Abstract
An umbrella review of previously published systematic reviews was conducted to determine the nature and extent of the patient and public involvement (PPI) in COVID-19 health and social care research and identify how PPI has been used to develop public health measures (PHM). In recent years, there has been a growing emphasis on PPI in research as it offers alternative perspectives and insight into the needs of healthcare users to improve the quality and relevance of research. In January 2022, nine databases were searched from 2020–2022, and records were filtered to identify peer-reviewed articles published in English. From a total of 1437 unique records, 54 full-text articles were initially evaluated, and six articles met the inclusion criteria. The included studies suggest that PHM should be attuned to communities within a sociocultural context. Based on the evidence included, it is evident that PPI in COVID-19-related research is varied. The existing evidence includes written feedback, conversations with stakeholders, and working groups/task forces. An inconsistent evidence base exists in the application and use of PPI in PHM. Successful mitigation efforts must be community specific while making PPI an integral component of shared decision-making.
1. Introduction
Over the past decade, there has been an increased emphasis on the importance of patient and public involvement (PPI) in health and social research as it provides alternative views and insights into the needs of healthcare users to improve the quality and relevance of research [1]. PPI integration into health and social care research gained momentum before the COVID-19 pandemic. However, the rapid response to the pandemic resulted in PPI being viewed as non-essential, leading to its minimal inclusion in research and, thereby, minimizing the contribution of patients, the public, and, particularly, minority groups in helping find solutions to the pandemic crisis [1].
The concept of patient and public involvement refers to conducting research ‘with’ or ‘by’ the public rather than ‘to’, ‘about,’ or ‘for’ them. Patients, potential patients, caregivers, and people who use health and social care services, as well as the representatives of organizations representing such people, are considered the public [2]. PPI creates an active partnership with patients, healthcare providers, members of the public, and researchers, with the goal of influencing and shaping research in a manner that is relevant and inclusive to individuals of various backgrounds and ethnicities [3]. The integration of PPI has been demonstrated to produce positive impacts on the quality and appropriateness of research during all stages of the research process, including the development of user-focused research objectives and questions, user-friendly information, improvements in recruitment strategies, the consumer-focused interpretation of data, and the enhanced implementation and dissemination of study results [4]. The National Institute for Health and Care Research (NIHR) has been instrumental in firmly entrenching PPI inclusion across publicly funded research in the United Kingdom, and a similar prioritization of PPI has been observed in other parts of Europe, Canada, the United States, and Australia [5]. Ireland, too, has adopted a nationwide approach to embedding PPI in all academic health and social care research through the creation of a network on PPI [6].
Patient and public involvement (PPI) is not a recent phenomenon. It shares attributes with participatory research, community and citizen engagement, consumer involvement, and community empowerment. While we are citing the NIHR definition, many other conceptualizations exist. What they have in common is the central, co-producing, and participatory role of patients, as well as members of the public and communities, in the research process.
Although the past decade has shown the great expansion of the PPI evidence base, the reporting of PPI and its impact is inconsistent as well as lacking in information about the context and process of patient and public engagement. The inadequate reporting of PPI creates significant barriers to advancing the adoption of PPI strategies in health and social care research as it produces substantial challenges in the appraisal, interpretation, and synthesis of evidence for systematic reviews, as well as the ethical implications of reporting PPI to improve quality and transparency for the use of research findings [5]. Particularly during the pandemic, a high number of systematic reviews relating to COVID-19 were conducted with PROSPERO records indicating findings that were not replicable and poorly reported [7].
In order to implement strategies to address the COVID-19 pandemic, such as patient and public involvement and the utilization of public health measures, it is critically important to have consistent and reproducible findings. On the societal level, PPI-generated trust and acceptance in research, greater benefits for the community, new and improved services, valuable changes in practice/partnership lead to positive changes and outcomes, and finally, improved relationships between professionals and communities [8].
Public health measures (PHM) aim to reduce the transmission, severity of illness, and death and are critical strategies to address pre-COVID-19 pandemic outbreaks, such as severe acute respiratory syndrome (SARS) and influenza. PHM strategies prior to the COVID-19 pandemic included personal and pharmaceutical measures such as travel, social distancing, the use of personal protective equipment, and medications [9]. PHM during COVID-19 was defined as actions taken by individuals or various groups of people, such as national and local governments, academic and research institutions, communities, and international entities, to slow or stop the spread of infectious diseases [10]. They can exist as non-pharmaceutical groups and are a combination of behavioral, environmental, social, and systems interventions that are used to contain the infection and mitigate disease risk [11,12]. PHM are not limited to public messaging and education but include restrictions to activities and limited access to facilities and institutions, including systems-level interventions (e.g., local and national lockdowns, contact management), and behavioral interventions (e.g., physical distancing/isolation/quarantine, hand hygiene precautions, mandatory use of face masks).
Focusing on patient and public involvement (PPI) can enable the right questions and depth of understanding to exist for problems from the user’s perspective. PPI enhances the efficiency, design, and quality of healthcare initiatives and facilitates decision-making regarding resource allocations and the usability of services by including information about the capabilities, needs, and priorities of local people [13]. PPI has an impact on equity if it succeeds in bringing together diverse communities and social groups and provides a ‘voice’ for marginalized groups, thus reducing the over-representation of some interests. Attention should be directed to the implementation of PPI, as it can have the adverse effect of enlarging the gap between communities and creating greater inequities, particularly among marginalized populations. PPI implementation should accommodate populations who may have limited access to resources and are impacted by varying and unforeseen circumstances [14].
