Adverse Childhood Experiences and Mental Health among Students Seeking Psychological Counseling Services
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Measures
2.4. Data Analysis
3. Results
3.1. Descriptive Statistics
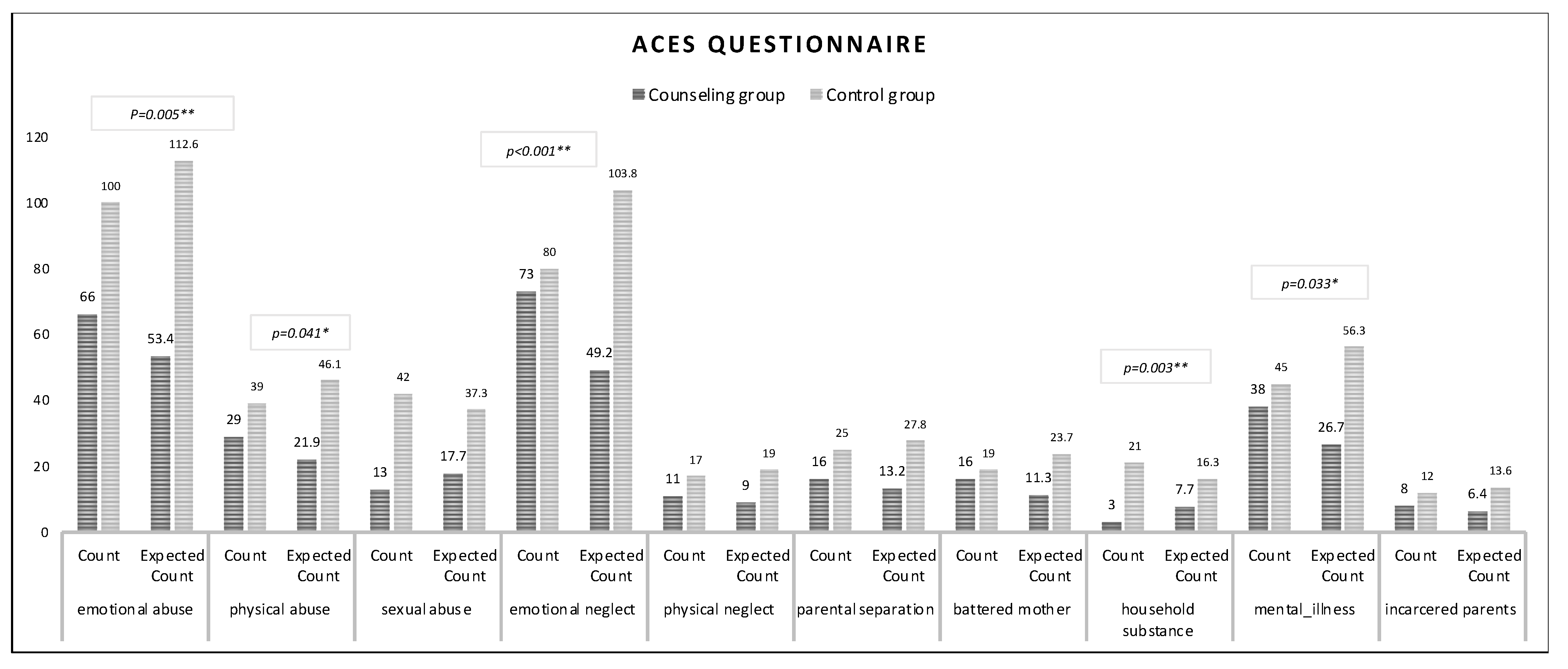
3.2. ACEs
3.3. Psychological Distress Symptoms
3.4. Personality Traits and Coping Strategies
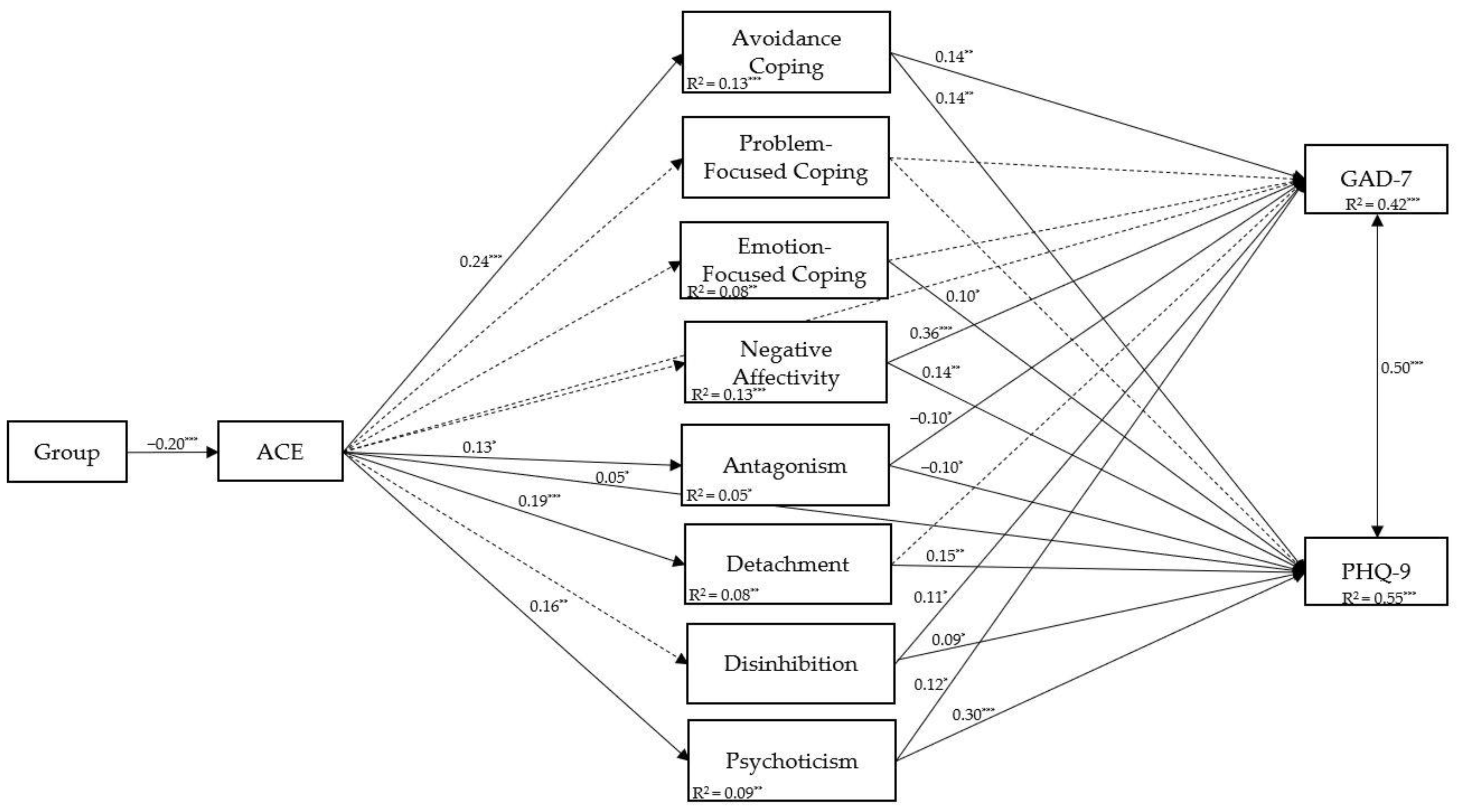
3.5. Correlation and Mediation Analyses
4. Discussion
4.1. Implications for University Psychological Counseling and Future Directions
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sweeney, A.; Filson, B.; Kennedy, A.; Collinson, L.; Gillard, S. A Paradigm Shift: Relationships in Trauma-Informed Mental Health Services. BJPsych Adv. 2018, 24, 319–333. [Google Scholar] [CrossRef] [PubMed]
- Petruccelli, K.; Davis, J.; Berman, T. Adverse Childhood Experiences and Associated Health Outcomes: A Systematic Review and Meta-Analysis. Child Abus. Negl. 2019, 97, 104127. [Google Scholar] [CrossRef] [PubMed]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 2019, 56, 774–786. [Google Scholar] [CrossRef]
- Merrick, M.T.; Ports, K.A.; Ford, D.C.; Afifi, T.O.; Gershoff, E.T.; Grogan-Kaylor, A. Unpacking the Impact of Adverse Childhood Experiences on Adult Mental Health. Child Abus. Negl. 2017, 69, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Oral, R.; Ramirez, M.; Coohey, C.; Nakada, S.; Walz, A.; Kuntz, A.; Benoit, J.; Peek-Asa, C. Adverse Childhood Experiences and Trauma Informed Care: The Future of Health Care. Pediatr. Res. 2016, 79, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Nelson, C.A.; Scott, R.D.; Bhutta, Z.A.; Harris, N.B.; Danese, A.; Samara, M. Adversity in childhood is linked to mental and physical health throughout life. BMJ 2020, 371, m3048. [Google Scholar] [CrossRef] [PubMed]
- Substance Abuse and Mental Health Services Administration. Center for Substance Abuse Treatment Chapter 3: Understanding the Impact of Trauma. In Trauma-Informed Care in Behavioral Health Services; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2014. [Google Scholar]
- Kleber, R.J. Trauma and Public Mental Health: A Focused Review. Front. Psychiatry 2019, 10, 451. [Google Scholar] [CrossRef]
- Musso, P.; Coppola, G.; Pantaleo, E.; Amoroso, N.; Balenzano, C.; Bellotti, R.; Cassibba, R.; Diacono, D.; Monaco, A. Psychological Counseling in the Italian Academic Context: Expected Needs, Activities, and Target Population in a Large Sample of Students. PLoS ONE 2022, 17, e0266895. [Google Scholar] [CrossRef]
- Adachi, Y.; Yoshikawa, H.; Yokoyama, S.; Iwasa, K. Characteristics of University Students Supported by Counseling Services: Analysis of Psychological Tests and Pulse Rate Variability. PLoS ONE 2020, 15, e0218357. [Google Scholar] [CrossRef]
- Davies, E.; Read, J.; Shevlin, M. The Impact of Adverse Childhood Experiences and Recent Life Events on Anxiety and Quality of Life in University Students. High. Educ. 2022, 84, 211–224. [Google Scholar] [CrossRef]
