Identifying Environmental Impact Factors for Sustainable Healthcare: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Methodological Overview
2.2. Search Strategy and Selection Criteria
2.3. Data Abstraction and Analysis
3. Results
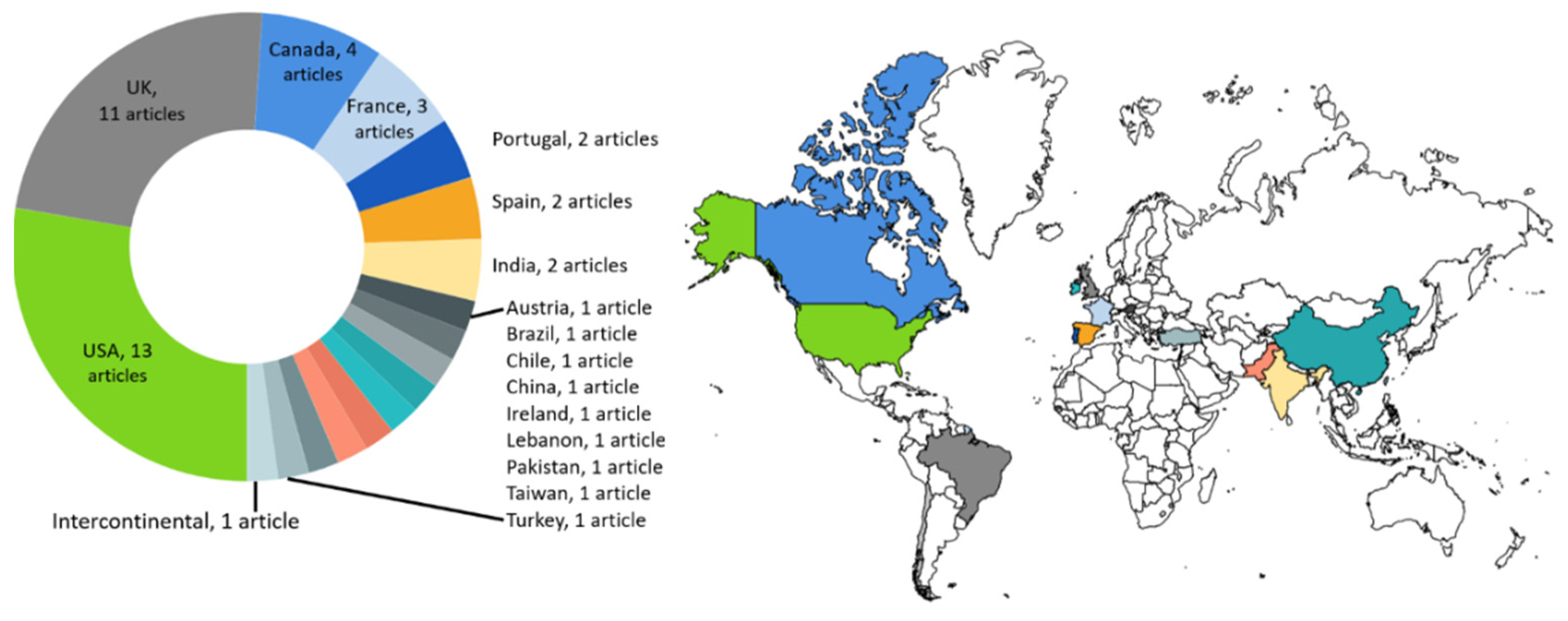
3.1. Descriptive Analysis
3.2. Content Analysis
3.2.1. Healthcare Settings, Environmental Pressures and Impact Factors
3.2.2. Completeness of Identified Factors
4. Discussion
4.1. Interpretation within the Context of the Wider Literature
4.2. Implications for Practice
4.2.1. A “Menu-Card” for Selecting Environmental Impact Factors
4.2.2. Development of New Environmental Impact Factors
4.3. Limitations
4.4. Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Van Daalen, K.R.; Romanello, M.; Rocklöv, J.; Semenza, J.C.; Tonne, C.; Markandya, A.; Dasandi, N.; Jankin, S.; Achebak, H.; Ballester, J.; et al. The 2022 Europe report of the Lancet Countdown on health and climate change: Towards a climate resilient future. Lancet Public Health 2022, 7, e942–e965. [Google Scholar] [CrossRef] [PubMed]
- Pichler, P.P.; Jaccard, I.S.; Weisz, U.; Weisz, H. International Comparison of Health Care Carbon Footprints. Environ. Res. Lett. 2019, 14, 064004. [Google Scholar] [CrossRef]
- Eckelman, M.J.; Huang, K.; Lagasse, R.; Senay, E.; Dubrow, R.; Sherman, J.D. Health Care Pollution And Public Health Damage In The United States: An Update: Study Examines Health Care Pollution and Public Health Damage in the United States. Health Aff. 2020, 39, 2071–2079. [Google Scholar] [CrossRef]
- Lenzen, M.; Malik, A.; Li, M.; Fry, J.; Weisz, H.; Pichler, P.-P.; Chaves, L.S.M.; Capon, A.; Pencheon, D. The Environmental Footprint of Health Care: A Global Assessment. Lancet Planet. Health 2020, 4, e271–e279. [Google Scholar] [CrossRef]
- Corvalan, C.; Villalobos Prats, E.; Sena, A.; Campbell-Lendrum, D.; Karliner, J.; Risso, A.; Wilburn, S.; Slotterback, S.; Rathi, M.; Stringer, R.; et al. Towards Climate Resilient and Environmentally Sustainable Health Care Facilities. Int. J. Environ. Res. Public Health 2020, 17, 8849. [Google Scholar] [CrossRef] [PubMed]
- Mortimer, F.; Isherwood, J.; Wilkinson, A.; Vaux, E. Sustainability in Quality Improvement: Redefining Value. Future Healthc. J. 2018, 5, 88–93. [Google Scholar] [CrossRef]
- Spoyalo, K.; Lalande, A.; Rizan, C.; Park, S.; Simons, J.; Dawe, P.; Brown, C.J.; Lillywhite, R.; MacNeill, A.J. Patient, Hospital and Environmental Costs of Unnecessary Bloodwork: Capturing the Triple Bottom Line of Inappropriate Care in General Surgery Patients. BMJ Open Qual. 2023, 12, e002316. [Google Scholar] [CrossRef]
- Ghannadpour, S.F.; Zandieh, F.; Esmaeili, F. Optimizing Triple Bottom-Line Objectives for Sustainable Health-Care Waste Collection and Routing by a Self-Adaptive Evolutionary Algorithm: A Case Study from Tehran Province in Iran. J. Clean. Prod. 2021, 287, 125010. [Google Scholar] [CrossRef]
- McArdle, S. ISQua’s Statement on Sustainability in Health Care. Available online: https://isqua.org/latest/isqua-s-statement-on-sustainability-in-health-care.html (accessed on 11 July 2023).
