How Does Living in Temporary Accommodation and the COVID-19 Pandemic Impact under 5s’ Healthcare Access and Health Outcomes? A Qualitative Study of Key Professionals in a Socially and Ethnically Diverse and Deprived Area of London
Abstract
:1. Introduction
2. Methods
2.1. Participant Sample and Recruitment
- ○
- Inclusion Criteria:
- ▪
- Professional who is currently working and/or has worked with U5TA and their families either directly or indirectly, i.e., does not interact with families but is still responsible for them (e.g., someone in the local authority or higher-up administration in a non-profit, services, management, etc.).
- ▪
- Currently working in the London Borough of Newham (LBN) at the time of the interview.
- ▪
- Come from one of the following stakeholder groups: Health Visitor (HV), Health Professional (HP), Non-profit Organisation (NP), and the Local Authority of LBN (LA).
- ▪
- Professionals could be from any department, specialities, and/or field as long as they meet the other criteria.
- ○
- Exclusion Criteria:
- ▪
- Professional who has not worked with U5TA and their families in any capacity.
- ▪
- Not currently working in LBN.
2.2. Study Design
Topic Guide
2.3. Data Analysis
3. Results
3.1. Professional Characteristics
Role Types and Services Provided
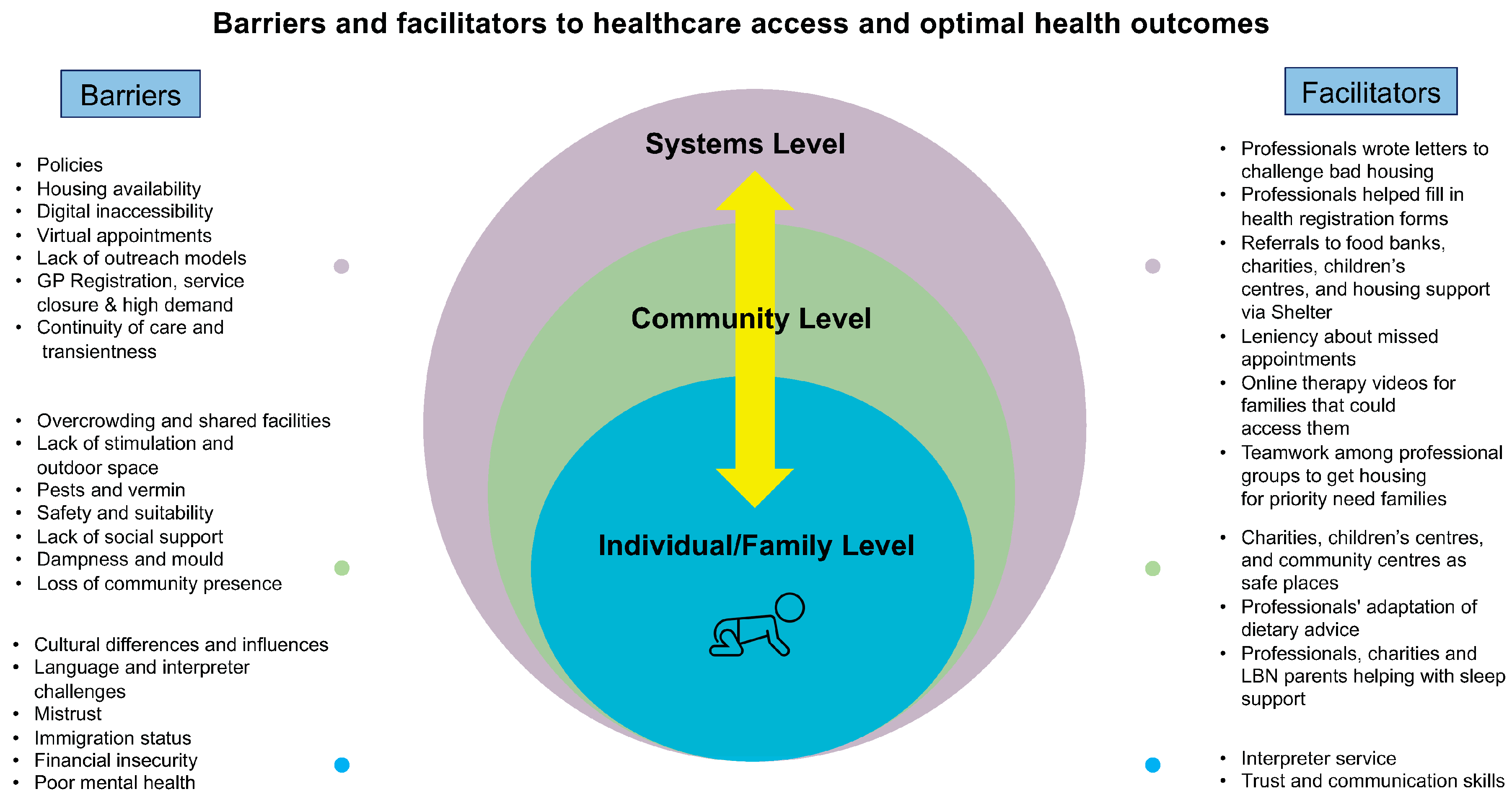
3.2. Barriers and Facilitators
3.2.1. Individual/Family Level
I. Poor Mental Health
“…Well, [parents] cannot look after their children. So definitely, it’s like, it flows down, you know, so that is, I mean, that social effects is no good for the children that we work with. I think things that might make it easier for families to engage, you [know], to have good accommodation that is number one. If you have a roof over your head, if you are comfortable, if your mind is settled, definitely, we have better health outcomes for these families, but because you know they are depressed, a lot of anxiety…” (HV2)
“…then it stops them accessing everything you know. They’re so concerned about their housing that it just ripples out from there, just affects everything, so it really kind of almost makes me a bit redundant because I can’t help.” (HP4)
II. Language and Interpreter Challenges
“So much information on the NHS website; they are like in British English. So, for people that do not have English as their first language, then it’s a big barrier because they don’t understand what you’re saying. Our areas as identified, you know, like a language barrier [in] homelessness is a key, key issue.” (HV2)
“…I think they’re all [language, cultural differences] definitely barriers, but I think that we always try to sort of think of ways around them like we always have access to [the] language line. So, we always have interpreters that we can use over the phone, which makes a really big difference.” (NP1)
III. Cultural Differences and Influences
“…[One] Mum said to me today: ‘I went to the local shops’ because she was looking for some shops to buy her own cultural fruit because she’s African, and she said, ‘I couldn’t find those shops.’ She says she ‘feels like an alien down the street’ because she’s not… seeing the people that resemble her ethnicity, and so yeah, I understand what she means about the alien analogy." (LA1)
"For instance, you might tell them that for a newborn child, they don’t need to put them on a pillow or something, but in terms of some of the culture, they prefer to put the babies on the pillow to [give] support. They feel that otherwise, their head is not going to be the way they want it. They want the baby to lie still in one place and all that. So those are some things, and if you don’t understand the culture, they might see it as you’re being disrespectful or something.” (HV5)
“…sometimes language barrier also makes it very difficult to give them the information that you feel that they need, because sometimes you might even go [through an] interpreter, but then again, sometimes the interpreter might be biased because they are the same like this. They speak the same language, so sometimes what you’re telling them…you don’t know what they say to them.” (HV5)
“In some families where they live in the hierarchical setup, the in-laws or the grandparents have a real influence on child rearing and development. So, in terms of seeking or adopting public health advice around weaning, for example, health, nutrition that [are] influenced by the practices of maybe the mother-in-law, that sister-in-law or the grandparents in terms of how a new mom would feed. So, you’ve got that conflicting advice, and you’ve also got some of its own things around cultural practices of what they did, culturally, which, as far as they’re concerned: ‘When I looked after you, you grew up fine. You’re fine’…” (HV3)