- Watt, T.; Ceballos, N.; Kim, S.; Pan, X.; Sharma, S. The Unique Nature of Depression and Anxiety among College Students with Adverse Childhood Experiences. J. Child Adolesc. Trauma 2020, 13, 163–172. [Google Scholar] [CrossRef]
- Bae, S.M. Long-Term Effect of Adverse Childhood Experiences, School Disengagement, and Reasons for Leaving School on Delinquency in Adolescents Who Dropout. Front. Psychol. 2020, 11, 2096. [Google Scholar] [CrossRef] [PubMed]
- Lecy, N.; Osteen, P. The Effects of Childhood Trauma on College Completion. Res. High. Educ. 2022, 63, 1058–1072. [Google Scholar] [CrossRef]
- Brown, M.J.; Masho, S.W.; Perera, R.A.; Mezuk, B.; Pugsley, R.A.; Cohen, S.A. Sex Disparities in Adverse Childhood Experiences and HIV/STIs: Mediation of Psychopathology and Sexual Behaviors. AIDS Behav. 2017, 21, 1550–1566. [Google Scholar] [CrossRef] [PubMed]
- Osborn, T.G.; Li, S.; Saunders, R.; Fonagy, P. University Students’ Use of Mental Health Services: A Systematic Review and Meta-Analysis. Int. J. Ment. Health Syst. 2022, 16, 57. [Google Scholar] [CrossRef]
- Vescovelli, F.; Melani, P.; Ruini, C.; Bitti, P.E.R.; Monti, F. University Counseling Service for Improving Students’ Mental Health. Psychol. Serv. 2017, 14, 470. [Google Scholar] [CrossRef]
- Estric, C.; Calati, R.; Lopez-Castroman, J. Adverse Childhood Experiences and Neurocognition in Borderline Personality Disorder: A Call-to-Action Perspective Review. Harv. Rev. Psychiatry 2022, 30, 248–260. [Google Scholar] [CrossRef]
- Porter, C.; Palmier-Claus, J.; Branitsky, A.; Mansell, W.; Warwick, H.; Varese, F. Childhood adversity and borderline personality disorder: A meta-analysis. Acta Psychiatr Scand. 2020, 141, 6–20. [Google Scholar] [CrossRef]
- Krakau, L.; Tibubos, A.N.; Beutel, M.E.; Ehrenthal, J.C.; Gieler, U.; Brähler, E. Personality Functioning as a Mediator of Adult Mental Health following Child Maltreatment. J. Affect. Disord. 2021, 291, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Godbout, N.; Daspe, M.È.; Runtz, M.; Cyr, G.; Briere, J. Childhood Maltreatment, Attachment, and Borderline Personality-Related Symptoms: Gender-Specific Structural Equation Models. Psychol. Trauma 2019, 11, 90. [Google Scholar] [CrossRef]
- Frewen, P.; Brown, M.; DePierro, J.; D’Andrea, W.; Schore, A. Assessing the Family Dynamics of Childhood Maltreatment History with the Childhood Attachment and Relational Trauma Screen (CARTS). Eur. J. Psychotraumatology 2015, 6, 27792. [Google Scholar] [CrossRef]
- Grusnick, J.M.; Garacci, E.; Eiler, C.; Williams, J.S.; Egede, L.E. The Association between Adverse Childhood Experiences and Personality, Emotions and Affect: Does Number and Type of Experiences Matter? J. Res. Personal. 2020, 85, 103908. [Google Scholar] [CrossRef]
- Yang, J.Z.; Kang, C.Y.; Yuan, J.; Zhang, Y.; Wei, Y.J.; Xu, L.; Zhou, F.; Fan, X. Effect of Adverse Childhood Experiences on Hypothalamic–Pituitary–Adrenal (HPA) Axis Function and Antidepressant Efficacy in Untreated First Episode Patients with Major Depressive Disorder. Psychoneuroendocrinology 2021, 134, 105432. [Google Scholar] [CrossRef]