- Crosby, P.B. Crosby’s 14 Steps to Improvement. Qual. Prog. 2005, 38, 60–64. [Google Scholar]
- Marr, B. Key Performance Indicators, 1st ed.; Pearson: Harlow, UK, 2013; pp. 311–343. [Google Scholar]
- Seelbach, C.L.; Brannan, G.D. Quality Management; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Schmidt, L.; Bohnet-Joschko, S. Planetary Health and Hospitals’ Contribution—A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 13536. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan — a web and mobile app for systematic reviews. Systematic Review 2016, 5, 210. [Google Scholar] [CrossRef]
- OECD. Framework of OECD Work on Environmental Data and Indicators. In Environment at a Glance 2013; OECD Publishing: Paris, France, 2013; pp. 9–10. [Google Scholar] [CrossRef]
- Prats, E.V. WHO Guidance for Climate-Resilient and Environmentally Sustainable Health Care Facilities, 1st ed.; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Jolibois, B.; Guerbet, M.; Vassal, S. Glutaraldehyde in Hospital Wastewater. Arch. Environ. Contam. Toxicol. 2002, 42, 137–144. [Google Scholar] [CrossRef]
- Gilliam, A.D.; Davidson, B.; Guest, J. The Carbon Footprint of Laparoscopic Surgery: Should We Offset? Surg. Endosc. 2008, 22, 573. [Google Scholar] [CrossRef]
- Seifrtová, M.; Pena, A.; Lino, C.M.; Solich, P. Determination of Fluoroquinolone Antibiotics in Hospital and Municipal Wastewaters in Coimbra by Liquid Chromatography with a Monolithic Column and Fluorescence Detection. Anal. Bioanal. Chem. 2008, 391, 799–805. [Google Scholar] [CrossRef]
- Somner, J.E.A.; Stone, N.; Koukkoulli, A.; Scott, K.M.; Field, A.R.; Zygmunt, J. Surgical Scrubbing: Can We Clean up Our Carbon Footprints by Washing Our Hands? J. Hosp. Infect. 2008, 70, 212–215. [Google Scholar] [CrossRef] [PubMed]
- Lin, A.Y.C.; Wang, X.H.; Lin, C.F. Impact of Wastewaters and Hospital Effluents on the Occurrence of Controlled Substances in Surface Waters. Chemosphere 2010, 81, 562–570. [Google Scholar] [CrossRef]
- Masino, C.; Rubinstein, E.; Lem, L.; Purdy, B.; Rossos, P.G. The Impact of Telemedicine on Greenhouse Gas Emissions at an Academic Health Science Center in Canada. Telemed. E-Health 2010, 16, 973–976. [Google Scholar] [CrossRef] [PubMed]
- Connor, A.; Lillywhite, R.; Cooke, M.W. The Carbon Footprint of a Renal Service in the United Kingdom. QJM 2010, 103, 965–975. [Google Scholar] [CrossRef] [PubMed]
- Zander, A.; Niggebrugge, A.; Pencheon, D.; Lyratzopoulos, G. Changes in Travel-Related Carbon Emissions Associated with Modernization of Services for Patients with Acute Myocardial Infarction: A Case Study. J. Public Health 2011, 33, 272–279. [Google Scholar] [CrossRef]
- Eker, H.H.; Bilgili, M.S. Statistical Analysis of Waste Generation in Healthcare Services: A Case Study. Waste Manag. Res. 2011, 29, 791–796. [Google Scholar] [CrossRef]
- Riedel, L.M. Environmental and Financial Impact of a Hospital Recycling Program. AANA J. 2011, 79, S8–S14. [Google Scholar]