IV. Immigration Status and Financial Insecurity
“…in terms of the deprivation that a lot of these families experience who do not have recourse to public funds because of their immigration issues, they are families who have struggled the worst, I would say, during the pandemic…families were stuck…didn’t have any status at the time, who were very much invisible, but were working for cash-in-hand, so they were maintaining their families. But the pandemic happened, and all the work stopped. Therefore, they weren’t able to pay their rent, so, therefore, they were coming through the front doors of social care, and these are the families that we’ve been working quite long and hard with since the beginning of COVID.” (LA1)
V. Mistrust and Communication Skills
“…some people don’t believe in immunisation…and you tell them about immunisation, [and] it’s not something that they do, or they want to do…when I was in the Jewish community…Immunisation you have to literally [have to] win their trust before they can immunise their children, and if one person says to them, this nurse is good, you can let her immunise your child, yes, the whole of them will come, but if something negative, nobody will come to you, so you also need to win their trust.” (HV5)
“I think the work that we have to do is about gaining their confidence in using our services. It may be that you’re dealing with a client that has been moved 20 times, so by the time that they see us, it might be that their faith in services is completely eroded because they just have kind of been left behind. They’ve been unseen, unknown, unnoticed….” (HV4)
" I think it’s more about understanding because health visiting services, in particular, is not something that’s universal, universally available across the world, so I think it’s kind of breaking the barriers in terms of understanding what our role is and what we can bring to that family. So, I think this is where [the] kind of our communication skills are important, you know, and it’s about utilising interpreters so that we can be clear to parents, so that…we know that they can understand what we’re saying to them and then they can be involved in the discussion as well." (HV4)
3.2.2. Community Level
I. Safety and Suitability
“…I don’t think I’ve been to any temporary accommodation, that is, you know, that is conducive for families. I don’t think I’ve been to any, to be honest with you.” (HV2)
“There were safety issues as well…one family was in a converted pub, and they had two rooms…there was a safety aspect in terms of the parents had to be with the children all the time. They had to go down the corridor and downstairs to do the washing up in a tiny sink. There were no kitchen facilities, and yeah, it was really, really tough for them…there was sort of like bunk beds in one room, so there wouldn’t have been anywhere for the children to play. The access to the building was a fire escape…[but] I think mom had a buggy [and how] she just used to struggle going up and down with the buggy, as well as the other children…” (HP5)
“It’s a B&B…but [I] think it’s now used mainly for our temporary accommodation. It’s a very big building, but even when you are going in as a professional, you are scared because the lighting in the building is not right…we see people loitering around smoking, you know, so you, yourself as a professional, you feel all scared and, you know, on top [of] homeless families that have young children, they’re not able to come out because it’s not safe for them…” (HV2)
III. Lack of Stimulation and Outdoor Space
“Children grow by, you know, play and stimulation, but in their case, they are limited; they can’t do all that. There is no garden for them to play, so they are confined to the four corners of the room, thereby making their health condition worse.” (HV2)
“But then in terms of their milestones, I think I have seen in terms of speech development…there’s been an increase in the amount of throwback I had to do in speech delay. And I think that’s definitely tied into COVID and that there are no children centres, so it’s stimulation issues, so it’s kind of lack of stimulation that could be the cause of it. But then, also the fact that there aren’t any facilities that are available in the Community for children to access, play and explore [or] school to help improve those skills [which] are lacking." (HV4)
