Interventions for COVID-19 Vaccine Hesitancy: A Systematic Review and Narrative Synthesis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
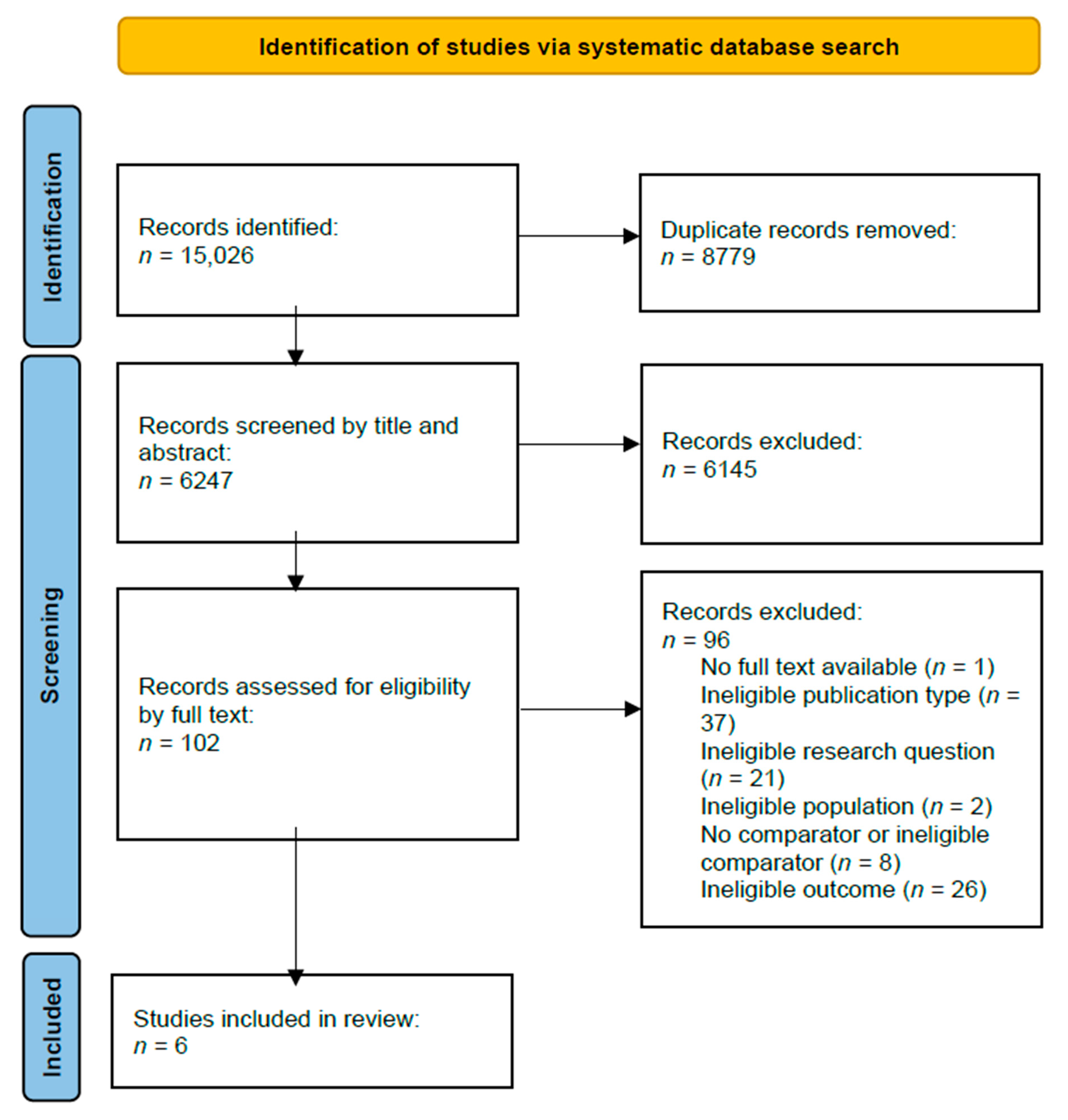
2.3. Study Selection
2.4. Data Extraction
2.5. Risk of Bias Assessment
2.6. Data Synthesis
3. Results
3.1. Overview of Included Studies
3.2. Risk of Bias Assessment
3.3. Effectiveness of COVID-19 Vaccine Hesitancy Interventions
3.3.1. Text-Based Interventions
3.3.2. Infographics
3.3.3. ‘Opt-Out’ Interventions
4. Discussion
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention (CDC). Ten Great Public Health Achievements. 1999. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/00056796.htm (accessed on 2 November 2022).