- Grimmond, T.; Reiner, S. Impact on Carbon Footprint: A Life Cycle Assessment of Disposable versus Reusable Sharps Containers in a Large US Hospital. Waste Manag. Res. 2012, 30, 639–642. [Google Scholar] [CrossRef]
- Power, N.E.; Silberstein, J.L.; Ghoneim, T.P.; Guillonneau, B.; Touijer, K.A. Environmental Impact of Minimally Invasive Surgery in the United States: An Estimate of the Carbon Dioxide Footprint. J. Endourol. 2012, 26, 1639–1644. [Google Scholar] [CrossRef] [PubMed]
- Goullé, J.P.; Saussereau, E.; Mahieu, L.; Cellier, D.; Spiroux, J.; Guerbet, M. Importance of Anthropogenic Metals in Hospital and Urban Wastewater: Its Significance for the Environment. Bull. Environ. Contam. Toxicol. 2012, 89, 1220–1224. [Google Scholar] [CrossRef] [PubMed]
- Tay, S.; Weinberg, L.; Peyton, P.; Story, D.; Briedis, J. Financial and Environmental Costs of Manual versus Automated Control of End-Tidal Gas Concentrations. Anaesth. Intensive Care 2013, 41, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Morris, D.S.; Wright, T.; Somner, J.E.A.; Connor, A. The Carbon Footprint of Cataract Surgery. Eye 2013, 27, 495–501. [Google Scholar] [CrossRef]
- Gros, M.; Rodríguez-Mozaz, S.; Barceló, D. Rapid Analysis of Multiclass Antibiotic Residues and Some of Their Metabolites in Hospital, Urban Wastewater and River Water by Ultra-High-Performance Liquid Chromatography Coupled to Quadrupole-Linear Ion Trap Tandem Mass Spectrometry. J. Chromatogr. A 2013, 1292, 173–188. [Google Scholar] [CrossRef]
- Southorn, T.; Norrish, A.; Gardner, K.; Baxandall, R. Reducing the Carbon Footprint of the Operating Theatre: A Multicentre Quality Improvement Report. J. Perioper. Pract. 2013, 23, 144–146. [Google Scholar] [CrossRef]
- Debois, W.; Prata, J.; Elmer, B.; Liu, J.; Fominyam, E.; Salemi, A. Improved Environmental Impact with Diversion of Perfusion Bypass Circuit to Municipal Solid Waste. J. Extra Corpor. Technol. 2013, 45, 143–145. [Google Scholar] [CrossRef]
- Diwan, V.; Stålsby Lundborg, C.; Tamhankar, A.J. Seasonal and Temporal Variation in Release of Antibiotics in Hospital Wastewater: Estimation Using Continuous and Grab Sampling. PLoS ONE 2013, 8, e68715. [Google Scholar] [CrossRef]
- Lui, J.T.; Rudmik, L.; Randall, D.R. Reducing the Preoperative Ecological Footprint in Otolaryngology. Otolaryngol. Head Neck Surg. 2014, 151, 805–810. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, C.J.; Gerstenmaier, J.F.; O’Neill, A.C.; McEvoy, S.H.; Hegarty, C.; Heffernan, E.J. “EcoRadiology”—Pulling the Plug on Wasted Energy in the Radiology Department. Acad. Radiol. 2014, 21, 1563–1566. [Google Scholar] [CrossRef]
- Maamari, O.; Brandam, C.; Lteif, R.; Salameh, D. Health Care Waste Generation Rates and Patterns: The Case of Lebanon. Waste Manag. 2015, 43, 550–554. [Google Scholar] [CrossRef] [PubMed]
- Dias-Ferreira, C.; Santos, T.; Oliveira, V. Hospital Food Waste and Environmental and Economic Indicators—A Portuguese Case Study. Waste Manag. 2015, 46, 146–154. [Google Scholar] [CrossRef]