IV. Pests, Vermin, Dampness, and Mould
“Another major one is like infection. When they are in a more dirty environment, it affects their health, especially children with asthma. When they live in an environment that is damp with mould, it increases, you know, the rate at which they wheeze. It affects the respiratory system, and then they start having to go to Accident and Emergency all the time…” (HV2)
“ I would say breathing, definitely respiratory difficulties, which then leads onto triggering other things like skin irritations, especially when you’ve got pests, and there’s droppings around the properties. [Be]cause children, especially under-fives, they will crawl, they will walk, they will pick things up and put them in their mouths and so, there’s quite a lot that I would say would affect them and that could be the worst-case scenario that affects their development.” (LA1)
V. Social Support and Community Presence
“…we don’t have any power to change where they’re living…we don’t have that authority…it’s in the hands of the housing services or who’s working with that family, but you know, before COVID, at least we could provide them with alternative places, provide them with safe places that they could go to—children centres, activity groups, you know where, at least, that they can have that safe space where their children can play, where they can explore, and you know it would be an escape from their surroundings…because…being in these places would be detrimental to anybody’s mental health…it’s not healthy either…it’s quite small, it’s cold, it’s damp so, at least, we were able to provide…these safe places in the community where…their children could play and safely and learn these new skills and even be exposed to other children because they wouldn’t [or] might not have that [at] home,…which is important for them to develop…” (HV4)
"There’s low self-esteem for [the] parent. They are not happy. They’re not comfortable…with what they’ve got. They’re not able to mix with other parents…even when they take their children to school because they’re not proud of where they are living, so it has a significant impact, not on the child alone, [but] then even on the parent…” (HV2)
“We probably aren’t reaching as many families as we could be because we don’t have a community presence at the moment with everything shift[ing] into digital services, and also not all families are tech savvy…we may do our initial contacts with our clients, but our main way of communicating with them moving forward to deal with their case would be via email and telephone, and it’s not very often that you will get good correspondence back and because it’s just not the way that they are used to dealing with things.” (NP2)
3.2.3. Systems Level
I. GP Registration, Service Closure, and High Demand
“…when I’m thinking about it, it [COVID] has made a huge impact…I’ve got lots of families who want to [go to] dentists, and there’s specialist dentist service, but they can’t get to them. Health visitors aren’t going out…There’s a lot that’s changed for COVID because if we’ve all shut down, although we didn’t, this is what I don’t get, I still carried on—I did a lot of stuff with video, admittedly for a while, but we opened clinics up again. Not quite sure why everyone else hasn’t…even that GPs and things like, what’s happening? So, I do worry…they haven’t got the same access they would have before COVID because there just isn’t the appointments that were, everyone’s really behind.” (HP4)
“Because I think before…clients that I work with, quite often see the same health visitor like every week or something at the Children’s centre because that’s where he goes, so they just happened to kind of see them. But now it’s kind of relying on that client or that health visitor to go out of their way to have a call or visit, which obviously the health visitor has just to do to the best ability, but they have to see so many different families that maybe families those that they need support but who don’t know how to reach out for it.” (NP1)
II. Continuity of Care and Transientness