- Peck, M.; Gacic-Dobo, M.; Diallo, M.S.; Nedelec, Y.; Sodha, S.S.; Wallace, A.S. Global Routine Vaccination Coverage, 2018. MMWR. Morb. Mortal. Wkly. Rep. 2019, 68, 937–942. [Google Scholar] [CrossRef] [PubMed]
- Omer, S.B.; Salmon, D.A.; Orenstein, W.A.; Dehart, M.P.; Halsey, N. Vaccine Refusal, Mandatory Immunization, and the Risks of Vaccine-Preventable Diseases. N. Engl. J. Med. 2009, 360, 1981–1988. [Google Scholar] [CrossRef]
- Dubé, E.; Gagnon, D.; MacDonald, N.E.; Sage Working Group on Vaccine Hesitancy. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 2015, 33, 4191–4203. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization (WHO). Ten Threats to Global Health in 2019; World Health Organization: Geneva, Switzerland, 2019; Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 2 November 2022).
- Rosen, B.; Waitzberg, R.; Israeli, A.; Hartal, M.; Davidovitch, N. Addressing vaccine hesitancy and access barriers to achieve persistent progress in Israel’s COVID-19 vaccination program. Isr. J. Health Policy Res. 2021, 10, 43. [Google Scholar] [CrossRef]
- Lorini, C.; Santomauro, F.; Donzellini, M.; Capecchi, L.; Bechini, A.; Boccalini, S.; Bonanni, P.; Bonaccorsi, G. Health literacy and vaccination: A systematic review. Hum. Vaccines Immunother. 2018, 14, 478–488. [Google Scholar] [CrossRef] [Green Version]
- Ganie, A.R.; Mukhter, I. Misinformation induced anxieties and fear affecting vaccination programs: Challenge for COVID-19 vaccination program. J. Fam. Med. Prim. Care 2022, 11, 405. [Google Scholar] [CrossRef]
- Rief, W. Fear of Adverse Effects and COVID-19 Vaccine Hesitancy: Recommendations of the Treatment Expectation Expert Group. JAMA Health Forum 2021, 2, e210804. [Google Scholar] [CrossRef]
- Quinn, S.C.; Andrasik, M.P. Addressing Vaccine Hesitancy in BIPOC Communities—Toward Trustworthiness, Partnership, and Reciprocity. N. Engl. J. Med. 2021, 385, 97–100. [Google Scholar] [CrossRef]
- Vergara, R.J.D.; Sarmiento, P.J.D.; Lagman, J.D.N. Building public trust: A response to COVID-19 vaccine hesitancy predicament. J. Public Health 2021, 43, e291–e292. [Google Scholar] [CrossRef]
- Agarwal, R.; Dugas, M.; Ramaprasad, J.; Luo, J.; Li, G.; Gao, G. Socioeconomic privilege and political ideology are associated with racial disparity in COVID-19 vaccination. Proc. Natl. Acad. Sci. USA 2021, 118, e2107873118. [Google Scholar] [CrossRef]
- Larson, H.J.; Gakidou, E.; Murray, C.J. The Vaccine-Hesitant Moment. N. Engl. J. Med. 2022, 387, 58–65. [Google Scholar] [CrossRef]
- Skafle, I.; Nordahl-Hansen, A.; Quintana, D.S.; Wynn, R.; Gabarron, E. Misinformation About COVID-19 Vaccines on Social Media: Rapid Review. J. Med. Internet Res. 2022, 24, e37367. [Google Scholar] [CrossRef]
- Vosoughi, S.; Roy, D.; Aral, S. The spread of true and false news online. Science 2018, 359, 1146–1151. [Google Scholar] [CrossRef] [PubMed]
- Dube, E.; Bettinger, J.A.; Halperin, B.; Bradet, R.; Lavoie, F.; Sauvageau, C.; Gilca, V.; Boulianne, N. Determinants of parents’ decision to vaccinate their children against rotavirus: Results of a longitudinal study. Health Educ. Res. 2012, 27, 1069–1080. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, P.J.; Humiston, S.G.; Marcuse, E.K.; Zhao, Z.; Dorell, C.G.; Howes, C.; Hibbs, B. Parental Delay or Refusal of Vaccine Doses, Childhood Vaccination Coverage at 24 Months of Age, and the Health Belief Model. Public Health Rep. 2011, 126 (Suppl. 2), 135–146. [Google Scholar] [CrossRef] [Green Version]
- Smith, P.J.; Humiston, S.G.; Parnell, T.; Vannice, K.S.; Salmon, D.A. The Association Between Intentional Delay of Vaccine Administration and Timely Childhood Vaccination Coverage. Public Health Rep. 2010, 125, 534–541. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 2 November 2022).