- Thiel, C.L.; Eckelman, M.; Guido, R.; Huddleston, M.; Landis, A.E.; Sherman, J.; Shrake, S.O.; Copley-Woods, N.; Bilec, M.M. Environmental Impacts of Surgical Procedures: Life Cycle Assessment of Hysterectomy in the United States. Environ. Sci. Technol. 2015, 49, 1779–1786. [Google Scholar] [CrossRef] [PubMed]
- De Sa, D.; Stephens, K.; Kuang, M.; Simunovic, N.; Karlsson, J.; Ayeni, O.R. The Direct Environmental Impact of Hip Arthroscopy for Femoroacetabular Impingement: A Surgical Waste Audit of Five Cases. J. Hip. Preserv. Surg. 2016, 3, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Maughan, D.; Lillywhite, R.; Pearce, S.; Pillinger, T.; Weich, S. Evaluating Sustainability: A Retrospective Cohort Analysis of the Oxfordshire Therapeutic Community. BMC Psychiatry 2016, 16, 285. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Zhou, R.; Du, C.; Meng, F.; Wang, Y.; Wu, L.; Wang, F.; Xu, Y.; Yang, X. The Carbon Footprints of Home and In-Center Peritoneal Dialysis in China. Int. Urol. Nephrol. 2017, 49, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Jha, R.R.; Singh, N.; Kumari, R.; Patel, D.K. Ultrasound-Assisted Emulsification Microextraction Based on a Solidified Floating Organic Droplet for the Rapid Determination of 19 Antibiotics as Environmental Pollutants in Hospital Drainage and Gomti River Water. J. Sep. Sci. 2017, 40, 2694–2702. [Google Scholar] [CrossRef]
- MacNeill, A.J.; Lillywhite, R.; Brown, C.J. The Impact of Surgery on Global Climate: A Carbon Footprinting Study of Operating Theatres in Three Health Systems. Lancet Planet. Health 2017, 1, e381–e388. [Google Scholar] [CrossRef]
- Berner, J.E.; Gras, M.D.P.; Troisi, L.; Chapman, T.; Vidal, P. Measuring the Carbon Footprint of Plastic Surgery: A Preliminary Experience in a Chilean Teaching Hospital. J. Plast. Reconstr. Aesthet. Surg. 2017, 70, 1777–1779. [Google Scholar] [CrossRef]
- Esmaeili, A.; McGuire, C.; Overcash, M.; Ali, K.; Soltani, S.; Twomey, J. Environmental Impact Reduction as a New Dimension for Quality Measurement of Healthcare Services: The Case of Magnetic Resonance Imaging. J. Health Care Qual. Assur. 2018, 31, 910–922. [Google Scholar] [CrossRef] [PubMed]
- Khan, B.A.; Khan, A.A.; Ali, M.; Cheng, L. Greenhouse Gas Emission from Small Clinics Solid Waste Management Scenarios in an Urban Area of an Underdeveloping Country: A Life Cycle Perspective. J. Air Waste Manag. Assoc. 2019, 69, 823–833. [Google Scholar] [CrossRef]
- Wilkinson, A.J.K.; Braggins, R.; Steinbach, I.; Smith, J. Costs of Switching to Low Global Warming Potential Inhalers. An Economic and Carbon Footprint Analysis of NHS Prescription Data in England. BMJ Open 2019, 9, e028763. [Google Scholar] [CrossRef]
- Kooner, S.; Hewison, C.; Sridharan, S.; Lui, J.; Matthewson, G.; Johal, H.; Clark, M. Waste and Recycling among Orthopedic Subspecialties. Can. J. Surg. 2020, 63, E278–E283. [Google Scholar] [CrossRef]
