzel, A. Primary care physicians’ knowledge, confidence, and attitude in the management of acute low back pain (ALBP). Arthritis. Rheum. 1995, 38, S385. [Google Scholar]
- Leysen, M.; Nijs, J.; Van Wilgen, P.; Demoulin, C.; Dankaerts, W.; Danneels, L.; Roussel, N. Attitudes and beliefs on low back pain in physical therapy education: A cross-sectional study. Braz. J. Phys. Ther. 2020, 25, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Brunner, E.; Probst, M.; Meichtry, A.; Luomajoki, H.; Dankaerts, W. Comparison of clinical vignettes and standardized patients as measures of physiotherapists’ activity and work recommendations in patients with non-specific low back pain. Clin. Rehabil. 2016, 30, 85–94. [Google Scholar] [CrossRef]
- Evans, D.; Foster, N.; Underwood, M.; Vogel, S.; Breen, A.; Pincus, T. Testing the effectiveness of an innovative information package on practitioner reported behaviour and beliefs: The UK Chiropractors, Osteopaths and Musculoskeletal Physiotherapists Low back pain Management (COMPLeMENT) trial. BMC Musculoskelet. Disord. 2005, 6, 41. [Google Scholar] [CrossRef]
- Darlow, B.; Stanley, J.; Dean, S.; Abbott, J.; Garrett, S.; Wilson, R. The Fear Reduction exercised Early (FREE) approach to management of low back pain in general practice: A pragmatic cluster-randomised controlled trial. PLoS Med. 2019, 16, e1002897. [Google Scholar] [CrossRef] [PubMed]

| Themes | Approach | Code | Description |
|---|---|---|---|
| Beliefs | Biopsychosocial | B1 | Misbeliefs of the patient that pain is linked to tissue damage or to a biomechanical cause |
| B2 | Misbeliefs of the patient that rest/avoiding movement will lead to a decrease in pain | ||
| B3 | Misbeliefs that moving in a very specific way is necessary to decrease the pain | ||
| Biomedical | B4 | Attributing the cause of pain to bad movements or postures, etc. | |
| B5 | Linking pain to ageing | ||
| B6 | Describing a specific pathology or impairment in anatomical structure as cause of the pain | ||
| Previous experiences | Biopsychosocial | PE1 | The lack of success is explained by previous treatments that were too biomechanically focussed |
| Biomedical | PE2 | The lack of success is explained by the fact that the previous treatment was not well enough executed in a biomechanical framework | |
| Emotions | Biopsychosocial | E1 | The fact that the patient worries about the pain and about movement might contribute to the pain |
| Biomedical | E2 | Depression or a mentally fragile situation is the cause of pain | |
| Patient’s behaviour | Biopsychosocial | PB1 | The sedentary aspect or the avoidance behaviour of the patient might contribute to the pain |
| Biomedical | PB2 | The patient suffers from pain because he did not do his exercises well enough or did not comply enough | |
| Contextual factors | Biopsychosocial | CF1 | The unhelpful influence of the family might be related to the pain |
| Biomedical | CF2 | The patient is not able to adapt to his changed environment |
| n (%) | ||||
|---|---|---|---|---|
| Flanders | Wallonia | France | Total | |
| Population | 308 (100%) | 189 (100%) | 173 (100%) | 670 (100%) |
| Gender | ||||
| Female | 201 (65%) | 106 (56%) | 92 (53%) | 399 (60%) |
| Male | 107 (35 %) | 83 (44%) | 81 (47%) | 271 (40%) |
| Estimation new LBP patients/month | ||||
| 1–5 | 72 (23%) | 71 (38%) | 28 (16%) | 171 (26%) |
| 5–10 | 106 (34%) | 75 (40%) | 68 (39%) | 249 (37%) |
| 10–15 | 69 (22%) | 27 (14%) | 29 (17%) | 125 (19%) |