With the use of PPI, not only are the patient and public considered stakeholders, but they are also simultaneously the ones receiving care and are directly affected by their involvement.
2. Aim, Objectives and Research Questions
For this study, we used the umbrella review as a research methodology which consists of collecting, reviewing, and analyzing systematic reviews and meta-analyses on a specific research topic [15,16]. The primary aim of this umbrella review was to determine and describe the nature and extent of the patient and public involvement (PPI) in COVID-19 health and social care research. A second aim was to identify research gaps in PPI to inform future studies and research funding priorities.
In this review, the objectives were to:
- Explore the scientific evidence of incorporating PPI.
- Summarize the current evidence on COVID-19, including PPI, and determine where and when the research was conducted.
- Identify the members of the public and the types of patients who participated.
- Identify any gaps in the literature or study designs that should be further explored and emphasized in future public health measures (PHM) and PPI research.
To help us plan for conducting a structured database that could search for relevant systematic reviews, we developed research questions based on the population, phenomena of interest, and context (PICo) framework. The following research questions followed the population, phenomena of interest, and context (PICo) framework [15] in which the population included the general public regardless of age, gender, and race/ethnicity:
- Have systematic reviews of PHM during the COVID-19 pandemic reported on assessed PPI activities?
- What were the PPI activities, and who/what populations were likely to be left out?
- What are the similarities and differences in the effectiveness of PHM between the systematic review studies?
3. Research Design
The findings of reviews pertinent to a research question can be compared and contrasted via an umbrella review [15]. Therefore, this review was conducted using the JBI manual for evidence synthesis for umbrella reviews [16], along with the PRISMA-ScR checklist [17]. Before undertaking this umbrella review, a protocol was registered with PROSPERO: CRD42022307608 [18].
3.1. Search Stratgey
Using the PICo framework [19], synonyms, keywords, and controlled vocabulary terms were identified by a public health librarian (N.T.) with expertise in conducting systematic reviews, and this was reviewed for accuracy by the lead author (N.F.) of the research team. These terms were developed under the following concepts: (P) patient and public involvement; (I) public health measures; (Co) COVID-19 and full search strategies are presented in Supplementary Materials Table S1. A systematic review filter was adapted from the National Library of Medicine [20] to filter the results by article type. A three-step search approach was used to identify the relevant literature reviews:
- We conducted preliminary searches to find published reviews in the literature on patient and public involvement (PPI) and public health measures (PHM) during the pandemic. Among the databases searched were the 3iE Database, BMC Systematic Reviews, Campbell Collaboration, Centre for Reviews and Dissemination, Cochrane Library, JBI Evidence Synthesis, PROSPERO, and Google Scholar.
- In the next stage of the search, nine databases (EBSCO interface—Academic Search Ultimate, APA PsycINFO, CINAHL, Family & Society Studies Worldwide, Health Source: Nursing/Academic Edition, MEDLINE; Epistemonikos, ScienceDirect and WHO COVID-19 Global Literature) were searched on 21 January 2022.
- Finally, a Google Scholar search was again conducted with the included studies identified from the title/abstract stage. Using the cited by feature, reference lists were checked to identify additional studies that could be appropriate for inclusion.
3.2. Inclusion and Exclusion Criteria
The umbrella review included the literature reviews published in English in peer-reviewed journals. Since the pandemic began at the beginning of 2020, the studies were limited to 2020–2022. Any type of literature review was considered (e.g., systematic review, rapid review, integrative review, scoping review, narrative review, meta-analyses, etc.) with studies of any design:
- Qualitative studies include designs such as grounded theory, ethnography, phenomenology, action research, and qualitative descriptive.
- Quantitative studies include both experimental (e.g., randomized trials, non-randomized trials) and observational (e.g., cohort, cross-sectional) study designs.
- We also considered case series, individual case reports, health intervention, or service development.
Studies with human participants were included regardless of age, gender, and race/ethnicity. The interventions/phenomena of interest were public health measures (PHM), and the World Health Organization’s Taxonomy and Glossary of Public Health and Social Measures [10] was used to identify related terms as inclusion criteria for PHM. Studies, including PPI, defined as research carried out by patients and members of the public contributing to the design, implementation, and dissemination of research, were included. Regardless of the geographical location, all settings of the study were included (e.g., healthcare facilities of any type including, but not restricted to schools, in-patients, hospitals, medical centers, community-based care, and long-term care facilities). Non-systematic reviews and individual research studies were excluded.
3.3. Study Screening and Selection
Ten graduate students (D.A., L.B., S.L., C.L., E.M., A.M., A.N., L.R., M.D.S., and A.D.S.) organized into five groups independently screened titles/abstracts and then full texts for inclusion. All students involved in reviewing the studies were Master of Public Health and Master of Health Administration graduate students. Several meetings were held prior to reviewing the articles to discuss definitions of PPI and analysis strategies for the purpose of training. Prior to the screening, reviewers were provided with a list of inclusion criteria. This was undertaken to ensure that reviews were conducted consistently among the ten reviewers as a method to minimize reviewer bias. To minimize selection bias, the screening was independently completed by two group members. Discrepancies during the title/abstract and full-text review stages were resolved through discussion among the reviewers within each group. If a consensus could not be reached, a third reviewer (N.F.) was consulted. Throughout the reviews, multiple meetings were conducted to discuss all the decisions completed independently or through a second reviewer. Reviewer and selection bias is possible; however, protocols were in place prior to starting the review process to ensure that these biases were minimal.