“So they may be in the area, and we may not even know about them. But some of the barriers are also around whose clients are they because they [are] really registered to another local authority and therefore, one could argue that they are the responsibility of the health visitors in that area. However, while living temporarily in our area, I think geographically, we hold an element of responsibility, but there’s a barrier in communication between I think with some of the clinicians may experience, barriers in terms of communication around notification of movements into and out of the borough in a timely manner. For that really hinders developing…implementing effective care packages to…meet the individualised needs of those families.” (HV3)
III. Digital Inaccessibility and Virtual Appointments
“I think we all assumed that most families did [have internet access], but it’s still something that, yeah, not all have, especially if they’re in temporary accommodation. I think, you know, things aren’t always set up, and because they don’t know how long they’re going to be there…it’s something we’re still battling with and again.” (HP3)
“…the technology as well, it’s not 100% sometimes, it can cause like glitches in the assessment. It might not work, or they can’t hear you; they can’t hear me. I think it’s better now, now that we have video, it’s made things better, the assessment better. As opposed to the beginning of lockdown when it was just on the telephone, which is more difficult because you can’t see anything, so all you can take is what the parent has told you at that point.” (HV4)
“But then again, we always have failsafe, so we do have options to bring them into clinic. But then it’s not the ‘go to’ anymore, virtual is the ‘go to’ now, so I have found it challenging.” (HV4)
IV. Housing Availability
“…some families, they live in their boxes because they sometimes tell them, oh, you’re going to be here for three months, six months, and they’re waiting to be moved forever, and you’ve got families that they’ve been living in accommodation for ages, some of them up to eight [years] you know so they’re just sitting there waiting. Obviously,…the demand to live in London is more…” (HV7)
“You receive an email from new housing saying there’s no houses out there for this family at the moment. There’s nothing. He may have to wait a year even being on emergency [list].” (HV1)
“…I think that the housing, in a way, it can impact it’s like a chain reaction. It can impact loads of other parts of the family’s life. Most about primarily their health basically poor housing can equal to having poor health because it limits the access to health services if there are not services that are kind of in tune to picking up those families that are kind of transients basically.” (HV4)
V. Policies and Lack of Outreach Models
“So, I think in terms of accessing, I think it is harder when population groups are a bit more dispersed …in the sense of I’m comparing it with rough sleeping and you can have more, there’s more outreach models that you’ll know certain hostels that you can work closely with. There might be outreach street workers. I’m not saying it in any way, this makes this easier, but you’ve got greater strategies. I think, with families in temporary accommodation, that can be a bit harder. I think they’re not necessarily as visible in terms of being seen as homeless.” (LA3)
4. Discussion
4.1. Strengths and Limitations
4.2. Implications and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kopanitsa, V.; McWilliams, S.; Leung, R.; Schischa, B.; Sarela, S.; Perelmuter, S.; Sheeran, E.; d’Algue, L.M.; Tan, G.C.; Rosenthal, D.M. A systematic scoping review of primary health care service outreach for homeless populations. Fam. Pract. 2022, 39, cmac075. [Google Scholar] [CrossRef] [PubMed]
- Rosenthal, D.; Lewis, C.; Heys, M.; Schoenthaler, A.; Ucci, M.; Hayward, A. Barriers to Optimal Health for Under 5s Experiencing Homelessness and Living In Temporary Accommodation in High-Income Countries: A Scoping Review. Ann. Public Health Res. 2021, 8, 1103. [Google Scholar]
- Rosenthal, D.M.; Ucci, M.; Heys, M.; Hayward, A.; Lakhanpaul, M. Impacts of COVID-19 on vulnerable children in temporary accommodation in the UK. Lancet Public Health 2020, 5, e241–e242. [Google Scholar] [CrossRef] [PubMed]
- Scott, E. Lockdown 1.0 and the Pandemic One Year on: What Do We Know about the Impacts? UK Parliament- House of Lords Library. 2021. Available online: https://lordslibrary.parliament.uk/lockdown-1-0-and-the-pandemic-one-year-on-what-do-we-know-about-the-impacts/ (accessed on 16 January 2022).
- WHO Director-General. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 23 November 2022).