- Dempster, K.S.; O’Leary, D.D.; MacNeil, A.J.; Hodges, G.J.; Wade, T.J. Linking the Hemodynamic Consequences of Adverse Childhood Experiences to an Altered HPA Axis and Acute Stress Response. Brain Behav. Immun. 2021, 93, 254–263. [Google Scholar] [CrossRef]
- Sheffler, J.L.; Piazza, J.R.; Quinn, J.M.; Sachs-Ericsson, N.J.; Stanley, I.H. Adverse Childhood Experiences and Coping Strategies: Identifying Pathways to Resiliency in Adulthood. Anxiety Stress Coping 2019, 32, 594–609. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. (Eds.) Stress, Appraisal, and Coping; Springer: Berlin/Heidelberg, Germany, 1984. [Google Scholar]
- Gipple, D.E.; Lee, S.M.; Puig, A. Coping and Dissociation among Female College Students: Reporting Childhood Abuse Experiences. J. Coll. Couns. 2006, 9, 33–46. [Google Scholar] [CrossRef]
- Shapiro, D.L.; Levendosky, A.A. Adolescent Survivors of Childhood Sexual Abuse: The Mediating Role of Attachment Style and Coping in Psychological and Interpersonal Functioning. Child Abus. Negl. 1999, 23, 1175–1191. [Google Scholar] [CrossRef]
- Grummitt, L.; Barrett, E.; Kelly, E.; Newton, N. An Umbrella Review of the Links between Adverse Childhood Experiences and Substance Misuse: What, Why, and Where Do We Go from Here? Subst. Abus. Rehabil. 2022, 13, 83–100. [Google Scholar] [CrossRef]
- Holahan, C.J.; Holahan, C.K.; Moos, R.H.; Brennan, P.L.; Schutte, K.K. Stress Generation, Avoidance Coping, and Depressive Symptoms: A 10-Year Model. J. Consult. Clin. Psychol. 2005, 73, 658. [Google Scholar] [CrossRef]
- Miethe, S.; Wigger, J.; Wartemann, A.; Fuchs, F.O.; Trautmann, S. Posttraumatic Stress Symptoms and Its Association with Rumination, Thought Suppression and Experiential Avoidance: A Systematic Review and Meta-Analysis. J. Psychopathol. Behav. Assess. 2023, 45, 480–495. [Google Scholar] [CrossRef]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults—Impact on Children. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef]
- Hughes, K.; Bellis, M.A.; Hardcastle, K.A.; Sethi, D.; Butchart, A.; Mikton, C.; Jones, L.; Dunne, M.P. The Effect of Multiple Adverse Childhood Experiences on Health: A Systematic Review and Meta-Analysis. Lancet Public Health 2017, 2, e356–e366. [Google Scholar] [CrossRef]
- Zarse, E.M.; Neff, M.R.; Yoder, R.; Hulvershorn, L.; Chambers, J.E.; Chambers, R.A. The Adverse Childhood Experiences Questionnaire: Two Decades of Research on Childhood Trauma as a Primary Cause of Adult Mental Illness, Addiction, and Medical Diseases. Cogent Med. 2019, 6, 1581447. [Google Scholar] [CrossRef]
- Taber, K.S. The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Res. Sci. Educ. 2018, 48, 1273–1296. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B. Validation and Utility of a Self-Report Version of PRIME-MD: The PHQ Primary Care Study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef]