3.4. Assessment of Methodological Quality/Critical Appraisal of the Included Systematic Reviews
The public health librarian (N.T.) assigned full-text articles identified from the title/abstract review to each group member. These articles were then independently assessed by the other group members for methodological quality using the JBI Critical Appraisal Checklist for systematic reviews and research syntheses [16]. This checklist is designed to check the quality of the systematic reviews, not the quality of the included primary studies. The final appraisal column was calculated for risk of bias by classifications of “N/A”, “No”, and “Unclear”. These were then compared to the risk of bias number ranges—Low (0–3), Medium (4–6), High (7–11)—and assigned to the corresponding level. This umbrella review included all studies, regardless of their methodological quality.
3.5. Data Extraction
Data extraction was completed by one reviewer using the JBI Data Extraction Form for the Review of Systematic Reviews and Research Syntheses [16]. Data were independently checked and verified by a second reviewer. A third reviewer (N.F.) was consulted when there was a lack of consensus.
3.6. Data Summary
To discuss the findings, the research team compared and contrasted the data extracted from the included studies. An analysis of the data was conducted in a tabular format and was complemented by a narrative synthesis.
4. Results
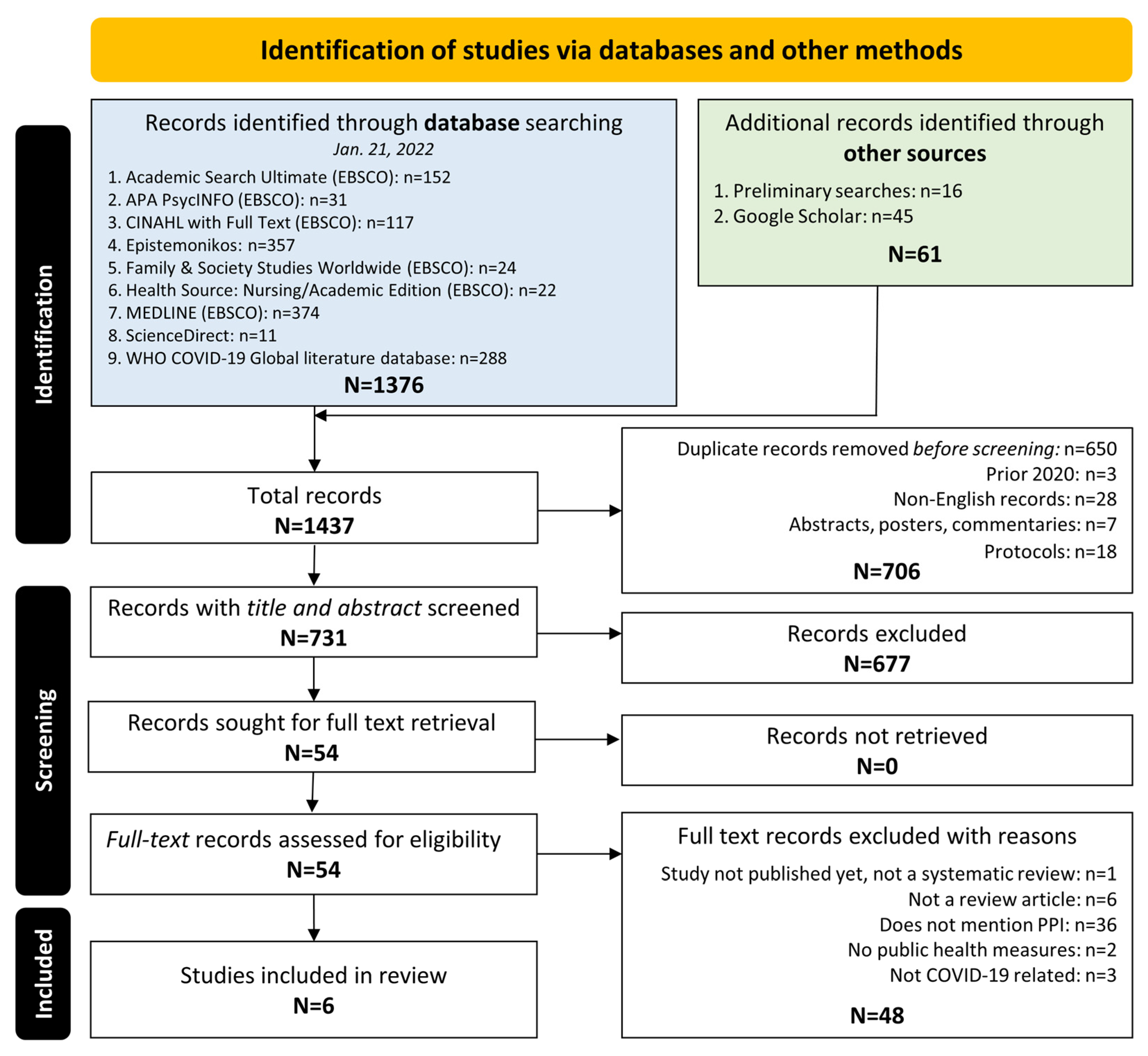
4.1. Study Inclusion
The search and screening process can be seen in Figure 1. We obtained a total of 1437 records across all databases and imported these into Zotero: a citation management software [21]. After removing 706 duplicates, a total of 731 distinct records were screened based on the title/abstract in Rayyan: a tool that allows for the independent screening and coding of studies [22]. Fifty-four articles were identified for a full-text review, with a final selection of six systematic reviews that met the inclusion criteria [23,24,25,26,27,28]. In Supplementary Materials Table S2, the excluded full-text articles are listed along with their reasons for exclusion (e.g., no patient and public involvement (PPI) or public health measures (PHM) being discussed, or the articles not being review studies).