- Radcliff, E.; Crouch, E.; Strompolis, M.; Srivastav, A. Homelessness in Childhood and Adverse Childhood Experiences (ACEs). Matern. Child Health J. 2019, 23, 811–820. [Google Scholar] [CrossRef]
- Lewer, D.; King, E.; Bramley, G.; Fitzpatrick, S.; Treanor, M.C.; Maguire, N.; Bullock, M.; Hayward, A.; Story, A. The ACE Index: Mapping childhood adversity in England. J. Public Health 2020, 42, e487–e495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ONS. UK Homelessness: 2005 to 2018-Assessment of the Comparability and Coherence of Existing UK Government Data Sources on Homelessness. 2019. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/housing/articles/ukhomelessness/2005to2018 (accessed on 16 January 2022).
- Shelter England. 253,000 People Are Trapped in Temporary Accommodation—Shelter England. Available online: https://england.shelter.org.uk/media/press_release/homeless_in_a_pandemic_253000_people_are_trapped_in_temporary_accommodation_ (accessed on 31 October 2021).
- Shelter England. Homelessness in England 2021. 2021. Available online: https://assets.ctfassets.net/6sxvmndnpn0s/2PuyTofvY2k2Fi6uJxcd98/68fb35a1267c54ab3fc05896b8ab7a85/FINAL_Homelessness_in_England_2021_report.pdf (accessed on 30 May 2022).
- Ministry of Housing Communities & Local Government. Live Tables on Homelessness—GOV.UK. Statut Homelessness Dataset. 2020. Available online: https://www.gov.uk/government/statistical-data-sets/live-tables-on-homelessness#statutory-homelessness-live-tables (accessed on 11 October 2021).
- Authority, G.L. GLA Population Projections. Available online: https://apps.london.gov.uk/population-projections/ (accessed on 19 February 2022).
- Newham Council. Newham—Population—UTLA GLA | Newham | InstantAtlas Reports. Available online: https://www.newham.info/population/#/view-report/1ee4f94e929141d0bb9e4792ecdd8e89/___iaFirstFeature (accessed on 9 February 2022).
- Rosenthal, D.M.; Ucci, M.; Heys, M.; Schoenthaler, A.; Lakhanpaul, M.; Hayward, A.; Lewis, C. A Citizen Science Approach to Identifying Indoor Environmental Barriers to Optimal Health for Under 5s Experiencing Homelessness in Temporary Accommodation. Int. J. Environ. Res. Public Health 2022, 19, 3976. [Google Scholar] [CrossRef] [PubMed]
- Rosenthal, D.M.; Lakhanpaul, M. Child Health and Homelessness. In Transforming Early Childhood in England; Cameron, C., Moss, P., Eds.; UCL Press: London, UK, 2020; Available online: https://www.uclpress.co.uk/products/128464. (accessed on 18 September 2020).
- Lester, H.; Bradley, C.P. Barriers to Primary Healthcare for the Homeless: The General Practitioner’s Perspective. Eur. J. Gen. Pract. 2009, 7, 6–12. [Google Scholar] [CrossRef]
- Otokiti, A.U.; Thein, Y.Z.; Alabi, O. Challenges Faced by the Homeless Population in New York City: An Analysis of HealthCare Delivery and Utilization of Care. N. Y. Med. J. 2018, 12, 5–13. [Google Scholar]
- McLaughlin, C.G.; Wyszewianski, L. Access to Care: Remembering Old Lessons. Health Serv. Res. 2002, 37, 1441. [Google Scholar] [CrossRef] [Green Version]
- Rosenthal, D.M.; Heys, M.; Schoenthaler, A.; Hayward, P.A.; Ucci, M.; Lewis, C. How did living in temporary accommodation and the COVID-19 pandemic impact under 5s’ healthcare access and health outcomes? A qualitative study of key professionals in a socially and ethnically diverse and deprived area of London. Lancet 2022, 400, S75. [Google Scholar] [CrossRef]
- Palinkas, L.A.; Horwitz, S.M.; Green, C.A.; Wisdom, J.P.; Duan, N.; Hoagwood, K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm. Policy Ment. Health 2015, 42, 533. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parker, C.; Scott, S.; Geddes, A. Snowball Sampling; Atkinson, P., Delamont, S., Cernat, A., Sakshaug, J.W., Williams, R.A., Eds.; SAGE: New York, NY, USA, 2020. [Google Scholar] [CrossRef]
- Taylor, S.J.; Bogdan, R.; DeVault, M. Introduction to Qualitative Research Methods; Wiley: Hoboken, NJ, USA, 2016. [Google Scholar]
- Zoom Video Communications Inc. Security Guide-Zoom Video Communications Inc. Available online: https://d24cgw3uvb9a9h.cloudfront.net/static/81625/doc/Zoom-Security-White-Paper.pdf (accessed on 26 April 2022).