- Krueger, R.F.; Eaton, N.R. Personality Traits and the Classification of Mental Disorders: Toward a More Complete Integration in DSM-5 and an Empirical Model of Psychopathology. Personal. Disord. Theory Res. Treat. 2010, 1, 97. [Google Scholar] [CrossRef]
- Carver, C.S.; Scheier, M.F.; Weintraub, K.J. Assessing Coping Strategies: A Theoretically Based Approach. J. Personal. Soc. Psychol. 1989, 56, 267. [Google Scholar] [CrossRef]
- Carver, C.S. You Want to Measure Coping but Your Protocol’s Too Long: Consider the Brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef]
- Kline, R.B. TXTBK Principles and Practices of Structural Equation Modelling, 4th ed.; The Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- Preacher, K.J.; Hayes, A.F. Asymptotic and Resampling Strategies for Assessing and Comparing Indirect Effects in Multiple Mediator Models. Behav. Res. Method. 2008, 40, 879–891. [Google Scholar] [CrossRef]
- Wen, Z.; Fan, X. Monotonicity of Effect Sizes: Questioning Kappa-Squared as Mediation Effect Size Measure. Psychol. Method. 2015, 20, 193. [Google Scholar] [CrossRef]
- Kessler, R.C.; McLaughlin, K.A.; Green, J.G.; Gruber, M.J.; Sampson, N.A.; Zaslavsky, A.M.; Aguilar-Gaxiola, S.; Alhamzawi, A.O.; Alonso, J.; Angermeyer, M.; et al. Childhood Adversities and Adult Psychopathology in the WHO World Mental Health Surveys. Br. J. Psychiatry 2010, 197, 378–385. [Google Scholar] [CrossRef]
- Mauritz, M.W.; Goossens, P.J.J.; Draijer, N.; van Achterberg, T. Prevalence of Interpersonal Trauma Exposure and Trauma-Related Disorders in Severe Mental Illness. Eur. J. Psychotraumatology 2013, 4, 19985. [Google Scholar] [CrossRef]
- Giano, Z.; Ernst, C.W.; Snider, K.; Davis, A.; O’Neil, A.M.; Hubach, R.D. ACE Domains and Depression: Investigating Which Specific Domains Are Associated with Depression in Adulthood. Child Abus. Negl. 2021, 122, 105335. [Google Scholar] [CrossRef]
- Chapman, D.P.; Whitfield, C.L.; Felitti, V.J.; Dube, S.R.; Edwards, V.J.; Anda, R.F. Adverse Childhood Experiences and the Risk of Depressive Disorders in Adulthood. J. Affect. Disord. 2004, 82, 217–225. [Google Scholar] [CrossRef]
- Desch, J.; Mansuri, F.; Tran, D.; Schwartz, S.W.; Bakour, C. The association between adverse childhood experiences and depression trajectories in the Add Health study. Child Abuse Negl. 2023, 137, 106034. [Google Scholar] [CrossRef]
- Tsehay, M.; Necho, M.; Mekonnen, W. The Role of Adverse Childhood Experience on Depression Symptom, Prevalence, and Severity among School Going Adolescents. Depress Res. Treat. 2020, 18, 5951792. [Google Scholar] [CrossRef]
- Danese, A.; Moffitt, T.E.; Pariante, C.M.; Ambler, A.; Poulton, R.; Caspi, A. Elevated Inflammation Levels in Depressed Adults with a History of Childhood Maltreatment. Arch. Gen. Psychiatry 2008, 65, 409–415. [Google Scholar] [CrossRef]
- Heim, C.; Newport, D.J.; Mletzko, T.; Miller, A.H.; Nemeroff, C.B. The Link between Childhood Trauma and Depression: Insights from HPA Axis Studies in Humans. Psychoneuroendocrinology 2008, 33, 693–710. [Google Scholar] [CrossRef]