- World Health Organization (WHO). COVID-19 Vaccines; World Health Organization: Geneva, Switzerland; Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines (accessed on 2 November 2022).
- Public Health Agency of Canada. COVID-19 Vaccination Coverage in Canada. 2022. Available online: https://health-infobase.canada.ca/covid-19/vaccination-coverage (accessed on 2 November 2022).
- Failla, G.; Pantovic, A.; Al-Ajlouni, Y.; Ricciardi, W.; Cascini, F. How the population worldwide is reacting to the COVID-19 vaccines: A systematic review on hesitancy. Eur. J. Public Health 2021, 31 (Suppl. 3), ckab164-405. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Wake, A.D. The Willingness to Receive COVID-19 Vaccine and Its Associated Factors: “Vaccination Refusal Could Prolong the War of This Pandemic”—A Systematic Review. Risk Manag. Health Policy 2021, 14, 2609–2623. [Google Scholar] [CrossRef]
- Dhanani, L.Y.; Franz, B. A meta-analysis of COVID-19 vaccine attitudes and demographic characteristics in the United States. Public Health 2022, 207, 31–38. [Google Scholar] [CrossRef]
- Muhajarine, N.; Adeyinka, D.A.; McCutcheon, J.; Green, K.L.; Fahlman, M.; Kallio, N. COVID-19 vaccine hesitancy and refusal and associated factors in an adult population in Saskatchewan, Canada: Evidence from predictive modelling. PLoS ONE 2021, 16, e0259513. [Google Scholar] [CrossRef]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; et al. Strategies for Addressing Vaccine Hesitancy—A Systematic Review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olson, O.; Berry, C.; Kumar, N. Addressing Parental Vaccine Hesitancy towards Childhood Vaccines in the United States: A Systematic Literature Review of Communication Interventions and Strategies. Vaccines 2020, 8, 590. [Google Scholar] [CrossRef] [PubMed]
- Vujovich-Dunn, C.; Kaufman, J.; King, C.; Skinner, S.R.; Wand, H.; Guy, R.; Leask, J. A systematic review and meta-analysis of effectiveness of decision aids for vaccination decision-making. Vaccine 2021, 39, 3655–3665. [Google Scholar] [CrossRef] [PubMed]
- Reñosa, M.D.C.; Landicho, J.; Wachinger, J.; Dalglish, S.L.; Bärnighausen, K.; Bärnighausen, T.; McMahon, S.A. Nudging toward vaccination: A systematic review. BMJ Glob. Health 2021, 6, e006237. [Google Scholar] [CrossRef]
- Batteux, E.; Mills, F.; Jones, L.F.; Symons, C.; Weston, D. The Effectiveness of Interventions for Increasing COVID-19 Vaccine Uptake: A Systematic Review. Vaccines 2022, 10, 386. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [Green Version]
- Covidence Systematic Review Software: Veritas Health Innovation (2022). Available online: www.covidence.org (accessed on 26 April 2022).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Crutcher, M.; Seidler, P.M. Maximizing Completion of the Two-Dose COVID-19 Vaccine Series with Aid from Infographics. Vaccines 2021, 9, 1229. [Google Scholar] [CrossRef]
- Chan, D.K.; Alegria, B.D.; Chadaga, S.R.; Goren, L.J.; Mikasa, T.J.; Pearson, A.M.; Podolsky, S.R.; Won, R.S.; LeTourneau, J.L. Rapid Deployment of Multiple Tactics to Address Severe Acute Respiratory Syndrome Coronavirus 2 Vaccine Uptake in Healthcare Employees with a Focus on Those Who Identify as Black, Indigenous, and People of Color. Open Forum Infect. Dis. 2022, 9, ofac012. [Google Scholar] [CrossRef]