- Sah, L.K.; Singh, D.R.; Sah, R.K. Conducting Qualitative Interviews using Virtual Communication Tools amid COVID-19 Pandemic: A Learning Opportunity for Future Research. JNMA J. Nepal Med. Assoc. 2020, 58, 1103. [Google Scholar] [CrossRef] [PubMed]
- Archibald, M.M.; Ambagtsheer, R.C.; Casey, M.G.; Lawless, M. Using Zoom Videoconferencing for Qualitative Data Collection: Perceptions and Experiences of Researchers and Participants. Int. J. Qual. Methods 2019, 18, 1609406919874596. [Google Scholar] [CrossRef] [Green Version]
- Roberts, K.; Dowell, A.; Nie, J.B. Attempting rigour and replicability in thematic analysis of qualitative research data; A case study of codebook development. BMC Med. Res. Methodol. 2019, 19, 66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ritchie, J.; Spencer, L. (Eds.) Qualitative data analysis for applied policy research. In The Qualitative Researcher’s Companion; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2002; pp. 187–208. [Google Scholar] [CrossRef]
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 2013, 13, 117. [Google Scholar] [CrossRef] [Green Version]
- Fereday, J.; Adelaide, N.; Australia, S.; Eimear Muir-Cochrane, A. Demonstrating Rigor Using Thematic Analysis: A Hybrid Approach of Inductive and Deductive Coding and Theme Development. Int. J. Qual. Methods 2006, 5, 80–92. [Google Scholar] [CrossRef]
- Goldsmith, L.J. Using Framework Analysis in Applied Qualitative Research. Qual. Rep. 2021, 26, 2061–2076. [Google Scholar] [CrossRef]
- Salihu, H.M.; Wilson, R.E.; King, L.M.; Marty, P.J.; Whiteman, V.E. Socio-ecological Model as a Framework for Overcoming Bar-riers and Challenges in Randomized Control Trials in Minority and Underserved Communities. Int. J. MCH AIDS 2015, 3, 85–95. [Google Scholar]
- Rosenthal, D.M. Barriers and Facilitators to Optimising Health Outcomes and Accessing Health Care Services among under 5s Experiencing Homelessness in temporary Accommodation (U5TA) in England: A Case Study of a local authority in East London. Ph.D. Thesis, University College London, London, UK, 2018. [Google Scholar]
- Rosenthal, D.M.; Ucci, M.; Hayward, A.; Teakle, A.; O’Toole, S.; Whitaker, L.; Hauari, H.; Hollingworth, K.; Cameron, C.; Schoenthaler, A.; et al. 605 Socio-political determinants of health inequalities during the COVID-19 pandemic: Under 5s and their families living in temporary accommodation in a socially diverse and deprived population—Newham, East London. Arch. Dis. Child. 2022, 107 (Suppl. 2), A70–A71. [Google Scholar] [CrossRef]
- Rosenthal, D.M.; Hayward, A.; Ucci, M.; Teakle, A.; O’Toole, S.; Whitaker, L.; Hauari, H.; Hollingworth, K.; Cameron, C.; Schoenthaler, A.; et al. 576 Parental mental health and associations between living in temporary accommodation and socio-political determinants during the COVID-19 pandemic. Arch. Dis. Child. 2022, 107 (Suppl. 2), A71–A72. [Google Scholar] [CrossRef]
- Boyatzis, R.E. Transforming Qualitative Information: Thematic Analysis and Code Development; SAGE: New York, NY, USA, 1998; p. 184. Available online: http://books.google.com/books?hl=en&lr=&id=_rfClWRhIKAC&pgis=1 (accessed on 8 July 2021).
- QSR International. Best Qualitative Data Analysis Software for Researchers | NVivo. QSR International. Available online: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home?creative=605555104699&keyword=nvivo&matchtype=e&network=g&device=c&gclid=Cj0KCQiAyMKbBhD1ARIsANs7rEEmS573T9mQwlPzfwU-JWgQACMl4I8_lDGdjuOTUU3vyBYIgXXqO5saAvuKEALw_wcB (accessed on 13 November 2022).
- Schoenthaler, A.; Rosenthal, D.M.; Butler, M.; Jacobowitz, L. Medication adherence improvement similar for shared decision-making preference or longer patient-provider relationship. J. Am. Board Fam. Med. 2018, 31, 752–760. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. Review of Mandation for the Universal Health Visiting Service. 2016. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/592893/Review_of_mandation_universal_health_visiting_service.pdf (accessed on 6 July 2022).
- Group BFP. COVID-19 Timeline—British Foreign Policy Group. Available online: https://bfpg.co.uk/2020/04/covid-19-timeline/ (accessed on 7 March 2022).