- Craig, F.; Tenuta, F.; Rizzato, V.; Costabile, A.; Trabacca, A.; Montirosso, R. Attachment-Related Dimensions in the Epigenetic Era: A Systematic Review of the Human Research. Neurosci. Biobehav. Rev. 2021, 125, 654–666. [Google Scholar] [CrossRef]
- Sun, H.; Kennedy, P.J.; Nestler, E.J. Epigenetics of the Depressed Brain: Role of Histone Acetylation and Methylation. Neuropsychopharmacology 2013, 38, 124–137. [Google Scholar] [CrossRef] [PubMed]
- Lin, E.; Tsai, S.J. Epigenetics and Depression: An Update. Psychiatry Investig. 2019, 16, 654. [Google Scholar] [CrossRef] [PubMed]
- Green, C.; Shen, X.; Stevenson, A.J.; Conole, E.L.S.; Harris, M.A.; Barbu, M.C.; Hawkins, E.L.; Adams, M.J.; Hillary, R.F.; Lawrie, S.M.; et al. Structural Brain Correlates of Serum and Epigenetic Markers of Inflammation in Major Depressive Disorder. Brain Behav. Immun. 2021, 92, 39–48. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. Neurobiological and Systemic Effects of Chronic Stress. Chronic Stress 2017, 1, 2470547017692328. [Google Scholar] [CrossRef]
- Penninx, B.W.J.H.; Lange, S.M.M. Metabolic Syndrome in Psychiatric Patients: Overview, Mechanisms, and Implications. Dialogues Clin. Neurosci. 2018, 20, 63–73. [Google Scholar] [CrossRef]
- Back, S.N.; Flechsenhar, A.; Bertsch, K.; Zettl, M. Childhood Traumatic Experiences and Dimensional Models of Personality Disorder in DSM-5 and ICD-11: Opportunities and Challenges. Curr. Psychiatry Rep. 2021, 23, 60. [Google Scholar] [CrossRef]
- Quah, S.K.L.; Cockcroft, G.J.; McIver, L.; Santangelo, A.M.; Roberts, A.C. Avoidant Coping Style to High Imminence Threat Is Linked to Higher Anxiety-Like Behavior. Front. Behav. Neurosci. 2020, 14, 34. [Google Scholar] [CrossRef]
- APA American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Hofmann, S.G.; Hay, A.C. Rethinking Avoidance: Toward a Balanced Approach to Avoidance in Treating Anxiety Disorders. J. Anxiety Disord. 2018, 55, 14–21. [Google Scholar] [CrossRef]
- Wojcik, K.D.; Cox, D.W.; Kealy, D. Adverse Childhood Experiences and Shame- and Guilt-Proneness: Examining the Mediating Roles of Interpersonal Problems in a Community Sample. Child Abus. Negl. 2019, 98, 104233. [Google Scholar] [CrossRef]
- Servidio, R.; Costanza, S.A.; Costabile, A.; Boca, S. Future Orientation and Symptoms of Anxiety and Depression in Italian University Students during the COVID-19 Pandemic: The Role of Resilience and the Perceived Threat of COVID-19. Healthcare 2022, 10, 974. [Google Scholar] [CrossRef]
- Capone, V.; Caso, D.; Donizzetti, A.R.; Procentese, F. University Student Mentalwell-Being during COVID-19 Outbreak: What Are the Relationships between Information Seeking, Perceived Risk and Personal Resources Related to the Academic Context? Sustainability 2020, 12, 7039. [Google Scholar] [CrossRef]