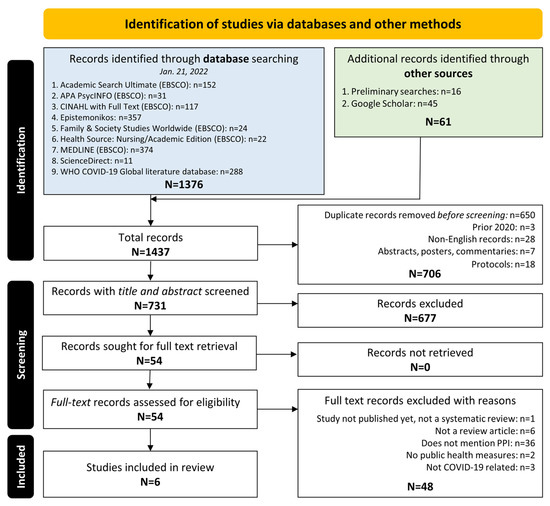
Figure 1.
PRISMA flow diagram.
4.2. Methodological Quality of Included Systematic Reviews
We assessed the methodological quality of the six included reviews from the title/abstract stage and reported the findings in Supplementary Materials Table S3. Two reviewers appraised the quality of each article by following the JBI Critical Appraisal Checklist for Systematic Reviews and Research Syntheses. Scores were assigned for adherence to each question. The final appraisal column was calculated for risk of bias by classifications of “N/A”, “No”, and “Unclear”. These then were compared to the risk of bias number ranges—Low (0–3), Medium (4–6), High (7–11)—and were assigned to the corresponding level. This umbrella review included six studies, regardless of their methodological quality. After the initial evaluations of articles, disagreements were assessed and resolved by a designated third reviewer. The “Risk of Bias” column is a result of the total number of points scored for each appraisal question. The six reviews were not eliminated according to their results in this tool.
4.3. Characteristics of Included Studies
The included six reviews were published in 2021, and their summaries are presented in Supplementary Materials Table S4. Our research questions were clearly stated in all the included reviews either in the title, abstract, or in text. A publication bias was not addressed in all the included reviews. Three reviews were determined to have a medium-level risk of bias [23,24,25], and the remaining three reviews were considered to have a low-level risk of bias [26,27,28]. The sources of the included studies and inclusion criteria were appropriate for all reviews. The criteria for appraisal included an appropriate and independent appraisal and was conducted in most of the included studies. The methods used to minimize error in data extraction were not specified in most of the included studies. There were two or more databases searched in all the included studies.
4.4. Findings of the Review
Table 1 and Table 2 show the patient and public involvement (PPI) measures and research findings for each of the six studies included in this review. Table 3 provides an overview of the quantitative and qualitative studies and the PPI, and public health measure (PHM) approaches to groups/populations, settings, outcomes, benefits, and gaps identified in the study.

Table 1.
Quantitative data from included review articles.

Table 2.
Qualitative data from included review articles.

Table 3.
Overview of quantitative and qualitative findings.
5. Summary of Evidence
Table 4 provides a summary of evidence on the effects of patient and public involvement (PPI) in public health measures (PHM) and community involvement included in the studies of our review. The findings and communities involved in each study differed with respect to the behavioral, social, and/or systems interventions that were used to contain the virus and mitigate transmission. Several themes emerged relating to the benefits of PPI, PHM approaches to PPI populations, PPI engagement strategies, and challenges to PPI in health and social research.

Table 4.
Summary of evidence for the effect of patient and public involvement (PPI) on public health measures (PHM) and community involvement.
5.1. Benefits of Patient and Public Involvement (PPI)
During COVID-19 in the United Kingdom, over 4000 local volunteer groups were formed, with as many as three million participants to meet the communities’ needs during the pandemic. In addition, the National Health Service recruited three times their initial target of volunteers, demonstrating that the public wanted to be involved [26]. Mao et al. [26] pointed out that when traditional public services struggled to respond effectively, mutual aid groups played a role in the COVID-19 response. These groups established new partnerships, networks, and knowledge that may continue to be beneficial in the long term. For example, during the pandemic, some of the existing volunteer groups were able to adjust, change focus, and adapt to new needs and challenges.
Adebisi et al. [23] suggested that PPI can work toward improving weak healthcare systems, combating the spread of misinformation, and better meeting the needs of vulnerable populations. Raymond & Ward [28] identified similar findings and expanded further by advising that community engagement was indispensable for designing public health interventions. This allowed for the complexity of individuals with an emphasis on different influences creating inequity and marginalization. Banerjee et al. [24] found PPI to be lacking; however, there was sustained interest on the patient’s and the public’s behalf and a willingness to engage. With improved PPI for the individuals and populations considered at high risk of mortality during the COVID-19 pandemic, there needs to be an improvement in decision making, increased comprehension in regard to the understanding of risks, and increased discussions with healthcare professionals and family members [24].