- Dai, H.; Saccardo, S.; Han, M.A.; Roh, L.; Raja, N.; Vangala, S.; Modi, H.; Pandya, S.; Sloyan, M.; Croymans, D.M. Behavioural nudges increase COVID-19 vaccinations. Nature 2021, 597, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Lieu, T.A.; Elkin, E.P.; Escobar, P.R.; Finn, L.; Klein, N.P.; Durojaiye, C.; Prausnitz, S.; Quesenberry, C.P.; Sawyer, D.; Teran, S.; et al. Effect of Electronic and Mail Outreach from Primary Care Physicians for COVID-19 Vaccination of Black and Latino Older Adults: A Randomized Clinical Trial. JAMA Netw. Open 2022, 5, e2217004. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.J.; Mallozzi, C.; Shaw, P.A.; Reitz, C.; McDonald, C.; Vandertuyn, M.; Balachandran, M.; Kopinsky, M.; Sevinc, C.; Johnson, A.; et al. Effect of Text Messaging and Behavioral Interventions on COVID-19 Vaccination Uptake: A Randomized Clinical Trial. JAMA Netw. Open 2022, 5, e2216649. [Google Scholar] [CrossRef] [PubMed]
- Tentori, K.; Pighin, S.; Giovanazzi, G.; Grignolio, A.; Timberlake, B.; Ferro, A. Nudging COVID-19 Vaccine Uptake by Changing the Default: A Randomized Controlled Trial. Med. Decis. Mak. 2022, 42, 837–841. [Google Scholar] [CrossRef]
- Guerra, F.A. Delays in Immunization Have Potentially Serious Health Consequences. Pediatr. Drugs 2007, 9, 143–148. [Google Scholar] [CrossRef]
- Serra-Garcia, M.; Szech, N. Choice Architecture and Incentives Increase COVID-19 Vaccine Intentions and Test Demand. SSRN Electron. J. 2021. WZB Discussion Paper, No. SP II 2021-302. [Google Scholar] [CrossRef]
- Dhanani, L.Y.; Franz, B. An experimental study of the effects of messaging strategies on vaccine acceptance and hesitancy among Black Americans. Prev. Med. Rep. 2022, 27, 101792. [Google Scholar] [CrossRef]
- Chambers, L.; Wilson, K.; Hawken, S.; Puxty, J.; Crowe, L.; Lam, P.-P.; Farmanova-Haynes, E.; McNeil, S.; McCarthy, A. Impact of the Ottawa Influenza Decision Aid on healthcare personnel’s influenza immunization decision: A randomized trial. J. Hosp. Infect. 2012, 82, 194–202. [Google Scholar] [CrossRef]
- Wroe, A.L.; Turner, N.; Owens, R.G. Evaluation of a decision-making aid for parents regarding childhood immunizations. Health Psychol. 2005, 24, 539–547. [Google Scholar] [CrossRef]
- Witteman, H.O.; Chipenda Dansokho, S.; Exe, N.; Dupuis, A.; Provencher, T.; Zikmund-Fisher, B.J. Risk communication, values clarification, and vaccination decisions. Risk Anal. 2015, 35, 1801–1819. [Google Scholar] [CrossRef] [Green Version]
- Clancy, C.M.; Cebul, R.D.; Williams, S.V. Guiding individual decisions: A randomized, controlled trial of decision analysis. Am. J. Med. 1988, 84, 283–288. [Google Scholar] [CrossRef]
- Shourie, S.; Jackson, C.; Cheater, F.M.; Bekker, H.L.; Edlin, R.; Tubeuf, S.; Harrison, W.; McAleese, E.; Schweiger, M.; Bleasby, B. A cluster randomised controlled trial of a web based decision aid to support parents’ decisions about their child’s Measles Mumps and Rubella (MMR) vaccination. Vaccine 2013, 31, 6003–6010. [Google Scholar] [CrossRef] [PubMed]
- Barber, A.; West, J. Conditional cash lotteries increase COVID-19 vaccination rates. J. Health Econ. 2022, 81, 102578. [Google Scholar] [CrossRef]
- Lang, D.; Esbenshade, L.; Willer, R. Did Ohio’s Vaccine Lottery Increase Vaccination Rates? A Pre-Registered, Synthetic Control Study. J. Exp. Politi. Sci. 2022, 1–19. [Google Scholar] [CrossRef]
- Mallow, P.J.; Enis, A.; Wackler, M.; Hooker, E.A. COVID-19 financial lottery effect on vaccine hesitant areas: Results from Ohio’s Vax-a-million program. Am. J. Emerg. Med. 2022, 56, 316–317. [Google Scholar] [CrossRef]
- Sehgal, N.K. Impact of Vax-a-Million Lottery on COVID-19 Vaccination Rates in Ohio. Am. J. Med. 2021, 134, 1424–1426. [Google Scholar] [CrossRef] [PubMed]
- Walkey, A.J.; Law, A.; Bosch, N.A. Lottery-Based Incentive in Ohio and COVID-19 Vaccination Rates. JAMA 2021, 326, 766–767. [Google Scholar] [CrossRef] [PubMed]
- Ohio Department of Health. Ohio Vax-a-Million Details Announced. 2021. Available online: https://odh.ohio.gov/media-center/odh-news-releases/odh-news-release-05-17-21 (accessed on 2 November 2022).