- Hsu, S.; Theil, C.; Mello, M.; Slutzman, J. Dumpster Diving in the Emergency Department: Quantity and Characteristics of Waste at a Level I Trauma Center. West, J. Emerg. Med. 2020, 21, 1211. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira Klein, M.; Serrano, S.V.; Santos-Neto, Á.; Da Cruz, C.; Brunetti, I.A.; Lebre, D.; Gimenez, M.P.; Reis, R.M.; Silveira, H.C.S. Detection of Anti-Cancer Drugs and Metabolites in the Effluents from a Large Brazilian Cancer Hospital and an Evaluation of Ecotoxicology. Environ. Pollut. 2021, 268, 115857. [Google Scholar] [CrossRef] [PubMed]
- Rammelkamp, Z.; Dirnberger, J.; Johnson, G.; Waisbren, S. An Audit of All Waste Leaving the Operating Room: Can the Surgical Suite Be More Environmentally Sustainable? World Med. Health Policy 2021, 13, 126–136. [Google Scholar] [CrossRef]
- García-Sanz-Calcedo, J.; De Sousa Neves, N.; Almeida Fernandes, J.P. Measurement of Embodied Carbon and Energy of HVAC Facilities in Healthcare Centers. J. Clean. Prod. 2021, 289, 125151. [Google Scholar] [CrossRef]
- Patel, S.D.; Smith-Steinert, R. Greening the Operating Room, One Procedure at a Time. J. Clim. Chang. Health 2021, 2, 100014. [Google Scholar] [CrossRef]
- Cameron, T.W.; Vo, L.V.; Emerson, L.K.; Emerson, M.V.; Emerson, G.G. Medical Waste Due to Intravitreal Injection Procedures in a Retina Clinic. J. Vitreoretin. Dis. 2021, 5, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Chua, A.L.B.; Amin, R.; Zhang, J.; Thiel, C.L.; Gross, J.S. The Environmental Impact of Interventional Radiology: An Evaluation of Greenhouse Gas Emissions from an Academic Interventional Radiology Practice. J. Vasc. Interv. Radiol. 2021, 32, 907–915.e3. [Google Scholar] [CrossRef] [PubMed]
- Baxter, N.B.; Yoon, A.P.; Chung, K.C. Variability in the Use of Disposable Surgical Supplies: A Surgeon Survey and Life Cycle Analysis. J. Hand Surg. Am. 2021, 46, 1071–1078. [Google Scholar] [CrossRef] [PubMed]
- Wang, E.Y.; Zafar, J.E.; Lawrence, C.M.; Gavin, L.F.; Mishra, S.; Boateng, A.; Thiel, C.L.; Dubrow, R.; Sherman, J.D. Environmental Emissions Reduction of a Preoperative Evaluation Center Utilizing Telehealth Screening and Standardized Preoperative Testing Guidelines. Resour. Conserv. Recycl. 2021, 171, 105652. [Google Scholar] [CrossRef]
- Grinberg, D.; Buzzi, R.; Pozzi, M.; Schweizer, R.; Capsal, J.F.; Thinot, B.; Le, M.Q.; Obadia, J.F.; Cottinet, P.J. Eco-Audit of Conventional Heart Surgery Procedures. Eur. J. Cardiothorac. Surg. 2021, 60, 1325–1331, Erratum in Eur. J. Cardiothorac. Surg. 2021, 60, 1481–1481. [Google Scholar] [CrossRef]
- Talibi, S.S.; Scott, T.; Hussain, R.A. The Environmental Footprint of Neurosurgery Operations: An Assessment of Waste Streams and the Carbon Footprint. Int. J. Environ. Res. Public Health 2022, 19, 5995. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, G.A.; Petit, H.J.; Reiter, A.J.; Westrick, J.C.; Hu, A.; Dunn, J.B.; Gulack, B.C.; Shah, A.N.; Dsida, R.; Raval, M.V. Environmental Impact and Cost Savings of Operating Room Quality Improvement Initiatives: A Scoping Review. J. Am. Coll. Surg. 2023, 236, 411–423. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.K.; Ellenbecker, M.J.; Moure-Ersaso, R. Alternatives for Treatment and Disposal Cost Reduction of Regulated Medical Wastes. Waste Manag. 2004, 24, 143–151. [Google Scholar] [CrossRef]