5.2. Public Health Measures (PHM) Approaches
All six review articles discussed the different approaches that communities around the world took in response to mitigating and controlling the COVID-19 pandemic. Ernawati et al. [25] identified an evaluation of society’s awareness around knowledge, attitude, and practice (KAP) in the prevention of COVID-19 as an effective transmission prevention strategy. Similarly, Mao et al. [26] reviewed a combination of behavioral and social approaches and found that community involvement and volunteering were imperative in the public’s response to COVID-19. Adebisi et al. [23] described an approach by South African governments in which they urged citizens to obey COVID-19 precaution measures. Many awareness programs were implemented in order to address pandemic stigmatization, fear, and misinformation related to COVID-19 [23]. They also noted the South African Ministry of Health utilized social media platforms to spread awareness regarding COVID-19. Banerjee et al. [24] found studies that provided publicly available portals, although none were specifically aimed for utilization by the patients and the public. Pegollo et al. [27] discussed the utilization of digital contact tracing (DCT) in response to reducing infection incidence. Lastly, Raymond & Ward [28] noted that local context and community engagement were crucial when implementing public health interventions in order to combat COVID-19.
5.3. Patient and Public Involvement (PPI) Population and Engagement Strategies
All community engagement actors and approaches were characterized by a combination of local leaders, community and faith-based organizations, community groups, health facility committees, individuals, and key stakeholders. However, the studies did not include specific equity considerations. Raymond & Ward [28] discussed the impact of COVID-19 on low- and middle-income countries. They identified the barriers created by poverty, inequality, and the inability to comply with lockdown orders. Several adaptive responses were identified in communities throughout different countries, leading the authors to conclude that community engagement holds the potential for future solutions through local context to develop social solutions and effective engagement and communication.
Regarding engagement strategies, Adebisi et al. [23] identified 13 African countries that implemented numerous risk communication and community engagement (RCCE) strategies in response to the decreasing prevalence of COVID-19. Pegollo et al. [27] reviewed digital contact tracing (DCT) in the general population of several countries. The reviewers note that downloading an application was a crucial step in the engagement process and for contract tracing to be successful. Individuals in support of DCT felt it was essential to protect others, and the positive effects outweighed concerns relating to privacy and surveillance. The uptake of DCT was lower in individuals with fewer non-pharmacological interventions, such as mask-wearing and social distancing. Overall, areas of interest regarding engagement in the use of DCT included privacy, government trust/surveillance, cybersecurity, social media sentiment, communication, and usefulness [27].
5.4. Challenges to Patient and Public Involvement (PPI) and Public Health Measures (PHM) during the COVID-19 Pandemic
This study included reviews that identified several challenges experienced by communities during the pandemic. Adebisi et al. [23] identified the main challenges to include trust and distrust among the government and officials, cultural, social, and religious resistance, the spreading of misinformation, and continuous issues caused by weak healthcare systems. Raymond & Ward [28] noted challenges relating to misinformation and the fear of being socially denounced, causing pandemic sanctions. An additional challenge was explaining the COVID-19 virus using a combination of different traditional, religious, and scientific ideologies, causing confusion for the public [28]. Pegollo et al. [27] noted the challenge of sharing personal data in healthcare when citizens’ values of privacy had to be overcome. A solution recommended by the authors was to develop a digital solution that was bound by law and respected citizens’ concerns. Mao et al. [26] found many challenges to be centered around constraints and limitations on in-person gatherings and mandating individuals, communities and institutions to adopt unfamiliar practices to continue serving the surrounding communities. Both studies by Mao et al. [26] and Raymond & Ward [28] mentioned the public’s challenge with combating social isolation. Banerjee et al. [24] discovered that the development of COVID-19 mortality risk tools with public engagement was lacking, and there was an absence of mortality risk information designed for patients with underlying conditions. The reviewers found that overall, there was an urgent need to better understand the specific information desired by communities, and further evaluate the impact on vulnerable populations to improve public health. Though traditional modes and models of governance and health systems infrastructures were challenged by COVID-19, regional context and public engagement were essential ideas when creating adequate public health interventions to meet the issues associated with the pandemic [28].
6. Discussion
Table 5 shows the overall evidence of patient and public involvement (PPI) in the included reviews. The table is divided into four categories: COVID-19 public health measures, PPI approach and mechanisms, the diversity of PPI stakeholder groups, and the benefits of efficacy that use PPI strategies. Each category is followed by a general combined overview of the studies included in the review.

Table 5.
Overview of evidence for patient and public involvement (PPI) included in the reviews.
The purpose of this umbrella review is to provide an overview and synthesis of previously published systematic reviews to determine the nature and extent of PPI in COVID-19 health and social care research to identify where PPI has been used to develop public health measures (PHM). The aim of this umbrella review is to explore scientific evidence for the benefit of incorporating PPI, summarizing the evidence of COVID-19 and PPI to determine where and when the research was conducted, identify members of the public and patients who participated and identify gaps in the literature that need to be further explored.
This umbrella review found that when the public and patients were involved in research practices and processes, valuable perspectives were both generated and found useful for the target audience and community at large. Currently, there is a limited number of studies on PPI during the COVID-19 pandemic, resulting in a gap in the literature relating to this evolving public health topic. The lack of information about the context and process of PPI relating to COVID-19 creates barriers to advancing strategies that can address the pandemic.
While each of the included reviews looked at different measures and levels of patient and public involvement (PPI), there were some commonalities. Through PPI, communities were able to mobilize efforts and identify and adapt to community needs [23,26]. Overall the studies reviewed highlighted PPI involvement in various stages; however, there was a lack of consistent engagement and follow-up throughout the processes [25,26,27]. Furthermore, there were both lacking and inconsistent methods established to report and share effective PPI strategies.