- Acharya, B.; Dhakal, C. Implementation of State Vaccine Incentive Lottery Programs and Uptake of COVID-19 Vaccinations in the United States. JAMA Netw. Open 2021, 4, e2138238. [Google Scholar] [CrossRef]
- Sprengholz, P.; Eitze, S.; Felgendreff, L.; Korn, L.; Betsch, C. Money is not everything: Experimental evidence that payments do not increase willingness to be vaccinated against COVID-19. J. Med. Ethics 2021, 47, 547–548. [Google Scholar] [CrossRef]
- Milkman, K.L.; Patel, M.S.; Gandhi, L.; Graci, H.; Gromet, D.; Ho, Q.D.H.; Kay, J.; Lee, T.; Akinola, M.; Beshears, J.; et al. A Mega-Study of Text-Based Nudges Encouraging Patients to Get Vaccinated at an Upcoming Doctor’s Appointment. SSRN Electron. J. 2021. [Google Scholar] [CrossRef]
- Khatri, H.; Cox, N.; Rajagopala, L.; Bateman, J. P076 Innovative SMS based COVID-19 vaccination video advice: Real-world evidence of the positive impact on vaccination uptake in a large single-centre cohort. Rheumatology 2022, 61 (Suppl. 1), keac133-075. [Google Scholar] [CrossRef]
- Gopalakrishnan, S.; Ganeshkumar, P. Systematic reviews and meta-analysis: Understanding the best evidence in primary healthcare. J. Fam. Med. Prim. Care 2013, 2, 9–14. [Google Scholar] [CrossRef]
| Research question | Study implements and evaluates a non-financial intervention intended to address COVID-19 vaccine hesitancy and increase vaccine uptake |
| Population | Adults who are hesitant to receive the COVID-19 vaccine |
| Intervention | Intervention implemented to address COVID-19 vaccine hesitancy and increase COVID-19 vaccination rates |
| Comparator | Eligible comparators included:
|
| Outcome | COVID-19 vaccination rate (i.e., self-reported, immunization/medical records) |
| Study design | Peer-reviewed comparative studies (i.e., randomized controlled trials, non-randomized trials, cohort studies, case-control studies) |
| Citation | Study Design | Participants and Study Period | Intervention Type | Comparator | Outcome Variable | Key Findings | Risk of Bias |
|---|---|---|---|---|---|---|---|
| Chan et al., 2022 [36] | Non-randomized uncontrolled before–after study | Healthcare employees (n = 13,942) living in Oregon and Washington state, USA (August–October 2021) | Complex intervention with multiple components (including town halls, meetings, optional vaccine counselling, etc.) | Before–after comparison | Rate of complete vaccination among participants (immunization records obtained via state CDC Immunization Information Systems and reconciled with EMR employee data) | 9.8% absolute increase in complete vaccination rate after intervention | Moderate |
| Crutcher & Seidler, 2021 [35] | Non-randomized controlled cluster trial | Adults and children >12 years (number of participants not reported) living in Los Angeles, California, USA (June–July 2021) | Educational infographic | Control group (county-wide) comparison and before–after comparison | Completion of second vaccine dose for COVID-19 (determined from Lincoln Park vaccination site records) | The Lincoln Park vaccination site served 15.8% more second-dose recipients when compared to all of Los Angeles County vaccine sites in the same timeframe | Moderate |
| Dai et al., 2021 [37] | 2 sequential randomized controlled trials | Adult patients (n = 93,354 for first trial, n = 67,092 for second trial) from the UCLA Health patient list in Los Angeles, California, USA (January–May 2021) | Text-based reminders with or without video | Control group (for both trials) | Vaccination rates (immunization records available through the UCLA healthcare system) | The first reminder (first trial intervention) resulted in a 3.57% absolute increase in vaccine uptake, and the second reminder (second trial intervention) resulted in a 1.06% absolute increase. | Low |
| Lieu et al., 2022 [38] | Randomized controlled trial | Latino and Black adults (n = 8287) living in Northern California, USA (March–May 2021) | Culturally tailored outreach via letters and secure electronic messaging | Control group (usual care) | Completion of at least 1 dose of a COVID-19 vaccine (according to state immunization records) | Patients receiving both standard (adjusted HR: 1.17; 95% CI, 1.04–1.31) and culturally tailored (aHR: 1.22; 95% CI, 1.09–1.37) outreach demonstrated higher vaccination rates compared to usual care | Some concerns |