- Cameron, C.; Moss, P. (Eds.) Transforming Early Childhood in England–Towards a Democratic Education; UCL Press: London, UK, 2020; Available online: https://www.uclpress.co.uk/collections/open-access/products/128464 (accessed on 10 December 2022).
- England and Wales Census 2011. Regional Ethnic Diversity—GOV.UK Ethnicity Facts and Figures. Published 1 August 2018; Last updated 11 July 2019. Available online: https://www.ethnicity-facts-figures.service.gov.uk/uk-population-by-ethnicity/national-and-regional-populations/regional-ethnic-diversity/latest#ethnic-diversity-by-area (accessed on 10 December 2022).
- We Are Researching. We Are Newham. Education and Play; UCL: London, UK, 2022; unpublished.
- Hobbs, A.; Bernard, R. Impact of COVID-19 on Early Childhood Education & Care—POST. UK Parliament Rapid Response. Available online: https://post.parliament.uk/impact-of-covid-19-on-early-childhood-education-care/ (accessed on 10 December 2022).
- Conti, G.; Dow, A. The Impacts of COVID-19 on Health Visiting in England First Results. 2020. Available online: https://discovery.ucl.ac.uk/id/eprint/10106430/ (accessed on 6 January 2021).
- House of Commons. The Housing Health and Safety Rating System (HHSRS)—House of Commons Library. 2019. Available online: https://commonslibrary.parliament.uk/research-briefings/sn01917/ (accessed on 30 June 2022).
- Arnaud, A.; Lioret, S.; Vandentorren, S.; Le Strat, Y. Anaemia and associated factors in homeless children in the Paris region: The ENFAMS survey. Eur. J. Public Health 2018, 28, 616–624. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Department for Levelling Up, Housing and Communities. Chapter 17: Suitability of Accommodation-Homelessness Code of Guidance for Local Authorities-Guidance-GOV.UK. 2018. Available online: https://www.gov.uk/guidance/homelessness-code-of-guidance-for-local-authorities/chapter-17-suitability-of-accommodation (accessed on 14 January 2022).
- The Homelessness (Suitability of Accommodation) (Amendment) (England) Order 2022. 2022. Available online: https://www.legislation.gov.uk/uksi/2022/521/contents/made (accessed on 7 July 2022).
- The Licensing and Management of Houses in Multiple Occupation and Other Houses (Miscellaneous Provisions) (England) Regulations. 2006. Available online: https://www.legislation.gov.uk/uksi/2006/373/made/data.pdf (accessed on 22 October 2022).
- Gov.UK. HM Government Social Distancing Review: Report; Government of the United Kingdom: London, UK, 2021. [Google Scholar]
- Thompson, E.L.; Galvin, A.M.; Rohr, D.; Klocek, C.; Lowe, H.; Spence, E.E. Navigating the system for families experiencing homelessness: A community-driven exploration of barriers encountered. J. Child. Poverty 2020, 26, 253–267. [Google Scholar] [CrossRef]
- Odd, D.; Stoianova, S.; Williams, T.; Odd, D.; Kurinczuk, J.J.; Wolfe, I.; Luyt, K. What is the relationship between deprivation, modifiable factors and childhood deaths: A cohort study using the English National Child Mortality Database. BMJ Open 2022, 12, e066214. [Google Scholar] [CrossRef]
- Richards, R.; Merrill, R.M.; Baksh, L. Health behaviors and infant health outcomes in homeless pregnant women in the United States. Pediatrics 2011, 128, 438–446. [Google Scholar] [CrossRef]
- Stein, J.A.; Lu, M.C.; Gelberg, L. Severity of homelessness and adverse birth outcomes. Health Psychol. 2000, 19, 524–534. [Google Scholar] [CrossRef]
- The Health Foundation. Relationship between Health and Residential Moves. Available online: https://health.org.uk/evidence-hub/housing/housing-stability-and-security/relationship-between-health-and-residential-moves (accessed on 27 August 2022).
- Cutts, D.B.; Bovell-Ammon, A.; de Cuba, S.E.; Sheward, R.; Shaefer, M.; Huang, C.; Black, M.M.; Casey, P.H.; Coleman, S.; Sandel, M.; et al. Homelessness During Infancy: Associations With Infant and Maternal Health and Hardship Outcomes. Cityscape A J. Policy Dev. Res. 2018, 20, 119–132. [Google Scholar]
- Roze, M.; Vandentorren, S.; Melchior, M. Mental health of mothers and children of homeless families in Ile de France. Results of the ENFAMS survey. Neuropsychiatr. Enfance Adolesc. 2019, 67, 313–318. [Google Scholar] [CrossRef]
- National Health Care for the Homeless Council. FACT SHEET Medical Ethics and COVID-19: Naming and Addressing the Moral Injury of Care during COVID-19. 2022. Available online: www.nhchc.org (accessed on 5 August 2022).