- Salama, K.; AlObireed, A.; AlBagawi, M.; AlSufayan, Y.; AlSerheed, M. Assessment of Occupational Radiation Exposure among Medical Staff in Health-Care Facilities in the Eastern Province, Kingdom of Saudi Arabia. Indian J. Occup. Environ. Med. 2016, 20, 21. [Google Scholar] [CrossRef]
- Kim, Y. The Radiation Problem and Its Solution from a Health Communication Perspective. J Korean Med. Sci. 2016, 31 (Suppl. S1), S88. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, A.; Tanigawa, K.; Ohtsuru, A.; Yabe, H.; Maeda, M.; Shigemura, J.; Ohira, T.; Tominaga, T.; Akashi, M.; Hirohashi, N.; et al. Health Effects of Radiation and Other Health Problems in the Aftermath of Nuclear Accidents, with an Emphasis on Fukushima. Lancet 2015, 386, 479–488. [Google Scholar] [CrossRef] [PubMed]
- Aboah, M.; Miyittah, M.K. Estimating Global Water, Sanitation, and Hygiene Levels and Related Risks on Human Health, Using Global Indicators Data from 1990 to 2020. J. Water Health 2022, 20, 1091–1101. [Google Scholar] [CrossRef] [PubMed]
- Van Minh, H.; Hung, N.V. Economic Aspects of Sanitation in Developing Countries. Environ. Health Insights 2011, 5, EHI.S8199. [Google Scholar] [CrossRef]
- Steenmeijer, M.A.; Rodrigues, J.F.D.; Zijp, M.C.; Waaijers-van Der Loop, S.L. The Environmental Impact of the Dutch Health-Care Sector beyond Climate Change: An Input–Output Analysis. Lancet Planet. Health 2022, 6, e949–e957. [Google Scholar] [CrossRef]
- Urden, L.D. Patient Satisfaction Measurement: Current Issues and Implications. Prof. Case Manag. 2002, 7, 194–200. [Google Scholar] [CrossRef]
- Kilbourne, A.M.; Keyser, D.; Pincus, H.A. Challenges and Opportunities in Measuring the Quality of Mental Health Care. Can. J. Psychiatry 2010, 55, 549–557. [Google Scholar] [CrossRef]
- Freeman, T. Using Performance Indicators to Improve Health Care Quality in the Public Sector: A Review of the Literature. Health Serv. Manag. Res. 2002, 15, 126–137. [Google Scholar] [CrossRef]
- Turnhout, E.; Tuinstra, W.; Halffman, W. Environmental Expertise: Connecting Science, Policy and Society, 1st ed.; Cambridge University Press: Cambridge, UK, 2019. [Google Scholar] [CrossRef]
- Diao, M.; Holloway, T.; Choi, S.; O’Neill, S.M.; Al-Hamdan, M.Z.; Van Donkelaar, A.; Martin, R.V.; Jin, X.; Fiore, A.M.; Henze, D.K.; et al. Methods, Availability, and Applications of PM 2.5 Exposure Estimates Derived from Ground Measurements, Satellite, and Atmospheric Models. J. Air Waste Manag. Assoc. 2019, 69, 1391–1414. [Google Scholar] [CrossRef]



| % (n) | |
|---|---|
| Geographical area (based on country of research) | |
| Europe | 43.5 (20) |
| North America | 34.8 (16) |
| Asia-Pacific | 15.2 (7) |
| South America | 4.3 (2) |
| Intercontinental | 2.2 (1) |
| Healthcare setting (based on main focus of research) | |
| Single hospital | 63.0 (29) |
| Multiple hospitals | 19.6 (9) |
| National level | 4.3(2) |