To establish effective community engagement, local organizations need to improve the support provided as well as enhance collaboration and cooperation [23,26]. This may be performed by implementing a follow-up system with the patients and public to ensure their continued involvement, as the decision-making process is critical for everyone involved. Community engagement needs to also better include more geographical settings amongst various populations [28]. Nevertheless, the evidence supports the fact that when barriers were created by poverty and inequality, communities could formulate adaptive responses to COVID-19 [28]. When PPI has an equity-based focus, it allows communities experiencing these inequities to take targeted action, develop solutions, and create conditions for health and well-being. PPI can bring together diverse communities and social groups and provides a ‘voice’ for marginalized populations. As the reviews demonstrated, PPI has the potential to combat the spread of misinformation, resulting in increased trust in public health measures [23,28].
7. Limitations
A thorough review was conducted for this umbrella review. However, considering the fact that 1437 records were narrowed down to six articles for inclusion, the relevant studies may have been omitted due to systematic errors during the selection, appraisal, or data extraction process. This umbrella review only includes evidence from the six systematic reviews previously detailed, which may result in desirable details of certain interventions being omitted. In addition, the six articles included in the review addressed PPI in various settings, allowing us to draw conclusions regarding the benefit of PPI as it relates to COVID-19. We relied on the information included in the articles, which is an inherent weakness. For example, an umbrella review is unable to identify a phenomenon that has not been addressed in systematic reviews. An inherent bias may also be a limitation of this review due to one round of appraisal and extraction.
8. Conclusions
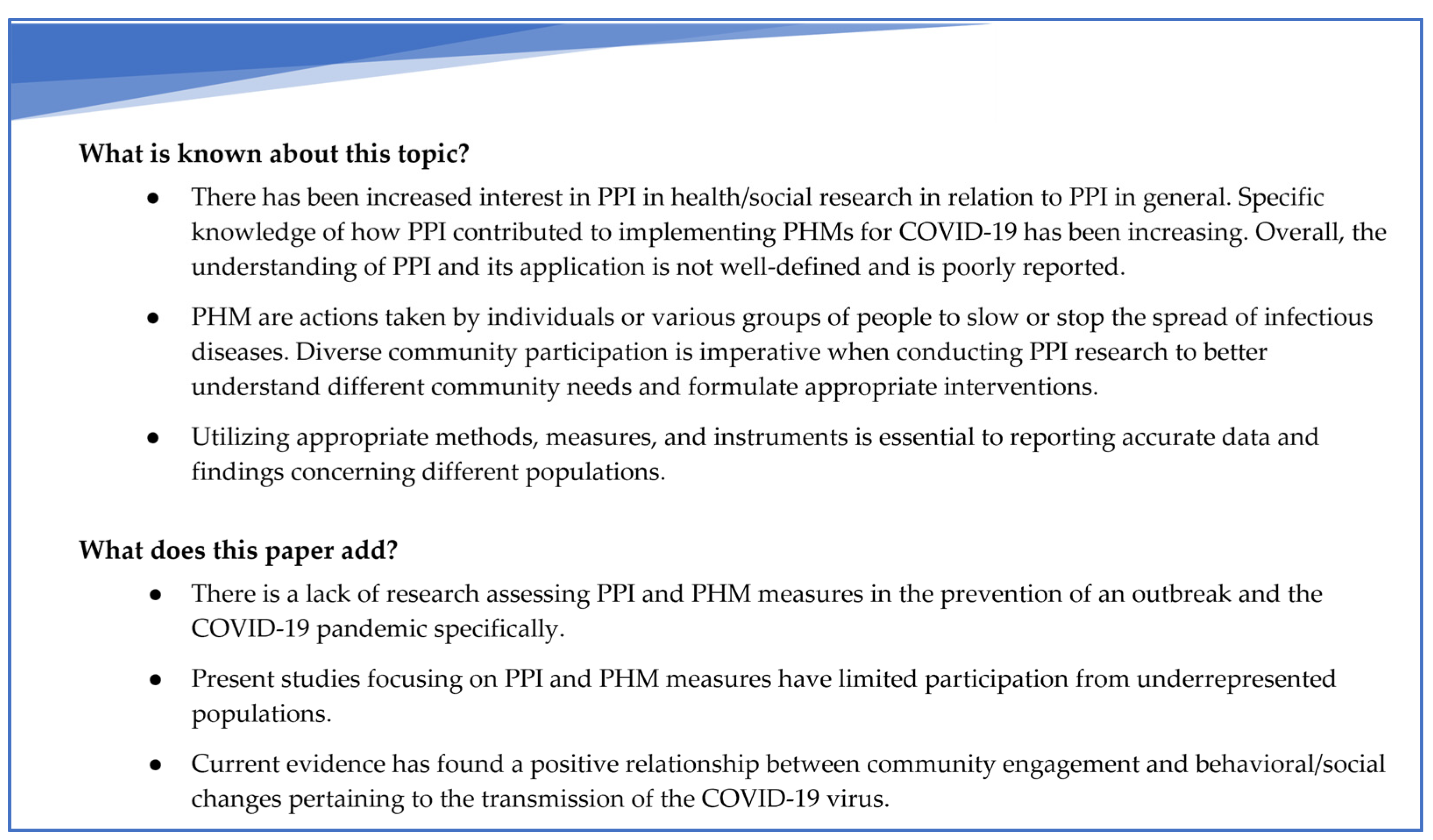
Figure 2 outlines the existing knowledge on patient and public involvement (PPI) in health and social research, as well as how this paper contributes to it.