| Mehta et al., 2022 [39] | Randomized controlled trial | Adults (n = 16,045) living in Philadelphia, Pennsylvania, USA (April–July 2021) | Text message, with standard, scarcity, clinical endorsement, and endowment message framing | Control group (received standard telephone call) | Proportion of patients who completed the first dose of the COVID-19 vaccine within 1 month of intervention (according to EMR) | No detectable increase in vaccine uptake among patients receiving text messages or behaviourally informed message content compared to telephone calls only | Low |
| Tentori et al., 2022 [40] | Randomized controlled trial | Adults (n = 2000) living in Trento Province, Italy (July–August 2021) | Vaccine appointment booking, with option to ‘opt-out’ | Control group (received usual ‘opt-in’ option to schedule vaccination appointment) | Vaccination rate (obtained from provincial records) | 32% relative increase in vaccination rate among those in ‘opt-out’ group when compared to the ‘opt-in’ (control) group | Low |
| Intervention | Observation and Rationale |
|---|---|
| Text-based reminders and outreach | Basic reminders and outreach delivered by SMS text messages, letters, or secure electronic messaging may be effective at increasing COVID-19 vaccine uptake [37,38]. Text message reminders have similarly been shown to increase influenza vaccination rates [57]. However, this type of outreach may not always be effective, particularly if individuals have already received previous reminders [39]. |
| Videos | Authors of 1 high-quality RCT did not observe higher vaccine uptake among participants who received an informational video compared to participants who only received a text reminder [37]. However, a study by Khatri et al. (2022) reported that an educational video on COVID-19 vaccines was associated with increased COVID-19 vaccine intentions [58]. |
| Infographics | Further research is needed to determine whether educational infographics are an effective intervention for COVID-19 vaccine hesitancy. However, results from a moderate-quality non-randomized study suggest that infographics may encourage first vaccine dose recipients to return for their second dose [35]. |
| Opt-out vaccine appointment scheduling | Preliminary evidence suggests that opt-out vaccine appointment scheduling systems may be effective at increasing COVID-19 vaccine uptake [40] and intentions [42]. |
| Multi-modal interventions | Results from a moderate-quality non-randomized study suggest that a multi-modal intervention approach (with elements such as town halls, staff meetings, and vaccine safety education and counselling) may be effective at increasing vaccine uptake, specifically among healthcare workers [36]. Further research is needed to determine whether certain components of the multiple intervention approach described by Chan et al. (2022) are more effective than others [36], and whether this approach could be feasibly generalized to a broader population. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Terrell, R.; Alami, A.; Krewski, D. Interventions for COVID-19 Vaccine Hesitancy: A Systematic Review and Narrative Synthesis. Int. J. Environ. Res. Public Health 2023, 20, 6082. https://doi.org/10.3390/ijerph20126082
Terrell R, Alami A, Krewski D. Interventions for COVID-19 Vaccine Hesitancy: A Systematic Review and Narrative Synthesis. International Journal of Environmental Research and Public Health. 2023; 20(12):6082. https://doi.org/10.3390/ijerph20126082
Chicago/Turabian StyleTerrell, Rowan, Abdallah Alami, and Daniel Krewski. 2023. "Interventions for COVID-19 Vaccine Hesitancy: A Systematic Review and Narrative Synthesis" International Journal of Environmental Research and Public Health 20, no. 12: 6082. https://doi.org/10.3390/ijerph20126082