| Healthcare center | 2.2 (1) |
| Healthcare center and home | 2.2 (1) |
| Mental healthcare (multiple centers) | 2.2 (1) |
| Primary healthcare (multiple centers) | 2.2 (1) |
| Renal service | 2.2 (1) |
| Multiple healthcare centers incl. renal services | 2.2 (1) |
| Healthcare activities (based on main focus of research) | |
| Surgery 1 | 43.5 (20) |
| All-in setting | 30.4 (14) |
| Radiology 2 | 6.5 (3) |
| Renal services | 4.3 (2) |
| Ambulance transport coronary incidents | 2.2 (1) |
| Emergency care | 2.2 (1) |
| Intravitreal injection | 2.2 (1) |
| Medication prescription (inhalers) | 2.2 (1) |
| Teleconsultation | 2.2 (1) |
| Use of sharps containers | 2.2 (1) |
| Multiple departments | 2.2 (1) |
| Article | Country and Healthcare Setting | Healthcare Activities | Environmental Impact (Pressure)—Number per Type | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Resource Use | Pollutant Emission | Waste Generation | Mixed | ||||||
| Water | Energy | Mixed | Air | Water | |||||
| Jolibois et al. (2002) [18] | France, hospital | All-in setting | 1 | ||||||
| Gilliam et al. (2008) [19] | UK, hospital | Laparoscopic surgery | 1 | ||||||
| Seifrtová et al. (2008) [20] | Portugal, multiple hospitals | All-in setting | 4 | ||||||
| Somner et al. (2008) [21] | UK, multiple hospitals | Surgical scrubbing | 2 | 1 | |||||
| Lin et al. (2010) [22] | Taiwan, multiple hospitals | All-in setting | 10 | ||||||
| Masino et al. (2010) [23] | Canada, health center | Teleconsultation | 1 | ||||||
| Connor et al. (2010) [24] | UK, renal service | Renal services | 1 | 4 | 11 | 4 | |||
| Zander et al. (2011) [25] | UK, hospital | Ambulance transport coronary incidents | 2 | ||||||
| Eker and Bilgili (2011) [26] | Turkey, multiple healthcare centers incl renal services | All-in setting | 30 | ||||||
| Riedel (2011) [27] | USA, hospital | All-in setting | 2 | ||||||
| Eckelman et al. (2012) [3] | USA, hospital | Use of laryngeal mask airway | 2 | ||||||
| Grimmond and Reiner (2012) [28] | USA, hospital | Use of sharps containers | 2 | ||||||
| Power et al. (2012) [29] | USA, national | Laparoscopic surgery | 3 | 2 | |||||
| Goullé et al. (2012) [30] | France, hospital | All-in setting | 3 | ||||||
| Tay et al. (2013) [31] | Australia, hospital | Use of anesthetics | 2 | ||||||
| Morris et al. (2013) [32] | UK, hospital | Cataract surgery | 1 | 1 | 8 | 1 | 1 | ||
| Gros et al. (2013) [33] | Spain, hospital | All-in setting | 16 | ||||||
| Southorn et al. (2013) [34] | UK, multiple hospitals | Orthopedic surgery | 3 | ||||||
| Debois et al. (2013) [35] | USA, hospital | Coronary surgery | 1 | ||||||
| Diwan et al. (2013) [36] | India multiple hospitals | All-in setting | 14 | ||||||
| Lui et al. (2014) [37] | Canada, multiple hospitals | Head and neck surgery | 16 | ||||||
| McCarthy et al. (2014) [38] | Ireland, hospital | Radiology | 1 | ||||||
| Maamari et al. (2015) [39] | Lebanon, multiple hospitals | All-in setting | 1 | ||||||
| Dias-Ferreira et al. (2015) [40] | Portugal, hospital | Per department | 19 | ||||||