- Porru, F.; Schuring, M.; Bültmann, U.; Portoghese, I.; Burdorf, A.; Robroek, S.J.W. Associations of University Student Life Challenges with Mental Health and Self-Rated Health: A Longitudinal Study with 6 Months Follow-Up. J. Affect. Disord. 2022, 296, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.; Fernando, S.; Churchill, A.M.; Cornish, P.; Henderson, J.; Shah, J.; Tee, K.; Salmon, A. Scoping Review of Stepped Care Interventions for Mental Health and Substance Use Service Delivery to Youth and Young Adults. Early Interv. Psychiatry 2022, 16, 327–341. [Google Scholar] [CrossRef] [PubMed]
- Karatekin, C.; Ahluwalia, R. Effects of Adverse Childhood Experiences, Stress, and Social Support on the Health of College Students. J. Interpers. Violence 2020, 35, 150–172. [Google Scholar] [CrossRef]
- Von Cheong, E.; Sinnott, C.; Dahly, D.; Kearney, P.M. Adverse Childhood Experiences (ACEs) and Later-Life Depression: Perceived Social Support as a Potential Protective Factor. BMJ Open 2017, 7, e013228. [Google Scholar] [CrossRef]
- Morgan, C.A.; Chang, Y.H.; Choy, O.; Tsai, M.C.; Hsieh, S. Adverse Childhood Experiences Are Associated with Reduced Psychological Resilience in Youth: A Systematic Review and Meta-Analysis. Children 2022, 9, 27. [Google Scholar] [CrossRef]
| Variable | Counseling Group (N = 121) | Non-Counseling Group (N = 255) | Value | p-Value | |
|---|---|---|---|---|---|
| Gender | 9.841 | 0.002 ** | |||
| Male | Count | 37 | 42 | ||
| Expected count | 25.4 | 53.6 | |||
| % within groups | 30.6% | 16.5% | |||
| Female | Count | 84 | 213 | ||
| Expected count | 95.6 | 201.4 | |||
| % within groups | 69.4% | 83.5% | |||
| Relationship status | 1.568 | 0.667 | |||
| Single | Count | 61 | 121 | ||
| Expected count | 59 | 123 | |||
| % within groups | 52.1% | 49.6% | |||
| Engaged | Count | 56 | 120 | ||
| Expected count | 57 | 119 | |||
| % within groups | 47.9% | 49.2% | |||
| Married | Count | 0 | 1 | ||
| Expected count | 0.3 | 0.7 | |||
| % within groups | 0.00% | 0.4% | |||
| Separated | Count | 0 | 2 | ||
| Expected count | 0.6 | 1.4 | |||
| % within groups | 0.00% | 0.8% | |||
| Residential status | 2.686 | 0.443 | |||
| University residence | Count | 16 | 28 | ||
| Expected count | 13.9 | 30.1 | |||
| % within groups | 14.8% | 12.00% | |||
| Apartment | Count | 5 | 6 | ||
| Expected count | 3.5 | 7.5 | |||
| % within groups | 4.6% | 2.6% | |||
| Living with family | Count | 56 | 115 | ||
| Expected count | 54.2 | 116.8 | |||
| % within groups | 51.9% | 49.4% | |||
| Apartment with roommates | Count | 31 | 84 | ||
| Expected count | 36.4 | 78.6 | |||
| % within groups | 28.7% | 36.1% | |||
| GAD-7 level | 22.569 | <0.001 ** | |||
| Minimal | Count | 3 | 28 | ||
| Expected count | 10 | 21 | |||
| % within groups | 2.5% | 11.00% | |||
| Mild | Count | 30 | 103 | ||
| Expected count | 42.8 | 90.2 | |||
| % within groups | 24.8% | 40.4% | |||
| Moderate | Count | 46 | 74 | ||
| Expected count | 38.6 | 81.4 | |||
| % within groups | 38.00% | 29.00% | |||
| Severe | Count | 42 | 50 | ||