- Ranmal, R.; Tinson, A.; Marshall, L. How do Health Inequalities Intersect with Housing and Homelessness? Eur. J. Homelessness 2021, 15, 113–121. [Google Scholar]
- Galdas, P. Revisiting Bias in Qualitative Research: Reflections on Its Relationship With Funding and Impact. Int. J. Qual. Methods 2017, 16, 1609406917748992. [Google Scholar] [CrossRef]
- Pearce, A.; Dundas, R.; Whitehead, M.; Taylor-Robinson, D. Pathways to inequalities in child health. Arch. Dis. Child. 2019, 104, 998–1003. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Link, B.G.P.J. Social conditions as fundamental causes of disease. J. Health Soc. Behav. 1995, 35, 80–94. [Google Scholar] [CrossRef] [Green Version]
- Krieger, J.; Higgins, D.L. Housing and Health: Time Again for Public Health Action. Am. J. Public Health 2002, 92, 758. [Google Scholar] [CrossRef] [PubMed]
| Professional Group | Number of Professionals n (%) |
|---|---|
| Health Visitors | 7 (44) |
| Health Professionals | 4 (25) |
| Non-profit Sector | 2 (13) |
| Local Authority | 3 (19) |
| Age Group | n (%) |
| 25–29 | 3 (19) |
| 30–34 | 1 (6) |
| 35–39 | 1 (6) |
| 40–44 | 2 (13) |
| 45–49 | 4 (25) |
| 50–54 | 3 (19) |
| 55–59 | 1 (6) |
| 60–64 | 1 (6) |
| Gender | n (%) |
| Male | 2 (13) |
| Female | 14 (88) |
| Ethnic Group | n (%) |
| White (British and/or Any other White British background) | 7 (44) |
| Black (African or Caribbean) | 5 (31) |
| Asian or Asian British: Bangladeshi | 1 (6) |
| Mixed Ethnic background | 3 (19) |
| How Long Professionals Have Been in Current Role (Time Spans) | n (%) |
| =<6 months | 3 (19) |
| 7 month–1 year | 2 (13) |
| 1.1–2.5 years | 5 (31) |
| 2.6–5 years | 1 (6) |
| 5.1–10 years | 4 (25) |
| >10 years | 1 (6) |
| Total | 16 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosenthal, D.M.; Schoenthaler, A.; Heys, M.; Ucci, M.; Hayward, A.; Teakle, A.; Lakhanpaul, M.; Lewis, C. How Does Living in Temporary Accommodation and the COVID-19 Pandemic Impact under 5s’ Healthcare Access and Health Outcomes? A Qualitative Study of Key Professionals in a Socially and Ethnically Diverse and Deprived Area of London. Int. J. Environ. Res. Public Health 2023, 20, 1300. https://doi.org/10.3390/ijerph20021300
Rosenthal DM, Schoenthaler A, Heys M, Ucci M, Hayward A, Teakle A, Lakhanpaul M, Lewis C. How Does Living in Temporary Accommodation and the COVID-19 Pandemic Impact under 5s’ Healthcare Access and Health Outcomes? A Qualitative Study of Key Professionals in a Socially and Ethnically Diverse and Deprived Area of London. International Journal of Environmental Research and Public Health. 2023; 20(2):1300. https://doi.org/10.3390/ijerph20021300
Chicago/Turabian StyleRosenthal, Diana Margot, Antoinette Schoenthaler, Michelle Heys, Marcella Ucci, Andrew Hayward, Ashlee Teakle, Monica Lakhanpaul, and Celine Lewis. 2023. "How Does Living in Temporary Accommodation and the COVID-19 Pandemic Impact under 5s’ Healthcare Access and Health Outcomes? A Qualitative Study of Key Professionals in a Socially and Ethnically Diverse and Deprived Area of London" International Journal of Environmental Research and Public Health 20, no. 2: 1300. https://doi.org/10.3390/ijerph20021300
APA StyleRosenthal, D. M., Schoenthaler, A., Heys, M., Ucci, M., Hayward, A., Teakle, A., Lakhanpaul, M., & Lewis, C. (2023). How Does Living in Temporary Accommodation and the COVID-19 Pandemic Impact under 5s’ Healthcare Access and Health Outcomes? A Qualitative Study of Key Professionals in a Socially and Ethnically Diverse and Deprived Area of London. International Journal of Environmental Research and Public Health, 20(2), 1300. https://doi.org/10.3390/ijerph20021300