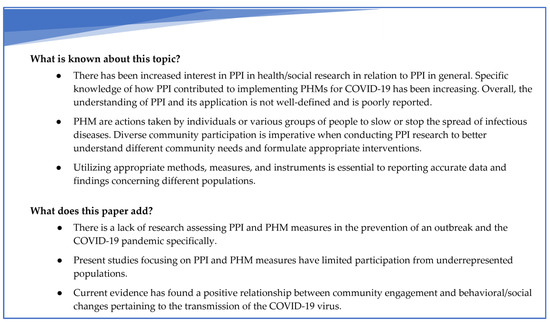
Figure 2.
Summary of the existing knowledge on patient and public involvement (PPI) in health and social research and contributions of this umbrella review to it.
In exploring the current and potential ways that we may utilize and benefit from patient and public involvement (PPI) in regard to COVID-19 and public health, we came across many gaps in the literature. A review of the literature presented several opportunities for future practice. Several of the studies indicated that volunteerism, community cohesion, and/or the spontaneous development of assistance programs were prevalent in the public response to COVID-19 [25,26,28]. Policymakers should include these groups when implementing public health measures (PHM). Community and volunteer groups in PPI can be instrumental in gaining public support for PHM and promoting adherence.
Digital technology should be used by policymakers to include the public in data collection and shared decision making. Patient portals or apps can be used to collect public health information and provide feedback. The use of web-based meeting spaces allows for PPI with the inclusion of a wider range of community members and groups when discussing methods of pandemic control and deciding which PHM would be most beneficial to the community. It is critical to respect the privacy concerns of citizens when utilizing digital technology [27].
Some of the included studies also suggest that PHM should be tailored to communities and set within a sociocultural context [23,26,28]. Successful mitigation efforts should be community-specific and have PPI that is integral to shared decision making. This umbrella review highlighted the lack of decision making when patients and the public were involved in PPI, which should be addressed and assessed in further research. Further research should be conducted with PPI to determine which PHM could benefit particular communities and which PHM might cause aversion to adherence. The literature revealed that PHM that did not have widespread community support or did not consider the socio-cultural context were less likely to be followed. Further research is needed to determine the effectiveness of PHM when culturally competent PPI is included in decision making and implementation.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20064887/s1, Table S1: Search terms and search strategies; Table S2: Excluded articles with reasons; Table S3: Assessment of methodological quality/critical appraisal of included studies; Table S4: Summaries of included studies.
Author Contributions
Conceptualization, K.F., T.K., N.F. and N.T.; keyword identification, N.F. and N.T.; search strategies and literature searches, N.T.; acquisition, analysis, and interpretation of data, N.F., D.A., L.B., S.L., C.L., E.M., A.M., A.N., L.R., M.D.S. and A.D.S.; drafting and revising the manuscript—all authors contributed equally. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study did not require ethical approval.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Murphy, E.; Tierney, E.; Shé, É.N.; Killilea, M.; Donaghey, C.; Daly, A.; Roche, M.; Loughlin, D.M.; Dinneen, S. COVID-19: Public and Patient Involvement, Now More than Ever. HRB Open Res. 2020, 3, 35. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Research. What Is Patient and Public Involvement and Public Engagement? Available online: https://www.spcr.nihr.ac.uk/PPI/what-is-patient-and-public-involvement-and-engagement (accessed on 8 March 2023).
- National Institute for Health and Care Research Annual Report 2020/2021. Available online: https://www.nihr.ac.uk/documents/annual-report-20202021/30206 (accessed on 20 June 2022).
- Brett, J.; Staniszewska, S.; Mockford, C.; Herron-Marx, S.; Hughes, J.; Tysall, C.; Suleman, R. Mapping the Impact of Patient and Public Involvement on Health and Social Care Research: A Systematic Review. Health Expect. 2014, 17, 637–650. [Google Scholar] [CrossRef] [PubMed]
- Staniszewska, S.; Brett, J.; Simera, I.; Seers, K.; Mockford, C.; Goodlad, S.; Altman, D.G.; Moher, D.; Barber, R.; Denegri, S.; et al. GRIPP2 Reporting Checklists: Tools to Improve Reporting of Patient and Public Involvement in Research. BMJ 2017, 358, j3453. [Google Scholar] [CrossRef] [PubMed]
- PPI Ignite Network. Promoting Excellence and Inspiring Innovation. Available online: https://ppinetwork.ie/ (accessed on 17 January 2023).
- Dotto, L.; Kinalski, M.D.A.; Machado, P.S.; Pereira, G.K.R.; Sarkis-Onofre, R.; dos Santos, M.B.F. The Mass Production of Systematic Reviews about COVID-19: An Analysis of PROSPERO Records. J. Evid. Based Med. 2021, 14, 56–64. [Google Scholar] [CrossRef] [PubMed]
- McKenna, H. Perspectives: Patient and Public Involvement and Research Impact: A Reciprocal Relationship. J. Res. Nurs. 2015, 20, 723–728. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control Guide to Public Health Measures to Reduce the Impact of Influenza Pandemics in Europe—‘The ECDC Menu’. Available online: https://www.ecdc.europa.eu/en/publications-data/guide-public-health-measures-reduce-impact-influenza-pandemics-europe-ecdc-menu (accessed on 17 January 2023).