| Expected count | 29.6 | 62.4 | |||
| % within groups | 34.7% | 19.6% | |||
| PHQ-9 level | 51.259 | <0.001 ** | |||
| N | Count | 4 | 51 | ||
| Expected count | 17.7 | 37.3 | |||
| % within groups | 3.3% | 20.00% | |||
| Mild | Count | 35 | 117 | ||
| Expected count | 48.9 | 103.1 | |||
| % within groups | 28.9% | 45.9% | |||
| Moderate | Count | 45 | 63 | ||
| Expected count | 34.8 | 73.2 | |||
| % within groups | 37.2% | 24.7% | |||
| Moderately severe | Count | 26 | 21 | ||
| Expected count | 15.1 | 31.9 | |||
| % within groups | 21.5% | 8.2% | |||
| Severe | Count | 11 | 3 | ||
| Expected count | 4.5 | 9.5 | |||
| % within groups | 9.1% | 1.2% | |||
| Mean (SD) | Skewness | Kurtosis | 95% CI | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Counseling | Non-Counseling | Counseling | Non-Counseling | Counseling | Non-Counseling | t | p-Value | Lower | Upper | |
| ACE-Q | 2.26 (1.74) | 1.57 (1.67) | 0.39 | 1.31 | −0.84 | 2.24 | 3.676 | <0.001 ** | 0.32 | 1.055 |
| GAD-7 | 12.46 (4.37) | 9.97 (4.49) | −0.13 | 0.29 | −0.67 | −0.82 | 5.077 | <0.001 ** | 1.528 | 3.46 |
| PHQ-9 | 12.58 (5.24) | 8.22 (4.30) | 0.49 | 0.64 | −0.30 | 0.29 | 8.541 | <0.001 ** | 3.355 | 5.362 |
| PID-5 | ||||||||||
| Negative affectivity | 9.12 (2.55) | 8.27 (2.68) | −0.12 | −0.23 | −0.39 | −0.19 | 2.915 | 0.004 ** | 0.276 | 1.422 |
| Antagonism | 3.21 (2.64) | 2.56 (2.25) | 1.00 | 1.03 | 0.61 | 0.81 | 2.469 | 0.014 * | 0.132 | 1.167 |
| Detachment | 5.89 (2.67) | 4.80 (2.65) | 0.17 | 0.54 | −0.54 | 0.12 | 3.719 | <0.001 ** | 0.515 | 1.67 |
| Disinhibition | 4.98 (2.80) | 4.49 (2.35 | 0.59 | 0.30 | 0.57 | −0.30 | 1.77 | 0.078 | −0.054 | 1.032 |
| Psychoticism | 6.42 (3.13) | 5.41 (2.97) | 0.09 | 0.39 | −0.58 | −0.16 | 3.039 | 0.003 ** | 0.358 | 1.67 |
| Brief-COPE | ||||||||||
| Emotion-focused strategies | 30.02 (5.22) | 26.93 (5.17) | 0.17 | 0.30 | −0.22 | −0.20 | 5.401 | <0.001 ** | 1.966 | 4.217 |
| Problem-focused strategies | 20.98 (4.69) | 20.36 (4.57) | 0.28 | 0.08 | −0.29 | −0.31 | 1.232 | 0.219 | −0.374 | 1.627 |
| Avoidance coping | 15.88 (3.20) | 14.20 (3.07) | 0.22 | 1.02 | −0.18 | 2.20 | 4.879 | <0.001 ** | 1.001 | 2.352 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| - | |||||||||||||
| 0.118 * | - | ||||||||||||
| 0.227 ** | 0.287 ** | - | |||||||||||
| 0.134 ** | 0.139 ** | 0.276 ** | - | ||||||||||
| 0.073 | 0.229 ** | 0.330 ** | 0.357 ** | - | |||||||||
| 0.181 ** | 0.462 ** | 0.404 ** | 0.327 ** | 0.370 ** | - | ||||||||
| −0.004 | 0.062 | −0.263 ** | 0.082 | −0.027 | 0.081 | - | |||||||
| 0.104 * | 0.309 ** | 0.053 | 0.146 ** | 0.045 | 0.234 ** | 0.544 ** | - | ||||||
| 0.280 ** | 0.427 ** | 0.332 ** | 0.282 ** | 0.272 ** | 0.467 ** | 0.143 ** | 0.374 ** | - | |||||
| 0.154 ** | 0.562 ** | 0.286 ** | 0.106 * | 0.272 ** | 0.425 ** | 0.116 * | 0.323 ** | 0.442 ** | - | ||||
| 0.292 ** | 0.482 ** | 0.443 ** | 0.180 ** | 0.318 ** | 0.571 ** | 0.038 | 0.325 ** | 0.506 ** | 0.696 ** | - | |||