| Thiel et al. (2015) [41] | USA, hospital | Hysterectomy (robotic vs. human) | 2 | ||||||
| De Sa et al. (2016) [42] | Canada, hospital | Orthopedic surgery (total knee arthroplasty) | 7 | ||||||
| Maughan et al. (2016) [43] | UK, multiple mental healthcare centers | All-in setting | 1 | 2 | 1 | ||||
| Chen et al. (2017) [44] | China, healthcare center and home | Peritoneal dialysis | 1 | 2 | 9 | 2 | |||
| Jha et al. (2017) [45] | India, hospital | All-in setting | 13 | ||||||
| MacNeill et al. (2017) [46] | Canada, UK and USA, multiple hospitals | Surgery | 4 | 2 | 2 | 18 | |||
| Berner et al. (2017) [47] | Chile, hospital | Surgery 1 | 6 | 12 | 3 | ||||
| Esmaeli et al. (2018) [48] | UK, hospital | Diagnostical radiology | 3 | ||||||
| Khan et al. (2019) [49] | Pakistan, multiple hospitals | All-in setting | 4 | ||||||
| Wilkinson et al. (2019) [50] | UK, national | Medication prescription (inhalers) | 1 | ||||||
| Kooner et al. (2019) [51] | Canada, hospital | Orthopedic surgery 2 | 11 | ||||||
| Hsu et al. (2020) [52] | USA, hospital | Emergency care | 13 | ||||||
| De Oliveira Klein et al. (2021) [53] | Brazil, hospital | All-in setting | 5 | ||||||
| Rammelkamp et al. (2021) [54] | USA, hospital | Surgery 3 | 44 | ||||||
| Garcia-Sanz-Calcedo et al. (2021) [55] | Spain, multiple primary healthcare centers | All-in setting | 1 | 1 | |||||
| Patel and Smith-Steinert (2021) [56] | USA, hospital | Surgery | 1 | ||||||
| Cameron et al. (2021) [57] | USA, hospital | Intravitreal injection | 4 | ||||||
| Chua et al. (2021) [58] | USA, hospital | Interventional radiology | 1 | 2 | 4 | ||||
| Baxter et al. (2021) [59] | UK, multiple hospitals | Wrist and radius injury surgery | 1 | ||||||
| Wang et al. (2021) [60] | USA, hospital | Elective spinal surgery | 1 | ||||||
| Grinberg et al. (2021) [61] | France, hospital | Coronary surgery | 1 | 2 | 1 | ||||
| Talibi et al. (2022) [62] | UK, hospital | Neuro surgery | 1 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sijm-Eeken, M.; Jaspers, M.; Peute, L. Identifying Environmental Impact Factors for Sustainable Healthcare: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 6747. https://doi.org/10.3390/ijerph20186747
Sijm-Eeken M, Jaspers M, Peute L. Identifying Environmental Impact Factors for Sustainable Healthcare: A Scoping Review. International Journal of Environmental Research and Public Health. 2023; 20(18):6747. https://doi.org/10.3390/ijerph20186747
Chicago/Turabian StyleSijm-Eeken, Marieke, Monique Jaspers, and Linda Peute. 2023. "Identifying Environmental Impact Factors for Sustainable Healthcare: A Scoping Review" International Journal of Environmental Research and Public Health 20, no. 18: 6747. https://doi.org/10.3390/ijerph20186747
APA StyleSijm-Eeken, M., Jaspers, M., & Peute, L. (2023). Identifying Environmental Impact Factors for Sustainable Healthcare: A Scoping Review. International Journal of Environmental Research and Public Health, 20(18), 6747. https://doi.org/10.3390/ijerph20186747