- World Health Organization. Tracking Public Health and Social Measures: Taxonomy and Glossary. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/phsm (accessed on 23 March 2022).
- Michie, S.; West, R. Behavioural, Environmental, Social, and Systems Interventions against Covid-19. BMJ 2020, 370, m2982. [Google Scholar] [CrossRef] [PubMed]
- Talic, S.; Shah, S.; Wild, H.; Gasevic, D.; Maharaj, A.; Ademi, Z.; Li, X.; Xu, W.; Mesa-Eguiagaray, I.; Rostron, J.; et al. Effectiveness of Public Health Measures in Reducing the Incidence of COVID-19, SARS-CoV-2 Transmission, and Covid-19 Mortality: Systematic Review and Meta-Analysis. BMJ 2021, 375, e068302. [Google Scholar] [CrossRef] [PubMed]
- Pizzo, E.; Doyle, C.; Matthews, R.; Barlow, J. Patient and Public Involvement: How Much Do We Spend and What Are the Benefits? Health Expect. 2015, 18, 1918–1926. [Google Scholar] [CrossRef] [PubMed]
- Adeyemi, I.; Sanders, C.; Ong, B.N.; Howells, K.; Quinlivan, L.; Gorman, L.; Giles, S.; Amp, M.; Monaghan, E.; Naseem, S.; et al. Challenges and Adaptations to Public Involvement with Marginalised Groups during the COVID-19 Pandemic: Commentary with Illustrative Case Studies in the Context of Patient Safety Research. Res. Involv. Engag. 2022, 8, 13. [Google Scholar] [CrossRef] [PubMed]
- Aromataris, E.; Fernandez, R.; Godfrey, C.M.; Holly, C.; Khalil, H.; Tungpunkom, P. Summarizing Systematic Reviews: Methodological Development, Conduct and Reporting of an Umbrella Review Approach. JBI Evid. Implement. 2015, 13, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Aromataris, E.; Fernandez, R.; Godfrey, C.; Holly, C.; Khalil, H.; Tungpunkom, P. Chapter 10: Umbrella Reviews. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020; Available online: https://jbi-global-wiki.refined.site/space/MANUAL (accessed on 8 March 2023).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Fouladi, N.; Tchangalova, N.; Ajayi, D.; Bonilla, L.; Lovett, C.; Liggett, S.; Manukulasuriya, M.; Millwee, E.; Munoz, A.; Njonkou, C.; et al. COVID-19 Public Health Measures and Patient and Public Involvement (PPI) in Health and Social Care Research: An Umbrella Review Protocol. PROSPERO. 2022. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022307608 (accessed on 8 March 2023).
- Lockwood, C.; Munn, Z.; Porritt, K. Qualitative Research Synthesis: Methodological Guidance for Systematic Reviewers Utilizing Meta-Aggregation. Int. J. Evid. Based Healthc. 2015, 13, 179–187. [Google Scholar] [CrossRef] [PubMed]
- National Library of Medicine Search Strategy Used to Create the Pubmed Systematic Reviews Filter. Available online: https://www.nlm.nih.gov/bsd/pubmed_subsets/sysreviews_strategy.html (accessed on 6 February 2023).
- Puckett, J. Zotero: A Guide for Librarians, Researchers, and Educators; Association of College and Research Libraries: Chicago, IL, USA, 2011; ISBN 978-0-8389-8589-2. [Google Scholar]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan: A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Adebisi, Y.A.; Rabe, A.; Lucero-Prisno III, D.E. Risk Communication and Community Engagement Strategies for COVID-19 in 13 African Countries. Health Promot. Perspect. 2021, 11, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, A.; Pasea, L.; Manohar, S.; Lai, A.G.; Hemingway, E.; Sofer, I.; Katsoulis, M.; Sood, H.; Morris, A.; Cake, C.; et al. ‘What Is the Risk to Me from COVID-19?’: Public Involvement in Providing Mortality Risk Information for People with ‘High-Risk’ Conditions for COVID-19 (OurRisk.CoV). Clin. Med. 2021, 21, e620–e628. [Google Scholar] [CrossRef] [PubMed]
- Ernawati, K.; Cantika, I.B.; Isaputri, R.R.; Andari, A.W.; Ramadhan, M.F.; Nathasia, S.K.; Rifqatussa’adah, R.; Hasibuan, H.S.; Astuti, L.T.M.; Ismail, Y. Community Knowledge, Attitudes and Behaviors in Prevention of COVID-19 Transmission: A Systematic Review. Int. J. Public Health Sci. 2021, 10, 16–26. [Google Scholar] [CrossRef]
- Mao, G.; Fernandes-Jesus, M.; Ntontis, E.; Drury, J. What Have We Learned about COVID-19 Volunteering in the UK? A Rapid Review of the Literature. BMC Public Health 2021, 21, 1470. [Google Scholar] [CrossRef] [PubMed]
- Pegollo, L.; Maggioni, E.; Gaeta, M.; Odone, A. Characteristics and Determinants of Population Acceptance of COVID-19 Digital Contact Tracing: A Systematic Review. Acta Biomed. 2021, 92, e2021444. [Google Scholar] [CrossRef] [PubMed]
- Raymond, C.B.; Ward, P.R. Community-Level Experiences, Understandings, and Responses to COVID-19 in Low- and Middle-Income Countries: A Systematic Review of Qualitative and Ethnographic Studies. Int. J. Environ. Res. Public Health 2021, 18, 12063. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).