| 0.072 | −0.129 * | 0.015 | −0.059 | −0.076 | −0.163 ** | −0.056 | −0.001 | −0.082 | −0.042 | −0.071 | - | ||
| 0.077 | 0.252 ** | 0.053 | −0.116 * | 0.023 | 0.079 | −0.064 | 0.043 | 0.046 | 0.162 ** | 0.114 * | 0.020 | - | |
| −0.187 ** | −0.149 ** | −0.189 ** | −0.127 * | −0.091 | −0.155 ** | −0.064 | −0.269 ** | −0.245 ** | −0.254 ** | −0.404 ** | −0.070 | 0.162 ** | - |
| Pathway | Estimate | SE | z | p | 95% [CI] | Effect Size | ||
|---|---|---|---|---|---|---|---|---|
| ACE-Q -> GAD-7 | PM | SE | 95%CI | |||||
| Total effect | 0.09 | 0.05 | 1.94 | 0.049 * | [0.00, 0.18] | |||
| Direct effect | 0.00 | 0.04 | 0.11 | 0.909 | [−0.07, 0.08] | |||
| Total indirect effect | 0.09 | 0.03 | 2.64 | <0.001 ** | [0.02, 0.15] | |||
| Specific indirect effect | ||||||||
| ACE-Q -> Avoidance -> GAD-7 | 0.03 | 0.01 | 2.35 | 0.019 * | [0.01, 0.07] | 0.38 | 0.16 | [0.07, 0.70] |
| ACE-Q -> PHQ-9 | ||||||||
| Total effect | 0.21 | 0.05 | 4.30 | <0.001 ** | [0.12, 0.31] | |||
| Direct effect | 0.10 | 0.04 | 2.37 | 0.02 * | [0.02, 0.18] | |||
| Total indirect effect | 0.12 | 0.03 | 3.67 | <0.001 ** | [0.05, 0.18] | |||
| Specific indirect effects | ||||||||
| ACE-Q -> Detachment -> PHQ-9 | 0.03 | 0.01 | 2.55 | 0.011 * | [0.01, 0.06] | 0.14 | 0.05 | [0.03, 0.24] |
| ACE-Q -> Psychoticism -> PHQ-9 | 0.05 | 0.02 | 2.79 | 0.005 ** | [0.02, 0.08] | 0.22 | 0.08 | [0.06, 0.38] |
| ACE-Q -> Avoidance ->PHQ-9 | 0.03 | 0.01 | 2.215 | 0.027 * | [0.01, 0.07] | 0.15 | 0.07 | [0.02, 0.29] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Craig, F.; Servidio, R.; Calomino, M.L.; Candreva, F.; Nardi, L.; Palermo, A.; Polito, A.; Spina, M.F.; Tenuta, F.; Costabile, A. Adverse Childhood Experiences and Mental Health among Students Seeking Psychological Counseling Services. Int. J. Environ. Res. Public Health 2023, 20, 5906. https://doi.org/10.3390/ijerph20105906
Craig F, Servidio R, Calomino ML, Candreva F, Nardi L, Palermo A, Polito A, Spina MF, Tenuta F, Costabile A. Adverse Childhood Experiences and Mental Health among Students Seeking Psychological Counseling Services. International Journal of Environmental Research and Public Health. 2023; 20(10):5906. https://doi.org/10.3390/ijerph20105906
Chicago/Turabian StyleCraig, Francesco, Rocco Servidio, Maria Luigia Calomino, Francesca Candreva, Lucia Nardi, Adriana Palermo, Alberto Polito, Maria Francesca Spina, Flaviana Tenuta, and Angela Costabile. 2023. "Adverse Childhood Experiences and Mental Health among Students Seeking Psychological Counseling Services" International Journal of Environmental Research and Public Health 20, no. 10: 5906. https://doi.org/10.3390/ijerph20105906
APA StyleCraig, F., Servidio, R., Calomino, M. L., Candreva, F., Nardi, L., Palermo, A., Polito, A., Spina, M. F., Tenuta, F., & Costabile, A. (2023). Adverse Childhood Experiences and Mental Health among Students Seeking Psychological Counseling Services. International Journal of Environmental Research and Public Health, 20(10), 5906. https://doi.org/10.3390/ijerph20105906