| 15–20 | 24 (8%) | 9 (5%) | 15 (9%) | 48 (7%) |
| >20 | 37 (12%) | 4 (2%) | 7 (4%) | 48 (7%) |
| Median (Q1–Q3) | ||||
| Flanders | Wallonia | France | Total | |
| Age (years) | 34 (27–47) | 30 (26–40) | 27 (25–33) | 30 (26–43) |
| Work experience (years) | 10 (4–25) | 7 (3–18) | 5 (2–10) | 7 (3–21) |
| Theme | Differentiation | Code | N% | Example of Quotes |
|---|---|---|---|---|
| Beliefs | Biopsychosocial approach | B1 | 12 | “Misinterpretation that pain equals damage” |
| B2 | 16 | “The belief that rest is necessary” | ||
| B3 | 14 | “Advise to avoid certain movements” | ||
| Neutral | B-n | 15 | “His insight of pain” | |
| Biomedical approach | B4 | 23 | “Wrong posture of the back”, “Weak muscle strength” | |
| B5 | 4 | “Age” | ||
| B6 | 12 | “Osteoarthritis with possible disc problem” | ||
| Previous experience | Biopsychosocial approach | PE1 | 5 | “Conflicting information between professionals” |
| Neutral | PE-n | 6 | “No explanation about his back pain” | |
| Biomedical approach | PE2 | 3 | “Incorrect exercises” | |
| Emotions | Biopsychosocial approach | E1 | 28 | “Fear of movement”, “Fear of pain” |
| Neutral | E-n | 46 | “Grief due to death of wife” | |
| Biomedical approach | E2 | 4 | “Mental fragility” | |
| Patients behaviour | Biopsychosocial approach | PB1 | 52 | “Lack of physical activity”, “Lack of exercise” |
| Neutral | PB-n | 1 | “Lifestyle” | |
| Biomedical approach | PB2 | 0.1 | “Poor exercise performance by the patient” | |
| Contextual factor | Biopsychosocial approach | CF1 | 18 | “Overprotection of the children” |
| Neutral | CF-n | 32 | “Alone without his partner” | |
| Biomedical approach | CF2 | 1 | “Change of activities in connection with the loss of his wife, adaptation necessary” |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vanderstraeten, R.; Fourré, A.; Demeure, I.; Demoulin, C.; Michielsen, J.; Anthierens, S.; Bastiaens, H.; Roussel, N. How Do Physiotherapists Explain Influencing Factors to Chronic Low Back Pain? A Qualitative Study Using a Fictive Case of Chronic Non-Specific Low Back Pain. Int. J. Environ. Res. Public Health 2023, 20, 5828. https://doi.org/10.3390/ijerph20105828
Vanderstraeten R, Fourré A, Demeure I, Demoulin C, Michielsen J, Anthierens S, Bastiaens H, Roussel N. How Do Physiotherapists Explain Influencing Factors to Chronic Low Back Pain? A Qualitative Study Using a Fictive Case of Chronic Non-Specific Low Back Pain. International Journal of Environmental Research and Public Health. 2023; 20(10):5828. https://doi.org/10.3390/ijerph20105828
Chicago/Turabian StyleVanderstraeten, Rob, Antoine Fourré, Isaline Demeure, Christophe Demoulin, Jozef Michielsen, Sibyl Anthierens, Hilde Bastiaens, and Nathalie Roussel. 2023. "How Do Physiotherapists Explain Influencing Factors to Chronic Low Back Pain? A Qualitative Study Using a Fictive Case of Chronic Non-Specific Low Back Pain" International Journal of Environmental Research and Public Health 20, no. 10: 5828. https://doi.org/10.3390/ijerph20105828
APA StyleVanderstraeten, R., Fourré, A., Demeure, I., Demoulin, C., Michielsen, J., Anthierens, S., Bastiaens, H., & Roussel, N. (2023). How Do Physiotherapists Explain Influencing Factors to Chronic Low Back Pain? A Qualitative Study Using a Fictive Case of Chronic Non-Specific Low Back Pain. International Journal of Environmental Research and Public Health, 20(10), 5828. https://doi.org/10.3390/ijerph20105828






